Abstract
Introduction
COVID-19 morbidity and mortality has disproportionately affected vulnerable populations such as minority racial/ethnic groups. Understanding disparities in vaccine intentions and reasons for vaccine hesitancy are important for developing effective strategies for ameliorating racial/ethnic COVID-19 inequities.
Methods
Using six waves of the large, nationally representative Census Bureau’s Household Pulse Survey data from January 6-March 29, 2021 (n = 459,235), we examined national and state estimates for vaccination intent, defined as receipt of ≥ 1 dose of the COVID-19 vaccine or definite intent to be vaccinated, by race/ethnicity with stratification by household income and age group. In separate logistic regression models, we also examined the interaction between race/ethnicity and household income, and race/ethnicity and age group, and its association with vaccination intent. Lastly, we examined reasons for not vaccinating by race/ethnicity.
Results
Vaccination intent differed by racial/ethnic group, household income, and age group nationally and by Health and Human Services (HHS) region and state. A significant interaction was observed between race/ethnicity and household income (F(8,72) = 4.50, p < 0.001), and race/ethnicity and age group (F(8,72) = 15.66, p < 0.001). Non-Hispanic Black adults with lower income (<$35,000) and younger age (18–49 years) were least likely to intend to vaccinate. Similar disparities across racial/ethnic groups were seen across most HHS regions and states. Concerns about possible side effects and effectiveness were significantly higher among all minority groups compared to non-Hispanic White adults.
Conclusion
Disparities in vaccination intent by racial/ethnic groups underscore the need for interventions and recommendations designed to improve vaccination coverage and confidence in underserved communities, such as younger and lower income racial/ethnic minority groups. Efforts to reduce disparities and barriers to vaccination are needed to achieve equity in vaccination coverage, and ultimately, to curb COVID-19 transmission.
Keywords: COVID-19 vaccination, Vaccine confidence, Vaccine hesitancy, Race, Ethnicity, Disparities
1. Introduction
COVID-19 morbidity and mortality has disproportionately affected vulnerable populations such as minoritized racial/ethnic groups [1], [2], [3], [4], [5], [6], [7]. Studies have demonstrated disparities in COVID-19 infection, hospitalization, and case fatality by geography, race/ethnicity, age, and sociodemographic characteristics [8], [9], [10], [11]. For example, non-Hispanic (NH) Black and Hispanic populations had more years of life lost before 65 years due to COVID-19 than NH White populations [10]. Black populations also had higher age-standardized incidence and mortality rates than White populations [4]. In addition, neighborhoods with higher proportions of racial/ethnic minorities and/or those living in poverty have higher infection and death rates from COVID-19 than neighborhoods that have less racially/ethnically diverse populations and lower poverty levels [10].
Reasons for elevated risk of COVID-19 infection, morbidity and mortality among racial/ ethnic minority groups are varied. First, these populations are more likely to live in crowded conditions and densely populated neighborhoods of lower sociodemographic status and in multigenerational households [5], [6]. They are also more likely to rely on public transportation and have jobs or live with others that have jobs that cannot be performed remotely, such as transit workers, grocery store clerks, nursing aides, construction workers, and household workers [5], [6] These factors reduce the ability to socially distance and increase the likelihood of exposure to COVID-19 [5], [6].
Moreover, due to other forms of social disadvantage such as chronic stress and inadequate access to healthy diets, these groups are more likely to have underlying comorbidities that are associated with more severe COVID-19 outcomes, such as diabetes, cardiovascular disease, asthma, HIV, and morbid obesity [4], [8]. Lastly, racial and ethnic minority groups also experience disparities related to limited or lack of health insurance, greater barriers to quality healthcare, lower rates of COVID-19 testing early in the pandemic, and food and housing insecurity which increases their risk for COVID-19 infection and greater disease severity [4], [8].
Data from December 2020 to February 2021 demonstrates that NH Black populations were less likely to have received a COVID-19 vaccine and less likely to intend to be vaccinated compared with NH White populations [12], [13], [14]. Compared to all other racial/ethnic groups, NH Black persons had the highest proportion of non-intent to get the vaccine in September 2020 (56.1%) and December 2020 (46.5%), with no significant difference between this time period (−9.6, 95% confidence interval: −20.4 to 1.2), suggesting the need to prioritize improving vaccine confidence in this population [15]. Non-intent to be vaccinated also varied by household income and educational level, age group, sex, region, urbanicity, and health insurance status. Younger age groups, people with lower income and educational attainment, people living in rural areas, and people without health insurance had the lowest level of vaccination intent compared to their respective counterparts [15]. However, it is unclear if and how these variables interact to affect COVID-19 vaccination intent, nationally, as well as by region and state. As the COVID-19 vaccine is now available for all adults, identifying groups and perceptions of those who are least likely to get vaccinated is important for developing targeted messages and strategies to improve vaccination coverage and confidence in those populations, and ultimately, bring an end to the COVID-19 pandemic.
To assess COVID-19 vaccination intent by race/ethnicity, and its possible interaction with annual household income and age, we used data from the Census Bureau’s Household Pulse Survey (HPS), which is a large, nationally representative survey that collects data on COVID-19 vaccination coverage and intent as well as other social and economic characteristics during the pandemic. We examined national, regional, and state estimates for receipt of ≥ 1 dose of the COVID-19 vaccine, intention to vaccinate, and reasons for not vaccinating by sociodemographic characteristics , with stratification by race/ethnicity, income and age group. Identifying disparities in vaccination coverage and intent will lead to actionable interventions and recommendations designed to improve uptake and confidence among these vulnerable populations and the general public.
