Abstract
Objectives
Measurement of food insecurity in older adults is focused on financial barriers to food access. Given that older adults are particularly susceptible to additional access-related barriers including functional limitations and lack of social support, the objective of this study was to construct a summary indicator of food insecurity incorporating these domains.
Methods
We used nationally representative survey data from Round 5 of the National Health and Aging Trends Study (NHATS; n = 7,070). We constructed a summary indicator of food insecurity using factors within the following three domains: functional, social support, and financial limitations. First, we identified the prevalence of food insecurity among the sample as defined by the new summary indicator. Then, we estimated unadjusted and adjusted logistic regression models to assess the association between the expanded measure of food insecurity and biopsychosocial factors.
Results
In 2015, 4.3% (95% confidence interval [CI] 3.75–4.94) of community-dwelling older adults, approximately 1,673,775 million people, were characterized as having food insecurity. Multivariable-adjusted regression models identified that being homebound (odds ratio [OR] 3.49, 95% CI 2.03, 6.00), frail (OR 9.50, 95% CI 4.92–18.37), and experiencing community disability (OR 5.19, 95% CI 3.90–6.90) was associated with food insecurity.
Discussion
Food insecurity among older adults is broader than lacking adequate financial resources to obtain food; it is also associated with social and functional limitations. A more comprehensive conceptualization will aid future study on the impact of food insecurity on health status, utilization, and outcomes to inform senior nutrition program targeting and services.
Keywords: Functional health status, Measurement, Nutrition, Social support
Adults aged 65 years and older are a rapidly increasing segment of the population, which is projected to represent roughly one in six Americans by the year 2060 (Mather et al., 2015). As many Americans age on fixed incomes, they face increased constraints on their ability to afford necessary medical care in addition to food, housing, and other basic living expenses (U.S. Committee on Aging, 1969). Food insecurity is defined by the United States Department of Agriculture (USDA) as a “limited or uncertain availability of nutritionally adequate and safe foods” (Anderson, 1990). Food insecurity is estimated to have more than doubled among American older adults since 2001 (Baker-Lutz et al., 2019). In 2017, 5.5 million older adults (or 7.7%) were food insecure (Baker-Lutz et al., 2019). Food insecurity rates are higher among older adults that experience functional limitations, are homebound, socially isolated, live alone, live in rural/southern geographies, or have multiple comorbidities (Lee & Frongillo, 2001). Therefore, it is imperative to understand the complex role of food insecurity on the lives and health outcomes of older adults.
Food insecurity is strongly associated with poor health outcomes such as worse glycemic control in diabetes (Seligman et al., 2007, 2011), worse depressive symptoms (Siefert et al., 2004), and poor blood pressure control (Seligman & Schillinger, 2010). It also impacts chronic disease management as it leads to reliance on poorer quality foods and forces trade-offs between health care and nutrition, which compromises medication adherence (Afulani et al., 2015; Srinivasan & Pooler, 2018). Importantly, food insecurity is associated with postponing needed medical care and medications, increased emergency department visits, and hospitalizations (Kushel et al., 2006).
Prior work has examined the prevalence of food insecurity among older adults as it relates to specific diseases (e.g., diabetes, peripheral arterial disease, and depression; Melchior et al., 2009; Redmond et al., 2016; Seligman et al., 2007), outcomes (e.g., cost-related nonadherence and health expenditures; Berkowitz et al., 2018; Srinivasan & Pooler, 2018), and in specific geographic regions (e.g., Georgia, California, rural areas, and Boston; Durazo, et al., 2011; Lee et al., 2010; Wong et al., 2016). While there is increasing literature on food insecurity among older adults, measurement has traditionally focused on financial barriers to food access (Ziliak & Gundersen, 2017). The gold standard measure for food insecurity in survey research is the USDA Household Food Security Survey Module (HFSSM) (Coleman-Jensen et al., 2012) scale. It includes the following four household food conditions, events, or behaviors: anxiety about insufficient food budget or supply, perception that food eaten is inadequate in quality or quantity, reduced food intake, and reduced food intake among children (Bickell et al., 2000). This measure focuses on financial constraints and leaves out concepts that influence food insecurity in older populations, such as social support and/or reduced mobility or function (Lee & Frongillo, 2001; Sahyoun & Basiotis, 2000; Wolfe et al., 1996).
Conceptual Framework for Food Insecurity Measurement
To expand the concept of food insecurity within older adults, Wolfe et al. (2003) proposed items to supplement the USDA’s HFSSM. Data gathered from qualitative interviews with 46 older adult households recruited from subsidized housing programs, churches, and meal programs were used to identify a set of 14 functional, transportation, psychological, and social limitations related to food insecurity (Wolfe et al., 2003). Wolfe et al. (2003) used these items to create a measure of food insecurity for older adults validated through quantitative comparison to the HFSSM including an assessment of each item’s performance. Additionally, Goldberg and Mawn (2015) conducted a research to understand the antecedents of food insecurity among older Americans utilizing the social ecological model and the National Health and Nutrition Examination Survey (NHANES). They found that difficulty preparing meals and lack of support were positively associated with increased food insecurity. Motivated by the complexity of food insecurity among older adults beyond age and income, Warren et al. (2020) created a taxonomy of needs for food and food assistance to support program targeting for nutritional outreach effort. By interviewing 147 older adults sampled from 12 food assistance programs across nine states, they created a taxonomy focused on older adult’s ability to access food and nutrition assistance across three domains: physical abilities (e.g., physical strength, ability to prepare food, walk or stand, and health status), consuming food (e.g., preferences, accessibility, affordability, and condition-related dietary needs), and access and use of transportation (Warren et al., 2020).
