Abstract
Objectives
This study investigated whether older adults with better relationships with their adult children have better subjective and objective sleep quality than older adults with less-positive relationships with their children. We also examined whether depressive symptoms and loneliness mediated the association between parent–child relationships and sleep among older adults.
Methods
Data were used from the second wave of the National Social life, Health, and Aging Project, in which 548 respondents (aged 62–90) participated in the sleep survey to measure their actigraph sleep activity for three consecutive days. Respondents also reported sleep quality (i.e., sleep duration and insomnia symptoms), contact frequency, and emotional closeness with their children.
Results
Results from structural equation modeling showed that greater emotional closeness with children was directly associated with better objective sleep characteristics (i.e., sleep fragmentation and amount of sleep). Also, more frequent contact with children was directly related to fewer insomnia symptoms among older adults. Moreover, emotional closeness with children was indirectly linked to insomnia symptoms via depressive symptoms among older adults.
Discussion
This study provided evidence for psychological pathways linking parent–child relationships and older parents’ subjective sleep. The findings have implications for health professionals and family counselors who help people with sleep problems and relationship difficulties.
Keywords: Depression, Intergenerational relationships, Loneliness, Sleep
Recent studies of sleep health in later life demonstrate that as people grow older, they tend to have difficulty falling asleep and have reduced duration and quality of sleep (Gulia & Kumar, 2018). Among many reasons accounting for older adults’ emerging sleep problems, such as medical comorbidity, medication and substance use, and psychosocial factors (e.g., depression, loneliness, and bereavement; Miner & Kryger, 2017), there is an increasing focus on the importance of family relations for sleep (Chen et al., 2016; Troxel et al., 2010). However, prior studies primarily focused on spousal relations and sleep quality (Chen et al., 2015; Lee et al., 2017; Troxel et al., 2010). In addition to spouses, adult children are important key members in older adults’ lives and networks. Thus, it is crucial to examine how older adults’ relationships with adult children are related to their sleep quality and quantity. Moreover, studies on family relations and sleep quality have mainly examined subjective sleep quality among older adults (Ailshire & Burgard, 2012; Lee et al., 2017; Wang et al., 2020). Because subjective measures of sleep quality depend on older adults’ cognitive capacity reflecting on their past experience, these reports may be biased by respondents’ health and cognitive conditions of older adults (Landry et al., 2015). Therefore, research is needed to incorporate both subjective and objective dimensions of sleep to better understand how family processes are related to older adults’ sleep quality (Hughes et al., 2018; Landry et al., 2015).
To fill this gap, this study investigated whether older adults’ relationships with their adult children are associated with their sleep by examining both subjective and objective sleep characteristics. Moreover, this study examined two underlying psychological mechanisms that may link parent–adult child relationships and sleep quality among older adults.
Parent–Child Relationships and Sleep
Earlier research based on the social support and stress process models established that close social relationships are directly linked to one’s well-being, including sleep quality (Ailshire & Burgard, 2012; Chen et al., 2016; Chung, 2017; Kent et al., 2015). Supportive relationships provide a sense of safety and reduced vigilance such that people with more social support have better sleep outcomes. Material and emotional support from social ties buffer the negative effect of stressors on sleep, as well as helping to reduce exposure to stressors, which undermine one’s sleep quality (Thoits, 2011). Negative social relations, on the other hand, represent a primary source of stress for older adults, and this stress may lead to negative emotions, poor sleep-related behaviors, and altered physiological responses—all of which increase the risk of sleep disturbance and sleep disorders.
Among all social relationships, the parent–child tie plays a crucial role for many individuals’ well-being across their life spans. Research has well documented the implications of intergenerational relationships (e.g., emotional quality and support exchanges) for aging parents’ physical and psychological well-being (for a review, see Fingerman et al., 2013). Regarding sleep outcomes, a handful of studies show that having a child in the household is associated with better sleep quality for parents (Troxel et al., 2009), and poor parent–child relationship quality is predictive of increased insomnia for older parents (Wang et al., 2020). However, less is known about how parent–child relationships are related to objective sleep for older parents.
