Abstract
Sexual minority men (SMM) disproportionately experience psychosocial risk factors and comorbid health concerns (e.g., HIV infection) that increase their vulnerability to COVID-19 infection and distress. The current study applied a socioecological approach to the Health Belief model to understand associations among perceived risk, optimistic bias (a perceived lower risk relative to similar others), united action (perceived community capacity for collective action) and COVID-19 behavioral prevention strategies among COVID-19-negative adult cisgender SMM. Participants (n = 859), recruited via a geo-location-based dating app in May 2020, completed an online survey. Results indicated significant interactions between perceived risk and optimistic bias on social distancing (B = −.03, p < .05), and between perceived risk and united action on number of preventive precautions (B = −.01, p < .01) and number of casual sex partners (B= −.20, p < .05). At low and average levels of perceived risk, socioecological constructs were positively associated with behavioral prevention strategies. At average levels of perceived risk and above, united action was negatively associated with number of casual sex partners, demonstrating evidence of the interaction between perception of interpersonal and community factors and perceptions of one’s own risk. These findings may help to inform how to mobilize increased engagement in COVID-19 behavioral prevention strategies among cisgender SMM.
Keywords: Preventive Health Behaviors, Collective Efficacy, Cognitive Heuristic, Men who have sex with men, Coronavirus
Introduction
The novel disease caused by the SARS-CoV-2 virus, coronavirus disease (COVID-19), has made a staggering and devastating global impact. Since COVID-19 was first identified in December 2019 in Wuhan, China, more than 2.5 million people have died worldwide (Johns Hopkins University, 2021). In the United States, more than 28 million people have been diagnosed with COVID-19 and at least 511,839 people have died following infection as of March 2, 2021 (Centers for Disease Control and Prevention [CDC], 2021a).
While the impact of the COVID-19 pandemic is vast, threatening not only an individual’s health but also their personal and social well-being, some populations have been disproportionately impacted (Bali et al., 2020; Clark et al., 2020; Lee & Miller, 2020). A series of commentaries published in June 2020 (including Lee & Miller, 2020; Hafi & Uvais, 2020; Salerno et al., 2020) and notes from the field (Marziali et al., 2020) emphasized the vulnerability of sexual minority populations during the COVID-19 crisis, citing increased social isolation (Lee & Miller, 2020; Salerno et al., 2020; Marziali et al., 2020), lack of access to supportive communities (potentially compounded by taking residence in abusive environments; Hafi & Uvais, 2020; Salerno et al., 2020), and obstacles to receiving physical and mental health care (Salerno et al., 2020). There is a need for focused attention on sexual minority males (SMM) within the body of research encompassing the COVID-19 pandemic and factors that contribute to the adoption of behavioral prevention strategies.
A growing body of literature has demonstrated evidence for these concerns. In a qualitative study examining the experiences of COVID-19 among fifteen SMM (i.e., gay, bisexual, or other men who have sex with men) living with HIV, participants voiced a number of concerns that arose due to the COVID-19 pandemic, including concerns about susceptibility, decreased engagement in other health behaviors (e.g., sleep and physical activity), and mental health consequences, including isolation and worry (Rhodes et al., 2020). These findings are supported by data from a cross-sectional study using a global sample of SMM, which found that COVID-19 negatively impacted economic status, mental health, and HIV prevention and treatment (Santos et al., 2020). Going further, survey data has demonstrated diminished sleep quality among SMM, attributed – in part – to worries about the pandemic and associated with emotional distress (Millar et al., 2020). Despite the host of complex factors increasing their risk of infection and complications of COVID-19 (Phillips et al., 2020), SMM remain largely understudied within the context of this pandemic.
Behavioral prevention strategies during COVID-19
Even though vaccine distribution has begun and gives hope for ending the COVID-19 pandemic, the availability of vaccines is limited. In addition, uncertainty remains around whether vaccines prevent transmission, when herd immunity will be achieved, and if the vaccines protect against new variants of the virus (CDC, 2021b). Thus, reducing viral transmission among communities continues to rely heavily on individual-level compliance with behavioral prevention strategies.
Social distancing – a behavioral intervention that decreases viral transmission by increasing physical distance between persons and limiting person-to-person contact among social networks (Glass et al., 2020; Koo et al., 2020) – was identified as a primary strategy to reduce the spread of SARS-CoV-2 during the first few months of the pandemic (Bourassa et al., 2020). Social distancing requires coordination of a number of behaviors, including utilizing lower-contact methods for social interactions (e.g., phone calls and video conferencing) and limiting use of higher-contact transportation (e.g., buses and trains). The Centers for Disease Control and Prevention (2020) also advise individuals to engage in a number of preventive precautions, including washing hands frequently with soap and water for at least 20 seconds and wearing a face mask (Chu et al., 2020; Konda et al., 2020; Rothe et al., 2020).
In response to the COVID-19 pandemic, a number of public health agencies, including the American Sexual Health Association (2020), also issued guidance around safer sex behaviors that reflected the broader non-pharmaceutical public health approaches to COVID-19 prevention. One of these risk reduction strategies is limiting the number of casual sex partners. There is mixed evidence surrounding the number of sex partners among SMM since the pandemic began; one study reported fewer sex partners (Sanchez et al., 2020), another reported an increase in the number of sex partners (Stephenson et al., 2020a), and Starks et al. (2020) found that, while the odds of condomless anal sex decreased, the number of casual sex partners overall was stable.
While these recommendations around behavioral prevention strategies are certainly applicable to the general population, there is a need to focus on SMM. This is not only because of the increased vulnerability of SMM during the pandemic, but also because there is some evidence that suggests predictors of COVID-19 health behaviors are different between sexual minority individuals and heterosexual individuals (Solomon et al., 2021). Given the history of the HIV epidemic, which similarly involved the implementation of a range of public health strategies that relied on individual and community engagement, the SMM community may have a potential reservoir of coping strategies (e.g., Quinn et al., 2020) and resilience. Being able to identify the unique predictors may help with reducing the risk of COVID-19 in SMM communities.
Factors Associated with Preventive Health Behaviors
Individuals’ engagement in behavioral prevention strategies to mitigate the widespread risks of COVID-19 can be conceptualized through an integration of the Health Belief Model (Rosenstock, 1974) and the socioecological framework derived from Bronfenbrenner’s Ecological Systems Theory (Bronfenbrenner, 1977; 1986; 1992). The Health Belief model identifies several individual-level factors, including perceived risk and self-efficacy, as key determinants of engagement in preventive health behaviors. The socioecological framework situates individuals’ health and health behaviors within multiple overlapping and interacting levels of influence, including interpersonal- and community-level factors. The current study responds to the call to include ecological measures to understand health behavior (Sallis et al., 2015) by substituting self-efficacy with a parallel community-level factor – collective efficacy – and by including optimistic bias, a measure of a cognitive heuristic with a comparative component, in an attempt to examine how factors spanning several levels of influence interact with perceived risk to shape health behaviors and prevent COVID-19.