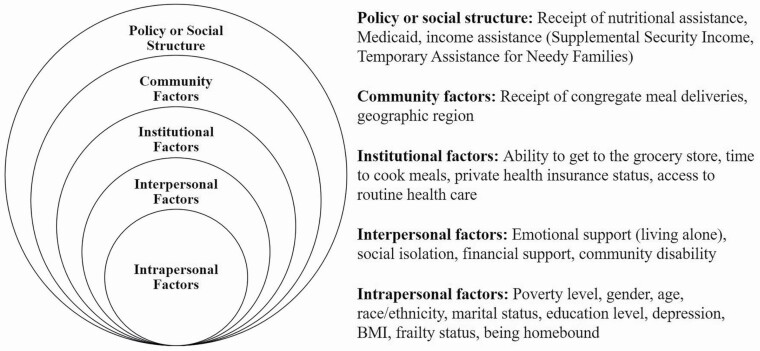
Building on the prior work of Wolfe et al. (2003), Goldberg and Mawn (2015), and Warren et al. (2020), and employing the social ecological model (Figure 1), we posit that food insecurity is influenced by intrapersonal factors (e.g., frailty, high levels of medical comorbidity, and being homebound), interpersonal factors (e.g., living alone and lack of social support), institutional factors (e.g., ability to get to the grocery store, time to cook meals, private health insurance status, and access to routine health care), community factors (e.g., receipt of congregate meal services), and policy or social structures (e.g., receipt of nutritional assistance, Medicaid status, and income assistance) specific to the multidimensional experience of aging (Figure 1; Goldberg & Mawn, 2015). Although validated measures of food insecurity are included in many nationally representative surveys, they focus on financial constraints and do not incorporate factors, such as social support, and/or reduced mobility or function, that are more likely to impact the older adult population (Jackson et al., 2019; Lee & Frongillo, 2001; Sahyoun & Basiotis, 2000; Wolfe et al., 1996). Therefore, we use the social ecological model to establish and test the construct validity of a summary indicator that accounts for this broader conceptualization of food insecurity within the National Health and Aging Trends Study (NHATS), a nationally representative cohort of older Americans. The dimensions proposed by Wolfe et al. (2003) and Warren et al. (2020) guided variable selection. For the purpose of our analysis, we defined food insecurity as a lack of food due to financial limitations, functional impairments, and social constraints.
Figure 1.
The social ecological model of contributing factors to food insecurity among older adults. Note: Adapted from Goldberg and Mawn (2015).
The objective of this study was to construct a summary indicator of food insecurity specific to older adults using the NHATS. We then sought to identify the prevalence of this phenomenon among older Americans. We examined differences in demographic and biopsychosocial characteristics between older Americans classified as food secure versus food insecure, as measured by the new summary indicator. Finally, we examined the construct validity of the summary indicator using relevant biopsychosocial factors known to be associated with food insecurity. This measure will help to improve our understanding of the impact of food insecurity on trends and dynamic processes in later life.
Method
Data and Sample
Data are from the 2015 wave of the NHATS, a nationally representative, population-based survey of Medicare beneficiaries aged 65 years and older (Kasper & Freedman, 2019). The NHATS was created to foster research to maximize health, reduce late-life disability, and enhance quality of life among older adults (Kasper & Freedman, 2019). The NHATS utilizes a complex survey sampling methodology to ensure national representative, and this includes oversampling individuals over the age of 90 and non-Hispanic Blacks (Kasper & Freedman, 2019). Participants in the NHATS undergo annual interviews, completing a detailed assessment battery that includes questions such as performance of daily activities, medical comorbidities, socioeconomic status, social support, and home environment. Our analytic sample includes the full community-dwelling NHATS sample (n = 7,070 individuals; 84.83% of the overall 2015 sample).
Measures
Summary indicator of food insecurity
Currently, the NHATS does not contain a predefined measure of food insecurity status, nor does it include the questions in the USDA-validated food insecurity scales. To enable the study of food insecurity in this population, our team constructed a new summary indicator to identify food insecurity. Consistent with existing multidimensional measures of food insecurity (Goldberg & Mawn, 2015; Wolfe et al., 2003) and accounting for items available in the NHATS, we developed our summary indicator using factors related to food insecurity within two domains of the adapted social ecological model: intrapersonal factors (financial limitations and functional support) and interpersonal factors (emotional support; Goldberg & Mawn, 2015). Where possible, we chose items aligned with Wolfe et al.’s (2003) measure of food insecurity designed for older adults (NHATS questions mapped to Wolfe et al.’s measure appear in Supplementary Table 1). These items were selected as they correspond to direct ways in which functional and social support limitations could limit an older adult’s ability to secure sufficient food. Variable selection was rooted in published literature (e.g., Goldberg & Mawn, 2015; Wolfe et al., 2003) and our conceptualization of how factors associated with aging may influence an individual’s ability to consistently obtain food.
The summary indicator included the following variables in the NHATS: going without groceries, going without hot meals, and going without eating due to lack of ability or social support to do so as well as skipping meals due to financial constraints (Table 1). Participants received one point for each of the five items with a positive response, then items were combined to create a summary score (possible range 0–5). NHATS participants with a summed score of zero were classified as food secure and those with a summed score of one or more were classified as food insecure.