2. Methods
2.1. Survey design
The Household Pulse Survey (HPS) is a nationally representative household survey that captures approximately 75,000 respondents in each survey cycle [16], [17]. It is conducted by the U.S. Census Bureau to help understand household experiences during the COVID-19 pandemic. The survey design of this study has been published previously [17]. The analyses were conducted from February to April 2021, using six waves of data collection (January 6 to March 29, 2021). The sample size for six survey waves was 459,235 total respondents, with response rates between 6.4% and 7.5% [18]. This study was reviewed by the Tufts University Health Sciences Institutional Review Board and considered not to be human subjects research.
2.2. COVID-19 questions
Beginning on January 6, 2021, the HPS added questions on COVID-19 vaccination coverage, intent, and reasons for not vaccinating. COVID-19 vaccination receipt (≥1 dose) was assessed by the following question: “Have you received a COVID-19 vaccine?” Among unvaccinated adults, intent to be vaccinated was assessed with the following question: “Once a vaccine to prevent COVID-19 is available to you, would you…definitely, probably, probably not, or definitely not get a vaccine.” Among those who did not get vaccinated or did not definitely intend to get vaccinated, respondents were asked reasons for not getting vaccinated: “Which of the following, if any, are reasons that you [probably will/probably won't/definitely won't] get a COVID-19 vaccine.” Response options were: 1) I am concerned about possible side effects of a COVID-19 vaccine, 2) I don't know if a COVID-19 vaccine will work, 3) I don't believe I need a COVID-19 vaccine, 4) I don't like vaccines, 5) My doctor has not recommended it, 6) I plan to wait and see if it is safe and may get it later, 7) I think other people need it more than I do right now, 8) I am concerned about the cost of a COVID-19 vaccine, 9) I don't trust COVID-19 vaccines, 10) I don't trust the government, and 11) Other.
2.3. Sociodemographic variables
Sociodemographic variables assessed were age group, sex, race/ethnicity, educational status, annual household income, insurance status, previous COVID-19 diagnosis, and geographic area (HHS region and state) [19]. Age was categorized as 18–49, 50–64, and ≥ 65 years. Race/ethnicity was categorized as NH White, NH Black, Hispanic, NH Asian, and NH other/multiple race. Educational status was categorized as high school degree or less, some college/college degree, and above college degree. Annual household income was categorized as <$35,000, $35,000–$74,999, and ≥$75,000. Insurance status was defined as having or not having insurance. Previous COVID-19 diagnosis was defined as a “yes” response to the following question: “Has a doctor or other healthcare provider ever told you that you have COVID-19?” Analyses by region, categorized as 10 Health and Human Services regionsn [19], and state were also determined.
2.4. Analysis
To examine vaccination intent by geographic area and race/ethnicity with stratification by income level and age group, data were combined for six waves of data collection from January 6 to March 29, 2021 (1/6–1/18, 1/20–2/1, 2/3–2/15, 2/17–3/1, 3/3–3/15, 3/17–3/29). Because the vaccination intent questions were only asked of those who were not vaccinated, assessing intent over time would show bias as more people got vaccinated (reducing the sample size of those who are asked about intent). To reduce this potential for bias, vaccination intent was assessed among everyone in the sample, including those who were vaccinated. Because the vaccine was not available to everyone from January to March 2021, and in order to examine disparities in vaccination coverage and intent to be vaccinated, vaccination intent was defined as receiving ≥ 1 dose of COVID-19 vaccine or reporting that one would “definitely” be vaccinated in the future since people who definitely intent to be vaccinated would likely be in the vaccinated group had the vaccine been available to them at the time.
Sociodemographic characteristics of the sample population was assessed. Vaccination intent was examined by sociodemographic characteristics and then stratified by race/ethnicity, income, age, and geographic area. Reasons for not getting vaccinated were assessed by race/ethnicity and different levels of vaccination intent (probably, probably not and definitely not). All estimates with relative standard errors greater than 30% were suppressed. Contrast tests for the differences in proportions, comparing each category to the referent category were conducted with a 0.05 significance level (α = 0.05). A logistic regression model was estimated to examine the interaction between race/ethnicity and annual household income on COVID-19 vaccination receipt (≥1 dose) and intent to get vaccinated, after controlling for age group, sex, educational status, HHS region, survey cycle, and prior COVID-19 diagnosis. A separate logistic regression model was estimated to examine the interaction between race/ethnicity and age group, adjusting for the same set of covariates. Adjusted Wald tests were used to assess overall interaction terms. All analyses accounted for the survey design to ensure a nationally representative sample using Stata version 16.1.
3. Results
Approximately 52% of respondents were 18–49 years, 26% are 50–64 years, and 22% are over 65 years (Table 1 ). The majority of respondents were female (52%), NH White (63%), have at least some college education (61%), have annual household incomes of ≥$75,000 (57%), and are insured (92%). Fourteen percent of respondents reported having a prior diagnosis of COVID-19. Overall, vaccination intent was highest among NH Asians (78.3%; 95% confidence interval (CI): 77.4–79.3), and lowest among NH Blacks (50.4; 95% CI: 49.5–51.4). Across all sociodemographic characteristics, vaccination intent was lowest among NH Blacks and NH other racial groups (Table 2 ). This trend was particularly strong among those with lower income levels (Table 2). Vaccination intent was also lower among those who had a previous COVID-19 diagnosis or were not sure if they had a previous diagnosis of COVID-19 compared to those who have not, with the lowest intent among NH Blacks (30.2%) compared to NH Whites (51.2%) among those who were not sure if they had a previous COVID-19 diagnosis.
Table 1.
