Abstract
Background:
Patient and community-level social and economic conditions impact hypertension risk and control. We examined adult hypertension management guidelines to explore whether and how existing guidelines refer to social care activities.
Objective:
To explore how hypertension guidelines reference social care activities.
Research Design:
Systematic scoping review of clinical guidelines for adult hypertension management. We employed a PubMed search strategy to identify all hypertension guidelines published in the US between 1977– 2019. We reviewed all titles to identify the most updated versions focused on non-pregnant adults with hypertension. We extracted instances where guidelines referred to social determinants of health (SDH) or social care activities. The primary outcome was how guidelines covered social care activities, defined using a framework adapted from the National Academies of Sciences, Engineering and Medicine (NASEM).
Results:
Search terms yielded 126 guidelines. Thirty-six guidelines met inclusion criteria. Of those 72% (26/36) recommended social care activities as part of hypertension management; 58% recommended clinicians change clinical practice based on social risk information. These recommendations often lacked specific guidance around how to directly address social risk factors or reduce the impact of these risks on hypertension management. When guidelines referred to specific social factors, patient financial security was the most common. Over time, hypertension guidelines have included more references to SDH.
Conclusion:
Information about SDH is included in many hypertension guidelines, but few guidelines provide clear guidance for clinicians or health systems on how to identify and address social risk factors in the context of care delivery.
Keywords: Hypertension, blood pressure, social determinants of health, guideline
Introduction
One third of US adults have hypertension, a major risk factor for mortality from heart disease and stroke1,2. Despite the life threatening consequences of uncontrolled hypertension and numerous treatment guidelines for elevated blood pressure, gaps in evidence remain in all aspects of the hypertension control cascade2. Though hypertension control across the US improved between 1999–2014, recent data suggest this trend has not continued: hypertension control rates went from 31.8% in 1999–2000 to 53.8% in 2013–2014 and 43.7% in 2017–2018. Significant disparities also persist across racial and ethnic groups3,4. Having lower income, identifying as non-Hispanic Black, and lacking health insurance all increase the risk of uncontrolled hypertension1,3,5,6. Disparities in blood pressure control contribute to higher cardiovascular morbidity and mortality among vulnerable and low socioeconomic groups7. Given the extent and consequences of uncontrolled disease, hypertension control is a central focus of public health, primary care, and several medical sub-specialties.
The rapidly evolving science around social determinants of health (SDH) is relevant to efforts to improve hypertension awareness, treatment, and control. The World Health Organization defines SDH as “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality of life outcomes and risk.”8 These SDH range from upstream political and social influences to more downstream, non-medical factors in patients’ physical and social environments that influence the ability both to prevent and treat hypertension. As examples, financial resources affect a patient’s ability to purchase medication and healthy food, which in turn impacts hypertension treatment and control9; housing stability and quality impact medication and food storage, ability to exercise, and access to primary care, which together impact all aspects of the hypertension control cascade; and transportation availability affects clinic attendance10 as well as the ability to obtain food and medications. As a result, over the last decade the healthcare sector’s interest in and activities around patients’ social conditions have expanded11. We conducted a scoping review of adult hypertension guidelines to explore if and how guidelines direct clinicians and health systems to ask about and intervene on patients’ social conditions as part of hypertension management.
Methods:
Data Sources and searches
We conducted a systematic scoping review of guidelines of essential hypertension management in adults. A systematic scoping review is the preferred review method “when a body of literature has not yet been comprehensively reviewed, or exhibits a large, complex, or heterogenous nature not amenable to a more precise systematic review,”12 which is the case in this evolving area of SDH research. Our method was similar to prior scoping reviews13, and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).
We defined guidelines as published recommendations for the management of elevated blood pressure, typically conducted in collaboration with professional organizations. Our team worked with an academic medical librarian to develop our search protocol. Using PubMed, we searched for publication type using the terms “hypertension guidelines,” “clinical guidelines,” and “clinical recommendations;” we limited the search to guidelines published in the US and included all dates up to the search date. Since the National Guidelines Clearinghouse closed in 2018, we utilized PubMed to abstract titles. We also included additional hypertension guidelines found by searching references from other articles or that were recommended by experts in the field (see Appendix 1 for search strategy and flowsheet in Figure 1).