Table 1.
Food Insecurity Summary Indicator Scoring Methodology
| NHATS item | Score |
|---|---|
| In the last month, did you skip any meals because there was not enough food, or money to buy food? | 1 point if yes |
| How many days in the last month did you skip meals? | 1 point if meals are skipped ≥ A few days |
| In the last month, did you ever go without groceries or personal items because it was too difficult to shop by yourself/no one was there to help or shop for you? | 1 point if yes |
| In the last month, did you ever go without a hot meal because it was too difficult for you to make one by yourself/no one was there to help or make one for you? | 1 point if yes |
| In the last month, did you ever go without eating because no one was there to help you/it was too difficult to feed yourself? | 1 point if yes |
| Food Insecurity Classification: | Individual received ≥1 point(s) |
Note: NHATS = National Health and Aging Trends Study.
Biopsychosocial factors
A valid summary indicator of food insecurity should be strongly associated with biopsychosocial factors previously correlated with food insecurity in older adults. We examined the association between the summary indicator and these biopsychosocial factors, including social isolation, community disability, being homebound, and frailty status.
We included a dichotomous measure of social isolation status based on a validated measure in the NHATS created by Cudjoe et al. (2020). Social isolation was assessed using living arrangement, core discussion network size, religious attendance, and social participation. Community disability status (yes/no) was measured using the criteria established by Keeney et al. (2019), using self-reported participation restrictions. Homebound status was characterized using the criteria validated by Ornstein et al. (2015), which measure the frequency that individuals left home, whether they had difficulty leaving home, and whether help was required to leave. As proposed by Ornstein et al. (2015), individuals were categorized into homebound, semi-homebound, and not homebound. Frailty was categorized into three levels using the approach by Bandeen-Roche et al. (2015), which operationalized the Frailty Phenotype by Fried et al. in the NHATS.
Sample characteristics
We examined the following sample characteristics: age (in 5-year categories from 65 to 90 years of age or older), sex, race/ethnicity (white non-Hispanic, Black non-Hispanic, Hispanic, and other), educational attainment (less than a high school diploma, a high school diploma or equivalent, or more than a high school diploma), marital status (married/living with a partner or not married/widowed), living arrangements (percent of individuals living alone), health insurance coverage (Medigap or Medicare supplemental coverage, Medicaid coverage, Tri-Care coverage, and/or Medicare Part D drug coverage), and income. For 43.1% of the sample, income was measured using the imputation methodology in Samuel et al. (2015) and Samuel et al. (2019)), which relies on reported total income, imputed income for missing data, and household size from the NHATS along with the Census Bureau’s 2014 federal poverty limit.
We also quantified receipt of meal assistance and medical comorbidity. Meal assistance was characterized as receipt of the Supplemental Nutrition Assistance Program (SNAP) benefits, and receipt of Meals on Wheels in the last month. Comorbidity was characterized using self-reported health conditions. We used the following 10 self-reported health conditions in the NHATS to create a count of chronic conditions: heart attack, heart disease (including angina or congestive heart failure), high blood pressure, arthritis, osteoporosis, diabetes, lung disease (including emphysema, asthma, or chronic bronchitis), stroke, dementia/Alzheimer’s disease, and cancer. The number of health conditions was summed and reported as none, one or two, three or four, and five or more.
Statistical analyses
Utilizing the summary indicator, we estimated the national prevalence of this expanded definition of food insecurity among community-dwelling older adults in the 2015 NHATS (n = 7,070). We generated national estimates of food insecurity, biopsychosocial factors, and sample characteristics. Sample and biopsychosocial characteristics were compared between those who were food insecure versus food secure using Rao-Scott chi-square tests. To establish the construct validity of the summary indicator of food insecurity, we estimated separate logistic regression models to evaluate the association between the summary indicator and relevant biopsychosocial factors (i.e., frailty status, social isolation, community disability, and being homebound; Ryvicker et al., 2020). We then estimated models adjusted for gender, age, race/ethnicity, marital status, education level, income, self-reported depression (assessed using the Patient Health Questionnaire-2 validated two question screening questionnaire), number of comorbidities, and living alone. While the previous medical conditions were reported by patients based on a doctor’s diagnosis, depression is assessed based on a validated screener, and thus separated in the analysis. We conducted two sensitivity analyses to identify the robustness of the construct validity of our summary indicator with known biopsychosocial factors. First, we examined the construct validity of the score using a cut point of two or more points. Second, we examined construct validity using only the most severe form of food insecurity (e.g., skipping meals due to financial constraints).
NHATS sample weights were included in all analyses to account for differential selection probabilities and potential nonresponse bias (DeMatteis et al., 2016). Our analyses were conducted in Stata version 16.1. This study utilized the public use sample person files of the NHATS. John Hopkins University Institutional Review Board approved the NHATS protocol and obtained informed consent from all participants (Kasper & Freedman, 2019).