Perceived risk, or the belief about the likelihood or probability of vulnerability and potential harm (Brewer et al., 2007), is a well-established, individual-level factor that predicts engagement in preventive precautions (Rosenstock, 1974; Ferrer & Klein, 2015). Perceived risk has been associated with preventive precautions against infectious diseases, including influenza, hepatitis, pneumonia, and Lyme disease (Brewer et al., 2007). A growing body of literature supports the hypothesis that perceived risk is associated with preventive health behaviors during the COVID-19 pandemic (e.g., Abdelrahman, 2020; Taghrir et al., 2020; Dryhurst et al., 2020; de Bruin & Bennett, 2020). A U.S. national survey conducted in March 2020 found an association between perceived risk and COVID-19 behavioral prevention strategies including: avoidance of public spaces, crowds, and individuals at high-risk; canceling or postponing travel plans; and, hand washing (Stephenson et al., 2020b). Among SMM, perceived risk for COVID-19 was found to be high between April and May 2020 (Stephenson et al., 2020a), yet comparatively lower than perceived risk for HIV during this same time. Drawing from HIV literature, which has established an association between perceived risk and preventive behaviors (i.e., number of sexual partners; Goedel et al., 2016), we sought to extend findings by examining perceived risk among SMM and its associations with engagement in COVID-19 behavioral prevention strategies.
Processing information about risk is multi-faceted and complex, and this may be exacerbated during the COVID-19 pandemic, when information rapidly changes. In situations where information needs to be processed quickly, individuals may rely on the use of cognitive heuristics, or mental shortcuts. One heuristic is optimistic bias, defined as the tendency to interpret information positively and in favor of one’s self, resulting in an overestimation of favorable outcomes and an underestimation of negative outcomes (Sharot, 2011; Weinstein, 1980). Having an unrealistic level of optimism around estimation of risk has been associated with increased engagement in riskier health behaviors, including risky sexual behaviors (Chapin, 2001) and decreased intention to engage in handwashing to prevent influenza (Kim & Niederdeppe, 2013). At least two studies (Wise et al., 2020; Park et al., 2020) have found that having an optimistic bias was associated with decreased engagement in social distancing, handwashing, and discussions surrounding risk and prevention, as well as decreased intention to seek information. Neither study examined these associations among SMM.
Individuals who have an optimistic bias when interpreting health messages tend to perceive their own risk of developing positive outcomes to be greater than that of demographically similar others across physical and mental health conditions, including HIV (Sohn et al., 2012), cancer (Fontaine & Smith, 1995), and schizophrenia (Prentice et al., 2005). This conceptualization of optimistic bias is comparative in its nature and may have implications about how an individual perceives risk of others in their social group, especially in uncertain situations. Thus, we propose that examining an individual’s optimistic bias surrounding risk of COVID-19 may be a way of approximating individual perceptions of the interpersonal level of the socioecological framework.
In addressing the highly contagious COVID-19, behavioral prevention strategy engagement is not only relevant to and initiated by an individual, but also to and by others within the individual’s community. Importantly, COVID-19 infection can occur from asymptomatic or pre-symptomatic carriers who may unknowingly transmit the virus to others (Wiersinga et al., 2020); therefore, individuals who engage in behaviors to prevent COVID-19 may do so not only to reduce their own risk, but also that of others in their community. As such, the extent to which an individual perceives their community’s ability to engage in COVID-19 prevention as a group to synchronously respond to a problem – or their collective efficacy (Bandura, 2000; Cain et al., 2013) – may be a particularly important factor.
Collective efficacy includes a number of domains, including united action, which is defined as a general “good feeling” that a community can work together on issues of importance (Carroll et al., 2005). Given the broad impact of the pandemic as well as the need for coordinated and sustained adoption of health behaviors throughout communities, united action may be salient when considering an individuals’ uptake of preventive health behaviors. To our knowledge, only one study to date (Dryhurst et al., 2020) has examined collective efficacy broadly in shaping perceived risk for COVID-19, and results indicated a negative association. Whether and how united action, specifically, may influence engagement in COVID-19 behavioral prevention strategies among SMM remains unknown. Consistent with the socioecological framework, united action may contextualize associations between perceived risk and behavioral prevention strategies.
Current Study
The current study is exploratory and utilizes an integration of the Health Belief model and socioecological framework to examine the associations between perceptions that exist on individual-, interpersonal-, and community-levels on COVID-19 behavioral prevention strategies (i.e., social distancing, COVID-19 precautions, and number of casual sex partners) in a sample of COVID-19 negative adult cisgender SMM. More specifically, we examine if the association between perceived risk and COVID-19 preventive behavioral strategies changes at different levels of optimistic bias and united action. We hypothesized that perceived risk would interact with optimistic bias and united action, such that individuals with a lower perceived risk would still report greater engagement in COVID-19 behavioral prevention strategies, particularly when perceptions of interpersonal and community factors indicate concern about the risk of COVID-19 to others in one’s social group and community (indicated by having higher optimistic bias and lower united action, respectively).
Methods
Procedure
A nationwide survey was administered between May 6 and May 15, 2020, to participants recruited through advertisements posted on a geo-location based social networking and dating application. Advertisements directed potential participants to a study screener that included a questionnaire assessing eligibility. Eligibility criteria for the survey included being 18-years or older, a U.S. resident, and English-proficient. If participants were eligible and interested in participating in the study, they were directed to an online consent form. After consenting, enrolled participants were directed to a Qualtrics survey with several questionnaires, including those described below. Upon completing the survey, participants were given the option to be entered into a random drawing to receive a $50 Amazon gift card. Full recruitment and procedures are described in Starks et al. (2020). All procedures were approved by the institutional review board of Hunter College, City University of New York.
A total of 1,001 completed the nationwide survey. Due to low respondent rates of cisgender females (n = 20), transgender, gender queer, and gender expansive folks (n = 38), these participants were excluded from the current study. An additional 84 participants were excluded from present analyses because they have tested positive for COVID-19, and therefore did not complete the survey measures related to perceived risk of COVID-19.
Participants
Participants included 859 racially diverse cisgender SMM. A majority of participants identified their race as Black (41.7%) or White (37.7%). Fewer SMM identified as either Latinx (12.2%) or multiracial or a different race or ethnicity (8.4%). A little more than half the sample (54.7%) earned at least $30,000 per year, and 81.6% identified their relationship status as single. Each geographic region of the U.S. was represented in the sample, with 41.8% from the South, 21.5% from the Northeast, 19.0% from the West, and 17.1% from the Midwest. Table 1 contains a summary of participant demographics.
Table 1.
Summary of Demographics (n = 859)
| n | % | |
|---|---|---|
| Race and Ethnicity | ||
| White | 324 | 37.7 |
| Black | 358 | 41.7 |
| Latino | 105 | 12.2 |
| Multiracial or other | 72 | 8.4 |
| Income | ||
| < $30,000/year | 338 | 39.3 |
| > $30,000/year | 470 | 54.7 |
| Region | ||
| South | 361 | 41.8 |
| Northeast | 183 | 21.5 |
| West | 162 | 19.0 |
| Midwest | 146 | 17.1 |
| Relationship Status | ||
| Single | 701 | 81.6 |
| Partnered | 158 | 18.4 |
|
| ||
| M | SD | |
|
| ||
| Age | 38.56 | 3.12 |
Notes. There are missing data for income and region
Measures
Demographics
Participants reported on several demographic characteristics including age, race and ethnicity, zip code of residence, income, and HIV status.
Perceived Risk
Perceived risk of COVID-19 was assessed using an adapted version of the Perceived Risk of HIV Scale created for this study (Napper et al., 2012). The 10-item scale was modified to assess perceived risk of COVID-19 by subsisting “Corona Virus or COVID-19” in place of “HIV.” The modified measure included affective items (e.g. “What is your gut feeling about how likely you are to get infected with the Corona Virus or COVID-19?” with response options ranging between 1, extremely unlikely, and 5, extremely likely), cognitive items (e.g. “There is a chance, no matter how small, I could get Corona Virus or COVID-19” with response options ranging between 1, strongly disagree, to 5, strongly agree), and salience of risk (e.g. “Picturing myself getting Corona Virus or COVID-19 is something I find: (1) very hard to do to (4) very easy to do”). A total sum of all 10 items was used for analyses, with higher scores reflecting greater perceived risk of COVID-19. The measure of Perceived Risk of COVID-19 has good internal reliability in the current study (α = 0.83).