Figure 1:
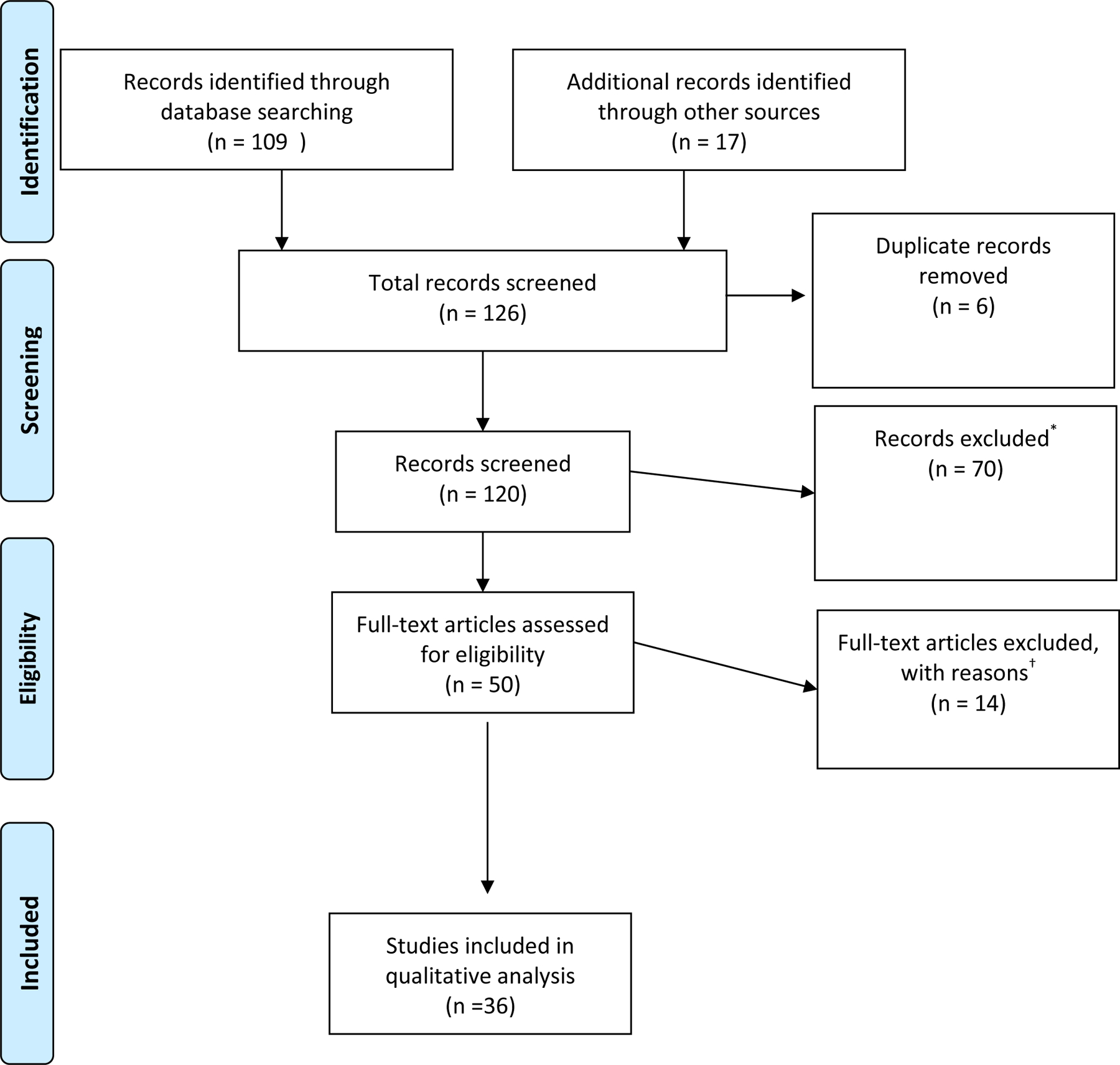
PRISMA inclusion flow diagram
* Reasons for exclusion: Pediatric n=13; Non-essential hypertension (pulmonary hypertension, intracranial hypertension, poral hypertension, radiology findings, renal hypertension, intraabdominal hypertension n=37; Outside of US guidelines n= 6; Pregnancy n= 10) ;4 were not guidelines.
† Unable to locate 3 guidelines; 11 excluded because a more updated guideline existed.
Study Selection
NR reviewed all English language guideline titles to ensure they met inclusion criteria. We included all guidelines on adult hypertension management published between 1977, when the first Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC) was published, and December 2019 when the PubMed search was conducted. We excluded non-US guidelines, those not published in English, and those addressing pulmonary, portal, renovascular, intra-abdominal, intracranial, pediatric, or pregnancy-related hypertension. We only included the most recent version of guidelines (same title and organizational authors) with one exception: both JNC7 and JNC8 were included given the differences in scope between the two guidelines.
Data extraction and assessment
We reviewed in full guidelines meeting inclusion criteria. Using natural language processing (NLP), we searched the text of a randomly selected 15 guidelines using SDH search terms developed for a previously published systematic review13. One author (NR) compared search results with a detailed manual review of these 15 guidelines. We then iteratively added additional SDH search terms to the NLP strategy. After establishing a final list of terms, we applied the NLP search terms to the remaining guidelines to locate text referring to SDH topics (see Appendix 1).