Results
Prevalence of Food Insecurity, Sample, and Biopsychosocial Characteristics
In the 2015 round of the NHATS, approximately 1.7 million (4.3%) community-dwelling older adults were classified as food insecure, as defined by the summary indicator (Table 2). Food insecurity was more prevalent among participants who were female, non-White, had less than a high school education, were not married/partnered, had lower income, received an Supplemental Security Income, and received Medicaid (Table 2). For example, individuals who had more than five comorbidities were more than twice as likely to be food insecure (23.9% vs. 9.10%, p < .001). Beyond Medicaid enrollment, health insurance was not significantly associated with food insecurity. Similarly, age was not significantly associated with food insecurity with the exception of participants aged 75–79 years. Food insecure older adults had higher rates of multiple comorbidities, depression, frailty, living alone, being homebound, community disability, and social isolation. Additionally, SNAP participation was more than twice as high among NHATS participants who were food insecure (16.3% vs. 6.6%, p < .001; Table 2). Biopsychosocial factors associated with worse health status were highly prevalent among those who were classified as food insecure (Table 3).
Table 2.
Sample Characteristics of Community-Dwelling NHATS Participants by Food Insecurity Status
| Characteristics | Analytic sample | Food insecure | Food secure |
|---|---|---|---|
| Sample n | 7,070 | 308 | 6,762 |
| Weighted n | 38,834,686 | 1,672,947 | 37,161,738 |
| Weighted % | — | 4.3% | 95.7% |
| Age | |||
| 65–69 | 2,152 (30.4%) | 113 (36.7%) | 1,891 (30.1%) |
| 70–74 | 1,942 (27.5%) | 78 (25.3%) | 1,729 (27.5%) |
| 75–79 | 1,344 (19.0%) | 45 (14.7%) | 1,204 (19.2%) |
| 80–84 | 861 (12.2%) | 32 (10.3%) | 770 (12.3%) |
| 85–89 | 520 (7.4%) | 22 (7.1%) | 462 (7.4%) |
| >90 | 251 (3.6%) | 18 (5.9%) | 216 (3.5%) |
| Sex*** | |||
| Female | 3,965 (54.7%) | 224 (72.6%) | 3,378 (53.9%) |
| Race/Ethnicity*** | |||
| White | 5,480 (77.5%) | 201 (65.3%) | 4,896 (78.1%) |
| Black | 582 (8.2%) | 41 (13.3%) | 502 (8.0%) |
| Hispanic | 513 (7.3%) | 34 (10.9%) | 430 (6.8%) |
| Other | 495 (7.0%) | 32 (10.5%) | 444 (7.1%) |
| Education* | |||
| <High school diploma | 1,380 (19.5%) | 82 (26.6%) | 1,204 (19.2%) |
| High school diploma | 1,783 (25.2%) | 85 (27.6%) | 1,575 (25.1%) |
| >High school diploma | 3,907 (55.3%) | 141 (45.8%) | 3,493 (55.7%) |
| Marital status*** | |||
| Married, living with partner | 4,139 (58.5%) | 111 (36.2%) | 3,735 (59.6%) |
| Not married, widowed | 2,931 (41.5%) | 197 (63.8%) | 2,537 (40.4%) |
| Income*** | |||
| ≤100% 2014 FPL | 1,149 (16.3%) | 92 (30.0%) | 980 (15.6%) |
| 100%–200% 2014 FPL | 1,502 (21.2%) | 101 (32.7%) | 1,300 (20.8%) |
| 200%–500% 2014 FPL | 2,632 (37.2%) | 83 (26.8%) | 2,365 (37.7%) |
| ≥500% FPL | 1,787 (25.3%) | 32 (10.5%) | 1,627 (25.9%) |
| Health coverage | |||
| Medigap supplement | 4,347 (61.5%) | 173 (56.0%) | 3,782 (61.7%) |
| Medicaid*** | 779 (11.0%) | 65 (21.2%) | 662 (10.6%) |
| Tri-care | 394 (5.6%) | 10 (3.4%) | 355 (5.7%) |
| Part D drug coverage | 4,301 (60.8%) | 203 (65.9%) | 3,801 (60.6%) |
| Number of comorbidities*** | |||
| 0 | 691 (9.8%) | 16 (5.2%) | 627 (10.0%) |
| 1–2 | 3,225 (45.6%) | 88 (28.5%) | 2,909 (46.4%) |
| 3–4 | 2,511 (35.5%) | 130 (42.4%) | 2,208 (35.2%) |
| 5+ | 643 (9.1%) | 74 (23.9%) | 528 (8.4%) |
| Depression*** | 872 (12.3%) | 95 (30.8%) | 722 (11.5%) |
| Living alone*** | 5,260 (27.4%) | 132 (42.8%) | 1,677 (26.7%) |
| Congregate meal participation*** | 153 (2.2%) | 22 (7.3%) | 120 (1.9%) |
| SNAP participation*** | 496 (7.0%) | 50 (16.3%) | 415 (6.6%) |
Note: FDL = federal poverty level; NHATS = National Health and Aging Trends Study.
*p < .05; **p < .01; ***p < .001.
Table 3.
Biopsychosocial Characteristics Among Community-Dwelling NHATS Participants, by Food Insecurity Status
| Characteristics | Analytic sample | Food insecure | Food secure |
|---|---|---|---|
| n | 7,070 | 308 | 6,762 |
| Estimate | 38,834,686 | 1,672,947 | 40,015,557 |
| Frailty status*** | |||
| Robust | 36.4% | 8.1% | 37.7% |
| Prefrail | 47.0% | 47.2% | 47.0% |
| Frail | 16.6% | 44.7% | 15.3% |
| Being homebound*** | |||
| Nonhomebound | 83.3% | 46.1% | 84.9% |
| Semi-homebound | 12.4% | 41.8% | 11.1% |
| Homebound | 4.3% | 12.1% | 4.0% |
| Community disability*** | |||
| Community disability | 28.6% | 71.9% | 26.6% |
| Social isolation** | |||
| Severely socially isolated | 5.0% | 8.7% | 4.8% |
| Socially isolated | 24.9% | 31.0% | 24.7% |
| Socially integrated | 70.1% | 60.3% | 70.5% |
Note: NHATS = National Health and Aging Trends Study.