Sociodemographic characteristics, United States, Household Pulse Survey, January 6 – March 29, 2021.
| % (95% CI) | |
|---|---|
| Total (n) | 459,235 |
| Age groups (y) | |
| 18–49 | 52.3 (52.2, 52.4) |
| 50–64 | 26.0 (25.8, 26.1) |
| ≥65 | 21.7 (21.7, 21.8) |
| Sex | |
| Male | 48.4 (48.4, 48.4) |
| Female | 51.6 (51.6, 51.6) |
| Race/ethnicity | |
| NH White | 62.5 (62.5, 62.6) |
| NH Black | 11.4 (11.4, 11.5) |
| Hispanic | 17.1 (17.0, 17.2) |
| NH Asian | 5.3 (5.2, 5.4) |
| NH Other | 3.6 (3.5, 3.7) |
| Education | |
| High school or less | 39.2 (39.2, 39.2) |
| Some college or college graduate | 47.7 (47.6, 47.8) |
| Above college graduate | 13.1 (13.0, 13.2) |
| Annual household income | |
| <$35,000 | 19.3 (19.1, 19.6) |
| $35,000 to <$75,000 | 23.3 (23.1, 23.5) |
| ≥$75,000 | 57.4 (57.1, 57.7) |
| Insurance status | |
| Insured | 91.7 (91.5, 92.0) |
| Not insured | 8.3 (8.0, 8.5) |
| Previous COVID-19 diagnosis | |
| Yes | 14.0 (13.8, 14.2) |
| No | 85.0 (84.8, 85.2) |
| Not sure | 1.0 (1.0, 1.1) |
Table 2.
COVID-19 vaccination intent* by race/ethnicity and sociodemographic characteristics, United States, Household Pulse Survey, January 6 – March 29, 2021
|
Weighted % (95% CI) |
|||||
|---|---|---|---|---|---|
| NH White (N = 343,698) | NH Black (N = 33,301) | Hispanic (N = 44,303) | NH Asian (N = 21,955) | NH Other/multiple races (N = 15,978) | |
| All adults (≥18 y) | 66.8 (66.5–67.1) | 50.4 (49.5–51.4)† | 60.8 (60.0–61.6)† | 78.3 (77.4–79.3)† | 53.8 (52.4–55.2)† |
| Age groups (y) | |||||
| 18–49 | 57.2 (56.7–57.7) | 36.5 (35.4–37.7)† | 54.4 (53.4–55.5)† | 74.4 (72.8–75.9)† | 47.9 (46.1–49.7)† |
| 50–64 | 66.4 (65.8–66.9) | 60.3 (58.4–62.2)† | 70.5 (68.8–72.1)† | 81.6 (80.0–83.2)† | 56.8 (54.0–59.6)† |
| ≥65 | 84.2 (83.7–84.7) | 78.2 (75.8–80.5)† | 78.0 (76.0–79.9)† | 90.3 (88.6–92.0)† | 71.9 (68.2–75.6)† |
| Sex | |||||
| Male | 66.3 (65.8–66.8) | 55.3 (53.7–56.9)† | 63.3 (61.8–64.7)† | 77.3 (75.6–79.0)† | 53.8 (51.4–56.2)† |
| Female | 67.2 (66.8–67.7) | 46.6 (45.4–47.8)† | 58.3 (57.3–59.3)† | 79.4 (78.0–80.8)† | 53.8 (51.8–55.8)† |
| Education | |||||
| High school or less | 55.9 (55.2–56.5) | 45.3 (43.4–47.1)† | 57.1 (55.8–58.4) | 70.5 (68.0–72.9)† | 44.2 (41.2–47.1)† |
| Some college or college graduate | 68.7 (68.4–69.1) | 51.5 (50.3–52.7)† | 63.4 (62.3–64.5)† | 78.0 (76.6–79.4)† | 57.6 (55.8–59.3)† |
| Above college graduate | 86.2 (85.8–86.7) | 66.0 (64.1–67.9)† | 77.1 (75.3–79.0)† | 87.1 (86.0–88.3) | 74.1 (71.4–76.7)† |
| Annual household income | |||||
| <$35,000 | 58.0 (57.0–58.9) | 41.5 (39.5–43.5)† | 54.9 (53.1–56.7)† | 72.8 (69.7–75.8)† | 46.1 (42.7–49.6)† |
| $35,000 to <$75,000 | 65.5 (65.0–66.0) | 51.7 (49.7–53.7)† | 63.6 (61.4–65.8) | 76.1 (73.4–78.7)† | 55.1 (51.7–58.5)† |
| ≥$75,000 | 74.7 (74.3–75.1) | 65.8 (64.0–67.7)† | 69.4 (68.0–70.8)† | 83.3 (81.7–84.9)† | 64.1 (61.1–67.1)† |
| Insurance status | |||||
| Insured | 69.9 (69.6–70.3) | 54.0 (52.8–55.1)† | 64.0 (62.7–65.3)† | 80.7 (79.6–81.8)† | 58.1 (56.3–59.9)† |
| Not insured | 42.6 (40.7–44.6) | 33.5 (30.1–36.9)† | 51.6 (49.1–54.2)† | 57.4 (52.7–62.0)† | 37.5 (32.8–42.2)† |
| Previous COVID-19 diagnosis | |||||
| Yes | 55.4 (54.5–56.4) | 46.4 (43.6–49.2)† | 59.1 (57.1–61.0)† | 78.3 (74.7–81.8)† | 47.7 (43.4–52.1)† |
| No | 68.4 (68.1–68.8) | 51.3 (50.3–52.3)† | 61.8 (60.8–62.7)† | 78.9 (77.9–80.0)† | 55.2 (53.6–56.8)† |
| Not sure | 51.2 (47.2–55.1) | 30.2 (20.5–40.0)† | 42.5 (36.2–48.8)† | 55.6 (43.0–68.3) | 36.8 (25.8–47.9)† |
Abbreviations: NH = non-Hispanic; COVID-19 = coronavirus disease 2019; CI = confidence interval.
Vaccination intent is defined as receiving ≥ 1 dose of COVID-19 vaccine or definitely will get vaccinated.
Significant differences in proportions comparing each group to the referent group (non-Hispanic white individuals).