We coded all guidelines using categories for social care established in a National Academies of Sciences, Engineering, and Medicine (NASEM) framework11. This framework defined five activities foundational to improving medical and social care integration at individual and population levels (Table 1). These “social care activities” refer to strategies healthcare delivery systems and practitioners may engage to identify and intervene on social risk factors in an attempt to improve health11. To our knowledge, this is the only published framework to comprehensively classify healthcare activities related to social care. The report’s patient-oriented activities include: 1. Increasing care team Awareness of social conditions that influence health; 2. Making Adjustments to clinical decision-making based on contextual data; and 3. Providing Assistance in the healthcare setting to link patients with available social resources. The Committee also underscored two community-oriented activities: 4. Those that facilitate Alignment of resources between the health and social services sectors; and 5. A complementary set of activities that engages the healthcare sector in Advocacy to improve community conditions. We added a sixth category, Acknowledgement, to capture guideline content in which the influence of socioeconomic status on health was described outside of the context of any of the five defined social care activities. The Acknowledgement category was one of exclusion. If guideline content did not describe a social care activity but still referred to the influence of socioeconomic status on hypertension, the reference was coded as Acknowledgement. All SDH-relevant text in the guidelines was then charted by two members of the research team (NR and LG) using these definitions. We held multiple sessions to address intercoder discrepencies and achieve agreement.
Table 1:
Definitions of healthcare system activities that strengthen social care integration and number of guidelines including healthcare activities related to social care, by category
| Activity | Definition | Transportation related example | N=36 (%) | Selected Example |
|---|---|---|---|---|
| Awareness | Activities that identify the social risk and assets of defined patients and populations | Ask people about their access to transportation | 10 (28) |
|
| Adjustment | Activities that focus on altering clinical care to accommodate identified social barriers | Reduce the need for in-person appointments by using other options such as telehealth appointments or reduce frequency of appointments. | 21 (58) |
|
| Assistance | Activities that reduce social risk by connecting patients with relevant social care resources | Providing transportation vouchers so that patients can travel to health care appointments. Vouchers can be used for ride-sharing services or public transportation. | 6 (17) |
|
| Alignment | Activities undertaken by health care systems to understand existing social care assets in the community, organize them to facilitate synergies, and invest in and deploy them to positively affect health outcomes | Invest in community ride-sharing programs; offer home visits by community health workers to monitor blood pressure | 5 (14) |
|
| Advocacy | Activities in which health care organizations work with partner social care organizations to promote policies that facilitate the creation and redeployment of assets or resources to address health and social needs. | Work to promote policies that fundamentally change the transportation infrastructure within the community or the location of clinics to improve accessibility. | 8 (22) |
|
| Acknowledgement | Any mention the influence of socioeconomic status on health without reference to specific social care integration activities. | Mention that patients may face transportation barriers to reach their clinical appointments | 18 (50) |
|
| Acknowledge Only | Guidelines include only acknowledgement activities | 2 (6) | ||
| None | No mention of any social care activity | 10 (28) |
Data synthesis and analysis
We summed types of recommendations by social care activity category. Additionally, within each social care activity category, we recorded the frequency of each SDH domain referenced (e.g. food, housing, or transportation insecurity; Appendix 2).
Results
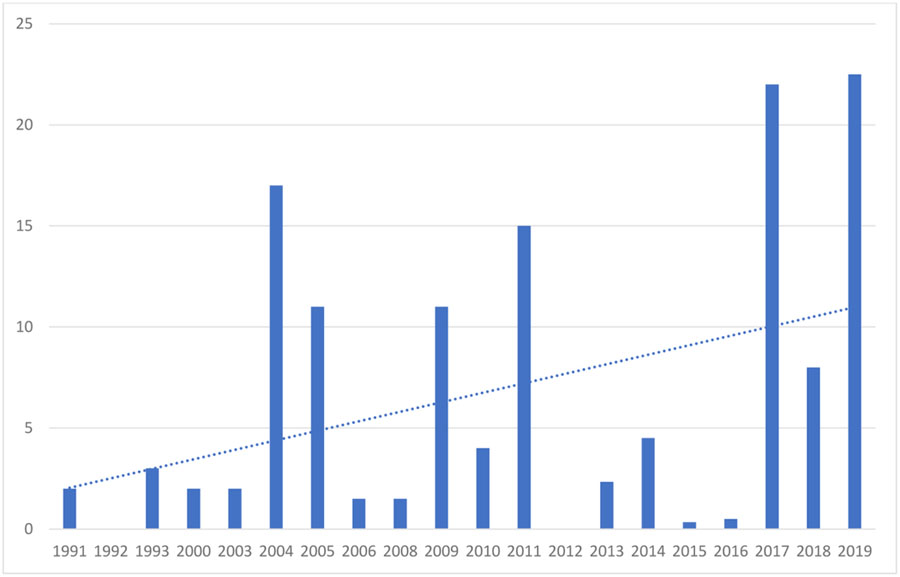
We screened 126 titles. After excluding six duplicates, we reviewed 120 full texts. Thirty-six of these 120 guidelines met inclusion criteria (Figure 1). Of the 36 guidelines reviewed, 10 guidelines (28%) recommended some form of Awareness activities; 21 (58%) included Adjustment recommendations; six (17%) described Assistance strategies; five (14%) described Alignment strategies, and eight (22%) included Advocacy recommendations. Two guidelines Acknowledged the influence of SDH on hypertension management without referencing any of the other social care activities. Of all reviewed guidelines, 28% (n=10) neither acknowledged SDH nor referenced social care activities (See Table 1 for summary and Appendix 2 for breakdown of results). Between 1991 and 2019, the average number of social care activities mentioned per guideline per year increased (Table 2).