*p < 0.05; **p < .01; ***p < .001.
Construct Validity of the Food Insecurity Summary Indicator
Our summary indicator of food insecurity was positively associated with all relevant biopsychosocial factors prior to adjustment (Table 4). After adjusting for relevant covariates, the food insecurity summary indicator was positively associated with frailty (odds ratio [OR] 9.50, 95% confidence interval [CI] 4.92–18.37), being homebound (OR 3.49, 95% CI 2.03, 6.00), and experiencing community disability (OR 5.19, 95% CI 3.90–6.90). After adjustment, there was no significant relationship between the social isolation composite and food insecurity. However, a component of social isolation, living with more than one person, was negatively associated with food insecurity (Supplementary Tables 4 and 5). These findings support our hypothesized associations between the food insecurity summary indicator and relevant biopsychosocial factors, and provide empirical evidence of the construct validity of the measure.
Table 4.
Odds of Biopsychosocial Factors by Food Insecurity Status, 2015
| OR | 95% CI | |
|---|---|---|
| Unadjusted models | ||
| Frailty status*** | ||
| Robust | — | — |
| Prefrail | 4.70 | 2.53, 8.74 |
| Frail | 13.68 | 7.94, 23.59 |
| Being homebound*** | ||
| Nonhomebound | — | — |
| Semi-homebound | 6.92 | 5.06, 9.45 |
| Homebound | 5.64 | 3.62, 8.79 |
| Community disability*** | ||
| Community disability | 7.08 | 5.43, 9.22 |
| Social isolation* | ||
| Socially integrated | — | — |
| Socially isolated | 1.47 | 1.08, 1.99 |
| Severely socially isolated | 2.12 | 1.34, 3.36 |
| Adjusted modelsa | ||
| Frailty status*** | ||
| Robust | — | — |
| Prefrail | 3.94 | 2.07, 7.50 |
| Frail | 9.50 | 4.92, 18.37 |
| Being homebound*** | ||
| Nonhomebound | — | — |
| Semi-homebound | 4.96 | 3.29, 7.47 |
| Homebound | 3.49 | 2.03, 6.00 |
| Community disability*** | ||
| Community disability | 5.19 | 3.90, 6.90 |
| Social isolation | ||
| Socially integrated | — | — |
| Socially isolated | 1.12 | 0.80, 1.57 |
| Severely socially isolated | 1.05 | 0.57, 1.96 |
Note: CI = confidence interval; NHATS = National Health and Aging Trends Study; OR = odds ratio.
aModels were adjusted for gender, age, race/ethnicity, marital status, education level, income, depression status, number of comorbidities, and living alone.
*p < .05; **p < .01; ***p < .0001.
Results of the sensitivity analyses defining food insecurity as two or more points on the scale were similar in magnitude and direction (Supplementary Tables 2 and 3). Prevalence of the most severe form of food insecurity, skipping meals due to financial constraints, was 1.80%, demonstrating that the nonfinancial measures resulted in a higher, more comprehensive view of the prevalence (Supplementary Table 6). We also performed similar construct validity analyses, which were nonsignificant given the small sample size, but in a similar direction (Supplementary Table 7).
Discussion
In this investigation, we establish a novel summary indicator of food insecurity in a nationally representative cohort of older adults. We find that approximately 5% of community-dwelling individuals can be classified as food insecure utilizing the new summary indicator. Furthermore, frailty status, being homebound, socially isolated, and experiencing community disability were associated with higher rates of food insecurity. While participants who were racial minorities were more likely to be food insecure, participants who were older (aged 75–89 years) and had higher incomes (≥100% federal poverty level) were less likely to be food insecure. In keeping with prior research, being female, having lower educational attainment, being unmarried, Medicaid participation, high comorbidities, and poor perceived health status were all associated with higher rates of food insecurity (Bhargava & Lee, 2017).
By utilizing a validated, nationally representative survey of older adults, this study is the first to create a summary indicator of food insecurity in the NHATS. This summary indicator is an effort to expand the conceptualization of food insecurity among older adults, particularly as it relates to the unique challenges faced by older adults including frailty, social isolation, community disability, and being homebound. In comparing our results to Goldberg and Mawn’s (2015), which also included data on their measure’s association with the biopsychosocial factors, the effect sizes had similar directions, but different magnitudes. Our magnitude was likely larger due to our study population (e.g., a nationally representative survey vs. qualitative interviews) or the use of aggregated biopsychosocial variables versus their use of disaggregated variables. Comprehensive study of food insecurity in older adults is essential given the serious health impacts it poses (Afulani et al., 2015). Among older adults, it is associated with increased disease burden, poor medication adherence (Afulani et al., 2015), falling (Wallace et al., 2007), and delaying necessary care (Bhargava et al., 2017). Nutrition interventions are important as the older population, most of whom live in the community, increases in size and diversity. We found that a large proportion of older adults classified as food insecure using our measure did not participate in meal assistance programs. This may indicate an unmet need that should be targeted in future outreach and enrollment efforts. Lastly, it is important to acknowledge that significant health events may contribute to or exacerbate an individual’s likelihood of experiencing food insecurity. This is an important area for future investigation within the NHATS.
