Abstract
Study Objectives
Cognitive-behavioral therapy for insomnia (CBT-I) is the recommended first-line treatment for cancer-related insomnia, but its accessibility is very limited in routine care. A stepped care approach has been recommended as a cost-effective way to make CBT-I more widely accessible. However, no controlled study has yet been published about the efficacy of this approach. The goal of this noninferiority randomized controlled trial (RCT) was to compare the short and long-term efficacy of a stepped care CBT-I (StepCBT-I) to a standard face-to-face CBT-I (StanCBT-I).
Methods
A total of 177 cancer patients were randomized to: (1) StanCBT-I (6 face-to-face CBT-I sessions; n = 59) or (2) StepCBT-I (n = 118). In the StepCBT-I group, patients with less severe insomnia first received a web-based CBT-I (n = 65), while those with more severe insomnia received 6 face-to-face CBT-I sessions (n = 53). In both cases, patients could receive up to three booster sessions of CBT-I if they still had insomnia symptoms following this first step.
Results
Results indicated that the Step-CBT-I group showed an Insomnia Severity Index score reduction and a sleep efficiency (on a sleep diary) increase that was not significantly inferior to that of StanCBT-I at all post-treatment time points. Analyses of secondary outcomes indicated significant time effects (ps < .001) and no significant group-by-time interactions (ps from .07 to .91) on other sleep diary parameters, sleep medication use, depression, anxiety, fatigue, and quality of life scores.
Conclusion(s)
The efficacy of stepped care CBT-I is not inferior to that of a standard face-to-face intervention and is a valuable approach to making this treatment more widely accessible to cancer patients.
Trial registration
ClinicalTrials.gov Identifier: NCT01864720 (https://clinicaltrials.gov/ct2/show/NCT01864720?term=Savard&draw=2&rank=6; Stepped Care Model for the Wider Dissemination of Cognitive-Behavioural Therapy for Insomnia Among Cancer Patients).
Keywords: insomnia, sleep, cancer, stepped care, cognitive-behavioral therapy, web-based intervention
Statement of Significance.
Stepped care models, beginning with a self-administered intervention followed, if needed, by a more intensive treatment, have repeatedly been proposed to help make cognitive-behavioral therapy for insomnia (CBT-I) more widely accessible. Yet, thus far only small uncontrolled trials have been published. In this noninferiority randomized controlled trial that comprised 177 cancer patients with insomnia symptoms, we compared the efficacy of a stepped care approach to deliver CBT-I (StepCBT-I) with that of a standard, face-to-face CBT-I (StanCBT-I). Results indicated that the StepCBT-I produced sleep improvements that were not significantly inferior to those of the StanCBT-I. Stepped care CBT-I is not inferior to a standard face-to-face intervention and is a valuable approach to making this treatment more widely accessible to cancer patients.
Introduction
Between 30% and 60% of cancer patients experience insomnia symptoms during their cancer care trajectory [1, 2]. Insomnia tends to persist over time (29% to 64% of the patients) [2] if no appropriate treatment is offered. Untreated chronic insomnia may lead to serious consequences including a higher risk of later developing other psychological disorders (e.g. depression) [3, 4], fatigue and cognitive impairments, diminished quality of life, and increased health care consultations [5] and risk for infections [6, 7].
Insomnia is a highly treatable disturbance. The efficacy of cognitive-behavioral therapy for insomnia (CBT-I) in cancer patients has been supported by several randomized controlled trials (RCTs) [8, 9], and current guidelines recommend using CBT-I as the first-line treatment for cancer-related sleep disturbances [10]. Up to 70% of cancer patients receiving CBT-I show a remission and sleep improvements are paralleled by reduced depression, anxiety, and fatigue symptoms and improved quality of life [11, 12].
Unfortunately, the accessibility to CBT-I is extremely limited due to a number of barriers [13, 14]. Self-administered forms of CBT-I are efficacious in the general population [15]. However, a meta-analysis indicated that sleep improvements from self-administered CBT-I were consistently of a lower magnitude than those from face-to-face CBT-I [16]. This is in keeping with the results of our RCT conducted in women with breast cancer which revealed that a video-based CBT-I (60-min video + 6 booklets) led to significantly greater sleep improvements than a no-treatment condition, but that a 6-session face-to-face CBT-I produced greater effects than the video-based intervention on key variables including insomnia severity [12].
This led us and others to conclude that self-administered CBT-I would be better used as part of a stepped care model [17, 18]. In stepped care, the entry level is generally a minimal intervention, such as self-help intervention, followed by a more intensive form of treatment if needed. As a result, more intensive and expensive treatments are reserved for patients who do not benefit or are not expected to benefit from first-line treatments [19]. To date, only two small, uncontrolled studies have tested a stepped care CBT-I offered in the general population [20] and cancer patients [21]. For the current study, we developed a web-based version of our video-based program as the first treatment step in view of the accumulating evidence supporting the efficacy of web-based CBT-I [22, 23]. To replicate what would most likely be done in real clinical settings, the second step, offered to unremitted patients, was composed of up to three face-to-face CBT-I sessions.
This noninferiority RCT compared the short- and long-term efficacy of a stepped care approach to deliver CBT-I (StepCBT-I) with that of standard professionally-administered treatment (StanCBT-I). It was hypothesized that StepCBT-I would be associated with sleep improvements (i.e. reduced insomnia severity and increased sleep efficiency [SE]) at all post-treatment time points not significantly inferior to those associated with StanCBT-I. A secondary goal was to compare treatment effects on other parameters from a sleep diary, depression, anxiety, fatigue, and quality of life.
Methods
Participants
Inclusion criteria
(1) Diagnosis of nonmetastatic cancer (any type; patients with metastatic were excluded because the course of their disease is less predictable and may affect sleep) in the past 18 months; (2) Insomnia Severity Index (ISI) score ≥ 8 or using regularly (≥1 night per week) a psychotropic medication as a sleep aid (e.g. hypnotic); (3) age between 18 and 75 years old (to avoid including patients with age-related cognitive impairments); (4) readily able to read and understand French; (5) access to the Internet; and (6) living within 50 km from the research center.
Exclusion criteria
(1) Life expectancy < 1 year (to avoid confounding the results with the psychological impact and physical symptoms of such a condition); (2) severe psychiatric disorder (e.g. psychotic, substance use disorder; because these patients need other types of intervention); (3) severe cognitive impairments (e.g. diagnosis of dementia, or Mini-Mental State Examination [MMSE] score < 24) that would have made participation in this study very challenging); (4) formal diagnosis of another sleep disorder (e.g. obstructive sleep apnea); (5) shift work in the past 3 months or in the next 12 months; and (6) have received a psychological treatment specifically for a sleep disorder. These eligibility criteria were selected to be the most representative of what could eventually be done in real clinical settings where it would be unrealistic, for example, to systematically conduct a diagnostic interview or a polysomnographic (PSG) assessment to confirm the presence of an insomnia disorder or to rule out the presence of another sleep disorder.