Adult child–parent relationships are often characterized by frequent contact and emotional closeness (Lye, 1996). Contact between generations is viewed as an important dimension of intergenerational solidarity and a good indicator of the strength of parent–child ties (Tosi & Grundy, 2019). Frequent contact with children provides more opportunities for companionship and interactions, reducing social isolation among older parents. Also, through regular contact with aging parents, adult children may ensure their parents’ current status and conditions and help them arrange support, when needed (Ward et al., 2014). Older parents with more frequent in-person contact with their children often enjoy better psychological well-being (Fingerman et al., 2016; Teo et al., 2015; Tosi & Grundy, 2019). Moreover, emotional closeness with adult children provides a sense of warmth, belonging, and security for older parents. With emotionally satisfying relations with adult children, older parents may have less vigilance and physiological arousal from stressors (Mikulincer & Shaver, 2005), which promotes better sleep. In contrast, older parents are more likely to have insomnia symptoms if they have strained relationships with their adult children (Wang et al., 2020). Thus, we expect that older parents with frequent contact and emotional closeness with their children will have better objective and subjective sleep.
Psychological Pathways Linking Parent–Child Relationships and Sleep
As the stress process model posits, supportive and strained social relations both have impacts on individuals’ well-being through psychological pathways (Pearlin, 2010). People with less supportive or more strained social relationships have worse psychological well-being, including higher levels of anxiety, worry, depression, and loneliness, which may lead to poorer sleep due to physiological arousal (Jackowska et al., 2016; Kahn et al., 2013). In this study, we focused on depressive symptoms and loneliness, which are highly prevalent among older adults and detrimental for an individual’s physical health and quality of life.
Parent–child relationships are among the most important for both adult children and their parents. There is extensive research on how parent–child relationships are related to older parents’ psychological well-being, including depression and loneliness (Koropeckyj-Cox, 2002; Reczek & Zhang, 2016; Tosi & Grundy, 2019). Depressive symptoms are associated with reports of sleep problems, such as difficulty falling asleep, fragmented sleep, early morning awakening, and waking feeling unrested (Hall, 2010). One recent study found that depression significantly mediated the relationship between social ties and subjective sleep quality among middle-aged and older adults (Kent et al., 2015). However, the role of depression in the association of parent–child relationship quality and sleep remains under-investigated.
Loneliness has long been recognized as a risk factor for sleep (Cacioppo et al., 2002). When experiencing loneliness, one can have increased feelings of vulnerability and unconscious vigilance for environmental queues, which undermine one’s sleep (Hawkley & Cacioppo, 2010). Although loneliness is an important aspect of social relations, little research has examined loneliness as a pathway connecting social relations and sleep; however, one study found that loneliness partially mediated the link between marital quality and self-reported troubled sleep (Chen et al., 2015). Most studies have considered loneliness itself as a social determinant for sleep quality (Cacioppo et al., 2002; Hawkley & Cacioppo, 2010). Yet, no published research investigates whether and how loneliness explains the association between parent–child relationships and older parents’ sleep.
Subjective and Objective Measures of Sleep
There is still no consensus on how to best measure sleep, and the health consequences of sleep may depend on how sleep is measured (Lauderdale et al., 2017). Most studies on the social determinants of sleep have focused on subjective sleep quality, relying on retrospective questions about sleep duration and self-reported sleep quality (Ailshire & Burgard, 2012; Kent et al., 2015). Objective measures of sleep characteristics—such as polysomnography and actigraphy—are shown to be modestly correlated, and the correlation between objective and subjective measures of sleep is also not strong (van den Berg et al., 2009; Lauderdale et al., 2008). Subjective indicators are easier to measure and more closely related to individuals’ psychological well-being, whereas objective measures are more straightforward in terms of interpretation and less biased by the emotional and cognitive status of respondents. Studies comparing objective and subjective measures of sleep indicate these measures target different aspects of sleep quality and each provides valuable insights for older adults’ health (Landry et al., 2015). Thus, sleep scholars recommend including both subjective and objective measures when examining sleep quality among older adults (Hughes et al., 2018).
