Respiratory syncytial virus (RSV) results in seasonal winter epidemics and accounts for 60–80% of bronchiolitis hospitalisations, the most common cause of admission to hospital for infants in high-income countries. Globally, rates of RSV infection and bronchiolitis have been remarkably low since early 2020.1 The implementation of stringent public health non-pharmacological interventions targeting COVID-19 has been credited for this success. Nevertheless, concerns have been raised about the potential for more severe RSV epidemics in the future due to a so-called immunity debt, a term proposed to describe the paucity of protective immunity arising from extended periods of low exposure to a given pathogen, leaving a greater proportion of the population susceptible to the disease.2 This immunity debt is a particular concern for RSV, for which temporary immunity is obtained through exposure to the virus and maternal antibodies wane quickly; without seasonal exposure, immunity decreases and susceptibility to future, and potentially more severe, infection increases.
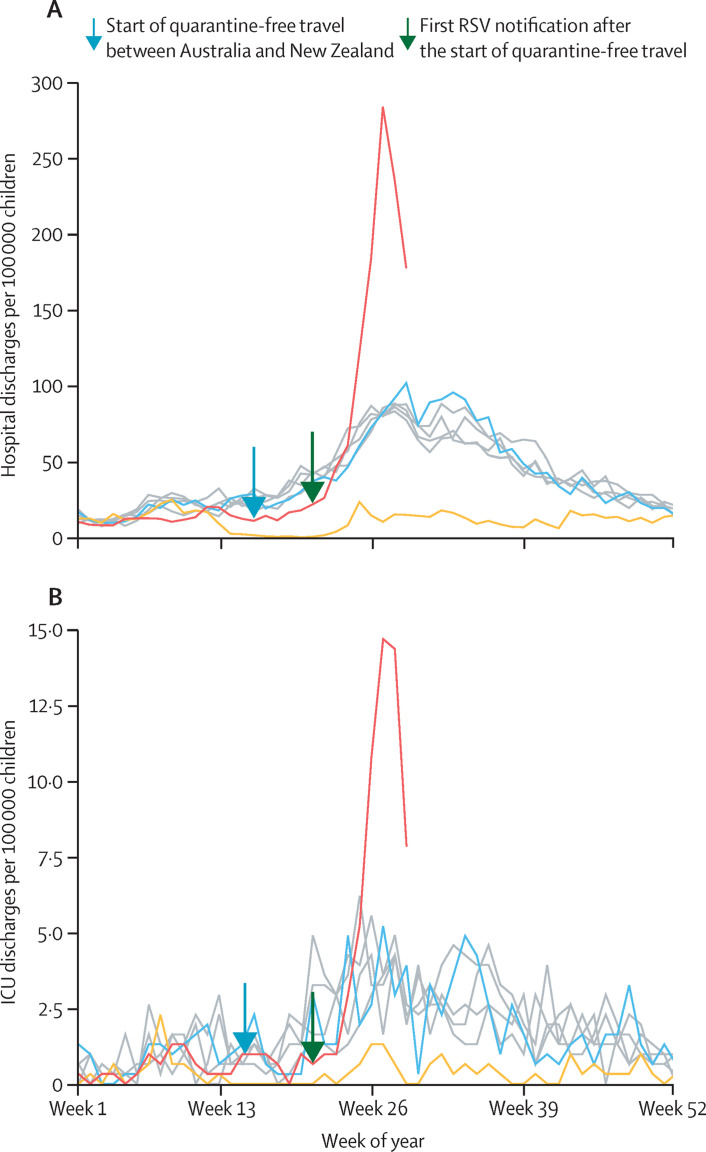
New Zealand had very low levels of RSV infection in 2020,3 with no seasonal epidemic of hospital admissions for bronchiolitis (figure ). A partial relaxation of New Zealand's strict border closure policy in April, 2021, to allow quarantine-free travel between Australia and New Zealand, was followed by a rapid increase in RSV cases in New Zealand and hence an increase in admissions due to bronchiolitis. At the peak (week 28, 2021), RSV surveillance numbers were more than five times the 2015–19 peak average.6, 7 Provisional national data for children aged 0–4 years show that in 2021 there were 866 hospital discharges for bronchiolitis during week 27 (bronchiolitis peak); an incidence rate of 284 per 100 000 children in this age group, which was three times higher than the average of peaks in 2015–19. A similar increase was seen in intensive care unit (ICU) discharges for bronchiolitis, with an incidence rate of 15 per 100 000 children aged 0–4 years, which was 2·8 times higher than the average of peaks in 2015–19. These similar rate increases in hospitalisation and ICU discharges suggest that although there was more disease, it was not more severe than in previous years.