Table 2:
Average number of social care activities per guideline per year
|
1. Awareness
Ten guidelines (28%) recommended that clinical teams conduct activities to identify social risks and assests of defined patients and populations. These included recommendations to screen patients for health literacy, food access, ability to pay for medications, and transportation availability. As examples, a 2004 guideline discussed screening for financial security, health literacy, and insurance status14; a 1993 guideline suggested screening for health literacy15; and a 2017 guideline encouraged clinicians to inquire about care affordability9. Only a 2019 publication recommended the use of a standardized social risk screening tool16.
2. Adjustment
Twenty-one guidelines (58%) recommended activities to adjust clinical care based on patients’ social risks. Such adjustments could address several aspects of the hypertension control cascade. The NASEM report underscores that adjustment activities (which accommodate care to patients’ social circumstances) differ from assistance interventions in that they do not involve intervening on the social risk itself, but instead reflect changes to care planning based on select social risks.
Financial security
Of the total 63 care adjustment strategies mentioned across 21 guidelines, over half (57% n=36/63) focused on adjustments to accommodate patients’ financial security. In these cases, guideline authors acknowledged that cost is a barrier to medication adherence (and therefore hypertension control) and suggested ways to reduce cost burdens15,17. Specific examples included prescribing generics9,18–21, altering daily dosages9,19, using combination pills22 or long-acting medication formulations9,21, and increasing the number of pills dispensed to minimize pharmacy visits and co-payments9. A 2017 guideline also recommended providing patients with scored tablets or pill cutters to reduce costs9.
Access to care
Nine guidelines raised ways to accommodate patients’ barriers to accessing care. For instance, guidelines recommended limiting the frequency of medical vists23; increasing telehealth visits16; utilizing electronic health record to tailor health advice to patients based on their social risk16; using remote blood pressure monitoring20,24,25; or offering medication home delivery16. Two guidelines highlighted opportunities to minimize laboratory tests as a strategy to reduce visits17,25. Three other guidelines suggested addressing patients’ transportation barriers and minimizing co-payments by reducing the frequency of office visits9,19,25. A 2013 guideline recommended that emergency room physicians initiate blood pressure medications in asymptomatic patients when patients’ social conditions made it difficult for them to establish primary care26.
Patient education, literacy, and cultural background
Five guidelines recommended adjusting care based on education, literacy level, and cultural background9,17,27,16,28. This included ensuring the presence of translators17, improving providers’ cultural competency9, and providing linguistically-appropriate educational materials28.
Quality reporting
A 2019 guideline highlighted the application of social risk data to quality mesurement. The authors noted that health systems may omit patients from the denominator of some hypertension quality metrics in cases where patients experience economic or access barriers to medication adherence16.
3. Assistance
Six guidelines (17%) described strategies that could improve multiple steps along the hypertension control cascade by directly intervening on social risks. These recommendations involved using clinic or community-based social service providers to facilitate connections with community or government social services16,23, including housing programs, food banks or other nutrition programs29, insurance or medication access programs14,29, or utility assistance programs9.
4. Alignment
Five (14%) guidelines raised topics related to Alignment strategies related to strengthening community-level social resources. For example, a 2005 guideline recommended several community education strategies, such as dissemination of physical activity and nutrition information to marginalized communities, not just patients in clinical settings28. JNC7 and a separate 2017 guideline elevated community organizations as liaisons to bridge cultural and language barriers and establish community-based HTN screening and referral programs9,29. A 2019 guideline highlighted several strategies intended to strengthen community partnerships that could improve healthy food access and enroll community members in federal nutrition assistance programs16.
5. Advocacy
Eight guidelines (22%) described ways that healthcare organizations can promote policies or societal investments that increase the availability of social resources as part of a strategy for reducing hypertension prevalence and morbidity. Seven of these described ways health systems can work with insurers to develop incentives for improved blood pressure control and/or lower costs of care. Several guidelines referenced activities that, if reimburseable, were likely to improve hypertension control, including obesity treatments28 and home blood pressure monitors30; one emphasized the importance of advocating for quality measures that account for how clinical teams assess and address patients’ SDH16.
Five guidelines surfaced the importance of healthy food access as a key community-level resource that could influence hypertension outcomes9,28,29,31,32. These guidelines emphasized the need for the healthcare sector to advocate for policy changes that would increase the availability of healthy food often alongside policies that increase access to physical activity opportunities. A 2017 guideline called on food manufacturers to reduce “the amount of sodium in food processing, as well as in fast food and restaurant food preparation”9.
Four guidelines called for increased research funding to improve evidence on the social and economic aspects of blood pressure control9,14,16,28. This included advocating for researchers and research subjects from diverse backgrounds in studies on hypertension and increased focus on improving the diversity of providers serving patients in low socioeconomic settings9.