Studies utilizing subjective and objective measures of sleep provided mixed results regarding depression and loneliness. Some studies found that subjective but not objective sleep was associated with depression among older adults (Gould et al., 2018). Other studies showed that self-reported short sleep duration, but not long sleep duration, was predictive of depression (Lippman et al., 2017), while another study suggested that both short and long sleep durations were related to higher risks for depression (Zhai et al., 2015). Loneliness was found to predict poorer objective sleep efficiency (Cacioppo et al., 2002), but loneliness was not significantly associated with self-reported sleep duration (Hawkley et al., 2010). Discrepancies in these studies’ findings may be due to the use of different measures of sleep (self-reported vs. measured by instruments), different sampling strategies (small laboratory sample vs. large national sample), and different study designs (prospective vs. cross-sectional). Thus, a comprehensive examination of parent–child relationship quality and older parents’ subjective and objective sleep would be helpful to understand the family and psychological process of sleep for older adults.
Covariates
Studies revealed that several sociodemographic characteristics influence one’s sleep. Sleep problems are more prevalent among older adults than younger ones (Miner & Kryger, 2017). A high level of education, being married, and being employed are associated with better subjective sleep quality and healthy sleep duration (Grandner et al., 2010; Krueger & Friedman, 2009). Black older adults are at increased risk for short sleep duration and/or poor sleep quality compared to Whites (Patel et al., 2010). Older adults with low income and more comorbidities are more likely to have complaints about their sleep (Grandner et al., 2010).
The Current Study
Using a nationally representative sample of U.S. older adults, this study aimed to examine the psychological pathways for the association between parent–adult child relationship quality (i.e., contact frequency and emotional closeness) and older parents’ sleep. Because sleep has multiple dimensions, objective and subjective measures of sleep are regulated by different psychophysiological processes and capture different aspects of sleep. Thus, we used both subjective and objective measures of sleep for a more comprehensive understanding of how parent–child relationships are related to sleep in later life. Specifically, we hypothesized direct effects of parent–adult child relationships on subjective and objective sleep:
Hypothesis 1a: Older adults with better parent–child relationships will have better objective sleep (e.g., less disturbance and fragmentation).
Hypothesis 1b: Older adults with better parent–child relationships will have better subjective sleep (i.e., longer duration and fewer insomnia symptoms).
This does not mean that we expected the strength of associations between parent–child relationships and two dimensions of sleep would be the same. Because objective and subjective dimensions of sleep are intrinsically different and regulated by different physiological and psychological processes, it is possible that one measure of sleep may be more sensitive to parent–child relationships than the other (Chen et al., 2016). Moreover, there is no theoretical guidance or consensus in the empirical findings regarding the different linkages for objective and subjective sleep. Thus, we did not have a specific hypothesis about the differences in parent–child relationships sleep links across two sleep dimensions.
In addition, this study examined how older adults’ psychological well-being (i.e., depressive symptoms and loneliness) mediated the link between parent–child relationship quality and their sleep. We hypothesized the mediation effects of depressive symptoms and loneliness, respectively:
Hypothesis 2a: Older adults with better parent–child relationships will have fewer depressive symptoms, and fewer depressive symptoms are associated with better objective sleep.
Hypothesis 2b: Older adults with better parent–child relationship quality will have fewer depressive symptoms, and fewer depressive symptoms are associated with better subjective sleep.
Hypothesis 3a: Older adults with better parent–child relationships will have a lower level of loneliness, and a lower level of loneliness is associated with better objective sleep.
Hypothesis 3b: Older adults with better parent–child relationships will have a lower level of loneliness, and a lower level of loneliness is associated with better subjective sleep.