Recruitment
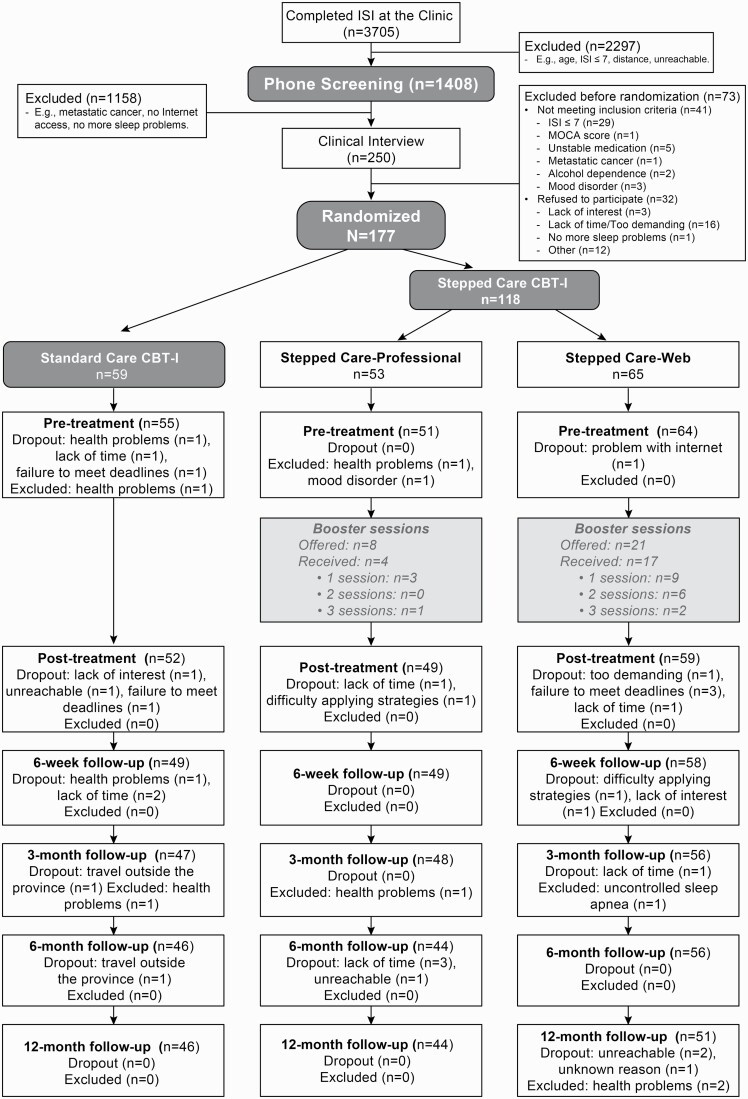
Participants were recruited between April 2014 and September 2017, mainly at the radio-oncology department of the CHU de Québec-Université Laval. As part of their routine care and for the purpose and duration of the study, all patients treated in this department completed at specific times in their cancer trajectory a psychological distress screening tool to which was attached the ISI. Patients were asked to provide written consent if they agreed that this information could be shared with our research team and to be contacted if they were eligible for this RCT (n = 3705 agreed; Figure 1). If they met the initial inclusion criteria (e.g. age, distance) and had an ISI score ≥ 8, patients (n = 1408) were contacted by phone to briefly assess their study eligibility and explain its goals and procedures. Other patients were recruited through direct referrals, ads in hospital waiting rooms, and via other sleep-related studies conducted by the research team. Consenting and eligible patients (n = 250) were then invited to a clinical interview 2 weeks later. In the meantime, they were asked to read and sign the informed consent form, complete a battery of self-report scales and keep a daily sleep diary for 2 weeks and wear an actigraphic recorder (not used here) for 7 consecutive 24-hour periods, all of which were sent by courier. The study was approved by the ethics committee of the CHU de Québec-Université Laval (#2012-1071).
Figure 1.
Flow chart.
Clinical interview and treatment allocation disclosure
The interview began by reviewing the informed consent form with the patients and by answering their questions. Then, questionnaires were reviewed to complete any missing data. Finally, the Montreal Cognitive Assessment (MoCA [24]) and the Structured Clinical Interview for DSM-IV (SCID [25]) were administered to screen out patients with cognitive and psychiatric disorders, as well as the Insomnia Interview Schedule (IIS [26], not used here). Seventy-three patients were excluded or refused to participate at that stage, thus leaving 177 patients for randomization. Finally, the treatment allocation was revealed to the participants.
Study design and randomization
The study used a randomized controlled noninferiority trial as this is the most rigorous methodology for testing whether a novel treatment, here the StepCBT-I, is as effective as the standard treatment [27]. An experimental design with two groups and a 1:2 allocation ratio was used. Eligible and consenting patients were randomly assigned to: (1) StanCBT-I consisting of six weekly face-to-face sessions administered individually (n = 59) or (2) StepCBT-I (n = 118; Figure 1). The entry level of the StepCBT-I differed depending on baseline insomnia severity: the first step was a web-based CBT-I for patients with less severe symptoms (ISI ≥ 8 and <15; n = 65), while six weekly face-to-face sessions of CBT-I administered individually were first offered to those with more severe symptoms (ISI ≥ 15; n = 53). For both these groups, the second step, which was only offered to unremitted patients, consisted of up to three face-to-face booster sessions of CBT-I administered every 2 weeks. Study measures were collected at pretreatment (T1), immediately after the first treatment step (T2; 6 weeks) and the second treatment step (T3; 3 months), as well as at 6- (T4) and 12-month (T5) follow-ups. The last follow-up assessment was completed in November 2018.
A computer-generated stratified randomization schedule was produced using SAS 9.4 PROC PLAN, under a permutated block randomization procedure with variable block sizes (6, 9, and 12 participants per block) to preserve the blind random assignment while minimizing between-groups imbalance during the trial. Stratification was performed based on baseline ISI scores (≥8 and <15, or ≥15). Results were contained in individually sealed, opaque envelopes prepared by an independent research assistant prior to study initiation, to keep research personnel blind as to the sequences of the patients’ group allocation. Envelopes were opened sequentially by a research assistant after the patient’s eligibility was confirmed, in the patient’s presence so both of them learned at the same time to what group the patient was assigned.
Intervention
The content of CBT-I was the same whether it was administered in face-to-face-sessions or self-administered through the Internet. Our CBT-I protocol is a 6-week multimodal intervention combining behavioral (i.e. stimulus control therapy, sleep restriction), cognitive (i.e. cognitive restructuring), and educational (i.e. sleep hygiene) strategies.
Standard care CBT-I
In this group, patients received six weekly sessions of CBT-I of approximately 50 min, offered individually by a clinician. Participants were instructed to read a short booklet before each treatment session. They received no further intervention after this 6-week intervention was completed, regardless of whether their insomnia was remitted or not.
Stepped care CBT-I
Based on our previous findings showing a small remission rate in patients with severe insomnia who had received a video-based CBT-I (24.6%) [12], the first step of treatment differed depending on baseline ISI scores (see Measures section for a justification of ISI scores used). This is in accordance with two main characteristics of stepped care models, that is, to offer as the first step a treatment modality that is likely to produce a significant gain and to adjust the level of the intervention to patients’ needs [28].
First step: patients having an ISI score ≥ 8 and < 15
Patients of this condition first completed our web-based CBT-I (www.insomnet.com). Each week, patients had to read the written information on the website, and then watch a video capsule (between 5 and 20 min each). The treatment material was identical to that of the video-based CBT-I that we previously developed and tested [12, 29], but was supplemented by the completion of daily sleep diaries on the website and interactive functionalities.
First step: patients having an ISI score ≥ 15
These patients received six weekly sessions of CBT-I administered individually by a clinician as described above.
Second step: all stepped care patients
Remitted patients (ISI < 8) at T2 received no further treatment. Patients who still obtained an ISI score ≥ 8 or reported using a hypnotic medication ≥ 1 night/week at T2 were then “stepped up” and received up to three 50-min booster sessions of CBT-I offered every 2 weeks individually by a clinician. An ISI score < 8 indicates the absence of insomnia [30] and the use of hypnotic medication ≥ 1 night/week was previously used to determine the presence of insomnia symptoms [31]. The content of these sessions was individualized to each patient’s needs based on a summary done at the first session to identify the strategies that had been tried, those that had been successful/unsuccessful, and the barriers that were encountered in their application. Individualized problem solving and motivational interviewing were performed based on that information. A research assistant called the stepped-up patients the week following the first two booster sessions to assess whether they needed to receive an additional treatment session, that is, if the patient still had insomnia symptoms (ISI score ≥ 8).