6. Acknowledgement
Eighteen guidelines acknowledged the influence of socioeconomic status on health outside the context of any of the five defined social care activities. Of these eighteen guidelines, two included narrative connecting SDH with hypertension management but did not refer to any NASEM social care categories anywhere in the document30,33. The remaining sixteen guidelines acknowledged ways in which SDH influence hypertension management in sections that did not otherwise recommend a specific social care activity. Authors of these sixteen guidelines referred to at least one NASEM action category in another section. Economic constraints (described in 36 of the 84 references to acknowledgement activities) were the most common social domain mentioned in the absence of explicit social care recommendations. In these instances, financial status was generally linked with hypertension risk factors and care1,2 or to specific treatment barriers, such as medication affordability9,16–18,20,23,29,34, lack of health insurance9,17,23,28,33, or limited access to care. Beyond financial risk, multiple guidelines referred to language and education barriers to prevention and treatment9,14,16,19,20,23,29, absence of safe space for physical activity9,29, and lack of adequate healthy food9,21,25,28,29,32.
Discussion
Despite ongoing efforts to improve hypertension outcomes, rates of hypertension control in the US have declined in recent years1,3,5, increasing the demand for innovative responses to decrease related morbidity and mortality. In parallel, strong and compelling evidence has emerged that SDH such as education, financial stability, insurance status, and access to healthcare impact blood pressure control35. The growing recognition of the intersection of SDH and hypertension outcomes has provoked important new questions about how addressing social adversity might improve hypertension awareness, treatment, and control. Yet there are big gaps in our understanding of what the healthcare sector’s role should be in this area.
Seventy-five percent of the hypertenension guidelines included in this review acknowledged associations between SDH and hypertension management and outcomes and references to SDH per guideline per year trended upward between 1991–2019. Two-thirds of these included recommendations about identifying, mitigating, or directly addressing SDH to improve hypertension management. When these types of social care recommendations were included, recommended actions were inconsistent across different guidelines. Adjustments were the most common social care activity our review identified. This may be because adjustments sit in the more traditional wheelhouse of clinical teams. Findings suggest that despite an awareness that social adversity impacts hypertension outcomes, clinicians and health systems are not yet equipped with the information needed to translate that awareness to improving care.
What can we glean from the review findings about hypertension-related social care? First, in cases where guidelines did make social care recommendations, there is an incongruence between screening and intervention recommendations. Of the 27 guidelines that recommended clinical care changes (Adjustment or Assistance) based on patients’ social risk, only 10 recommended some form of social risk screening. Of those, only one suggested using a standardized social risk assessment tool16. This may reflect the fact that more evidence is needed on social risk screening. Prior research not specific to hypertension, however, suggests patients find social risk screening acceptable36 and that clinicians are unlikely to accurately gauge patients’ social risks without those assessments37. If social risk screening is found to be an evidence-based practice that can help target interventions and improve hypertension outcomes, then actionable information on the workforce, training, and tools needed for screening should be referenced in guidelines.
Second, though some adjustment and assistance recommendations surfaced in the hypertension guidelines, there is little consistency or evidence-based information about how clinicians and healthcare systems can intervene on social risk to improve hypertension outcomes. For instance, only nine of the 36 guidelines suggested changes to medication regimens to address hypertension treatment barriers for low-income patients9,14,15,19,20,22,23,25,27. However, there is evidence on this topic that might be relevant to future guideline development. One recent review found that use of brand name antihypertensive medications resulted in higher costs for patients and reduced adherence38. Other studies found that combination pills improved adherence, likely both because of lower costs and reduced regimen complexity39. Medication adherence decreases with each additional antihypertensive medication prescribed40. A multi-pronged approach to hypertension intended to decrease health disparities across Kaiser Permanente involved SDH-related adjustment strategies, including standardized treatment algorithms to encourage combination pills as first line treatment41. Other studies have documented improved blood pressure medication adherence with reduced medication co-payments42. Future guidelines should review the rapidly evolving evidence on how these types of interventions affect the hypertension control cascade and patients’ experience of care.
Other strategies that only occasionally appeared in the guidelines involve using multi-disciplinary care teams to provide care concordant with patients’ language, literacy, and cultural norms or to more consistently bridge patients to community or government programs that provide social services. Yet here, too, there is an emerging evidence base specific to hypertension that might influence future guidelines. Community health worker-delivered counseling and education around cardiovascular risk prevention improved both systolic and diastolic blood pressure43. Peer education and increased workforce diversity both maximized language concordance between patients and providers and reduced hypertension disparities between different patient groups44. A primary care based study found that social screening and assistance-type navigation services modestly improved blood pressure and lipid levels45. Overall, future guidelines might seek to incorporate emerging, multi-disciplinary research on interventions that can mitigate the impacts of socioeconomic risks on hypertension management.
One guideline recommended adjusting quality metrics based on patients’ economic or other access barriers to care16. The presumed intention of this adjustment is to avoid penalizing health systems that care for individuals with limited socioeconomic means. Yet this practice could unintentionally eliminate accountability for hypertension outcomes for low-income patients and demands additional scrutiny.