Method
Data and Sample
This study employed data from the National Social life, Health, and Aging Project (NSHAP), a nationally representative study of older Americans (Waite et al., 2019). The first wave (2005–2006) used a probability sample of community-dwelling individuals aged 57–85 across the United States. Five years later (2010–2011), the second wave of NSHAP (N = 3,377) introduced a special module on daytime activity and sleep for a randomly selected one third of the primary sample respondents and their spouses. A wrist Actiwatch, along with an activity and sleep booklet, was mailed to 897 participants to collect information about their sleep and activity levels over three consecutive days (i.e., 72 h). A total of 780 participants completed this module and provided usable actigraphy data.
Drawing data from the second wave of the NSHAP, this study included respondents aged 62 years and older who participated in the sleep module (N = 548). No significant differences between the excluded respondents (n = 2,829) and respondents in the analytic sample (n = 548) were found with regard to age, gender, education, marital status, and household income. Missing values were handled with the Full Information Maximum Likelihood (FIML) method in Mplus 8.1.
Measures
Objective sleep
NSHAP used Actiwatch records (Philips/Respironics 2010) to measure the objective sleep characteristics of respondents. Four actigraph-estimated sleep characteristics were analyzed (Chen et al., 2015; for actigraph-measured sleep, see Lauderdale et al., 2014). These included (1) total sleep time (the length of the sleep interval from the first epoch counted as sleep to the last epoch counted as sleep in the main sleep interval, in hours); (2) percentage sleep (the ratio of the length of actual sleep time to total assumed sleep time, ranging 0–100); (3) sleep fragmentation index (the sum score of (a) the percentage of the sleep interval spent moving and (b) the percentage of immobile periods, ranging 0–100), and (4) wake after sleep onset (WASO; duration of WASO, in minutes). For each of the actigraph-estimated sleep characteristics, a mean score was created across three nights for each respondent. For a small number of respondents with fewer than three nights of usable actigraphy data, we examined one or two nights, as available, to calculate objective sleep indicators (Lauderdale et al., 2014).
Subjective sleep
Survey questions for subjective sleep characteristics included (a) hours of sleep and (b) insomnia symptoms. Respondents were asked to report their usual bedtime and wake-up time, separately for weekdays and weekends. Using this information, NSHAP calculated each respondent’s usual sleep duration for weekdays and weekends separately, and then multiplied weekday sleep duration by 5 and weekend sleep duration by 2 and divided by 7 to obtain an estimate of self-reported average weekly total sleep time (Lauderdale et al., 2014).
NSHAP included four questions on insomnia in the sleep booklet. These four questions included “How often do you have trouble falling asleep?” “How often do you have trouble with waking up during the night?” “How often do you have trouble with waking up too early and not being able to fall asleep again?” and “How often do you feel really rested when you wake up in the morning?” (Jenkins et al., 1988). Responses were rated at 0 (rarely or never), 1 (sometimes), and 2 (most of the time). A mean score was created across four items for insomnia, where a higher score indicates more insomnia symptoms (α = .61; range = 0–2).
Parent–child relationships
For each (biological or step) child, respondents were asked about their (a) contact frequency: “How often do you talk to this person?” with answers rated on a 7-point scale ranging from 1 (less than once a year) to 7 (every day) and (b) emotional closeness: “How close do you feel is your relationship with this person?” with answers rated on a 4-point scale ranging from 1 (not very close) to 4 (extremely close). Mean scores of each parent–child relationship characteristic were created for parents’ reports across all children, with higher scores indicating more frequent contact or greater emotional closeness with adult children.