Optimistic Bias
Optimistic bias was measured with a single measure: “How does your risk of developing coronavirus compare to others who have a similar background as you (i.e., age, gender, race/ethnicity, and health status)?” Participants rated their options on a scale of −2 (much higher than other people) to 2 (much lower than other people), with scores above 0 (the same as for other people) indicating an optimistic bias. This measure was adapted from a study by Bränström and colleagues (2006) which assessed optimistic bias in the context of readiness to change preventive behaviors to reduce skin cancer.
United Action
United action was measured with a 5-item subscale of the Collective Efficacy Scale (Carroll et al., 2005). Items were adapted to address specific community efforts and collective action; for example: “Our community can cooperate in the face of difficulties to reduce the spread of coronavirus.” Participants were asked to indicate the degree to which they agreed on a 5-point scale from 1 (strongly disagree) to 5 (strongly agree). Higher scores on this measure were representative of greater perceived united action. The measure of united action in the current study has good internal reliability (α = 0.90).
Social Distancing
Social distancing was measured by asking participants a single item: “To what extent are you are social distancing?” Response options included: “None of the time. I am doing everything the same”; “Some of the time. I am limiting social interaction to family members who live in my community”; “Some of the time. I have reduced the amount of times I am in public spaces, social gatherings, or at work”; “Most of the time. I only leave home to buy food and other essentials”; and, “All of the time. I am staying at home nearly all the time.”
COVID-19 Precautions
Participants were asked to indicate the COVID-19 precautions they were engaging in when they left the house in the past 30-days from a 7-item checklist. Options on the checklist included “I try to remain at least 6-feet away from others,” “I wear a face mask,” “I wear latex or rubber gloves,” “I wash my outer garments upon returning home,” and “I wash my hands immediately upon returning home.” Participants were also given the option to select “Other” and fill in any other precaution they used when leaving the house. Finally, participants could select “I do not take any specific precautions.” Responses were aggregated to create a sum score for the number of precaution behaviors endorsed, with “I do not take any specific precautions” coded as zero.
Number of Casual Sex Partners
Participants were asked to indicate their relationship status and identify their main partner. Respondents then reported on the number of sex partners, regardless of gender, with the item “In the past 30 days, how many casual partners did you have?”
Analytic Plan
SPSS v 23 was first utilized to examine the bivariate correlations between key variables of interests (e.g., perceived risk, optimistic bias, and united action) using Pearson’s product- moment correlation (r). Mplus v8 was then utilized to examine models predicting social distancing (an ordinal outcome), preventive precautions (a Poisson regression), and number of casual sex partners in the past 30 days, respectively (a negative binomial regression). Covariates in all models included race and ethnicity, U.S. region, and income. Additionally, having a main partner was entered as a in the model predicting number of casual sex partners in the past 30-days.
Consistent with the socioecological framework, a series of moderation models examined the interactions between individual-, interpersonal-, and community-level factors. Interaction effects were evaluated using a reverse hierarchical approach. Each model first tested the three-way interaction (i.e., perceived risk X optimistic bias X united action) while controlling for lower-order two-way interactions (i.e., perceived risk X optimistic bias, perceived risk X united action, optimistic bias X united action); direct effects of perceived risk, optimistic bias, and united action as well as demographic covariates. Where non-significant, three-way interactions were then dropped from the model and the lower-order two-way interactions were examined. Nonsignificant two-way interactions were dropped from the model sequentially in reverse order of magnitude. In addition to parameter p-values, the impact of removal on model fit was evaluated using procedures for robust (Satorra & Bentler, 2001) and strictly positive (Asparouhov & Muthén, 2013; Satorra & Bentler, 2010) log-likelihood testing. In instances where the significance of parameter p values and model likelihood changes conflicted, final decisions were informed by changes in Aikiki Information Criteria (AIC) and sample-size adjusted Bayesian Information Criteria (BIC). The significance of final models was also evaluated by comparing the log-likelihood to that of a null model in which all regression parameters were constrained to be zero.
Missing data ranged from 0% to 27% depending on the construct of interest. Full information maximum likelihood (FIML) estimation was utilized to impute cases with missing data. FIML is a superior method of handling data under missing at random assumptions (Enders & Bandalos, 2001), and is at least as robust as multiple imputation strategies in the presence of nonrandom missingness (Newman, 2003).
Results
Bivariate Associations
A summary of bivariate associations is presented in Table 2. Among variables of interest, united action was positively associated with social distancing and COVID-19 preventive precautions in the past 30-days. In contrast, united action and having an optimistic bias were negatively associated with number of casual sex partners in the past 30-days. Having an optimistic bias was not associated with social distancing or COVID-19 preventive precautions at the bivariate level. Similarly, perceived risk of COVID-19 was positively associated with COVID-19 preventive precautions but was not associated with social distancing nor casual sex partners at the bivariate level.
Table 2.
Summary of Bivariate Correlations
| M | SD | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|---|
| 1. Social Distancing | 3.67 | 1.05 | - | ||||
| 2. Preventive Behaviors | 3.12 | 1.20 | .24** | - | |||
| 3. Sex with Casual Partners | 1.43 | 3.09 | −.21** | -.15** | - | ||
| 4. United Action | 3.74 | 0.86 | .14** | .13** | −.09* | - | |
| 5. Optimistic Bias | 0.24 | 1.06 | .06 | −.02 | −.18** | .05 | - |
| 6. Perceived Risk | 33.45 | 7.83 | .07 | .21** | .02 | −.08 | −.33** |
Notes.
p < .05;
p <.01
Social Distancing
Stepwise removal of the 3-way interaction term (χ2(1) = .77, p = .380); the interaction between perceived risk and united effort (χ2(1) = 2.60, p = .107); as well as the interaction between united effort and optimistic bias (χ2(1) = 1.51, p = .219) resulted in non-significant changes in model log-likelihood and p-values for all parameters removed were non-significant. In contrast, constraining the interaction term between optimistic bias and perceived risk in a final step resulted in a significant decrease in model log-likelihood (χ2(1) = 5.31, p =.021) and the p-value for this parameter was significant. An omnibus test compared the log-likelihood value for the final model (containing the interaction between optimistic bias and perceived risk) to that of a baseline model wherein all the structural paths were constrained to be zero was significant (χ2(12) = 36.81, p < .001). Table 3 contains final model coefficients. Figure 1 displays the interaction between optimistic bias and perceived risk in the final model.
Table 3.