Understanding food insecurity and access in the aging population is increasingly important as the Center for Medicare and Medicaid Services (CMS) makes increasing efforts to prioritize nonmedical health care needs among older adults. In 2019, CMS allowed Medicare Advantage (MA) plans to offer supplemental benefits that utilize community services to address barriers to health care access or avoid costly care (e.g., emergency health care utilization; Meyers et al., 2019). These include benefits such as home-delivered meals and other services designed for daily maintenance (Meyers et al., 2019). Given that more than one third of Medicare beneficiaries (22 million people) are enrolled in an MA plan, it is essential to quantify social needs—such as food insecurity—among the Medicare eligible population (Meyers et al., 2019). This would enable health plans and policy makers to understand how these added benefits are impacting health status and disparities among and between MA and traditional Medicare beneficiaries. Incorporating biopsychosocial factors into food insecurity assessment for older adults would allow community service providers, health plans, medical systems, nonprofits, and policy makers to account for nonfinancial dimensions of food insecurity in this population. This could allow more vulnerable adults to benefit from programs such as home-delivered meals, case management, or congregate meals.
This research has several limitations. Although the NHATS oversamples older adults and non-Hispanic Blacks, we were unable to further explore differences in being classified as food insecure among different minority groups. According to Feeding America’s 2015 State of Senior Hunger Annual Report, 8.1% of older adults are food insecure and 3.2% had very low (i.e., severe) food insecurity (Ziliak & Gundersen, 2017). Ziliak and Gundersen (2017) analyze nationally representative data from the Current Population Survey, which includes the USDA HFSSM questionnaire, to derive food insecurity estimates for households that include older adults. As previously discussed, the HFSSM focuses on financial limitations to obtaining food, and does not include other difficulties older adults may face that are included in our NHATS summary indicator such as lack of social support and/or reduced mobility and function (Lee & Frongillo, 2001; Sahyoun & Basiotis, 2000; Wolfe et al., 1996). Despite this expanded definition of food insecurity encompassed by the NHATS questions, our rate could be lower, in part, because the NHATS restricts its survey to Medicare beneficiaries and excludes homeless or undocumented individuals. Furthermore, the indicator was limited to questions available in the NHATS, which were not as comprehensive as items proposed by Wolfe et al. (2003). For example, we were unable to capture hunger or nutritional quality of food. Finally, our measure uses items such as skipping meals due to financial constraints, which are likely indicative of a particularly severe form of food insecurity. Our finding that 4.3% of older adults are food insecure suggests that broadening the conceptualization of food insecurity through use of the proposed tool may allow for a more thorough assessment among older adults who are experiencing, or at risk for, severe forms of food insecurity, but are currently overlooked as existing measures do not include the biopsychosocial dimensions incorporated in the summary indicator. Finally, we were unable to test our measure against a “gold standard,” such as the HFSSM. The NHATS could allow more comprehensive research of food insecurity among older adults by including the validated HFSSM in a future supplement. Inclusion of the HFSSM would allow for the detection of less severe forms of food insecurity among NHATS participants, thereby improving the sensitivity of measures within NHATS to assess the full range of food insecurity experienced by older adults. Leveraging the panel survey design of NHATS, inclusion of HFSSM measures in future waves would also enhance the ability for these combined measures to be used for surveillance of participant-level changes in food security status over time. Additionally, inclusion of the HFSSM in NHATS would enable further validation testing of the proposed tool by allowing for direct comparison with the current gold standard, as well as how existing financial resource-driven definitions of food insecurity, when used in conjunction with our more expanded definition of food insecurity, may allow for a better understanding of the true burden of food insecurity among older adults.
Using data from the NHATS, we created a summary indicator of food insecurity among community-dwelling older adults. This measure expands on prior work to account for the biopsychosocial limitations older adults disproportionately face. Given that food insecurity is a multidimensional phenomenon among older adults, future work should include biopsychosocial factors to better identify food insecurity in this population.
Supplementary Material
Funding
This work was supported in part by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health; an Agency for Healthcare Research and Quality National Research Service Award T32 (Grant #5T32 HS000011-33 to T. Keeney); a Center on Health Services Training and Research fellowship funded by the Foundation for Physical Therapy Research (T. Keeney); and a Career Development Award from the Veterans Administration (CDA 14–422 to K. S. Thomas).
Conflict of Interest
None declared.
Author Contributions
Study concept and design: E. Tucher, T. Keeney, A. J. Cohen, and K. S. Thomas. Analysis and interpretation of data: E. Tucher, T. Keeney, and A. J. Cohen. Drafting of the manuscript: E. Tucher and T. Keeney. Critical revision of the manuscript for important intellectual content: E. Tucher, T. Keeney, A. J. Cohen and K. S. Thomas.