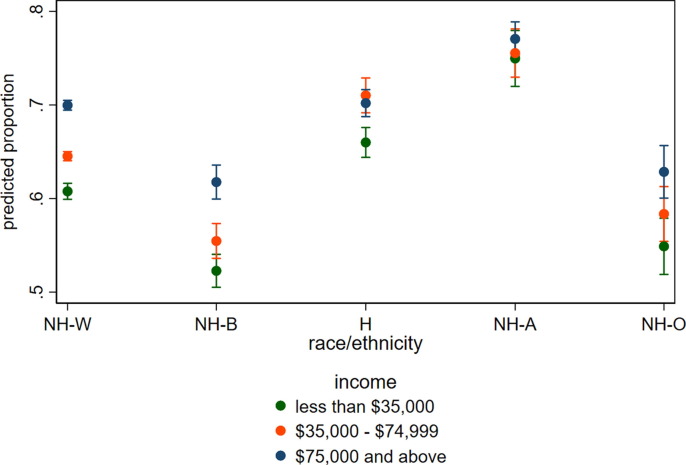
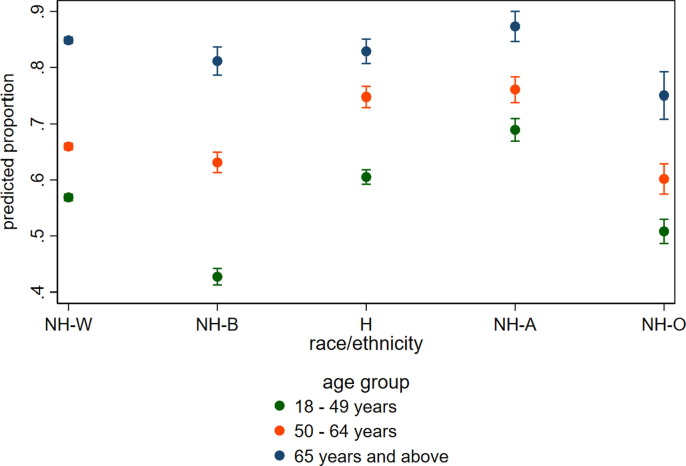
In multivariable models, a significant interaction was observed between race/ethnicity and income (Fig. 1 ; F(8,72) = 4.50, p < 0.001)), as well as between race/ethnicity and age group (Fig. 2 ; F(8,72) = 15.66, p < 0.001)). NH Black and NH other/multiple racial groups had the lowest proportion of adults intending to get vaccinated across all income levels, and the effect of income was smaller among NH Asian and Hispanic adults (Fig. 1). For example, the difference in the predicted probability of intent to vaccinate between NH Black individuals at the highest income level compared to the lowest income level was 9.5 percentage points (61.8% versus 52.3%) whereas the difference in the predicted probability of intent to vaccinate between NH Asian individuals at the highest income level compared to the lowest income level was 2.1 percentage points (77.1% versus 75.0%). Furthermore, people aged 18–49 years were less likely to intend to get vaccinated than people aged 65 years and older; however, the differences by age group depended on individuals’ racial/ethnic group (Fig. 2). For example, the difference in the predicted probability of intent to vaccinate between the oldest age group of NH Blacks compared to the youngest was larger than that for any other racial/ethnic group (38.4 percentage points for NH Blacks versus 28.0 percentage points for NH Whites, 24.2 percentage points for NH other/multiple racial groups, 22.4 percentage points for Hispanics, and 18.4 percentage points for NH Asians). This interaction partially reflects the low predicted probability of intent to vaccinate among people aged 18–49 years who identified as NH Black (42.7%, 95% CI = 41.2%, 44.2%).
Fig. 1.
Predicted proportion of vaccination intent by racial/ethnic and income group, United States, January 6 - March 29, 2021. Abbreviations: NH-W = Non-Hispanic White; NH-B = Non-Hispanic Black; H = Hispanic; NH-A = Non-Hispanic Asian, NH-O = Non-Hispanic other/multiple race category.
Fig. 2.
Predicted proportion of vaccination intent by racial/ethnic and age group, United States, January 6 - March 29, 2021. Abbreviations: NH-W = Non-Hispanic White; NH-B = Non-Hispanic Black; H = Hispanic; NH-A = Non-Hispanic Asian, NH-O = Non-Hispanic other/multiple race category.
All inter- and intra-group comparisons were statistically significant (p < 0.05) with the following exceptions: among people with intermediate incomes, there were no significant differences between people who identify as Hispanic and NH White (p = 0.008) or between people who identify as NH Black and NH other (p = 0.117) (Fig. 1). Among people in the oldest age group, there were no significant differences between people who identify as Hispanic or NH Black (p = 0.902) (Fig. 2). There were no significant differences between people in the middle and highest income groups who identified as NH Black (p = 0.054), Hispanic (p = 0.342), or NH other (p = 0.456). Finally, there were no significant differences between people in the lowest and middle income groups who identified asNH Asian (p = 0.129).
Vaccination intent differed by racial/ethnic group, household income, and age group, overall and by geographic area. Nationally, among people with an annual household income of <$35,000, intent was lowest among NH Black (41.5%) and NH other/multiple racial groups (46.1%) (Supplemental Table 1). By region, NH Black populations and NH other/multiple racial groups with incomes <$35,000 have the lowest intent in HHS region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) (37.0%) and HHS region 4 (Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee) (31.8%), respectively. Across states with non-suppressed estimates, intent was lowest among NH Black adults with incomes <$35,000 in Ohio (28.8%), while it was lowest for NH other/multiple racial groups with incomes <$35,000 in Florida (24.7%). By age group, vaccination intent was lowest among younger NH Black (36.5%) and NH other/multiple racial groups (47.9%) (18–49 years) (Supplemental Table 2). Among NH Black and NH other/multiple racial groups aged 18–49 years, vaccination intent was lowest in HHS region 4 (33.1% and 34.8%, respectively) (Supplemental Table 2). Across state with non-suppressed estimates, intent was lowest among NH Black and NH other/multiple racial groups aged 18–49 years in Iowa (22.1%) and Florida (25.8%), respectively.