Summary of models predicting social distancing, number of preventive behaviors and number of casual sex partners in the past 30-days.
| Social Distancing | Number of Preventive Precautions | Number of Casual Partners | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | (95%CI) | β | B | (95%CI) | β | B | (95%CI) | β | |
| Age | .01* | (0.002, 0.02) | .09 | .001 | (−0.002, 0.003) | .05 | .01 | (−0.01, 0.02) | .11 |
| Race and Ethnicity (ref = white) | |||||||||
| Black | .30 | (−0.04, 0.65) | .08 | .10** | (0.04, 0.17) | .35 | −.07 | (−0.45, 0.31) | −.06 |
| Latinx | .49* | (0.07, 0.91) | .09 | .10* | (0.01, 0.18) | .22 | −.15 | (−0.64, 0.34) | −.08 |
| Other | .74* | (0.24, 1.23) | .11 | .10 | (−0.09, 0.20) | .18 | −.43 | (−1.09, 0.23) | −.20 |
| Region (ref = south) | |||||||||
| North East | .18 | (−0.18, 0.54) | .04 | .08* | (0.10, 0.14) | .21 | −.62** | (−1.02, −0.22) | −.42 |
| Midwest | −.19 | (−0.61, 0.22) | −.04 | −.09* | (−0.18, −0.01) | −.23 | −.31 | (−0.77, 0.15) | −.20 |
| West | −.12 | (−0.52, 0.28) | −.02 | −.01 | (−0.08, 0.07) | −.02 | −.39* | (−0.78, −0.01) | −.26 |
| Income (ref = <$30,000/year) | −.11 | (−0.41, 0.20) | −.03 | .06 | (−0.002, 0.12) | .20 | −.06 | (−0.36, 0.24) | −.05 |
| HIV Status (ref = negative) | .35* | (0.001, 0.70) | .25 | ||||||
| Main Partner | - | - | - | - | - | - | −.18 | (−0.55, 0.19) | −.12 |
| United Action | .31** | (0.09, 0.51) | .14 | .06** | (0.02, 0.09) | .33 | −.23* | (−0.40, −0.06) | −.34 |
| Optimistic Bias | .21* | (0.03, 0.40) | .12 | .02 | (−0.01, 0.09) | .16 | −.42** | (−0.57, −0.27) | −.74 |
| Perceived Risk | .03* | (0.01, 0.06) | .12 | .01** | (0.008, 0.017) | .66 | −.03* | (−0.05, −0.01) | −.35 |
| Perceived Risk x Optimistic Bias | −.03* | (−0.06, −0.01) | −.15 | - | - | - | - | - | - |
| Perceived Risk x United Action | - | - | - | −.01** | (−0.01, −0.002) | −.40 | −.02* | (−0.04, −0.01) | −.30 |
Notes.
p < .05;
p < .01
Figure 1.
The association between optimistic bias and odds of being in a higher social distancing category at various levels of perceived risk
At average levels of perceived risk, having an optimistic bias was positively associated with social distancing. Similarly, perceived risk was also positively associated with social distancing among respondents with an average level of optimistic bias. The effect of having an optimistic bias diminished as risk perceptions increased. At low levels of perceived risk (1 SD below the mean) the effect of having an optimistic bias was significant and positive (B = .44, 95% CI: .13 to .75, p = .005). In contrast, at high levels of perceived risk (1 SD above the mean), the effect of having an optimistic bias was non-significant (B = −.02, 95% CI: −.27 to.23, p = .899). United action also contributed significantly to the prediction of social distancing, with higher scores associated with higher levels of social distancing. With respect to covariates, SMM who identified their racial/ethnic group as “Other” and Latinx reported engaging in a greater extent of social distancing, compared to SMM who identified as White. Region and income were not associated with social distancing in the past 30 days.
COVID-19 Precautions
Stepwise removal of the 3-way interaction term (χ2(1) = .25, p = .617) as well as the interaction between perceived risk and optimistic bias (χ2(1) = .02, p = .887) resulted in non-significant changes in model log-likelihood. Both parameters had nonsignificant p-values. While the removal of the nonsignificant bivariate interaction between united action and optimistic bias resulted in a statistically significant decrease in model log-likelihood per the strictly positive Satorra-Bentler χ2 test (χ2(1) = 8.18, p = .004) the change in AIC (difference = .533) and sample-size adjusted BIC (difference = 1.05) was small. These along with the non-significant p-value for the interaction term (p = .069) provided support for exclusion. In contrast, constraining the interaction term between united action and perceived risk in a final step resulted in a decrease in model log-likelihood that was at the threshold for statistical significance (χ2(1) = 3.77, p =.052); meanwhile, the changes in AIC (difference = 3.73) and sample-size adjusted BIC (difference = 2.15) were modestly larger and in combination with the statistically significant p-value (p = .003) pointed to the utility of retaining the interaction term. An omnibus test of the final model containing the interaction between united action and perceived risk was significant (χ2(12) = 82.64, p < .001). Table 3 contains final model coefficients. Figure 2 displays the interaction between united action and perceived risk in the final model.
Figure 2.
The association between united action and number of preventive behaviors at various levels of perceived risk
At average levels of perceived risk, united action was positively associated with the number of COVID-19 preventive precautions. Similarly, at average levels of united action, perceived risk was positively associated with the number of COVID-19 preventive precautions used. The effect of united action on number of COVID-19 preventive precautions diminished as perceived risk increased. At low levels of perceived risk, the effect of united action on COVID-19 precautions was significant and positive (B = .11, 95% CI: .05 to .18, p = .000). In contrast, at high levels of perceived risk, the effect of united action on COVID-19 preventive precautions was nonsignificant (B =.001, 95% CI: −.04 to .04, p = .98). Optimistic bias was not significantly associated with the number of COVID-19 preventive precautions.
With respect to covariates, SMM who identified their race and ethnicity as Black or Latinx engaged in a greater number of COVID-19 preventive precautions than their White peers. SMM from the Northeast region reported engaging in a higher number of COVID-19 preventive precautions, while those living in the Midwest reported lower numbers of COVID-19 preventive precautions, compared to SMM who live in the South.
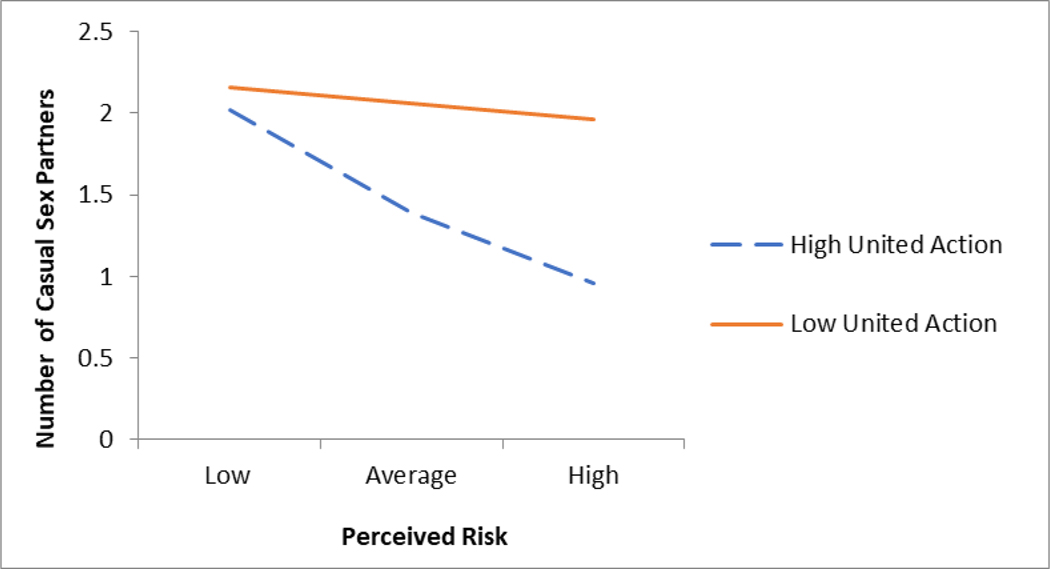
Sex with Casual Partners
Stepwise removal of the 3-way interaction term (χ2(1) = 1.49, p = .222); the interaction between united action and optimistic bias (χ2(1) = .39, p = .532); and the interaction between perceived risk and optimistic bias (χ2(1) = .44, p = .507); resulted in non-significant changes in model log-likelihood. All parameters removed had nonsignificant p-values. In contrast, constraining the interaction term between united action and perceived risk in a final step resulted in a significant decrease in model log-likelihood (χ2(1) = 16.25, p < .001). An omnibus test of the final model (containing the interaction between united action and perceived risk) was significant (χ2(14) = 63.85, p < .001). Table 3 contains final model coefficients. Figure 3 displays the interaction between optimistic bias an perceived risk in the final model.