References
- Afulani, P, Herman, D, Coleman-Jensen, A, & Harrison, G G. (2015). Food insecurity and health outcomes among older adults: The role of cost-related medication underuse. Journal of Nutrition in Gerontology and Geriatrics, 34(3), 319–342. doi: 10.1080/21551197.2015.1054575 [DOI] [PubMed] [Google Scholar]
- Anderson, S A. (1990). The 1990 Life Sciences Research Office (LSRO) Report on Nutritional Assessment defined terms associated with food access. Core indicators of nutritional state for difficult to sample populations. Journal of Nutrition, 120, 1559–1660. doi: 10.1093/jn/120.suppl_11.1555 [DOI] [PubMed] [Google Scholar]
- Baker-Lutz, H, Chapman, J, Crumbaugh, A S, Hake, M, Prasad, D, Preuss, L, Smith, M., Strayer, M., & Villarreal, Z. (2019). The state of senior hunger in 2017: Executive summary. Feeding America. Retrieved from https://www.feedingamerica.org/sites/default/files/2019-05/state-of-senior-hunger-in-2017_executive-summary.pdf
- Bandeen-Roche, K, Seplaki, C L, Huang, J, Buta, B, Kalyani, R R, Varadhan, R, Xue, Q., Walston, J. D., & Kasper, J D. (2015). Frailty in older adults: A nationally representative profile in the United States. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 70(11), 1427–1434. doi: 10.1093/gerona/glv133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz, S A, Basu, S, Meigs, J B, & Seligman, H K. (2018). Food insecurity and health care expenditures in the United States, 2011-2013. Health Services Research, 53(3), 1600–1620. doi: 10.1111/1475-6773.12730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhargava, V, & Lee, J S. (2017). Food insecurity and health care utilization among older adults. Journal of Applied Gerontology, 36(12), 1415–1432. doi: 10.1177/0733464815625835 [DOI] [PubMed] [Google Scholar]
- Bickell, G, Nord, M, Price, C, Hamilton, W, & Cook, J. (2000). Guide to measuring household food security. Retrieved from https://fns-prod.azureedge.net/sites/default/files/FSGuide.pdf
- Coleman-Jensen, A, Rabbitt, M P, & Gregory, C A (2012).U.S. Adult Food Security Survey Module: Three Stage Design. USDA Economic Research Service. http://www.ers.usda.gov/media/8279/ad2012.pdf
- Cudjoe, T K M, Roth, D L, Szanton, S L, Wolff, J L, Boyd, C M, & Thorpe, R J. (2020). The epidemiology of social isolation: National Health and Aging Trends Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(1), 107–113. doi: 10.1093/geronb/gby037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMatteis, J, Freedman, V A, & Kasper, J D. (2016). National Health and Aging Trends Study development of round 5 survey weights. NHATS Technical Paper #14. Johns Hopkins University School of Public Health. Retrieved from www.NHATS.org. [Google Scholar]
- Durazo, E M, Jones, M R, Wallace, S P, Arsdale, J V, Aydin, M, & Stewart, C. (2011). Older adults in California. Retrieved from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=21688692&retmode=ref&cmd=prlinks%0Apapers3://publication/uuid/E0D44D8B-A300-4CD4-84F1-566021F475B7
- Goldberg, S L, & Mawn, B E. (2015). Predictors of food insecurity among older adults in the United States. Public Health Nursing (Boston, Mass.), 32(5), 397–407. doi: 10.1111/phn.12173 [DOI] [PubMed] [Google Scholar]
- Gundersen, C, & Ziliak, J P. (2015). Food insecurity and health outcomes. Health Affairs (Project Hope), 34(11), 1830–1839. doi: 10.1377/hlthaff.2015.0645 [DOI] [PubMed] [Google Scholar]
- Jackson, J A, Branscum, A, Tang, A, & Smit, E. (2019). Food insecurity and physical functioning limitations among older U.S. adults. Preventive Medicine Reports, 14, 100829. doi: 10.1016/j.pmedr.2019.100829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper, J D, & Freedman, V A. (2019). National Health and Aging Trends Study user guide: Rounds 1–8 Beta Release. Johns Hopkins University School of Public Health. Retrieved from www.NHATS.org [Google Scholar]
- Keeney, T, & Jette, A M. (2019). Individual and environmental determinants of late-life community disability for persons aging with cardiovascular disease. American Journal of Physical Medicine & Rehabilitation, 98(1), 30–34. doi: 10.1097/PHM.0000000000001011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel, M B, Gupta, R, Gee, L, & Haas, J S. (2006). Housing instability and food insecurity as barriers to health care among low-income Americans. Journal of General Internal Medicine, 21(1), 71–77. doi: 10.1111/j.1525-1497.2005.00278.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J S, Fischer, J G, & Johnson, M A. (2010). Food insecurity, food and nutrition programs, and aging: Experiences from Georgia. Journal of Nutrition for the Elderly, 29(2), 116–149. doi: 10.1080/01639366.2010.480895 [DOI] [PubMed] [Google Scholar]
- Lee, J S & Frongillo, E A Jr. (2001). Factors associated with food insecurity among U.S. elderly persons: Importance of functional impairments. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56(2), S94–S99. doi: 10.1093/geronb/56.2.s94 [DOI] [PubMed] [Google Scholar]
- Mather, M, Jacobsen, L A, & Pollard, K M. (2015). Aging in the United States. Retrieved from https://www.prb.org/wp-content/uploads/2016/01/aging-us-population-bulletin-1.pdf