Interactive functionalities of Insomnet
Interactive functionalities included automated emails to remind participants to complete the treatment tasks and encourage adherence, give tailored feedback and information on changes in their sleep (e.g. texts, charts) based on their sleep diary data, and quizzes with an automated correction to reinforce patients’ understanding of the content. For instance, patients automatically received their weekly total wake time, total time spent in bed, and SE. Based on this information, they received an individualized sleep window for the following week (i.e. time in bed), which they were instructed not to exceed, and a tool helped them to select their bedtime and arising time (i.e sleep restriction procedures). Other examples of tailored feedback included reiterating the negative effects of napping to those patients who had reported doing so during the day and the importance of keeping a regular sleep/wake schedule to those who had reported variable bedtimes and arising times (stimulus control strategies).
Therapists' training and supervision
Therapists were doctoral students in clinical psycho-oncology who had to follow the treatment manual developed by J.S. and M.H.S., two therapists experienced in administering CBT-I in cancer patients. Before therapists began seeing patients, they had to read the treatment protocol and listen to several audiotapes of CBT-I sessions from a previous study. With regard to supervision, all treatment sessions were audiotaped and M.H.S. listened to each of the therapists’ first two sessions and two randomly selected sessions for each subsequent patient before providing individualized written feedback. All cases were also discussed during weekly group supervisions conducted by J.S. and M.H.S.
Measures
The main outcome measures for the noninferiority analyses were the total ISI score and SE derived from a daily sleep diary (completed for 2 weeks). Secondary measures were other parameters from the sleep diary and validated questionnaires. A questionnaire was administered to collect demographics (e.g. age, occupation), cancer treatments received, and psychological and medical comorbidity. Medical charts were consulted to collect/corroborate medical data.
Sleep measures
ISI [26, 30]: The ISI is a 7-item questionnaire designed to evaluate insomnia severity (e.g. difficulties falling asleep), impairment of daytime functioning due to sleep problems, noticeability of impairments, distress or worry caused by sleep difficulties, and dissatisfaction with sleep. Each item is rated using a five-point Likert scale ranging from “0” (not at all) to “4” (very much), for a total score ranging from 0 to 28. A score ≥ 8 indicates the presence of insomnia symptoms, while a score ≥ 15 indicates the possible presence of an insomnia syndrome [30]. These cutoff scores were used to stratify participants according to their insomnia severity and to determine what first treatment step they would receive and the cutoff score < 8 was used to establish if they had remitted after this first level of treatment. Sleep Diary: The dependent variables derived from the sleep diary are: sleep onset latency (SOL; time to sleep after lights out), wake after sleep onset (WASO; summation of nocturnal awakenings), total wake time (TWT; summation of SOL, WASO, and early morning awakening), total sleep time (TST; time in bed minus total wake time), sleep efficiency (SE: ratio of total sleep time to the actual time spent in bed), and use of sleep-promoting medications (type, frequency, and dosage). While subjective reports do not always correspond to PSG data, they still provide a reliable index of insomnia [32].
Other constructs
Hospital Anxiety and Depression Scale (HADS) [33, 34]: This questionnaire includes 14 items divided into two sub-scales: depression (HADS-D) and anxiety (HADS-A). Fatigue Symptom Inventory (FSI) [35]: The FSI is a multidimensional questionnaire developed for and validated in patients with cancer. It contains three subscales (fatigue intensity, impact of fatigue on quality of life, and duration of fatigue) for a total of 14 items. A composite fatigue score was derived by calculating the average of the three severity items (i.e. fatigue on the day they felt most fatigued, the least fatigued, and on average in the past week). The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (QLQ-C33) [36, 37]: This questionnaire was developed and validated with cancer patients to assess multidimensional aspects of quality of life. Only the overall quality of life item was used. Scores are transformed to give a value ranging from 0 to 100. Cronbach’s alphas obtained in this study were 0.739 for the ISI, 0.744 for HADS-D, 0.759 for the HADS-A, and 0.733 for the FSI.
Power analysis
The sample size estimate for the main hypotheses is based on standard power conditions for noninferiority trials [38]: one-tailed 5% alpha, 90% power, and an attrition rate of 20% (based on our previous RCT [12]). As recommended [38] and as in our prior work [39], a clinical margin of a maximum of four points on the ISI was used, which corresponds to half of the reduction that is considered a clinically significant change [40]. Thus, assuming a noninferiority margin of 4 units for the ISI, this RCT required a total sample of 151 to have sufficient power to reject the null hypothesis (N = 268 for a margin of 3 and N = 96 for a margin of 5). Hence, our initial sample (N = 177 patients; 158 after attrition at post-treatment) had sufficient power to test the main hypothesis. Similar computations yielded a margin of 4% for SE.
Statistical analyses
All data were double-entered. Analyses were performed using an intent-to-treat approach [41]. No data imputation was performed, since linear/generalized mixed models are robust to non-informative missing data [42]. Demographics, health-related data, medical comorbidity, medication use, cancer characteristics, and treatments were investigated as potential confounders and were planned to be included as covariates in the analyses if they met the following criteria: (1) a significant difference was obtained between the two conditions at baseline on that variable and (2) a correlation of .30 or more was obtained between the covariate and primary outcomes [43].
Noninferiority analyses
The noninferiority of a treatment can be established: (1) by computing a direct p-value to accept or reject the null hypothesis of inferiority at a 5% alpha level or (2) by verifying whether the estimated difference and the lower bound of its 95% confidence interval falls within the pre-established noninferiority margin [44]. For this study, the second strategy was preferred given that the difference between StanCBT-I and StepCBT-I (and it is 95% CI) was estimated from a split-plot mixed model (vs. binomial test for proportions or t-test on post-treatment means).
Secondary outcomes
Linear (for normal distributions) and generalized (for binary outcomes, i.e. remission rates and proportion of hypnotic users) mixed-effect regression models with covariates [45] were used to estimate the marginal means and test significant differences between temporal changes observed in the two groups for all secondary outcomes. Group, time, and covariates were included in the model as fixed main effects, with an additional random intercept according to patient ID. Between-groups differences at post-treatment assessments were computed by decomposing time-by-treatment interactions using a priori simple effects. No interim analysis was performed. Analyses were conducted using SAS 9.4 software with a standard two-tailed 5% alpha level.
Results
Baseline participants’ characteristics
On average, participants were 55.2 years old (Table 1). Females represented 86.3% of the sample and breast cancer was the most common type of neoplasia (76.7%). Since groups did not differ on any demographic and medical characteristics listed in Table 1, no covariate was included in the statistical models. Of the 177 patients initially randomized, 15 did not complete T2 and an additional 15 did not complete follow-ups (5 at T3, 5 at T4, and 5 at T5). All participants were White.
Table 1.