Our study should be interpreted in light of its limitations. First, given that the National Guideline Clearinghouse closed in 2018, it is difficult to ensure that we identified all relevant hypertension guidelines. We consulted with a medical librarian to design our search strategy, however, and there is no reason that omitted guidelines should systematically differ from those included in the review. Second, our review also was limited to English language guidelines published in the US. Countries with different healthcare infrastructure and payment models may better address patients’ social contexts. Third, we did not include race in our SDH-related search strategy. While many clinicians and research groups use race as a proxy for other SDH, such practices are problematic and an area of active debate46,47. While we understand race to be a social category, it is utilized in many guidelines as a genetic and biological category. It was not possible to address this complex issue within the space constraints of this publication. Future reviews should explore how hypertension guidelines acknowledge and recommend interventions related to race, racism, discrimination, and distrust. Fourth, we selected the NASEM framework for this review because we believe it is the only national effort to date that provides a comprehensive conceptual model defining a wide range of social care activities. Models such as the Outcomes from Addressing Social Determinants of Health in Systems (OASIS) are more limited to specific types of social care. OASIS, for instance, describes pathways through which screening and referrals to social services impact health outcomes but does not include the full range of potentially complementary social care activities48. The NASEM framework encompasses a wider range of activities that might be employed to identify, mitigate the health impacts of, or reduce social risks. Lastly, in some cases, the guidelines did not provide sufficient detail to understand all aspects of a given recommendation. We used an iterative two-reviewer process to discuss recommendations that were challenging to categorize using the NASEM framework, but it is possible that we may have miscategorized some of the references to SDH. We do not believe that this would change the review’s overall findings. Despite these limitations, to our knowledge, this is the first scoping review to use the NASEM framework on social care activities to gauge the translation of emerging SDH science into clinical hypertension guidelines.
In an article highlighting gaps between hypertension guidelines and clinical practice, DeVoe writes, “Where was the evidence-based guideline to answer [the patient’s] questions about whether spending money to buy this medication was more important than buying the healthy foods [the care team] had also recommended?”49 Our review underscores DeVoe’s point: existing guidelines fail to provide clinicians and healthcare systems with comprehensive, actionable, evidence-based guidance on how to integrate our growing knowledge about SDH into patient care. Attending to a patient’s financial situation and food security should not leave clinicians feeling like they are providing suboptimal hypertension care. Improving hypertension outcomes and decreasing disparities will require that the healthcare delivery system more systematically incorporate SDH-related interventions into hypertension management. More attention should be paid to strengthening research in this area, including efforts to assess patients’ social risks and to intervene on identified risks to improve hypertension prevention and treatment. As this evidence grows, future guidelines will need to ensure both the specificity and actionability of new recommendations about social care to facilitate implementation.
Supplementary Material
Appendix 1: Search strategy and search terms
Appendix 2: Summary of included guidelines
Prior presentation:
Components of this data were shared at the virtual 2020 NAPCRG conference as a poster presentation
Funding source:
No funding sources were used for this article. Dr. Razon is a research fellow at the Philip R. Lee Institute for Health Policy Studies at UCSF funded by the Agency for Healthcare Research and Quality (5T32HS022241-07).
Abbreviations:
- SDH
Social Determinants of Health
- NASEM
National Academies of Sciences, Engineering and Medicine
- AHA
American Heart Association
- ACC
American College of Cardiology
- ASH
American Society of Hypertension
- JNC
Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure
- NLP
Natural Language Processing
Footnotes
Conflict of interest: None declared
Availability of data and material: No dataset was used for this manuscript. Included guidelines are available in appendix 2.