Figure 3.
The association between united action and number of casual sex partners at various levels of perceived risk
At average levels of perceived risk, united action was negatively associated with the number of casual partners in the past 30-days. Similarly, at average levels of united action, perceived risk was negatively associated with the number of casual partners. The effect of united action on number of casual partners became more negative as perceived risk increased. Additional tests of simple effects found that at low levels of perceived risk the effect of united action on the number of casual sexual partners is nonsignificant (B = −.07, 95% CI: −.25 to .12, p = .470). In contrast, at high levels of perceived risk, the effect of united action on sex with casual partners was negative and significant (B = −.40, 95% CI: −.64 to −.16, p = .001).
With respect for covariates, SMM from the Northeast and West had fewer casual sex partners compared to SMM living in the South, and HIV-positive SMM had more casual sex partners compared to HIV-negative SMM. Relationship status (i.e., having a main partner), age, income, and race/ethnicity were not associated with number of casual sex partners in the past 30-days.
Discussion
To address the call for the inclusion of ecological measures to understand health behavior (Sallis et al., 2015), this study applied the socioecological framework to the Health Belief model to predict COVID-19 behavioral prevention strategies among cisgender SMM recruited from a geo-location based social networking and dating application. Results indicate that, for measures of COVID-19 behavioral prevention (i.e., extent of social distancing and number of COVID-19 precautions taken), individual risk perceptions and perceptions of social and community factors interact – and to some extent offset – each other. At higher levels of perceived risk, the associations between having an optimistic bias and united action with COVID-19 prevention outcomes were attenuated. In contrast, at average levels of perceived risk and below, associations between these higher-order interpersonal and community factors and COVID-19 behavioral prevention strategies strengthened. With respect to number of casual sex partners, individual-level risk perception amplified the protective association between united action and number of casual sex partners, such that united action was negatively associated with number of casual partners at average and high levels of perceived risk. These findings may help to inform how public health efforts can be mobilized by focusing on interpersonal and community factors to increase engagement in COVID-19 behavioral prevention among SMM, a vulnerable population amid the pandemic.
Robust research demonstrates the role of perceived risk on engagement in preventive health behaviors broadly (Brewer et al., 2007; Ferrer & Klein, 2015), and a growing body of literature focuses on this association specifically in the context of COVID-19 (de Bruin & Bennett, 2020; Dryhurst et al., 2020; Wise et al., 2020). In line with the Health Belief Model, we found that higher perceived risk was associated with greater engagement in COVID-19 behavioral prevention strategies (i.e., handwashing and social distancing) and fewer casual sex partners in the past 30-days in this sample of cisgender SMM. The directionality of our findings is consistent with evidence from a longitudinal study by Wise and colleagues (2020), which found that engagement in hand washing and social distancing increased as perceived risk increased over the course of five days early in the pandemic. However, other studies have found a negative association between perceived risk and COVID-19 preventive behaviors (e.g., Taghrir et al., 2020) suggesting individual perceptions of personal risk alone are not necessarily sufficient to understand engagement in preventive behaviors. Our results suggest that one plausible explanation for the mixed findings in previous research may arise from the failure to account for perceptions of one’s social group or community.
We found that perceived risk interacts with perceptions of risk and resilience at higher-order socioecological levels for SMM. In models predicting social distancing, the nature of the interaction suggested that factors at the individual- and interpersonal-levels offset one another, such that the association the perception of the higher-order influence (having an optimistic bias) with social distancing diminished as individual-level risk perceptions increased. We look to social comparison theory (Chapman, 2019; Buunk & Gibbons, 2007) to suggest an explanation for this interaction: when people perceive their individual risk to be high, experiencing their own risk to be greater than that of similar others may increase motivation to engage in preventive behaviors. It is possible that this may be particularly relevant in the case of social distancing behaviors among individuals using a social networking and dating application, where an individual may be making these comparisons with the person(s) with whom they are networking.
A similar pattern was found for number of preventive precautions, where the association between united action (a higher order influence) and number of COVID-19 preventive precautions was non-significant at high levels of perceived risk. It is possible that a higher level of perceived risk exacerbates participants’ need to engage in a greater number of preventive precautions, for example, handwashing and wearing a mask, to help reduce their chances of being diagnosed with COVID-19, regardless of what efforts are being made on part of their community.
As individual-level risk perception decreased, associations between community-level factors (e.g., optimistic bias and united action) and COVID-19 behavioral prevention strategies strengthened. Optimistic bias is a cognitive heuristic, that is, a tendency to foresee favorable outcomes for oneself. One way to conceptualize an optimistic bias is by use of comparisons between oneself and demographically similar others (i.e., age, gender, race/ethnicity, and health status; Weinstein, 1982); thus, foreseeing a favorable outcome for oneself is connected to a less favorable outcome predicted for similar others. This interpersonal perception of other’s risk appeared to compensate for lower levels of perceived risk in the prediction of social distancing. Associations between having an optimistic bias and social distancing were significant at low and average levels of individual perceived risk, but not at higher levels. While this interaction may be relevant to the general population, it is especially important among SMM, who face unique concerns and stressors about COVID-19 infection and transmission, including increased anxiety about transmission (Solomon et al., 2021).
Similarly, united action was significantly associated with the number of COVID-19 preventive precautions at average levels of perceived risk and below. Again, this points to the potential for perceptions of community-level resilience to lead to sustained individual prevention behavior, even as individual perceptions of risk decline. One potential explanation is that, even when perception of individual risk is modest or low, greater desire to align behavior with community norms becomes salient in shaping engagement in activities that would reduce the chance of transmission (e.g., wearing a mask, handwashing). Taken together, these findings confirm our prediction that individuals who engage in COVID-19 preventive behaviors may be doing so not only to reduce their own risk, but also that of others in their social group and community.
The interaction between perceived risk and united action was also significantly associated with number of casual sex partners – an interpersonal activity that involves engagement with others. Reducing the number of casual sex partners can be considered an ancillary COVID-19 prevention behavior. The number of casual sex partners was higher when individual risk perception was lower and when perception of the community’s ability to take action was also low. In contrast, united action amplified the association between risk perception and number of casual sex partners. At high levels of perceived risk, united action was negatively associated with number of casual sex partners. It is plausible that the relevance of sexual behavior to the specific social networking space made perceptions of community norms particularly salient for those SMM who had higher levels of concern about COVID-19 risk.
A number of demographic associations are noteworthy. SMM living in the Northeast – where rates of COVID-19 were the highest (Zhang & Schwartz, 2020) at the time of data collection (May 2020) – endorsed a greater number of COVID-19 preventive precautions and a smaller number of casual sex partners compared to SMM in the Midwest and in the South. Additionally, SMM who identified as Black and Latinx reported greater extent of social distancing and greater number of preventive precautions, and research has suggested that these are two racial/ethnic demographic groups that have disproportionately been impacted by COVID-19 (Tai et al., 2020). Therefore, SMM who may be at a greater risk due to their geographic location and race/ethnicity are engaging in more social distancing and COVID-19 preventive precautions. Finally, SMM who were HIV-positive reported having a greater number of casual sex partners compared to SMM who were HIV-negative, which adds to the call for research that examines the burden of COVID-19 among HIV-negative populations (Shiau et al., 2020). Further research focusing on SMM should focus on these demographic groups, as they potentially represent populations who are at a greater risk for COVID-19.