Reasons for not getting vaccinated differed by race/ethnic group (Table 3 ). Among those who probably will get vaccinated, concerns about possible side effects and effectiveness were significantly higher among all race/ethnic minority groups compared to NH White adults. For example, concerns about possible side effects ranged from 51.8% to 57.5% among minority groups compared to 49.5% among NH White adults. Furthermore, concerns about effectiveness of the vaccine ranged from 18.7% to 21.2% among minority groups compared to 16.3% among NH White adults. Among those who will probably not get vaccinated, lack of trust in the vaccine was higher among NH Blacks (28.5%) compared to NH Whites (24.2%), and concerns about the cost was higher among NH other/multiple racial groups (7.3%) compared to NH Whites (5.3%). Among adults who will definitely not get vaccinated, lack of doctor recommendation (9.8%) and other reasons for not getting vaccinated (29.5%) were higher among NH other/multiple racial groups than NH Whites (6.8% and 17.6%, respectively). Furthermore, 30% of NH other/multiple racial groups who said they would definitely not get vaccinated reported other reasons for not getting vaccinated, which is higher than seen among NH Whites (18%), suggesting there may be other reasons for non-vaccination among these groups. While not specifically stated, other reasons for not getting vaccinated may include access and logistical issues, such as time and transportation.
Table 3.
Reasons for not getting the COVID-19 vaccine by categories of vaccination intent, United States, Household Pulse Survey, January 6 – March 29, 2021
|
% (95% CI) |
|||||
|---|---|---|---|---|---|
| Non-Hispanic (NH) White (N = 82,460) | NH Black (N = 13,518) | Hispanic or Latino (N = 14,342) | NH Asian (N = 3,906) | NH Other/Multiple Races (N = 5,992) | |
| Would probably get vaccinated | |||||
| Concerned about possible side effects | 49.5 (48.7–50.4) | 52.8 (50.8–54.7)* | 51.8 (49.8–53.9)* | 58.1 (54.7–61.5)* | 57.5 (54.2–60.9)* |
| Don’t know if a vaccine will work | 16.3 (15.7–16.9) | 19.2 (17.3–21.0)* | 18.7 (16.9–20.6)* | 19.0 (16.6–21.3)* | 21.2 (18.0–24.4)* |
| Don’t believe I need a vaccine | 5.2 (4.7–5.6) | 3.9 (2.6–5.2) | 2.9 (2.2–3.6)* | 3.6 (2.3–5.0)* | 6.0 (4.1–8.0) |
| Don’t like vaccines | 4.9 (4.5–5.2) | 5.1 (4.4–5.9) | 5.0 (4.2–5.8) | 4.2 (2.5–5.9) | 6.6 (4.6–8.6) |
| Doctor has not recommended it | 7.0 (6.5–7.5) | 8.4 (7.1–9.7)* | 5.7 (4.7–6.7)* | 3.8 (2.7–4.9)* | 10.1 (8.2–12.0)* |
| Plan to wait and see if it is safe and may get it later | 52.6 (51.7–53.6) | 63.0 (60.6–65.3)* | 54.8 (52.5–57.0) | 61.8 (58.6–65.1)* | 58.2 (54.9–61.4)* |
| Other people need it more right now | 43.5 (42.7–44.4) | 21.1 (18.8–23.3)* | 33.9 (32.2–35.7)* | 37.1 (33.6–40.6)* | 38.9 (35.3–42.4)* |
| Concerned about the cost | 10.0 (9.4–10.5) | 8.6 (7.3–10.0) | 13.9 (12.1–15.8)* | 12.2 (10.1–14.2)* | 15.2 (12.2–18.3)* |
| Don’t trust COVID-19 vaccines | 7.1 (6.5–7.6) | 12.2 (10.7–13.6)* | 7.8 (6.7–8.9) | 6.3 (4.9–7.7) | 12.2 (9.9–14.5)* |
| Don’t trust the government | 11.1 (10.6–11.6) | 11.6 (10.3–12.8) | 8.3 (7.4–9.2)* | 3.6 (2.5–4.7)* | 13.7 (11.1–16.4) |
| Other reason for not getting vaccine | 9.2 (8.8–9.7) | 5.9 (5.0–6.9)* | 5.4 (4.7–6.1)* | 5.1 (3.9–6.4)* | 10.2 (8.0–12.3) |
| Would probably not get vaccinated | |||||
| Concerned about possible side effects | 51.7 (50.7–52.8) | 53.5 (51.5–55.6) | 52.0 (49.3–54.8) | 51.1 (44.8–57.3) | 57.2 (52.9–61.5)* |
| Don’t know if a vaccine will work | 21.8 (20.9–22.8) | 19.7 (17.3–22.1) | 23.3 (20.8–25.8) | 25.6 (19.6–31.6) | 25.0 (21.5–28.6) |
| Don’t believe I need a vaccine | 20.2 (19.0–21.3) | 8.9 (7.3–10.6)* | 13.9 (11.7–16.1)* | 9.3 (6.6–12.1)* | 18.6 (15.6–21.7) |
| Don’t like vaccines | 9.8 (9.0–10.5) | 9.9 (8.4–11.3) | 7.9 (6.2–9.6)* | 10.8 (6.8–14.8) | 18.2 (13.9–22.5)* |
| Doctor has not recommended it | 7.4 (6.7–8.2) | 7.1 (5.8–8.4) | 6.6 (5.1–8.1) | 3.2 (1.8–4.7)* | 8.7 (6.4–11.0) |
| Plan to wait and see if it is safe and may get it later | 57.2 (56.2–58.2) | 59.0 (56.7–61.2) | 55.7 (52.1–59.2) | 59.7 (53.2–66.1) | 55.2 (50.9–59.4) |