Figure.
Weekly discharge data from publicly funded hospitals (A) and ICUs (B) for children aged 0–4 years with bronchiolitis (ICD-10 code J21) in New Zealand, from week 1, 2015, to week 29, 2021
Data for 2015 and 2018 are represented by individual grey lines, which underlay the data for 2019 (blue line), 2020 (yellow line), and 2021 (red line). A nationwide level 4 lockdown was effective from week 13 to week 18, 2020, and a nationwide level 3 lockdowns in week 13, 2020, and from week 18 to week 20, 2020.4 Data for 2021 are provisional and from the New Zealand Ministry of Health Minimum National Dataset (unpublished data from New Zealand Ministry of Health; extracted Sept 7, 2021). The denominator for rates is the estimated New Zealand resident population aged 0–4 years from the beginning of quarter 1 in 2015 to the end of quarter 2 in 2021. All population estimates at June 30, 2018, and beyond use the 2018 baseline data.5 ICD-10=international classification of diseases tenth edition. ICU=intensive care unit. RSV=respiratory syncytial virus.
Despite New Zealand being largely free of COVID-19 and influenza—with only one hospitalisation and no ICU admissions due to COVID-19 in children aged 0–4 years and no positive influenza isolates in any age group8 as of week 29, 2021—the pressure on the New Zealand health system due to bronchiolitis has been substantial. In countries with a higher COVID-19 burden, particularly those in the northern hemisphere that are entering their third winter since the start of this pandemic, the pressures resulting from RSV epidemics might be even greater than has been seen in New Zealand. Planning for preventive measures is needed now. Infection control measures, such as keeping infants and children with respiratory symptoms at home, will be required, and hospitals should prepare for increased numbers of admissions than historical data suggest.
LH, TH, and RB were involved in conceptualisation. LH, TH, and AE collected the data. AE analysed the data and created the graphs. LH wrote the first draft of the manuscript; all authors contributed to the final version. TH declares research grants for COVID-19 treatment studies from the Health Research Council of New Zealand. RB declares independent research organisation funding from the Health Research Council of New Zealand. All other authors declare no competing interests. We thank Sean Carroll, Information Analyst at the Ministry of Health (New Zealand), for providing the raw New Zealand National Minimum Dataset data.
References
- 1.Agha R, Avner JR. Delayed seasonal RSV surge observed during the COVID-19 pandemic. Pediatrics. 2021;148 doi: 10.1542/peds.2021-052089. [DOI] [PubMed] [Google Scholar]
- 2.Cohen R, Ashman M, Taha MK, et al. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now. 2021;51:418–423. doi: 10.1016/j.idnow.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant CC, Huang QS, Trenholme A, Taylor S, Wood T. What can we learn from our 2021 respiratory syncytial virus experience? N Z Med J. 2021;134:7–12. [PubMed] [Google Scholar]
- 4.New Zealand Government History of the COVID-19 alert system. https://covid19.govt.nz/alert-levels-and-updates/history-of-the-covid-19-alert-system
- 5.Statistics New Zealand Estimated resident population by age and sex (1991+) (Qrtly-Mar/Jun/Sep/Dec) http://infoshare.stats.govt.nz/ViewTable.aspx?pxID=d8ec5398-cf0b-49fb-b4e6-8fdc309444ee
- 6.ESR . ESR; 2021. Laboratory-based virology weekly report, 2021.https://www.esr.cri.nz/our-research/research-projects/shivers-v-study/shivers-v-reports/laboratory-based-virology-weekly-report/ [Google Scholar]
- 7.Public Health Surveillance inforamtion for New Zealands Public Health Action . ESR; 2021. Laboratory-based virology weekly report, 2004–19.https://surv.esr.cri.nz/virology/virology_weekly_report.php [Google Scholar]
- 8.Hills T, Hatter L, Kearns N, Bruce P, Beasley R. COVID-19 border controls prevent a 2021 seasonal influenza epidemic in New Zealand. Public Health. 2021 doi: 10.1016/j.puhe.2021.09.013. published online Sept 20. [DOI] [PMC free article] [PubMed] [Google Scholar]