Limitations
The generalizability of findings is limited by eligibility criteria, which focused on cisgender, adult SMM who had not been diagnosed with COVID-19. These men were recruited in online social networking spaces and may not be representative of the overall SMM population. These cross-sectional data were collected during a nine-day period in May 2020. The COVID-19 pandemic is rapidly evolving, and longitudinal data are needed to determine the durability of findings across time. It is possible that patterns of behaviors have changed with the introduction of vaccinations in December 2020 and/or as a result of “quarantine fatigue.” The survey also relied on self-report data and participants’ perceptions, and therefore participants may have reported in ways that they perceived would be socially desirable (Van de Mortel, 2008). Finally, we acknowledge the limitations of measures, used to assess behavioral prevention strategies. More specifically, social distancing and optimistic bias are assessed using single items in the current study, which precluded direct assessment of reliability. Additionally, the measure of preventative precautions included items salient at the early stage of the pandemic when the survey was designed. The effectiveness of some strategies has since been debated (e.g., using rubber gloves). While likely not a perfect representation of actual behavioral risk, our measure of preventive precautions provides some indication of the scope or breadth of prevention behaviors people may have been using at the time.
Despite these limitations, the current study includes noted strengths. We recruited SMM who were using a social networking and dating application, a subsample of SMM who may be even more vulnerable to COVID-19, due to some evidence that suggests associations between social networking application use and greater sexual risk behaviors (Choi, Wong, & Fong, 2016). Thus, while focusing on this subsample may limit generalizability, it also allows us to identify predictors in a subsample of SMM that may benefit the most from targeted health messaging strategies. Furthermore, our theoretically grounded research question was informed by robust literature supporting each of these perceptions individually, as well as a growing body of literature suggesting these perceptions interact. By applying a socio-ecological approach to the Health Belief Model, we were able to capture the broader impact of interpersonal and community factors that may inform and shape health behavior within the context of COVID-19 for SMM.
Implications and Future Directions
Research examining trends in engagement in preventive behavior have almost exclusively focused on health messages targeting the individual, despite the fact that engagement in these health behaviors also affects and is affected by others in the community. To improve our understanding of how to best mitigate the spread of the virus, especially among vulnerable communities, our findings suggest that it is important to understand not only whether an individual perceives their own risk as being high, but also how an individual perceives their risk as compared to similar others and their community’s ability to handle the situation. Our findings point to the possibility that interpersonal and community factors may be a source of resilience for SMM, which may have broader implications for the prevention of COVID-19 as well as other health conditions.
We identify several possibilities for future directions. First, research should explore whether these interactions hold over time (i.e., longitudinally) and generalize to other COVID-19 prevention behaviors (e.g., vaccination) and to other health behaviors (e.g., PrEP adherence and drug use) and conditions (e.g., sexually transmitted infections) relevant to this population. This research would help to determine the extent to which COVID-19 related prevention behavior is reflective of a more global approach to health behaviors; this understanding may be especially important as guidelines and prevention strategies change. Seeing that the socioecological framework and Health Belief Model have previously been supported in the literature, we believe the interactions would also hold. Second, as previously suggested, research should examine whether perceptions of phenomena that exist at more distal ecological levels are, in fact, accurate reflections of what is existing at those levels. For example, to what extent do individual perceptions of united action align with objective, community-level assessments of united action? And, do individual perceptions of risk relative to similar others reflect social descriptive and injunctive norms? The associations between objective and subjective experience may open avenues for research questions that inform both public health messaging as well as health behavior interventions. Finally, research may benefit from observing the bi-directionality of the associations between perceptions and behaviors (Weinstein & Nicolich, 1993).
These findings may also help to inform health messaging strategies. Public health messages that target the individual’s risk alone versus those that integrating the symbiotic relationship between individuals and communities result in different patterns of intent of engaging in behavioral prevention strategies. Messages that emphasize the interplay of individuals, their social groups, and communities in community-wide prevention efforts for vulnerable populations, such as SMM, may be needed, especially among populations who perceive their own risk to be low.
Conclusions
We employed a cross-sectional survey design to investigate the interactions of perceptions of individual-, interpersonal-, and community-levels on engagement in COVID-19 behavioral prevention strategies. Consistent with the socioecological framework, perception of one’s self and social ecology affect health behavior in ways that are interactive. Our findings suggest that the more proximal belief of perceived risk contextualized beliefs about one’s social and community ecologies. The findings support applying a socio-ecological approach to understanding the engagement in health behaviors during the COVID-19 pandemic in a sample of cisgender SMM, a vulnerable population during this pandemic.
Public Significance Statement.
The health behaviors we engage in may reflect our understanding of our personal health risks. In certain situations, it is also possible that people may choose to engage in health behaviors to prevent others in their community from certain health conditions. The COVID-19 pandemic has created a unique circumstance to understand the latter, since early efforts to mitigate the spread of the virus relied on individuals complying with behavioral prevention strategies (e.g., social distancing, washing hands frequently with soap and water for at least 20 seconds). The question of how personal beliefs are associated with engaging in behavioral prevention strategies is particularly important to understand in a certain population, sexual minority men, due to evidence that this population may be at an increased risk of COVID-19 and its related distress. We found that three COVID-19 preventive health behaviors (i.e., social distancing, number of COVID-19 prevention precautions, and number of casual sex partners) were shaped by an interaction of three kinds of beliefs: (a) personal beliefs about one’s own risk, (b) beliefs about similar others in one’s interpersonal group and, (c) beliefs about the ability of one’s community to take action. These findings may help to inform how public health efforts can be mobilized to increase engagement in COVID-19 behavioral prevention strategies among sexual minority men.
Acknowledgement:
Analyses of these data were supported in part by a grant from the National Institute on Drug Abuse (R01 DA045613, PI: Starks). The authors thank the participants for their time and engagement. The authors also thank the study team, including S. Scott Jones, Ruben Jimenez, Trinae Adebayo, Brett Millar, Cynthia Cabral, Christine Cowles, Michael Suarez, Kory Kyre, Kendell Doyle, Stephen Bosco, and Daniel Sauermilch.
Footnotes
Author Note: We have no conflicts of interest to disclose.