Participants’ demographics and medical characteristics by group and overall at baseline (N = 177)
| Variable | StanCBT-I (N = 59) |
StepCBT-I (N = 118) |
Overall (N =177) |
Test (chi-square or t-test) |
|---|---|---|---|---|
| Age (years)—M (SD) | 54.8(11.1) | 55.5(10.0) | 55.2(10.4) | 0.18, p = .68 |
| Sex—% women (n) | 82.8(48) | 88.0(103) | 86.3(151) | 0.87, p = .34 |
| Education—% with at least college degree (n) | 87.9(51) | 89.0(105) | 88.6(156) | 0.04, p = .84 |
| Marital status—% married/common law (n) | 70.7(41) | 63.3(74) | 65.7(115) | 0.95, p = .33 |
| Family income—% (n) | 3.79, p = .43 | |||
| 0–39 K$ | 11.9(7) | 18.6(22) | 16.4 (29) | |
| 40–79K$ | 33.9(20) | 39.8(47) | 37.9(67) | |
| 80–119K$ | 22.0(13) | 21.2(25) | 21.5(38) | |
| 120K$ or more | 22.0(13) | 14.4(17) | 16.9(30) | |
| No answer | 10.2(6) | 5.9(7) | 7.3(13) | |
| Occupation—% (n) | 2.36, p = .50 | |||
| Working full/part time | 8.5(5) | 16.9(20) | 14.1(25) | |
| Sick leave | 54.2(32) | 48.3(57) | 50.3(89) | |
| Retirement | 30.5(18) | 28.0(33) | 28.8(51) | |
| Other | 6.8(4) | 6.8(8) | 6.8(12) | |
| Medical comorbidity—% (n) | 69.0(40) | 69.5(82) | 69.3(122) | 0.01, p = .94 |
| Psychotropic medication usage—% (n) | 47.5(28) | 46.6(55) | 46.9(83) | 0.01, p = .92 |
| Time since cancer diagnosis (months)—M (SD) | 7.9(3.5) | 9.7(11.2) | 9.2(9.5) | 1.54, p = .24 |
| Cancer diagnosis—% (n) | 4.47 (df = 3), p = .22 | |||
| Breast | 72.4(42) | 78.8(93) | 76.7(135) | |
| Prostate | 8.6(5) | 5.1(6) | 6.3(11) | |
| Gynecological | 8.6(5) | 2.5(3) | 4.6(8) | |
| Other | 10.3(6) | 13.6(16) | 12.5(22) | |
| Cancer stage—% (n) | 10.32 (df = 5), p = .07 | |||
| 0 | 8.5 (5) | 4.2 (5) | 5.7 (10) | |
| I | 15.3 (9) | 17.8 (21) | 17.0 (30) | |
| II | 1.7 (1) | 13.6 (16) | 9.6 (17) | |
| III | 6.8 (4) | 2.5 (3) | 4.0 (7) | |
| IV | 0.0 (0) | 1.7 (2)† | 1.1 (2)† | |
| Unkown/not available | 67.8 (40) | 60.2 (71) | 62.7 (111) | |
| Cancer treatments–% (n)* | ||||
| Surgery | 83.1(49) | 90.6(106) | 88.1(155) | 2.13, p = .14 |
| Chemotherapy | 55.9(33) | 48.7(57) | 51.1(90) | 0.82, p = .37 |
| Radiotherapy | 84.8(50) | 90.6(106) | 88.6(156) | 1.33, p = .25 |
| Hormone therapy | 42.4(25) | 52.1(61) | 48.9(86) | 1.50, p = .22 |
*All participants had completed their radiation therapy at study entry. Only three patients treated with chemotherapy were still on treatment at study entry. For hormone therapy, 74% of the 86 patients treated were still on treatment at study entry and this percentage was not significantly different between groups (63.2% for StanCBT-I vs. 78.2% for StepCBT-I), χ2 (1) = 1.67, p = .20.
†These patients were included because their cancers were stages IVA and had spread to lymph nodes only.
Comparison between completers and non-completers
Exploratory comparisons at T3 revealed that non-completers were less likely to have breast cancer (59% for non-completers vs. 80% for completers, p = .01). However, the completer status was unrelated to treatment condition (p = .15), sex (p = .53), age (p = .26), education (p = .60), marital status (p = .30), occupation (p = .15), time since cancer diagnosis (p = .68), medical comorbidity (p = .85), and psychotropic medication use (p = .33).
Noninferiority analyses
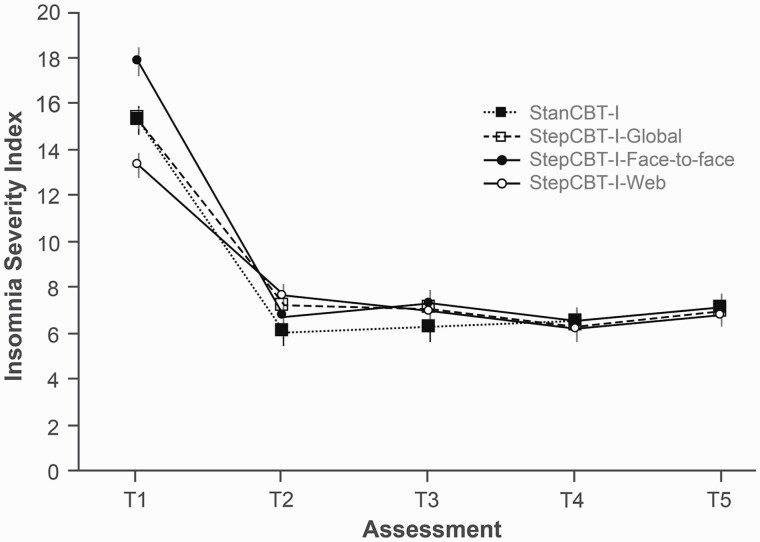
Table 2 shows mean scores obtained on all questionnaires and sleep parameters from the sleep diary at each time point. Figure 2 shows mean ISI scores obtained for both groups, as well as each StepCBT-I subgroup. As shown, although ISI scores at T1 differed between the two StepCBT-I subgroups due to the stratification on that variable, all groups ended up at T2–T5 at about the same level of insomnia severity.
Table 2.
Estimated means (95% CI) and effect sizes of time effects for sleep and psychological measures by group and time (N = 177)
| Variable and group | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|
| Insomnia severity (ISI; 0–28; cutoff ≥ 8) | |||||
| StanCBT-I | 15.3 (14.2–16.4) — |
6.0 (4.9–7.2) d = −2.20 |
6.3 (5.1–7.5) d = 0.05 |
6.5 (5.3–7.7) d = 0.06 |
7.1 (5.9–8.3) d = 0.14 |
| StepCBT-I | 15.3 (14.6–16.1) — |
7.2 (6.4–8.0) d = −1.95 |
7.1 (6.3–7.9) d = −0.03 |
6.3 (5.5–7.1) d = −0.18 |
6.9 (6.1–7.8) d = 0.15 |
| Sleep onset latency (min) | |||||
| StanCBT-I | 30.9 (26.4–35.4) — |
15.7 (10.9–20.5) d =−0.87 |
17.3 (12.4–22.1) d = 0.09 |