References
- 1.Wozniak G, Khan T, Gillespie C, Sifuentes L, Hasan O, Ritchey M, et al. Hypertension Control Cascade: A Framework to Improve Hypertension Awareness, Treatment, and Control. The Journal of Clinical Hypertension. 2016;18(3):232–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.High Blood Pressure | cdc.gov [Internet]. [cited 2020 Jan 10]. Available from: https://www.cdc.gov/bloodpressure/index.htm
- 3.Muntner P, Hardy S, Fine L, Jaeger B, Wozniak G, Levitan E, et al. Trends in Blood Pressure Control Among US Adults With Hypertension, 1999–2000 to 2017–2018. JAMA - Journal of the American Medical Association. 2020;324(12):1190–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoon S, Fryar CD, Carroll M. Hypertension Prevalence and Control Among Adults: United States, 2011–2014 [Internet]. Centers for Disease Control; 2015. Report No.: 220. Available from: https://www.cdc.gov/nchs/data/databriefs/db220.pdf [PubMed]
- 5.Foti K, Wang D, Appel L, Selvin E Hypertension Awareness, Treatment, and Control in US Adults: Trends in the Hypertension Control Cascade by Population Subgroup (National Health and Nutrition Examination Survey, 1999–2016). American Journal of Epidemiology. 2019;188(12):265–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, Guida F, et al. Socioeconomic status and the 25×25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. The Lancet. 2017;389:1229–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mensah GA, Cooper RS, Siega-Riz AM, Cooper LA, Smith JD, Brown CH, et al. Reducing Cardiovascular Disparities through Community-Engaged Implementation Research: A National Heart, Lung, and Blood Institute Workshop Report. Circulation Research. 2018;122(2):213–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Social Determinants of Health [Internet]. Available from: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
- 9.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Journal of the American College of Cardiology. 2018;71(19):e127–248. [DOI] [PubMed] [Google Scholar]
- 10.Chaiyachati KH, Hubbard RA, Yeager A, Mugo B, Shea JA, Rosin R, et al. Rideshare-Based Medical Transportation for Medicaid Patients and Primary Care Show Rates: A Difference-in-Difference Analysis of a Pilot Program. Journal of General Internal Medicine. 2018;33(6):863–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Academies of Sciences, Engineering and M. Integrating Social Care into the Delivery of Health Care. Integrating Social Care into the Delivery of Health Care. 2019. [PubMed] [Google Scholar]
- 12.Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare. 2015;13(3):141–6. [DOI] [PubMed] [Google Scholar]
- 13.Gottlieb LM, Wing H, Adler NE. A Systematic Review of Interventions on Patients’ Social and Economic Needs. Vol. 53, American Journal of Preventive Medicine. Elsevier Inc.; 2017. p. 719–29. [DOI] [PubMed] [Google Scholar]
- 14.Levey AS, Salem W, Anderson S, Greene JH. K/DOQI Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease. American Journal of Kidney Disease. 43AD;5(2004):s16–41. [PubMed] [Google Scholar]
- 15.Zanchetti A, Chalmers J, Arakawa K, Gyarfas I, Hamet P, Hansoon L, et al. 1993 Guidelines for the Management of Mild Hypertension. Hypertension. 1993;22(3):392–403.8349333 [Google Scholar]
- 16.Casey DE, Thomas RJ, Bhalla V, Commodore-Mensah Y, Heidenreich PA, Kolte D, et al. 2019 AHA/ACC clinical performance and quality measures for adults with high blood pressure: A report of the american college of cardiology/american heart association task force on performance measures. Circulation: Cardiovascular Quality and Outcomes. 2019. November 1;12(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levey AS, Salem W, Anderson S, Greene JH. K/DOQI Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease. American Journal of Kidney Disease. 43;5(2004):s16–41. [PubMed] [Google Scholar]
- 18.Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA, et al. Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher Versus Lower Blood Pressure Targets: A Clinical Practice Guideline From the American College of Physicians and the American Academy of Family Physicians. Annals of internal medicine. 2017. March 21;166(6):430–7. [DOI] [PubMed] [Google Scholar]
- 19.Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, et al. Resistant hypertension: Detection, evaluation, and management a scientific statement from the American Heart Association. Hypertension. 2018. November 1;72(5):E53–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: A report of the american college of cardiology foundation task force on clinical expert consensus documents. Circulation. 2011;123(21):2434–506. [DOI] [PubMed] [Google Scholar]
- 21.Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. Journal of clinical hypertension (Greenwich, Conn). 2014. January;16(1):14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gradman AH, Basile JN, Carter BL, Bakris GL. Combination therapy in hypertension. Journal of the American Society of Hypertension. 2010. January;4(1):42–50. [DOI] [PubMed] [Google Scholar]
- 23.Merz CNB, Alberts MJ, Balady GJ, Ballantyne CM, Berra K, Black HR, et al. ACCF/AHA/ACP 2009 competence and training statement: A curriculum on prevention of cardiovascular disease: A report of the american college of cardiology foundation/american heart association/american college of physicians task force on competence and tra. Vol. 120, Circulation. 2009. [DOI] [PubMed] [Google Scholar]
- 24.Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, et al. Measurement of blood pressure in humans: A scientific statement from the american heart association. Hypertension. 2019. May 1;73(5):E35–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Education Programs Working Group Report on the Management of Patients with Hypertension and High Blood Cholesterol. Annals of Internal Medicine. 1991;114(3):224–37. [DOI] [PubMed] [Google Scholar]