References
- Abdelrahman M. (2020). Personality traits, risk perception, and protective behaviors of Arab residents of Qatar during the COVID-19 pandemic. International Journal of Mental Health and Addiction. 10.1007/s11469-020-00352-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Sexual Health Association. (2020). Sex and COVID-19. https://www.ashasexualhealth.org/sex-in-the-time-of-covid-19/ [Google Scholar]
- Asparouhov T. & Muthén B. (2013, April 17). Computing the strictly positive Satorra-Bentler chi-square test in Mplus. Mplus Web Notes: No. 12. https://www.statmodel.com/examples/webnotes/SB5.pdf [Google Scholar]
- Bali S, Dhatt R, Lal A, Jama A, Van Daalen K, & Sridhar D. (2020). Off the back burner: Diverse and gender-inclusive decision-making for COVID-19 response and recovery. BMJ Global Health, 5(5), e002595. 10.1136/bmjgh-2020-002595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. (2000). Exercise of human agency through collective efficacy. Current Directions in Psychological Science, 9(3), 75–78. 10.1111/1467-8721.00064 [DOI] [Google Scholar]
- Bourassa KJ, Sbarra DA, Caspi A, & Moffitt TE (2020). Social distancing as a health behavior: County-level movement in the United States during the COVID-19 pandemic is associated with conventional health behaviors. Annals of Behavioral Medicine, 54(8), 548–556. 10.1093/abm/kaaa049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bränström R, Kristjansson S, & Ullen H. (2006). Risk perception, optimistic bias, and readiness to change sun related behaviour. The European Journal of Public Health, 16(5), 492–497. 10.1093/eurpub/cki193 [DOI] [PubMed] [Google Scholar]
- Brewer NT, Chapman GB, Gibbons FX, McCaul KD, & Weinstein ND (2007). Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology, 26(2), 136–145. 10.1037/0278-6133.26.2.136 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513–531. 10.1037/0003-066X.32.7.513 [DOI] [Google Scholar]
- Bronfenbrenner U. (1986). Ecology of the family as a context for human development: Research perspectives. Developmental Psychology, 22(6), 723–742. [Google Scholar]
- Bronfenbrenner U. (1992). Ecological systems theory. In: Vasta R (Ed). Six theories of child development: Revised Formulations and Current Issues. (pp. 187–249). Jessica Kingsley Publishers. [Google Scholar]
- Buunk AP & Gibbons FX (2007). Social comparison: The end of theory and the emergence of a field. Organizational Behavior and Human Decision Processes, 102(1), 3–21. 10.1016/j.obhdp.2006.09.007 [DOI] [Google Scholar]
- Cain D, Pitpitan EV, Eaton L, Carey KB, Carey MP, Mehlomakulu V, Harel O, Simbayi LC, Mwaba K, & Kalichman SC (2013). Collective efficacy and HIV prevention in South African townships. Journal of Community Health, 38(5), 885–893. 10.1007/s10900-013-9694-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll JM, Rosson MB, & Zhou J. (2005). Collective efficacy as a measure of community. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. (pp. 1–10). 10.1145/1054972.1054974 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Coronavirus Disease 2019 (COVID-19) Protect Yourself. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html [Google Scholar]
- Centers for Disease Control and Prevention. (2021a). Coronavirus Disease 2019 (COVID-19) United States COVID-19 Cases and Deaths by State. https://covid.cdc.gov/covid-data-tracker/#cases_casesinlast7days [Google Scholar]
- Centers for Disease Control and Prevention (2021b). Key things to know about COVID-19 vaccines. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/keythingstoknow.html [PubMed] [Google Scholar]
- Chapin J. (2001). It won’t happen to me: The role of optimistic bias in African American teens’ risky sexual practices. Howard Journal of Communication, 12(1), 49–59. 10.1080/10646170151143370 [DOI] [Google Scholar]
- Chapman GB (2019). A decision-science approach to health-behavior change. Current Directions in Psychological Science, 28(5), 469–474. 10.1177/0963721419854102 [DOI] [Google Scholar]
- Choi EPH, Wong JYH, & Fong DYT (2017). The use of social networking applications for smartphone and associated sexual risks in lesbian, gay, bisexual, and transgender populations: A systematic review. AIDS Care, 29(2), 145–155. 10.1080/09540121.2016.1211606 [DOI] [PubMed] [Google Scholar]
- Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schunemann HJ, El-harakeh A, Bognanni A, Lotfi T, Loeb M, & Hajizadeh A. (2020). Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. The Lancet, 395(10242), 1973–1987. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark E, Fredricks K, Woc-Colburn L, Bottazzi ME, & Weatherhead J. (2020). Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States. PLOS Neglected Tropical Diseases, 14(7), e0008484. 10.1371/journal.pntd.0008484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronavirus Resource Center. (2021). Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. https://coronavirus.jhu.edu/ [Google Scholar]
- de Bruin WB & Bennett D. (2020). Relationships between initial COVID-19 risk perceptions and protective health behaviors: A national survey. American Journal of Preventive Medicine, 59(2), 157–167. 10.1016/j.amepre.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryhurst S, Schneider CR, Kerr J, Freeman ALJ, Recchia G, Marthe van der Bles AM, Spiegelhalter D, & van der Linden S. (2020). Risk perceptions of COVID-19 around the world. Journal of Risk Research, 1–13. 10.1080/13669877.2020.1758193 [DOI] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8, 430–457. [PubMed] [Google Scholar]
- Ferrer RA & Klein WM (2015). Risk perceptions and health behavior. Current Opinion in Psychology, 5, 85–89. 10.1016/j.copsyc.2015.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine KR, & Smith S. (1995). Optimistic bias in cancer risk perception: A cross-national study. Psychological Reports, 77(1):143–146. 10.2466/pr0.1995.77.1.143 [DOI] [PubMed] [Google Scholar]
- Glass RJ, Glass LM, Beyeler WE, Min HJ (2006). Targeted social distancing designs for pandemic influenza. Emerging Infectious Diseases, 12(11), 1671–1681. 10.3201/eid1211.060255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goedel WC, Halkitis PN, & Duncan DT (2016). Behavior- and partner-based HIV risk perception and sexual risk behaviors in men who have sex with men (MSM) who use geographical-networking smartphone applications in New York City. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 93(2):400–496. 10.1007/s11524-016-0043-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafi B. & Uvais NA (2020). Difficulties faced by sexual and gender minorities during COVID-19 crisis. Psychiatry and Clinical Neurosciences, 74(8), 444. 10.1111/pcn.13080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HK & Niederdeppe J. (2013). Exploring optimistic bias and the integrative model of behavioral prediction in the context of a campus influenza outbreak. Journal of Health Communication, 18(2), 206–222. 10.1080/10810730.2012.688247 [DOI] [PubMed] [Google Scholar]
- Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, & Guha S. (2020). Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 14(5), 6339–6347. 10.1021/acsnano.0c03252 [DOI] [PubMed] [Google Scholar]
- Koo JR, Cook AR, Park M, Sun Y, Sun H, Lim JT, Tam C, & Dickens BL (2020). Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study. The Lancet Infectious Diseases, 20(6), 678–688. 10.1016/S1473-3099(20)30162-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H. & Miller VJ (2020). Disproportionate impact of COVID-19 on minority groups: A social justice concern. Journal of Gerontological Social Work, 1–5. 10.1080/01634372.2020.1777241 [DOI] [PubMed] [Google Scholar]