15.5 (10.6–20.5) d = −0.10 |
16.8 (11.9–21.7) d = 0.07 |
| StepCBT-I | 34.9 (31.8–38.1) — |
17.8 (14.5–21.1) d = −0.98 |
18.9 (15.6–22.2) d = 0.06 |
18.9 (15.5–22.2) d = 0.00 |
20.7 (17.3–24.1) d = 0.10 |
| Wake after sleep onset (min) | |||||
| StanCBT−I | 41.8 (35.3–48.3) — |
20.5 (13.6–27.4) d = −0.84 |
20.2 (13.3–27.2) d = −0.01 |
23.9 (16.9–30.9) d = 0.14 |
20.4 (13.3–27.4) d = −0.14 |
| StepCBT-I | 50.4 (45.8–55.0) — |
29.4 (24.6–34.8) d = −0.83 |
28.7 (23.9–33.5) d = −0.03 |
24.6 (19.8–29.4) d = −0.16 |
28.2 (23.3–33.0) d = 0.14 |
| Total wake time (min) | |||||
| StanCBT-I | 101.0 (90.4–111.6) — |
51.6 (40.3–62.9) d = −1.19 |
54.7 (43.3–66.2) d = 0.08 |
59.0 (47.4–70.6) d = 0.10 |
55.3 (43.7–66.9) d = −0.09 |
| StepCBT-I | 122.8 (115.3–130.3) — |
68.2 (60.4–75.9) d = −1.32 |
67.2 (59.3–75.0) d = −0.02 |
65.2 (57.3–73.1) d = −0.05 |
69.5 (61.5–77.5) d = 0.10 |
| Total sleep time (min) | |||||
| StanCBT-I | 407.4 (391.6–423.2) — |
410.4 (393.8–427.1) d = 0.05 |
417.8 (401.0–434.6) d = 0.12 |
421.3 (404.3–438.3) d = 0.06 |
432.7 (415.7–449.7) d = 0.19 |
| StepCBT-I | 421.3 (410.1–432.5) — |
431.1 (419.7–442.6) d = 0.16 |
438.9 (427.3–450.5) d = 0.13 |
445.4 (433.7–457.0) d = 0.10 |
445.5 (433.7–457.2) d = 0.00 |
| Sleep efficiency (%) | |||||
| StanCBT-I | 80.1 (78.0–82.2) — |
88.6 (86.4–90.8) d = 1.05 |
88.1 (85.9–90.3) d = −0.06 |
87.7 (85.4–90.0) d = −0.05 |
88.4 (86.2–90.7) d = 0.09 |
| StepCBT-I | 77.5 (76.0–78.9) — |
86.3 (84.8–87.8) d = 1.09 |
86.7 (85.2–88.2) d = 0.05 |
87.2 (85.7–88.8) d = 0.07 |
86.4 (84.8–87.9) d = −0.11 |
| Sleep medication (% of users) | |||||
| StanCBT-I | 47.5 (35.1–60.1) |
23.7 (14.6–36.2) |
23.7 (14.6–36.2) |
18.6 (10.6–30.6) |
18.6 (10.6–30.6) |
| StepCBT-I | 46.6 (37.8–55.6) |
27.1 (19.9–35.9) |
27.1 (19.9–35.9) |
23.7 (16.9–32.2) |
24.6 (17.6–33.2) |
| Anxiety symptoms (HADS-A; 0–21; cutoff ≥ 7) | |||||
| StanCBT-I | 7.1 (6.3–8.0) — |
4.4 (3.6–5.3) d = −0.85 |
4.2 (3.3–5.1) d = −0.08 |
4.8 (3.9–5.7) d = 0.19 |
4.8 (3.9–5.7) d = 0.00 |
| StepCBT-I | 6.7 (6.1–7.3) — |
4.9 (4.3–5.5) d = −0.56 |
5.1 (4.5–5.7) d = 0.05 |
4.8 (4.2–5.4) d = −0.07 |
5.0 (4.4–5.6) d = 0.06 |
| Depressive symptoms (HADS-D; 0–21; cutoff ≥ 7) | |||||
| StanCBT-I | 4.5 (3.8–5.3) — |
2.7 (2.0–3.4) d = −0.68 |
2.7 (1.9–3.5) d = 0.00 |
3.0 (2.2–3.7) d = 0.10 |
2.6 (1.8–3.3) d = −0.14 |
| StepCBT-I | 4.5 (4.0–5.0) — |
2.8 (2.3–3.3) d = −0.62 |
3.2 (2.7–3.7) d = 0.14 |
2.9 (2.3–3.4) d = −0.13 |
3.0 (2.4–3.5) d = 0.04 |
| Fatigue (FSI; 0–10; cutoff ≥ 3) | |||||
| StanCBT-I | 4.7 (4.3–5.1) — |
3.4 (2.9–3.8) d = −0.86 |
3.1 (2.6–3.5) d = −0.18 |
3.1 (2.7–3.6) d = 0.05 |
3.3 (2.9–3.8) d = 0.12 |
| StepCBT-I | 5.0 (4.7–5.3) — |
3.9 (3.6–4.2) d = −0.66 |
3.9 (3.6–4.2) d = 0.00 |
3.7 (3.4–4.0) d = −0.13 |
3.8 (3.5–4.1) d = 0.05 |
| Quality of life (QLQ–C33; 0–100) | |||||
| StanCBT-I | 61.5 (56.6–66.4) — |
74.5 (69.3–79.7) d = 0.69 |
75.4 (70.0–80.7) d = 0.05 |
76.1 (70.7–81.6) d = 0.04 |
78.2 (72.7–83.6) d = 0.11 |
| StepCBT-I | 62.3 (58.9–65.7) — |
70.9 (67.3–74.5) d = 0.46 |
71.7 (68.1–75.4) d = 0.04 |
73.1 (69.4–76.8) d = 0.07 |
71.4 (67.7–75.2) d = −0.09 |
For each cell, the first row is the estimated marginal means from the mixed model, the second row (in parenthesis) is the 95% confidence interval around marginal means and the third row is the within-condition effect size (Cohen’s d) between means at this time and previous time (only for continuous variables). ISI, Insomnia Severity Index; HADS-A, anxiety subscale of the Hospital Anxiety and Depression Scale; HADS-D, depression subscale of the Hospital Anxiety and Depression Scale; FSI, Fatigue Symptom Inventory; QLQ, Quality of Life Questionnaire.
Figure 2.
Means (and standard errors) of Insomnia Severity Index (ISI) scores by group (StanCBT-I, StepCBT-I-Global, StepCBT-I-Face-to-face, and StepCBT-I-Web) and time.
ISI
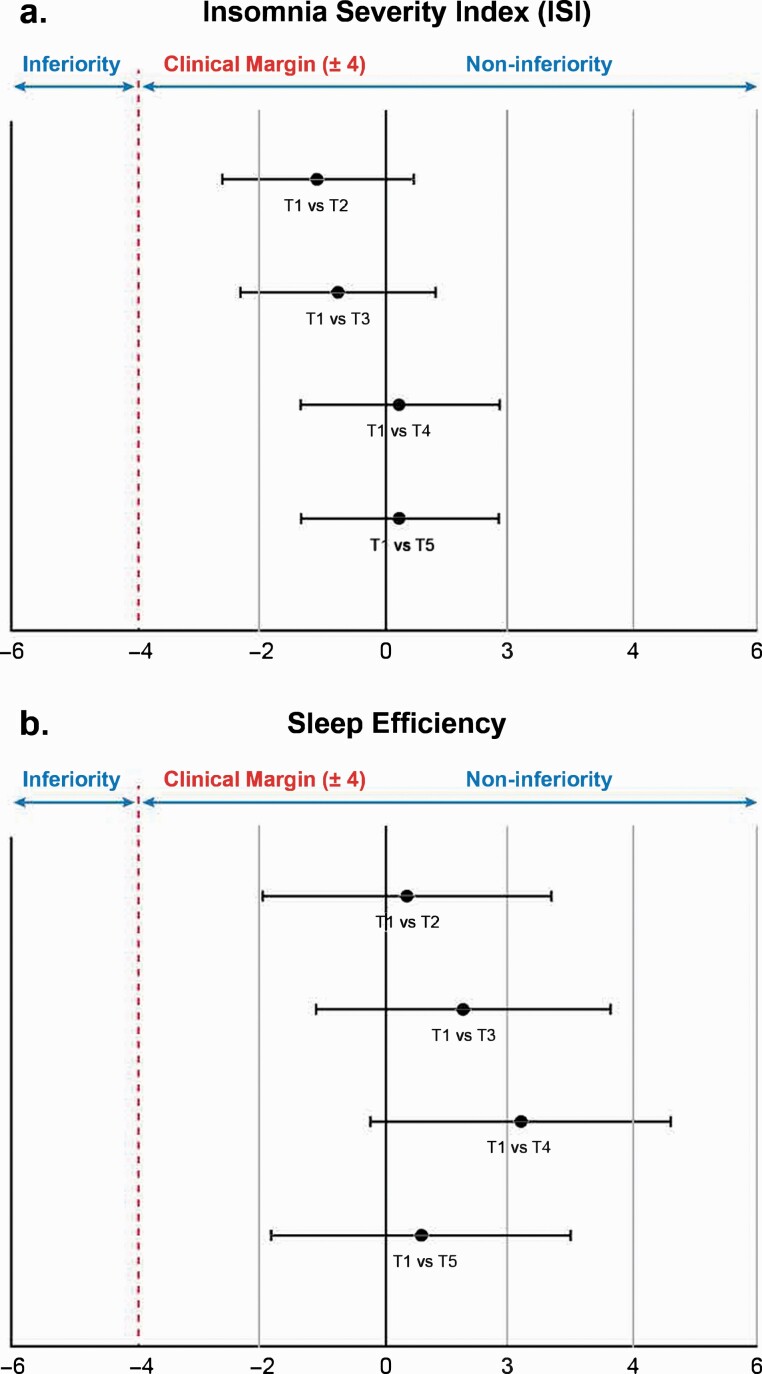
All between-group differences on ISI reductions from T1 fell well within the established clinical margin of ±4 points (Figure 3). StepCBT-I produced a mean ISI reduction of −8.16 points at T2 while StanCBT-I yielded a reduction of −9.24 points (delta = −1.08, 95% CI = −2.62 to 0.46). At T3, T4, and T5, respectively, deltas between the two groups change scores were −0.75 (95% CI = −2.33 to 0.82), +0.24 (95% CI = −1.36 to 1.84), and +0.23 (95% CI = −1.36 to 1.83).