Psychological well-being
We measured two aspects of older adults’ psychological well-being: (a) depressive symptoms and (b) loneliness. Depressive symptoms were assessed by a shortened version of the Center for Epidemiologic Studies-Depression (CES-D) scale (11 items). The CES-D scale has been widely used as the instrument to identify major depression among older adults (Andresen et al., 1994). Respondents were asked about their feelings during the last week, such as “I felt that everything I did was an effort” and “I felt sad.” Responses were rated at 0 (rarely or none of the time), 1 (some of the time), 2 (occasionally), and 3 (most of the time; reverse-coding for positive items such as happiness). The loneliness and sleep quality items were excluded due to overlapping information with other variables of interest in this study. Finally, we created a sum score across nine items to capture the number of depressive symptoms (α = .76; range = 0–27).
Loneliness was measured by the short version of the University of California Los Angeles (UCLA) loneliness scale (Hughes et al., 2004). Respondents were asked to assess their feelings regarding three aspects of life, including “How often do you feel that you lack companionship?” “How often do you feel left out?” and “How often do you feel isolated from others?” Responses were rated at 0 (never), 1 (hardly never), 2 (some of the time), and 3 (often). A sum score was generated for the three items, with a higher score indicating greater loneliness (α = .82; range = 0–9).
Covariates
Analyses also included respondent’s gender (1 = female and 0 = male), age (in years), race/ethnicity (1 = race or ethnic minority group member and 0 = non-Hispanic White), marital status (1 = married and 0 = unmarried), education (in years), household income (transformed by natural log), the number of living children, and number of chronic conditions (a sum score of 10 diseases including heart attack, congestive heart failure, stroke, diabetes, chronic obstructive pulmonary disease, cancer, arthritis, Alzheimer’s, and other dementia; range = 0–10).
Analytic Strategy
Structural equation modeling (SEM) was employed to examine the psychological pathways linking parent–child relationships with older adults’ sleep characteristics. Because we used latent constructs for the key study variables (i.e., insomnia symptoms, depressive symptoms, and loneliness), we tested the measurement model in the SEM. Measurement models specify the relationships between observed indicators and latent variables, ultimately allowing for the evaluation of the reliability of latent constructs. Criteria for model fit were based on the comparative fit index (CFI) and the root mean square error of approximation (RMSEA), such that a CFI value greater than .90 and an RMSEA value of less than .08 indicated a good fit (Kline, 2016).
First, we estimated a SEM model to examine the association between parent–child relationships and objective sleep among older adults (Hypothesis 1a). Two parent–child relationship characteristics (i.e., contact frequency and emotional closeness) and four objective sleep characteristics (i.e., total sleep time, WASO, percentage sleep, and sleep fragmentation index) were included in the SEM model simultaneously. The model included the covariates identified above.
Similarly, a SEM model was estimated to examine the associations between parent–child relationship and subjective sleep among older adults (Hypothesis 1b). Two parent–child relationship characteristics (i.e., contact frequency and emotional closeness) and two subjective sleep characteristics (i.e., sleep duration and insomnia symptoms) were included in the model. The model also included the set of observed covariates.
We conducted bootstrap tests of the mediation effects of depressive symptoms (Hypothesis 2a) and loneliness (Hypothesis 2b) in the association between parent–child relationships and objective sleep. Thus, indirect effect coefficients and 95% confidence intervals (CIs) were estimated using 1,000 bootstrapped samples to determine the significance of the indirect effects (Kline, 2016). We also conducted bootstrap tests to determine the significance of the mediation effects of depressive symptoms (Hypothesis 3a) and loneliness (Hypothesis 3b) in the associations between parent–child relationships and subjective sleep.
Results
Descriptive characteristics of the study sample are presented in Table 1. Respondents were, on average, 72.80 years old, and the majority of them were female (58%), non-Hispanic White (74%), and married (67%). We presented objective and subjective sleep characteristics in Table 2. Regarding actigraph-estimated sleep characteristics, the average sleep duration for respondents was 7.90 h and they spent 92% of the sleep interval asleep (percentage sleep). The average wake time after sleep onset was 38.88 min and the mean sleep fragmentation index was 14.27 on a scale from 0 to 100. As for subjective sleep characteristics, respondents, on average, reported 7.36 h of sleep time and they had moderate levels of insomnia symptoms (M = 1.07, range = 0–2). The measurement model for latent constructs of insomnia symptoms, depressive symptoms, and loneliness is presented in Supplementary Table 1.