| Other people need it more right now | 29.5 (28.3–30.7) | 18.3 (16.3–20.4)* | 24.9 (22.1–27.6)* | 26.2 (21.6–30.8) | 26.9 (23.3–30.5) |
| Concerned about the cost | 5.3 (4.8–5.8) | 4.7 (3.7–5.7) | 9.6 (7.4–11.8)* | 6.6 (3.1–10.2) | 7.3 (5.3–9.4)* |
| Don’t trust COVID-19 vaccines | 24.2 (23.1–25.2) | 28.5 (26.0–30.9)* | 24.2 (21.9–26.5) | 14.9 (11.0–18.8)* | 24.6 (21.5–27.8) |
| Don’t trust the government | 20.4 (19.7–21.2) | 19.3 (17.4–21.2) | 17.7 (15.3–20.1)* | 9.3 (6.3–12.4)* | 21.5 (18.7–24.3) |
| Other reason for not getting vaccine | 10.4 (9.8–11.0) | 7.2 (6.1–8.3)* | 9.3 (7.4–11.2) | 11.9 (7.2–16.6) | 13.4 (10.6–16.3)* |
| Would definitely not get vaccinated | |||||
| Concerned about possible side effects | 48.4 (47.0–49.8) | 48.2 (44.8–51.5) | 44.7 (40.4–49.0) | 35.4 (25.6–45.1)* | 50.3 (46.1–54.5) |
| Don’t know if a vaccine will work | 22.4 (21.3–23.6) | 24.0 (20.6–27.5) | 24.2 (20.4–28.0) | 19.4 (12.5–26.3) | 26.6 (21.8–31.4) |
| Don’t believe I need a vaccine | 35.7 (34.3–37.2) | 20.3 (17.9–22.7)* | 29.8 (26.0–33.6)* | 34.3 (24.6–44.1) | 31.5 (27.6–35.4) |
| Don’t like vaccines | 19.4 (18.1–20.6) | 20.6 (17.8–23.4) | 18.0 (15.0–20.9) | 16.1 (9.7–22.4) | 21.3 (17.7–25.0) |
| Doctor has not recommended it | 6.8 (6.1–7.6) | 6.6 (5.4–7.7) | 4.8 (3.6–6.1)* | † | 9.8 (7.0–12.6)* |
| Plan to wait and see if it is safe and may get it later | 20.7 (19.7–21.6) | 25.6 (22.9–28.4)* | 23.8 (21.0–26.7)* | 18.8 (11.1–26.6) | 22.3 (18.8–25.7) |
| Other people need it more right now | 13.0 (12.1–13.8) | 10.2 (8.0–12.4)* | 12.3 (9.5–15.1) | 16.7 (8.5–25.0) | 14.4 (10.9–17.8) |
| Concerned about the cost | 3.3 (2.6–3.9) | 3.8 (2.5–5.0) | 4.6 (3.4–5.7) | † | 4.2 (2.2–6.2) |
| Don’t trust COVID-19 vaccines | 50.3 (48.9–51.7) | 49.9 (46.9–53.0) | 43.0 (39.5–46.4)* | 36.2 (25.5–46.9)* | 50.7 (46.5–54.9) |
| Don’t trust the government | 41.8 (40.5–43.1) | 32.4 (29.4–35.4)* | 38.9 (35.2–42.6) | 31.1 (20.5–41.6) | 46.1 (41.5–50.6) |
| Other reason for not getting vaccine | 17.6 (16.7–18.4) | 10.3 (8.4–12.2)* | 21.4 (18.4–24.5)* | 24.4 (15.8–32.9) | 29.5 (26.2–32.9)* |
Abbreviations: NH = non-Hispanic; COVID-19 = coronavirus disease 2019; CI = confidence interval.
Significant differences in proportions comparing each group to the referent group (non-Hispanic white individuals).
Estimate was suppressed due to a relative standard error of >30%.
4. Conclusion and discussion
Vaccination intent varies by sociodemographic characteristics and geographic areas across all racial/ethnic groups. Prior studies have shown that people with lower sociodemographic status, younger age, and are NH Black were less likely to get vaccinated or intend to get vaccinated [20], [12], [13], [14], [15]. However, this is the first nationally representative study to show that vaccination intent differs by income and age group within racial/ethnic groups. Furthermore, the interaction between race/ethnicity and income and age group were found across most HHS regions and states. While this study provides data in early 2021 on the start of the vaccination campaign, data from more recent surveys suggest that disparities in vaccination coverage and intent by age and race/ethnicity continue to exist but are closing for some race groups [21], [22]. Intention to vaccinate was lowest among NH Blacks and NH other/multiple racial groups with incomes <$35,000 and between ages 18–49 years, with lower levels of intent to vaccinate across each income and age group compared to their respective NH White counterparts. While this study only examined vaccination coverage and intent among adults, studies have found that vaccination and intent among parents arehighly correlated with their willingness to vaccinate their children ages 12–17 years, for which the Pfizer-BioNTech vaccine has been approved. As a result, gaps and disparities in vaccination coverage and intent among adults are likely to be similar among adolescent children as well, highlighting the importance of addressing the disparities found in this study.