Figure 3.
Results of noninferiority analyses on ISI scores (top panel) and sleep efficiency (sleep diary; bottom panel). Data illustrated are between-groups differences on improvement obtained between baseline (T1) and subsequent time points (T2 to TS; delta values) as assessed with the ISI (total score; A) and sleep efficiency (sleep diary; B). Bars shows the 95% confidence intervals. Values falling within the established clinical margin of ±4 indicate noninferiority of the stepped care CBT-1 as compared to standard care CBT-1. Values falling on the right of the vertical bold line (i.e. positive deltas) indicate greater improvements in stepped care CBT-1 vs. standard care CBT-1.
SE
All between-groups differences on SE augmentation from T1 also fell well within the clinical margin of ±4% at each time point (Figure 3). At T2, the SE increase was 0.35 points higher in StepCBT-I than in StanCBT-I (+8.80% vs. +8.45%, respectively; 95% CI = −1.98 to 2.69). At T3 (95% CI = −1.11 to 3.64), T4 (95% CI = −0.23 to 4.59), and T5 (95% CI = −1.84 to 3.00), augmentations were 1.26, 2.18, and 0.60 points higher in StepCBT-I, respectively.
Remission at post-treatment (T2) and acceptation of step 2 for StepCBT-I
After initial treatment (T2), 72.0% of StanCBT-I patients and 57.8% of StepCBT-I were remitted (ISI < 8), a difference that was not significant, F(1,420) = 2.86, p = .09. While StepCBT-I patients who began with face-to-face sessions (StepCBT-I-Face-to-Face: 66.0%) showed a higher percentage of remission at T2 compared to the web-based program (StepCBT-I-Web: 50.6%), this difference was also nonsignificant, t(417) = 1.61, p = .11.
In the StepCBT-I-Face-to-Face subgroup, eight participants were still symptomatic and were offered at least one booster session (Figure 1). Four of them accepted (50%; three received one session and one received three). In the StepCBT-I-Web subgroup, 21 were still symptomatic and 17 (81%) accepted to receive one (nine patients) or more booster sessions (two sessions: six patients; three sessions: two patients).
Remission at T3–T5
At T3 (after additional treatment sessions were received by non-remitted StepCBT-I), 74.8% of participants were remitted in StanCBT-I compared to 59.3% for StepCBT-I. This difference was not significant, F(1,420) = 3.25, p = .07. No significant differences were also observed at T4 (63.2% vs. 64.6%, respectively), F(1,420) = 0.02, p = .88, and T5 (54.7% vs. 56.3%, respectively), F(1,420) = 0.03, p = .86. Comparisons of remission rates between the two StepCBT-I subgroups were not significant at T3 (59.0% for StepCBT-I-Face-to-Face vs. 59.7% for StepCBT-I-Web), t(417) = 0.07, p = .94, T4 (62.0% vs. 66.7%, respectively), t(417) = 0.49, p = .62, and T5 (54.2% vs. 58.0%, respectively), t(417) = 0.38, p = .70.
Secondary outcomes analyses
Group (2) × time (5) mixed models showed significant time effects for all other variables from the sleep diary (Table 2): SOL: F(4,582) = 52.67, p < .001; WASO: F(4,579) = 58.55, p < .001; TWT: F(4,583) = 103.83, p < .001; and TST: F(4,584) = 10.61, p < .001 (Table 2). Except for TST (all ds < .10), changes between T1 and T2 corresponded to large effect sizes [46]: SOL: −0.87 versus −0.98; WASO: −0.84 versus −0.83; TWT: −1.19 versus −1.32 for StanCBT-I and StepCBT-I, respectively. No significant change was found from T2 to T5 (all ds < .20). All group × time interactions also failed to reach significance: SOL: F(4,582) = 0.31, p = .87; WASO: F(4,579) = 1.70, p = .15; TWT: F(4,583) = 1.52, p = .19; TST: F(4,584) = 0.66, p = .62.
A significant time effect was found on the proportion of patients using a sleep medication, F(4,700) = 11.32, p < .001. The proportion decreased from 47.5% to 23.7% at T2 in StanCBT-I (OR = 0.34, 95% CI from 0.20 to 0.60) and from 46.6% to 27.1% in StepCBT-I (OR = 0.43, 95% CI from 0.31 to 0.59). No significant change was observed between T2 and T5, F(3,700) = 1.42, p = .24, and the group × time interaction was not significant, F(4,700) = 0.25, p = .91.
Similarly, significant time effects were found for anxiety, F(4,582) = 35.11, p < .001, depression, F(4,581) = 4.05, p < .001, fatigue, F(4,596) = 31.00, p < .001, and quality of life, F(4,589) = 9.00, p < .001, with improvements between T1 and T2 that correspond to moderate to large effect sizes (anxiety: d = -0.85 vs. −0.56; depression: −0.68 vs. −0.62; fatigue: −0.86 vs. −0.66; and quality of life: 0.69 vs. 0.46 in StanCBT-I and StepCBT-I groups, respectively). Again, no significant change between T2 and T5 (all ds < 0.20) was found and no group × time interaction was significant: anxiety: F(4,582) = 2.20, p = .07; depression: F(4,581) = 0.68, p = .60; fatigue: F(4,596) = 0.98, p = .42, and quality of life, F(4,589) = 1.11, p = .35.
Unremitted StepCBT-I patients at T2 who completed at least one booster session reported a significant decrease of anxiety from T2 to T3–T5 (from M = 6.1 at T2 to M = 4.0 at T5), F(3,115) = 3.60, p = .02, and fatigue (from M = 4.6 at T2 to 3.9 at T5), F(3,117) = 2.69, p = .05, while those who refused further treatment failed to show such reduction: anxiety (M = 6.0 from T2 to T5), F(3,114) = 0.42, p = .74, and fatigue (M = 4.2 from T2 to T5), F(3,116) = 0.10, p = .96. No significant main or interaction effects were found for depression and quality of life.
Discussion
This study conducted in patients with cancer compared the short- and long-term efficacy of a standard CBT-I, administered individually by a clinician, to a stepped care approach in which the intensity of the intervention was adjusted to the initial insomnia severity and the presence or absence of remission after the first treatment phase was completed. As hypothesized, results of noninferiority analyses indicated that the efficacy of the StepCBT-I was non-inferior to that of StanCBT-I in reducing insomnia severity (ISI) and increasing SE (sleep diary). More precisely, the findings showed that between-group differences on ISI and SE improvements were falling well within the established clinical margins (e.g. all within a delta of 1.08 for the ISI vs. established margin of 4). These results indicate that a stepped care approach, that includes about half of the patients beginning treatment with a web-based intervention, provides treatment effects that are not significantly inferior to those found when using standard six face-to-face CBT-I sessions.
Analyses of secondary outcomes indicated significant and mainly large time effects and no significant differences in treatment effects between StepCBT-I and StanCBT-I groups on other sleep diary variables, sleep medication usage, symptoms (depression, anxiety, and fatigue), and quality of life. This shows once again that treating insomnia efficaciously with CBT-I is associated with parallel changes in psychological distress and fatigue.