Table 1.
Characteristics of the Study Sample
| Variables | M | (SD) | Range |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Age | 72.80 | (7.38) | 62–91 |
| Female, % | 58 | ||
| Race/ethnic minority, % | 26 | ||
| Education, % | |||
| Less than high school | 18 | ||
| High school or equivalent | 25 | ||
| Some college | 36 | ||
| Bachelors or more | 21 | ||
| Married, % | 67 | ||
| Household income | 53,876.36 | (58,563.58) | 0–60,000 |
| Number of living children | 2.78 | (2.34) | 1–12 |
| Number of chronic conditionsa | 1.21 | (1.27) | 0–7 |
| Parent–child relationships | |||
| Contact frequencyb | 6.86 | (1.01) | 1–8 |
| Emotional closenessc | 3.27 | (0.56) | 1–4 |
| Psychological well-being | |||
| Depressive symptomsd | 3.47 | (3.85) | 0–27 |
| Lonelinesse | 2.65 | (3.56) | 0–9 |
Note: N = 548.
aSum score of 10 items coded 1 = yes and 0 = no.
bRated from 1 = less than once a year to 8 = every day.
cRate from 1 = not very close to 4 = extremely close.
dSum score of nine items rated from 0 = rarely or none of the time to 3 = most of the time.
eSum score of three items rated from 0 = never to 3 = often.
Table 2.
Summary Statistics of Sleep Characteristics
| Variables | M | (SD) | Range | 1a | 1b | 1c | 1d | 2a | 2b |
|---|---|---|---|---|---|---|---|---|---|
| 1. Objective sleep (actigraph-measured) | |||||||||
| a. Assumed sleep (in hours) | 7.90 | (1.31) | 1.64–12.09 | — | |||||
| b. WASO (in minutes) | 38.88 | (22.98) | 3.17–178.50 | .29*** | — | ||||
| c. Fragmentation (0–100) | 14.27 | (5.88) | 1.19–45.81 | −.05 | .77*** | — | |||
| d. Percent sleep (0–100) | 91.69 | (4.64) | 55.65–99.29 | −.01 | −.93*** | −.82*** | — | ||
| 2. Subjective sleep (self-reported) | |||||||||
| a. Sleep duration (in hours) | 7.36 | (1.41) | 3–11 | .23*** | −.11* | −.16*** | .17*** | — | |
| b. Insomnia symptomsa | 1.07 | (0.45) | 0–2 | .10* | .13** | .06 | −.09* | −.33*** | — |
Notes: WASO = wake up after onset. N = 548. Pearson correlations were based on 2-tailed tests.
aMean score of four items rated at 0 = rarely or never, 1 = sometimes, and 2 = most of time.
*p < .05. **p < .01. ***p < .001.
To begin, we estimated a model to examine the association between parent–child relationships and objective sleep characteristics among older adults (Table 3). Results from SEM showed that emotional closeness with children was associated with better objective sleep, including less fragmentation (B = −1.05, p = .033) and longer percent sleep (B = 0.82, p = .036). However, neither contact frequency nor psychological well-being (depressive symptoms and loneliness) was related to actigraph measures of sleep. We did not find any significant indirect effect of emotional closeness with children for actigraphy sleep characteristics through psychological well-being among older adults.
Table 3.