- Marziali ME, Card KG, McLinden T, Wang L, Trigg L, & Hogg RS (2020). Physical distancing in COVID-19 may exacerbate experiences of social isolation among people living with HIV. AIDS and Behavior, 24(8), 2250–2252. 10.1007/s10461-020-02872-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millar BM, Adebayo T, Dellucci TV, Behar E, Starks TJ (2020). Keeps me awake at night: The potential of the COVID-19 pandemic to affect sleep quality among sexual minority men in the USA. Psychology of Sexual Orientation and Gender Diversity. Advance online publication. 10.1037/sgd0000441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napper LE, Fisher DG, & Reynolds GL (2012). Development of the perceived risk of HIV scale. AIDS and Behavior, 16(4), 1075–1083. 10.1007/s10461-011-0003-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman DA (2003). Longitudinal modeling with randomly and systematically missing data: A simulation of ad hoc, maximum likelihood, and multiple imputation techniques. Organizational Research Methods, 6, 328–362. [Google Scholar]
- Park T, Ju I, Ohs JE, & Hinsley A. (2020). Optimistic bias and preventive behavioral engagement in the context of COVID-19. Research in Social and Administrative Psychology, 17(1), 1859–1866. 10.1098/rsos.200742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips IG, Felt D, Ruprecht MM, Wang X, Xu J, Pérez-Bill E, Bagnarol RM, Roth J, Curry CW, & Beach LB (2020). Addressing the disproportionate impacts of the COVID-19 pandemic on sexual and gender minority populations in the United States: Actions toward equity. LGBT Health, 7(6), 279–82. 10.1089/lgbt.2020.0187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prentice KJ, Gold JM, & Carpenter WT Jr. (2005). Optimistic bias in the perception of personal risk: Patterns in schizophrenia. The American Journal of Psychiatry, 162(3), 507–512. 10.1176/appi.ajp.162.3.507 [DOI] [PubMed] [Google Scholar]
- Quinn KG, Walsh JL, John SA, & Nyitray AG (2021). “I feel almost as though I’ve lived this before”: Insights from sexual and gender minority men on coping with COVID-19. AIDS and Behavior, 25, 1–8, 10.1007/s10461-020-03036-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Mann-Jackson L, Alonzo J, Garcia M, Tanner AT, Smart BD, Horridge DN, Van Dam CN, & Wilkin AM (2020). A rapid qualitative assessment of the impact of COVID-19 pandemic on a racially/ethnically diverse sample of gay, bisexual, and other men who have sex with men living with HIV in the US South. AIDS and Behavior, 1–10. 10.1007/s10461-020-03014-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock I. (1974). The health belief model and preventive behavior. Health Education Monographs, 2(4), 354–386. 10.1177/109019817400200405 [DOI] [PubMed] [Google Scholar]
- Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, Guggemos W, Drosten C, Vollmar P, Zwirglmair K, Zange S, Wölfel R, & Hoelscher M. (2020). Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. The New England Journal of Medicine, 382(10), 970–971. 10.1056/NEJMc2001468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno JP, Williams ND, & Gattamorta KA (2020). LGBTQ populations: Psychologically vulnerable communities in the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S239–S242. 10.1037/tra0000837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Owen N, & Fisher E. (2015). Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath KV (Eds.) Health Behavior: Theory, Research, and Practice. (pp. 43–64). Jossey-Bass/Wiley. [Google Scholar]
- Sanchez TH, Zlotorzynska M, Rai M, Baral SD (2020). Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS and Behavior, 24, 2024–2032. 10.1007/s10461-020-02894-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos GM, Ackerman B, Rao A, Wallach S, Ayala G, Lamontage E, Garner A, Holloway I, Arreola S, Silenzio V, Strömdahl S, Yu L, Strong C, Adamson T, Yakusik A, Doan T, Huang P, Cerasuolo D, Bishop A, Noori T, Pharris A, Aung M, Dara M, Chung SY, Hanley M, Baral S, Beyrer C, & Howell S. (2020). Economic, mental health, HIV prevention and HIV treatment impacts of COVID-19 and the COVID-19 response on a global sample of cisgender gay men and other men who have sex with men. AIDS and Behavior. 10.21203/rs.3.rs-33958/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A, & Bentler PM (2001). A scaled difference chi-square test statistic for moment structure analysis. Psychometrika, 66(4), 507–514. 10.1007/BF02296192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A. & Bentler PM (2010). Ensuring positiveness of the scaled difference chi-square test statistic. Psychometrika, 75, 243–248. 10.1007/s11336-009-9135-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharot T. (2011). The optimism bias. Current Biology, 21(23), R941–R945. 10.1016/j.cub.2011.10.030 [DOI] [PubMed] [Google Scholar]
- Shiau S, Krause KD, Valera P, Swaminathan S, & Halkitis PN (2020). The burden of COVID-19 in people living with HIV: A syndemic perspective. AIDS and Behavior. 10.1007/s10461-020-02871-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn A, Chun S, & Reid EA (2012). Adolescent optimistic bias toward HIV/AIDS in Seoul, South Korea. Asia Pacific Journal of Public Health, 24(5), 816–825. 10.1177/1010539511404395 [DOI] [PubMed] [Google Scholar]
- Solomon DT, Morey KE, Williams CJ, Grist CL, & Malesky AL (2021). COVID-19 health behaviors in a sexual minority sample: The impact of internalized stigma. Psychology of Sexual Orientation and Gender Diversity. Advance online publication. 10.1037/sgd0000466 [DOI] [Google Scholar]
- Starks TJ, Jones SS, Sauermilch D, Benedict M, Adebayo T, Cain D, & Simpson KN (2020). Evaluating the impact of COVID-19: A cohort comparison study of drug use and risky sexual behavior among sexual minority men in the U.S.A. Drug and Alcohol Dependence, 216, 108260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Chavanduka TMD, Rosso MT, Sullivan SP, Pitter RA, Hunter AS, & Rogers E. (2020a). Sex in the time of COVID-19: Results of an online survey of gay, bisexual and other men who have sex with men’s experience of sex and HIV prevention during the US COVID-19 epidemic. AIDS and Behavior. 10.1007/s10461-020-03024-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Chavanduka TM, Rosso MT, Sullivan SP, Pitter RA, Hunter AS, & Rogers E. (2020b). Contrasting the perceived severity of COVID-19 and HIV infection in an online survey of gay, bisexual, and other men who have sex with men during the U.S. COVID-19 epidemic. American Journal of Men’s Health, 14(5), 155798830957545. 10.1177/1557988320957545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taghrir MH, Borazjani R, & Shiraly R. COVID-19 and Iranian medical students: A survey on their related-knowledge, preventive behaviors and risk perception. Archives of Iranian Medicine, 23(4), 249–259. [DOI] [PubMed] [Google Scholar]
- Tai DBG, Shah A, Doubeni CA, Sia IG, & Wieland ML (2020). The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clinical Infectious Diseases, ciaa815. 10.1093/cid/ciaa815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Mortel TF (2008). Faking it: social desirability response bias in self-report research. Australian Journal of Advanced Nursing, 25(4), 40–48. [Google Scholar]
- Weinstein ND (1980). Unrealistic optimism about future life events. Journal of Personality and Social Psychology, 39(5), 806–820. 10.1037/0022-3514.39.5.806 [DOI] [Google Scholar]
- Weinstein ND (1982). Unrealistic optimism about susceptibility to health problems. Journal of Behavioral Medicine, 5(4), 441–460. 10.1007/BF00845372 [DOI] [PubMed] [Google Scholar]
- Weinstein ND & Nicolich M. (1993). Correct and incorrect interpretations of correlations between perceived risk and risk behaviors. Health Psychology, (3), 235–245. 10.1037/0278-6133.12.3.235 [DOI] [PubMed] [Google Scholar]
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, & Prescott HC (2020). Pathophysiology, transmission, diagnosis, and treatment of Coronavirus Disease 2019 (COVID-19): A review. JAMA, 324(8), 782–793. [DOI] [PubMed] [Google Scholar]
- Wise T, Zbozinek T, Michelini G, Hagan CC, & Mobbs D. (2020). Changes in risk perception and protective behavior during the first week of the COVID-19 pandemic in the United States. Royal Society Open Science, 7(9), 200742. 10.1098/rsos.200742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang CH & Schwartz GG (2020). Spatial disparities in coronavirus incidence and mortality in the United States: An ecological analysis as of May 2020. The Journal of Rural Health, 36(3), 433–445. 10.1111/jrh.12476 [DOI] [PMC free article] [PubMed] [Google Scholar]