This is the first randomized controlled trial on the effects of a stepped care CBT-I, although this approach has been recommended for at least a decade now as a cost-effective way to increase patient’s access to this treatment [47]. Our results are consistent with those of a handful of previous clinical trials supporting the efficacy of stepped care models to deliver CBT for mixed psychological disorders [48], social anxiety and panic disorder [49], and obsessive-compulsive disorder [50]. After the first step, 57.8% of our StepCBT-I patients were in remission from their insomnia (ISI < 8; 50.6% after the web-based and 66.0% after the face-to-face intervention) and 59.3% were remitted after the second step (booster sessions; 59.7% for StepCBT-I-Web vs. 59.0% for StepCBT-I-Face-to-Face format). It Is interesting to note that the remission rate of 57.8% in StepCBT-I-Web patients is better than we previously found with a video-based CBT-I in breast cancer patients (44.3%) [12]. Our remission rates also compare favorably with the only other study conducted in cancer patients thus far [51] which had a remission rate of 51% (26 out of 51; mean ISI score from 17.1 at baseline to 11.2 after step 1) after a first step composed of sleep hygiene and using a much more inclusive remission definition (ISI score < 12). Our stepped care approach is more intensive but our results suggest that this level of intensity is needed to make sure that the largest proportion of patients is successfully treated after the first level of care.
In the StepCBT-I group, as might have been predicted, the second level of care was offered to more patients from the web-based CBT-I (21/65; 32.3%) than from the face-to-face subgroup (8/53; 15.1%) and more patients from the StepCBT-I-Web (17/21; 81.0%) than from the StepCBT-I-Face-to-Face (4/8; 50.0%) accepted to receive additional treatment. Most patients received only one booster session (StepCBT-I-Web: 9/17 or 52.9%; StepCBT-I-Face-to-Face: 3/4 or 75.0%). At T3, T4, and T5, the remission rates of StepCBT-I patients were 59.3%, 64.6%, and 56.3%, respectively, and no significant difference was obtained with the StanCBT-I group (74.8%, 63.2%, and 54.7%, respectively). The remission rate of insomnia increased from 50.6% to 59.7% between T2 and T3 in those who received web-based CBT-I as their first treatment. Moreover, receiving booster sessions was associated with a greater decrease of anxiety and fatigue levels in the initially unremitted patients. Together, these findings emphasize the utility of providing booster sessions and confirm the clinical relevance of using a stepped care approach to administer CBT-I.
Our study is the first to compare, with sufficient statistical power, a stepped care CBT to high-intensity care as opposed to usual care. In most clinical settings, usual care amounts to doing nothing (or almost nothing) and thus sets the bar very low for proving the equivalent efficacy of a stepped care program [52]. Other strengths include the participants’ recruitment directly at the clinic, the small dropout rate, and the use of inclusive criteria, all of which increase the findings’ generalization. The fact that patients with heterogeneous complaints of insomnia (i.e. not diagnosed with an interview and no PSG to screen out patients with other sleep disorders) were eligible not only improves the study’s external validity but increases the applicability of this treatment modality in real clinical settings. On the other hand, our sample was all white, highly educated, and predominantly composed of women with breast cancer (76.7%). It will be important to replicate these findings in more diverse populations. Also, the sample represents a small proportion of all approached patients, thus affecting the study’s external validity. However, it is important to note that recruitment took place within a clinical setting offering cancer care to heterogeneous patients from all over eastern Quebec and that many patients were excluded due to older age and because they were living too far away to receive weekly face-to-face sessions. Now that, due to the COVID-19 pandemic, videoconferencing is more frequently used to offer psychotherapy sessions [53, 54], distance will become less of a barrier to participating in this type of program.
In the future, it would be interesting to assess whether it is possible to offer the web-based CBT-I as the first step to a larger number of patients (e.g. all patients regardless of their insomnia severity) without overly affecting the remission rate. This would make the treatment even more cost-effective. However, it will be important to ensure that a self-administered CBT-I offered to patients with more severe insomnia, that ends up being unsuccessful, does not translate into a lower interest and motivation to move on to the second step. Another avenue for future research would be to integrate into the stepped care model a preventive intervention for good sleepers. Indeed, given the many patients who develop insomnia during their cancer care trajectory, it would be extremely relevant to assess whether it is possible to avert its onset by providing an early and minimal form of CBT-I. We previously obtained encouraging results with a preventive booklet given to good sleepers before their chemotherapy for breast cancer but the results of this pilot study need replication in larger trials [55].
This study has significant clinical implications as it offers an alternative model of care to treat cancer-related insomnia that is less costly, while being not less efficacious, and which can therefore be more easily implemented in routine cancer care than standard CBT-I. Implementation of such a stepped care CBT-I could contribute considerably to improving patients’ access to CBT-I and thus reduce the psychological, physical, and financial burden of cancer-related insomnia.
Supplementary Material
Funding
This work was supported by the Canadian Institutes of Health Research (#125968).
Disclosure Statement
Financial Disclosure Statement
JS reports consulting fees from Astellas. CMM reports consulting fees from Eisai, Merck, Sunovion, Pear Therapeutics, and Weight Watchers and having received research grants from Idorsia, and Canopy Health. Stéphane Bouchard is president of Cliniques et Développement In Virtuo, a company that distributes virtual reality environments for the treatment of mental disorders. All of these are unrelated to this research work. All other authors report no competing interests.
Nonfinancial Disclosure Statement
None.
References
- 1. Palesh OG, et al. . Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol. 2010;28(2):292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Savard J, et al. . Natural course of insomnia comorbid with cancer: an 18-month longitudinal study. J Clin Oncol. 2011;29(26):3580–3586. [DOI] [PubMed] [Google Scholar]
- 3. Byrne EM, et al. . Sleep disorders and risk of incident depression: a population case-control study. Twin Res Hum Genet. 2019;22(3):140–146. [DOI] [PubMed] [Google Scholar]
- 4. Li L, et al. . Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016;16(1):375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Savard J, et al. . Chapter 130: Sleep and fatigue in cancer patients. In: Kryger MH RT, Dement WC, eds. Principles and Practice of Sleep Medicine. 6th ed. San Diego: Elsevier; 2017:1286–1293. [Google Scholar]
- 6. Ruel S, et al. . Insomnia and self-reported infections in cancer patients: an 18-month longitudinal study. Health Psychol. 2015;34(10):983–991. [DOI] [PubMed] [Google Scholar]
- 7. Ruel S, et al. . Insomnia, immune functioning and infections in cancer patients treated with chemotherapy: Results from a longitudinal study. Presented at: 38th Annual Meeting of the Society of Behavioral Medicine; March 2017 2017; San Diego, California, USA.