- Melchior, M, Caspi, A, Howard, L M, Ambler, A P, Bolton, H, Mountain, N, & Moffitt, T E. (2009). Mental health context of food insecurity: A representative cohort of families with young children. Pediatrics, 124(4), e564–e572. doi: 10.1542/peds.2009-0583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers, D J, Durfey, S N M, Gadbois, E A, & Thomas, K S. (2019). Early adoption of new supplemental benefits by Medicare advantage plans. Journal of the American Medical Association, 321(22), 2238–2240. doi: 10.1001/jama.2019.4709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornstein, K A, Leff, B, Covinsky, K E, Ritchie, C S, Federman, A D, Roberts, L, Kelley, A. S., Siu, A. L., & Szanton, S L. (2015). Epidemiology of the homebound population in the United States. JAMA Internal Medicine, 175(7), 1180–1186. doi: 10.1001/jamainternmed.2015.1849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redmond, M L, Dong, F, Goetz, J, Jacobson, L T, & Collins, T C. (2016). Food insecurity and peripheral arterial disease in older adult populations. The Journal of Nutrition, Health & Aging, 20(10), 989–995. doi: 10.1007/s12603-015-0639-0 [DOI] [PubMed] [Google Scholar]
- Ryvicker, M, Bollens-Lund, E, & Ornstein, K A. (2020). Driving status and transportation disadvantage among Medicare beneficiaries. Journal of Applied Gerontology, 39(9), 935–943. doi: 10.1177/0733464818806834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahyoun, N & Basiotis, P. (2000) Food insufficiency and the nutritional status of the elderly population. Nutrition Insights 18 2000. USDA Center for Nutrition Policy and Promotion. [Google Scholar]
- Samuel, L J, Glass, T A, Thorpe, R JJr, Szanton, S L, & Roth, D L. (2015). Household and neighborhood conditions partially account for associations between education and physical capacity in the National Health and Aging Trends Study. Social Science & Medicine (1982), 128, 67–75. doi: 10.1016/j.socscimed.2015.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel, L J, Szanton, S L, Seplaki, C L, Cudjoe, T K M, Thorpe, R JJr, & Agree, E M. (2019). Longitudinal and reciprocal associations between financial strain, home characteristics and mobility in the National Health and Aging Trends Study. BMC Geriatrics, 19(1), 338. doi: 10.1186/s12877-019-1340-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman, H K, Bindman, A B, Vittinghoff, E, Kanaya, A M, & Kushel, M B. (2007). Food insecurity is associated with diabetes mellitus: Results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. Journal of General Internal Medicine, 22(7), 1018–1023. doi: 10.1007/s11606-007-0192-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman, H K, Jacobs, E A, Lopez, A, Sarkar, U, Tschann, J, & Fernandez, A. (2011). Food insecurity and hypoglycemia among safety net patients with diabetes. Archives of Internal Medicine, 171(13), 1204–1206. doi: 10.1001/archinternmed.2011.287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman, H K, & Schillinger, D. (2010). Hunger and socioeconomic disparities in chronic disease. The New England Journal of Medicine, 363(1), 6–9. doi: 10.1056/NEJMp1000072 [DOI] [PubMed] [Google Scholar]
- Siefert, K, Heflin, C M, Corcoran, M E, & Williams, D R. (2004). Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. Journal of Health and Social Behavior, 45(2), 171–186. doi: 10.1177/002214650404500204 [DOI] [PubMed] [Google Scholar]
- Srinivasan, M, & Pooler, J A. (2018). Cost-related medication nonadherence for older adults participating in SNAP, 2013-2015. American Journal of Public Health, 108(2), 224–230. doi: 10.2105/AJPH.2017.304176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Committee on Aging . (1969, April 29). Economics of aging: Toward a full share in abundance. Senate Media. https://www.aging.senate.gov/imo/media/doc/publications/4291969.pdf
- Wallace, S P, Molina, L C, & Jhawar, M. (2007). Falls, disability and food insecurity present challenges to healthy aging. Policy Brief UCLA Center for Health Policy Research, ( Pb2007-5), 1–12. [PubMed] [Google Scholar]
- Warren, A M, Frongillo, E A, Alford, S, & McDonald, E. (2020). Taxonomy of Seniors’ needs for food and food assistance in the United States. Qualitative Health Research, 30(7), 988–1003. doi: 10.1177/1049732320906143 [DOI] [PubMed] [Google Scholar]
- Wolfe, W S, Frongillo, E A, & Valois, P. (2003). Understanding the experience of food insecurity by elders suggests ways to improve its measurement. The Journal of Nutrition, 133(9), 2762–2769. doi: 10.1093/jn/133.9.2762 [DOI] [PubMed] [Google Scholar]
- Wolfe, W S, Olson, C M, Kendall, A & Frongillio, E A. (1996). Understanding food insecurity in the elderly: A conceptual framework. Journal of Nutrition Education, 28, 92–100. doi: 10.1016/S0022-3182(96)70034-1 [DOI] [Google Scholar]
- Wong, J C, Scott, T, Wilde, P, Li, Y G, Tucker, K L, & Gao, X. (2016). Food insecurity is associated with subsequent cognitive decline in the Boston Puerto Rican health study. The Journal of Nutrition, 146(9), 1740–1745. doi: 10.3945/jn.115.228700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziliak, J P, & Gundersen, C (2017). The state of senior hunger in America 2015: An annual report. August. https://www.feedingamerica.org/sites/default/files/research/senior-hunger-research/state-of-senior-hunger-2015.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.