Structural Equation Model Results for Parent–Child Relationships and Older Parents’ Objective Sleep Characteristics
| Assumed sleep | WASO | Fragmentation | Percent sleep | |||||
|---|---|---|---|---|---|---|---|---|
| Variables | B | (SE) | B | (SE) | B | (SE) | B | (SE) |
| Parent–child relationships | ||||||||
| Contact frequencya | 0.08 | (0.06) | 0.93 | (1.11) | 0.06 | (0.28) | 0.09 | (0.23) |
| Emotional closenessb | 0.12 | (0.11) | −3.29 | (1.91) | −1.05* | (0.49) | 0.82* | (0.39) |
| Psychological well-being | ||||||||
| Depressive symptomsc | −0.00 | (0.22) | 1.25 | (4.00) | 0.42 | (1.03) | −0.29 | (0.82) |
| Lonelinessd | −0.14 | (0.12) | 3.03 | (2.10) | 0.77 | (0.54) | −0.52 | (0.43) |
| Sociodemographic characteristics | ||||||||
| Age | 0.02* | (0.01) | 0.03 | (0.15) | 0.07 (0.04) | 0.01 | (0.03) | |
| Female | 0.29* | (0.12) | −2.85 | (2.22) | −1.72** | (0.58) | 0.90* | (0.46) |
| Racial/ethnic minority | −0.16 | (0.14) | 3.09 | (2.59) | 1.43* | (0.67) | −0.74 | (0.53) |
| Education | ||||||||
| High school or equivalente | −0.18 | (0.19) | −5.16 | (3.41) | −0.44 | (0.88) | 0.77 | (0.70) |
| Some collegee | −0.22 | (0.18) | −5.20 | (3.19) | 0.21 | (0.82) | 0.77 | (0.65) |
| Bachelor or moree | −0.20 | (0.20) | −12.50** | (3.66) | −1.54 | (0.95) | 2.29** | (0.75) |
| Married | 0.17 | (0.13) | −4.52 | (2.35) | −0.64 | (0.61) | 1.07* | (0.48) |
| Household incomef | −0.00 | (0.01) | −0.29 | (0.24) | −0.05 | (0.06) | 0.08 | (0.05) |
| Number of living children | −0.01 | (0.04) | −0.52 | (0.66) | −0.02 | (0.17) | 0.10 | (0.14) |
| Number of chronic conditionsg | 0.10* | (0.05) | 0.74 | (0.84) | 0.18 | (0.22) | −0.04 | (0.17) |
| Intercept | 5.32*** | (0.80) | 57.68*** | (14.58) | 15.37*** | (3.76) | 84.23*** | (2.98) |
Notes: WASO = wake up after onset. N = 548. Model fit: comparative fit index = .93, root mean square error of estimation = .05.
aRated from 1 = less than once a year to 7 = every day.
bRated from 1 = not very close to 4 = extremely close.
cLatent construct of nine items rated from 0 = rarely or none of the time to 3 = most of the time.
dLatent construct of three items rated from 0 = never to 3 = often.
eReference category = less than high school.
fTransformed by natural log.
gSum score of 10 items coded 1 = yes and 0 = no.
*p < .05. **p < .01. ***p < .001.
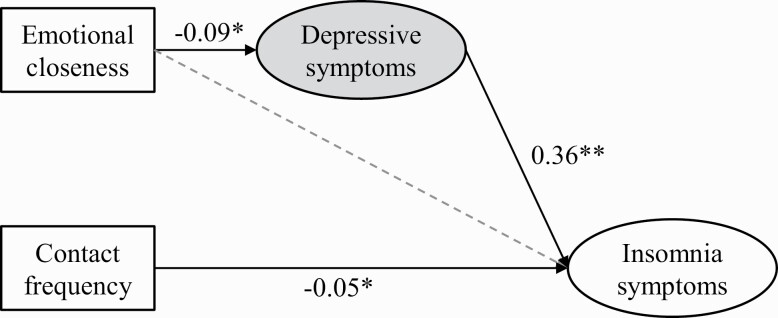
Next, regarding subjective sleep (Table 4), SEM results revealed that more frequent contact with children was associated with fewer insomnia symptoms among older adults (B = −0.05, p = .016). Additionally, older adults with more depressive symptoms reported more insomnia symptoms (B = 0.36, p = .003). Emotional closeness was not directly related to self-reported sleep duration or insomnia symptoms. In the mediation analysis for older adults’ subjective sleep, we found one significant indirect effect of emotional closeness with children on insomnia symptoms through depressive symptoms (B = −0.04, 95% CI = [−0.08 to −0.01]); thus, older adults who had greater emotional closeness with children reported fewer depressive symptoms (B = −0.09, p = .019), and fewer depressive symptoms were associated with fewer insomnia symptoms (B = 0.36, p = .003). Figure 1 illustrated the mediation results.