- 26.Burton JH, Godwin SA, Hahn SA, Lo B, Mace SE, Melnick ER, et al. Clinical Policy : Critical Issues in the Evaluation and Management of Adult Patients in the Emergency Department With Asymptomatic Elevated Blood Pressure. 2013;(1). [DOI] [PubMed] [Google Scholar]
- 27.Go AS, Bauman MA, Coleman King SM, Fonarow GC, Lawrence W, Williams KA, et al. An Effective Approach to High Blood Pressure Control A Science Advisory From the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2013;63:878–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith SC, Clark LT, Cooper RS, Daniels SR, Kumanyika SK, Ofili E, et al. Discovering the Full Spectrum of Cardiovascular Disease Minority Health Summit 2003 Report of the Obesity, Metabolic Syndrome, and Hypertension Writing Group. Circulation. 2005;111(10):134–9. [DOI] [PubMed] [Google Scholar]
- 29.Chobanian AV. The Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. U.S Department of Health and Human Services, National Heart, Lung, and Blood Institute; 2004. [PubMed] [Google Scholar]
- 30.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. AHA / ASH / PCNA Scientific Statement Call to Action on Use and Reimbursement for Home Blood Pressure Monitoring : Executive Summary A Joint Scientific Statement From the American Heart Association, American Society of Hypertension, and Preventive Cardi. 2008; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elijovich F, Weinberger MH, Anderson CAM, Appel LJ, Bursztyn M, Cook NR, et al. Salt sensitivity of blood pressure : A scientific statement from the American Heart Association. Hypertension. 2016. September 1;68(3):e7–46. [DOI] [PubMed] [Google Scholar]
- 32.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary Approaches to Prevent and Treat Hypertension A Scientific Statement From the American Heart Association. 2006;296–308. [DOI] [PubMed] [Google Scholar]
- 33.Egan BM, Bland VJ, Brown AL, Ferdinand KC, Hernandez GT, Jamerson KA, et al. Hypertension in african americans aged 60 to 79 years: Statement from the international society of hypertension in blacks. Journal of Clinical Hypertension. 2015. April 1;17(4):252–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dennison-himmelfarb C, Handler J, Lackland DT. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;1097(5):507–20. [DOI] [PubMed] [Google Scholar]
- 35.Carey R, Paul M, Bosworth H, Whelton P. Prevention and Control of Hypertension: JACC Health Promotion Series. Journal of American College of Cardiology. 2018;72(11):1278–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.De Marchis EH, Hessler D, Fichtenberg C, Adler N, Byhoff E, Cohen AJ, et al. Part I: A Quantitative Study of Social Risk Screening Acceptability in Patients and Caregivers. 2019; [DOI] [PMC free article] [PubMed]
- 37.Tong ST, Liaw WR, Kashiri PL, Pecsok J, Rozman J, Bazemore AW, et al. Clinician Experiences with Screening for Social Needs in Primary Care. Journal of American Board of Family Medicine. 2018;31(3):351–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choudhry NK, Denberg TD, Qaseem A. Improving adherence to therapy and clinical outcomes while containing costs: Opportunities from the greater use of generic medications: Best practice advice from the clinical guidelines committee of the American college of physicians. Annals of Internal Medicine. 2016. January 5;164(1):41–9. [DOI] [PubMed] [Google Scholar]
- 39.Gerbino PP, Shoheiber O. Adherence patterns among patients treated with fixed-dose combination versus separate antihypertensive agents. American Journal of Health-System Pharmacy. 2007. June 15;64(12):1279–83. [DOI] [PubMed] [Google Scholar]
- 40.Fung V, Huang J, Brand R, Newhouse JP, Hsu J. Hypertension treatment in a medicare population: adherence and systolic blood pressure control. Clinical therapeutics. 2007. May;29(5):972–84. [DOI] [PubMed] [Google Scholar]
- 41.Shaw KM, Handler J, Wall HK, Kanter MH. Improving blood pressure control in a large multiethnic California population through changes in health care delivery, 2004–2012. Preventing Chronic Disease. 2014;11(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chernew ME, Shah MR, Wegh A, Rosenberg SN, Juster IA, Rosen AB, et al. Impact of decreasing copayments on medication adherence within a disease management environment. Health affairs (Project Hope). 2008. January;27(1):103–12. [DOI] [PubMed] [Google Scholar]
- 43.Allen JK, Dennison Himmelfarb CR, Szanton SL, Bone L, Hill MN, Levine DM. COACH trial: A randomized controlled trial of nurse practitioner/ community health worker cardiovascular disease risk reduction in urban community health centers: Rationale and design. Contemp Clin Trials. 2011;32(3):403–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sim JJ, Handler J, Jacobsen SJ, Kanter MH. Systemic implementation strategies to improve hypertension: The Kaiser permanente southern california experience. Vol. 30, Canadian Journal of Cardiology. Pulsus Group Inc.; 2014. p. 544–52. [DOI] [PubMed] [Google Scholar]
- 45.Berkowitz SA, Catherine Hulberg A, Standish S, Reznor G, Atlas SJ. Addressing Unmet Basic Resource Needs as Part of Chronic Cardiometabolic Disease Management. JAMA Internal Medicine. 2017;177(2):244–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vyas DA., Eisenstein LG., Jones DS. Hidden in Plain Sight - Reconsidering the Use of Race Correction in Clinical Algorithms. New England Journal of Medicine. 2020;383(9):874–82. [DOI] [PubMed] [Google Scholar]
- 47.Peek M Racism and health: A call to action for health services research. Health Services Research. 2021;1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gurewich D, Garg A, Kressin N Addressing Social Determinants of Health Within Healthcare Delivery Systems: a Framework to Ground and Inform Health Outcomes. Journal of General Internal Medicine. 35(5):1571–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.DeVoe J Bridging the Gap Between Where the Quality Metric Ends and Real Life Begins—A Trusting Relationship. JAMA Internal Medicine. 2020;180(2):177–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: Search strategy and search terms
Appendix 2: Summary of included guidelines