This study demonstrates that the most vulnerable populations are NH Black and NH other/multiple racial groups, particularly those who are younger and have lower incomes. Although the vaccine is free for everyone in the U.S., adults of every racial/ethnic group mentioned cost as a barrier to vaccination (though more frequently in adults of NH other/multiple races than NH white adults). This suggests the need to clarify misinformation about the cost of the vaccines and emphasize the availability of the vaccines for all. Beyond this misperception about cost, however, even among those with the highest incomes, intent among NH Blacks and NH other/multiple racial groups are still much lower than those of NH Whites of similar incomes, suggesting ongoing reasons for vaccine hesitancy beyond simply access or misperception barriers in these populations. We find that concerns about possible vaccine side effects and effectiveness, lack of recommendation from a health care provider, and lack of trust in COVID-19 vaccines were significantly higher among NH Blacks and/or NH other/multiple racial groups compared to NH White adults. Indeed, other research identifies trust—and specifically, trust in science and medicine, which is lower among NH Black and Hispanic individuals than NH Whites and Asians—as a major predictor of vaccine hesitancy even after adjusting for a range of predictors including partisanship, ideology, education, income and region [22]. The history of racism in the US, which research has previously been found to be associated with a lack of trust in influenza vaccines, is likely also in play with the COVID-19 vaccine in these communities [23], [24]. Furthermore, 30% of NH other/multiple racial groups who said they would definitely not get vaccinated reported other reasons for not getting vaccinated, which is higher than seen among NH Whites (18%), reinforcing the notion that the determinates of trust in vaccines are complex and operate differently in different racial/ethnic communities.
Our results reinforce the recognized importance of strategies for reducing COVID-19 vaccine hesitancy and increasing trust in these populations through community-sensitive messages from trusted sources about the safety and effectiveness of vaccines, ensuring that healthcare providers are recommending (or having discussions about the importance of) vaccination, and addressing access barriers to vaccination by having vaccines available in convenient locations [26], [27], [28], [25].
This study also demonstrates high vaccination intent among NH Asian adults compared to NH White adults. A lower proportion of NH Asians reported that they did not believe they needed a vaccine and did not trust the government compared to NH Whites. NH Asian adults were also less likely to report lack of trust in COVID-19 vaccines compared to NH Black and Hispanic adults. These results suggest that perceived need and confidence in vaccines and trust in the government may be contributing factors to the higher vaccination coverage and intent among this group. Understanding motivators for vaccination, such as protecting the health of families and communities and resuming work, school, and social activities, is also important for developing appropriate strategies and interventions to increase vaccination coverage among all populations. Emphasizing the importance of vaccines in protecting one’s health and that of loves ones, as well as building trust in vaccines and the health professionals who recommend them, will help contribute to improving vaccination coverage and confidence among all racial/ethnic groups.
The findings in this study are subject to several limitations. First, COVID-19 vaccination status and diagnosis were based on self-report, which may not accurately reflect actual vaccination status or disease history for some respondents. Second, the HPS has a low response rate (<10%); however, non-response bias assessment conducted by the Census Bureau found that the survey weights adjusted for most of this bias, even though some bias may remain [29]. Finally, because data from January to March 2021 were used in this analysis, these results might not be reflective of the current prevalence of vaccine confidence. However, patterns in vaccination intent disparities by race/ethnicity, income, and age group are likely to be similar.
Disparities in vaccine confidence by racial/ethnic groups underscore the need for targeted interventions and messages to reach vulnerable communities, such as younger and lower income racial/ethnic minority groups, many of which are experiencing a disproportionate burden of COVID-19 infections and deaths. Despite the vaccine being available to everyone for free, over 25% of all adults in the U.S. have not received at least 1 dose of the COVID-19 vaccine as of August 2021 [30]. Understanding more about the reasons for ongoing levels of hesitancy and other access barriers to vaccination will lead to actionable interventions and recommendations designed to improve vaccination coverage and confidence, particularly among communities who are most vulnerable to COVID-19 infection and severe health outcomes. Efforts to reduce disparities and barriers to vaccination, and increase public trust and confidence, are needed to achieve equity in vaccination coverage.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
Laura Corlin was supported by Eunice Kennedy Shriver National Insti tute of Child Health & Human Development (NICHD) grant number K12HD092535 and by the Tufts University/Tufts Medical Centre Rapid Response Seed Funding Program.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.11.040.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Health Equity Data. Centers for Disease Control and Prevention. Available at: https://covid.cdc.gov/covid-data-tracker/#health-equity-data.
- 2.Gold J.A.W., Rossen L.M., Ahmad F.B., Sutton P., Li Z., Salvatore P.P., et al. Race, ethnicity, and age trends in persons who died from COVID-19—United States, May–August 2020. Morb Mortal Wkly Rep. 2020;69(42):1517–1521. doi: 10.15585/mmwr.mm6942e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cowger T.L., Davis B.A., Etkins O.S., Makofane K., Lawrence J.A., Bassett M.T., et al. Comparison of weighted and unweighted population data to assess inequities in coronavirus disease 2019 deaths by race/ethnicity reported by the US Centers for Disease Control and Prevention. JAMA Network Open. 2020;3(7):e2016933. doi: 10.1001/jamanetworkopen.2020.16933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mackey K., Ayers C.K., Kondo K.K., Saha S., Advani S.M., Young S., et al. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths: A systematic review. Ann Intern Med. 2021;174(3):362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hooper M.W., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020 Jun 23;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez L., Hart L.H., Katz M.H. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325(8):719. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- 7.Razai M.S., Kankam H.K., Majeed A., Esmail A., Williams D.R. Mitigating ethnic disparities in covid-19 and beyond. BMJ. 2021;372 doi: 10.1136/bmj.m4921. [DOI] [PubMed] [Google Scholar]
- 8.Gross C.P., Essien U.R., Pasha S., Gross J.R., Wang S.-y., Nunez-Smith M. Racial and ethnic disparities in population-level Covid-19 mortality. J Gen Intern Med. 2020;35(10):3097–3099. doi: 10.1007/s11606-020-06081-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baack BN, Abad N, Yankey D, Kahn, K, Razzaghi, H, Brookmeyer, K, Kolis, J, Wilhelm, E, Nguyen, KH, Singleton, J. COVID-19 Vaccination Coverage and Intent Among Adults Aged 18–39 Years — United States, March–May 2021. MMWR Morb Mortal Wkly Rep. ePub: 21 June 2021. http://dx.doi.org/10.15585/mmwr.mm7025e2. [DOI] [PMC free article] [PubMed]
- 10.Bassett M.T., Chen J.T., Krieger N. Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: A cross-sectional study. PLoS Med. 2020;17(10):e1003402. doi: 10.1371/journal.pmed.1003402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adhikari S., Pantaleo N.P., Feldman J.M., Ogedegbe O., Thorpe L., Troxel A.B. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Network Open. 2020 Jul 1;3(7):e2016938. doi: 10.1001/jamanetworkopen.2020.16938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Painter E.M., Ussery E.N., Patel A., Hughes M.M., Zell E.R., Moulia D.L., et al. Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program—United States, December 14, 2020–January 14, 2021. Morb Mortal Wkly Rep. 2021;70(5):174–177. doi: 10.15585/mmwr.mm7005e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kriss J.L., Reynolds L.E., Wang A., Stokley S., Cole M.M., Harris L.Q., et al. COVID-19 Vaccine Second-Dose Completion and Interval Between First and Second Doses Among Vaccinated Persons—United States, December 14, 2020− February 14, 2021. Morb Mortal Wkly Rep. 2021;70(11):389–395. doi: 10.15585/mmwr.mm7011e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Census Bureau Household Pulse Survey's COVID-19 Vaccination Coverage Tracker - available at https://www.census.gov/library/visualizations/interactive/household-pulse-survey-covid-19-vaccination-tracker.html.