- 8. Savard J, et al. . Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. J Clin Oncol. 2005;23(25):6083–6096. [DOI] [PubMed] [Google Scholar]
- 9. Garland SN, et al. . Sleeping well with cancer: a systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsychiatr Dis Treat. 2014;10:1113–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Howell D, et al. ; Sleep Disturbance Expert Panel on behalf of the Cancer Journey Advisory Group of the Canadian Partnership Against Cancer. A Pan-Canadian practice guideline: prevention, screening, assessment, and treatment of sleep disturbances in adults with cancer. Support Care Cancer. 2013;21(10):2695–2706. [DOI] [PubMed] [Google Scholar]
- 11. Fleming L, et al. . Does cognitive behaviour therapy for insomnia reduce clinical levels of fatigue, anxiety and depression in cancer patients? Psychooncology. 2014;23(6):679–684. [DOI] [PubMed] [Google Scholar]
- 12. Savard J, et al. . Is a video-based cognitive behavioral therapy for insomnia as efficacious as a professionally administered treatment in breast cancer? Results of a randomized controlled trial. Sleep. 2014;37(8):1305–1314. doi: 10.5665/sleep.3918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Davidson JR, et al. . How to provide insomnia interventions to people with cancer: insights from patients. Psychooncology. 2007;16(11):1028–1038. [DOI] [PubMed] [Google Scholar]
- 14. Koffel E, et al. . Increasing access to and utilization of cognitive behavioral therapy for insomnia (CBT-I): a narrative review. J Gen Intern Med. 2018;33(6):955–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ho FY, et al. . Self-help cognitive-behavioral therapy for insomnia: a meta-analysis of randomized controlled trials. Sleep Med Rev. 2015;19:17–28. [DOI] [PubMed] [Google Scholar]
- 16. van Straten A, et al. . Self-help therapy for insomnia: a meta-analysis. Sleep Med Rev. 2009;13(1):61–71. [DOI] [PubMed] [Google Scholar]
- 17. Espie CA. “Stepped care”: a health technology solution for delivering cognitive behavioral therapy as a first line insomnia treatment. Sleep. 2009;32(12):1549–1558. doi: 10.1093/sleep/32.12.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baglioni C, et al. . The European Academy for Cognitive Behavioural Therapy for Insomnia: An initiative of the European Insomnia Network to promote implementation and dissemination of treatment. J Sleep Res. 2020;29(2):e12967. [DOI] [PubMed] [Google Scholar]
- 19. Newman MG. Recommendations for a cost-offset model of psychotherapy allocation using generalized anxiety disorder as an example. J Consult Clin Psychol. 2000;68(4):549–555. [PubMed] [Google Scholar]
- 20. Vincent N, et al. . Stepped care for insomnia: an evaluation of implementation in routine practice. J Clin Sleep Med. 2013;9(3):227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhou ES, et al. . Developing efficient and effective behavioral treatment for insomnia in cancer survivors: Results of a stepped care trial. Cancer. 2020;126(1):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Soh HL, et al. . Efficacy of digital cognitive behavioural therapy for insomnia: a meta-analysis of randomised controlled trials. Sleep Med. 2020;75:315–325. [DOI] [PubMed] [Google Scholar]
- 23. Zachariae R, et al. . Efficacy of internet-delivered cognitive-behavioral therapy for insomnia – a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2016;30:1–10. [DOI] [PubMed] [Google Scholar]
- 24. Nasreddine ZS, et al. . The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. [DOI] [PubMed] [Google Scholar]
- 25. First MB, et al. . Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Edition (SCID-I/P, Version 2.0). New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 26. Morin CM. Insomnia: Psychological Assessment and Management. New York, NY: The Guilford Press; 1993:238. [Google Scholar]
- 27. Morland LA, et al. . Issues in the design of a randomized noninferiority clinical trial of telemental health psychotherapy for rural combat veterans with PTSD. Contemp Clin Trials. 2009;30(6):513–522. [DOI] [PubMed] [Google Scholar]
- 28. Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency. Narrative literature review. Br J Psychiatry. 2005;186:11–17. [DOI] [PubMed] [Google Scholar]
- 29. Savard J, et al. . Long-term effects of two formats of cognitive behavioral therapy for insomnia comorbid with breast cancer. Sleep. 2016;39(4):813–823. doi: 10.5665/sleep.5634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Savard MH, et al. . Empirical validation of the Insomnia Severity Index in cancer patients. Psychooncology. 2005;14(6):429–441. [DOI] [PubMed] [Google Scholar]
- 31. Savard J, et al. . Prevalence, natural course, and risk factors of insomnia comorbid with cancer over a 2-month period. J Clin Oncol. 2009;27(31):5233–5239. [DOI] [PubMed] [Google Scholar]
- 32. Coates TJ, et al. . Discriminating good sleepers from insomniacs using all-night polysomnograms conducted at home. J Nerv Ment Dis. 1982;170(4):224–230. [DOI] [PubMed] [Google Scholar]
- 33. Zigmond AS, et al. . The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. [DOI] [PubMed] [Google Scholar]
- 34. Savard J, et al. . Evaluating anxiety and depression in HIV-infected patients. J Pers Assess. 1998;71(3):349–367. [DOI] [PubMed] [Google Scholar]
- 35. Hann DM, et al. . Measurement of fatigue in cancer patients: development and validation of the Fatigue Symptom Inventory. Qual Life Res. 1998;7(4):301–310. [DOI] [PubMed] [Google Scholar]
- 36. Aaronson NK, et al. . The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–376. [DOI] [PubMed] [Google Scholar]
- 37. Osoba D, et al. . Modification of the EORTC QLQ-C30 (version 2.0) based on content validity and reliability testing in large samples of patients with cancer. Qual Life Res. 1997;6:103–108. [DOI] [PubMed] [Google Scholar]
- 38. Hwang IK, et al. . Design issues in noninferiority: equivalence trials. Drug Inf J. 1999;33:1205–1218. [Google Scholar]
- 39. Mercier J, et al. . A non-inferiority randomized controlled trial comparing a home-based aerobic exercise program to a self-administered cognitive-behavioral therapy for insomnia in cancer patients. Sleep. 2018;41(10). doi: 10.1093/sleep/zsy149. [DOI] [PubMed] [Google Scholar]
- 40. Morin CM, et al. . The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wiens BL, et al. . The role of intention to treat in analysis of noninferiority studies. Clin Trials. 2007;4(3):286–291. [DOI] [PubMed] [Google Scholar]
- 42. Mallinckrodt CH, et al. . Recommendations for the primary analysis of continuous endpoints in longitudinal clinical trials. Drug Inf J. 2008;42:303–319. [Google Scholar]
- 43. Frigon J-Y, et al. . Analysis of covariance: a proposed algorithm. Educ Psychol Meas. 1993;53:1–18. [Google Scholar]
- 44. Wellek S. Testing Statistical Hypotheses of Equivalence and Noninferiority. Boca Raton, FL: CRC Press; 2010. [Google Scholar]
- 45. Brown H, et al. . Applied Mixed Models in Medicine. 2nd ed. Hoboken, NJ: Wiley; 2006. [Google Scholar]
- 46. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 47. Espie CA, et al. . Randomized controlled clinical effectiveness trial of cognitive behavior therapy compared with treatment as usual for persistent insomnia in patients with cancer. J Clin Oncol. 2008;26(28):4651–4658. [DOI] [PubMed] [Google Scholar]
- 48. Salomonsson S, et al. . Stepped care in primary care – guided self-help and face-to-face cognitive behavioural therapy for common mental disorders: a randomized controlled trial. Psychol Med. 2018;48(10):1644–1654. [DOI] [PubMed] [Google Scholar]
- 49. Nordgreen T, et al. . Stepped Care Versus Direct Face-to-Face Cognitive Behavior Therapy for social anxiety disorder and panic disorder: a randomized effectiveness trial. Behav Ther. 2016;47(2):166–183. [DOI] [PubMed] [Google Scholar]
- 50. Tolin DF, et al. . Stepped care versus standard cognitive-behavioral therapy for obsessive-compulsive disorder: a preliminary study of efficacy and costs. Depress Anxiety. 2011;28(4):314–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zhou ES, et al. . Internet-delivered insomnia intervention improves sleep and quality of life for adolescent and young adult cancer survivors. Pediatr Blood Cancer. 2020;67(9):e28506. [DOI] [PubMed] [Google Scholar]
- 52. van Stratten A, et al. . Stepped care treatment delivery for depression: a systematic review and meta-analysis. 2014;45(2):231–246 [DOI] [PubMed] [Google Scholar]
- 53. Connolly SL, et al. . Rapid increase in telemental health within the department of veterans affairs during the COVID-19 Pandemic. Telemed J E Health. 2021;27(4):454–458. [DOI] [PubMed] [Google Scholar]
- 54. Mishkind MC, et al. . Telemental health response to the COVID-19 Pandemic: virtualization of outpatient care now as a pathway to the future. Telemed e-Health. 2020. Online ahead of print. doi: 10.1089/tmj.2020.0303. [DOI] [PubMed] [Google Scholar]
- 55. Marion LP, et al. . Feasibility of a preventive intervention for insomnia in women with breast cancer receiving chemotherapy. Behav Sleep Med. 2021;19(1):70–82. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.