- 15.Nguyen, K.H., Srivastav, A., Razzaghi, H., Williams, W., Lindley, M.C., Jorgensen, C., Abad, N. and Singleton, J.A., 2021. COVID‐19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, September and December 2020. [DOI] [PMC free article] [PubMed]
- 16.Household Pulse Survey. Census Bureau. Available at: https://www.census.gov/data/experimental-data-products/household-pulse-survey.html.
- 17.Fields JF, Hunter-Childs J, Tersine A, Sisson J, Parker E, Velkoff V, Logan C, and Shin H. Design and Operation of the 2020 Household Pulse Survey, 2020. U.S. Census Bureau. Available at: https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/2020_HPS_Background.pdf.
- 18.Source of the Data and Accuracy of the Estimates for the Household Pulse Survey. Census Bureau. Available at: https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/Phase3_Source_and_Accuracy_Week_27.pdf.
- 19.Regional offices. Health and Human Services. Available at: https://www.hhs.gov/about/agencies/iea/regional-offices/index.html.
- 20.Nguyen, KH., Nguyen, KC., Corlin, L., Allen, J., Chung, M. Trends in COVID-19 vaccination and intent, by socioeconomic characteristics and geographic area, adults ≥ 18 years, United States, January 6 – March 29, 2021. Ann Med.; 53(1): 1419–1428. [DOI] [PMC free article] [PubMed]
- 21.Latest Data on COVID-19 Vaccinations by Race/Ethnicity. KFF. https://www .kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/.
- 22.Kazemian S., Fuller S., Algara C. The role of race and scientific trust on support for COVID-19 social distancing measures in the United States. PLoS One. 2021 Jul 9;16(7) doi: 10.1371/journal.pone.0254127. PMID: 34242275; PMCID: PMC8270185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crouse Quinn S., Jamison A.M., Freimuth V.S., An J., Hancock G.R. Determinants of influenza vaccination among high-risk Black and White adults. Vaccine. 2017 Dec 18;35(51):7154–7159. doi: 10.1016/j.vaccine.2017.10.083. Epub 2017 Nov 7. PMID: 29126805; PMCID: PMC5712242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freimuth V.S., Jamison A.M., An J., Hancock G.R., Quinn S.C. Determinants of trust in the flu vaccine for African Americans and Whites. Soc Sci Med. 2017 Nov;193:70–79. doi: 10.1016/j.socscimed.2017.10.001. Epub 2017 Oct 4. PMID: 29028558; PMCID: PMC5706780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trends in COVID-19 Vaccine Confidence in the US. Centers for Disease Control and Prevention. Available at https://covid.cdc.gov/covid-data-tracker/#vaccine-confidence.
- 26.Marquez C., Kerkhoff A.D., Naso J., Contreras M.G., Castellanos Diaz E., Rojas S., Peng J., Rubio L., Jones D., Jacobo J., Rojas S., Gonzalez R., Fuchs J.D., Black D., Ribeiro S., Nossokoff J., Tulier-Laiwa V., Martinez J., Chamie G., Pilarowski G., DeRisi J., Petersen M., Havlir D.V. A multi-component, community-based strategy to facilitate COVID-19 vaccine uptake among Latinx populations: From theory to practice. PLoS One. 2021 Sep 20;16(9) doi: 10.1371/journal.pone.0257111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feifer R.A., Bethea L., White E.M. Racial Disparities in COVID-19 Vaccine Acceptance: Building Trust to Protect Nursing Home Staff and Residents. J Am Med Dir Assoc. 2021 Sep;22(9):1853–1855.e1. doi: 10.1016/j.jamda.2021.07.006. Epub 2021 Jul 21. PMID: 34375655; PMCID: PMC8292109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allen J.D., Feng W., Corlin L., Porteny T., Acevedo A., Schildkraut D., et al. Why are some people reluctant to be vaccinated for COVID-19? A cross-sectional survey among US Adults in May-June 2020. Preventive Medicine Reports. 2021;24:101494. doi: 10.1016/j.pmedr.2021.101494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nonresponse Bias Report for the 2020 Household Pulse Survey. Census Bureau. Available at: https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/2020_HPS_NR_Bias_Report-final.pdf.
- 30.COVID-19 Vaccinations in the United States. Centers for Disease Control and Prevention. Available at: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.