Table 4.
Structural Equation Model Results for Parent–Child Relationships and Older Parents’ Subjective Sleep Characteristics
| Sleep duration | Insomnia symptoms | |||
|---|---|---|---|---|
| Variables | B | (SE) | B | (SE) |
| Parent–child relationships | ||||
| Contact frequencya | 0.01 | (0.07) | −0.05* | (0.02) |
| Emotional closenessb | 0.13 | (0.12) | 0.02 | (0.04) |
| Psychological well-being | ||||
| Depressive symptomsc | −0.19 | (0.25) | 0.36** | (0.12) |
| Lonelinessd | −0.24 | (0.14) | 0.07 | (0.04) |
| Sociodemographic characteristics | ||||
| Age | 0.00 | (0.01) | 0.00 | (0.00) |
| Female | −0.14 | (0.14) | 0.05 | (0.04) |
| Racial/ethnic minority | −0.43* | (0.16) | −0.02 | (0.05) |
| Education | ||||
| High school or equivalente | −0.05 | (0.21) | −0.01 | (0.06) |
| Some collegee | −0.32 | (0.20) | −0.03 | (0.06) |
| Bachelor or moree | 0.06 | (0.23) | −0.09 | (0.07) |
| Married | 0.13 | (0.15) | −0.01 | (0.04) |
| Household incomef | −0.00 | (0.02) | 0.00 | (0.01) |
| Number of living children | −0.07 | (0.04) | 0.01 | (0.01) |
| Number of chronic diseasesg | −0.01 | (0.05) | 0.05** | (0.02) |
| Intercept | 6.53*** | (0.92) | — |
Notes: N = 548. Model fit: comparative fit index = .91, root mean square error of estimation = .04. Intercept for insomnia symptoms was omitted because insomnia symptoms were estimated as a latent construct with four items.
aRated from 1 = less than once a year to 7 = every day.
bRated from 1 = not very close to 4 = extremely close.
cLatent construct of nine items rated from 0 = rarely or none of the time to 3 = most of the time.
dLatent construct of three items rated from 0 = never to 3 = often.
eOmitted category = less than high school.
fTransformed by natural log.
gSum score of 10 items coded 1 = yes and 0 = no.
*p < .05. **p < .01. ***p < .001.
Figure 1.
Effects of parent–child relationships on older parents’ insomnia symptoms. Notes: N = 548. Model fit: comparative fit index = .90, root mean square error of estimation = .04. Only present unstandardized coefficients significant at p < .05. The solid lines indicate significant direct paths and the dash lines indicate nonsignificant paths. The indirect effect of emotional closeness on insomnia symptoms through depressive symptoms; B = −0.04, 95% CI = [−0.08 to −0.01]. *p < .05. **p < .01.
In addition, earlier studies suggested that both long and short sleep duration are risk factors for poor health and mortality. As such, the association between parent–child relationships and sleep duration may be nonlinear (U-shaped) rather than linear. To address this issue, we conducted sensitivity analyses recommended by Chen et al. (2015) by transforming self-reported and actigraph-estimated total sleep time into ordinal variables with three categories: short sleep duration (shorter than 7 h), intermediate sleep duration (7–9 h), and long sleep duration (longer than 9 h). We used multinomial logistic regressions to examine the association of parent–child relationships with the odds of short sleep duration and long sleep duration and found no significant association between parent–child contact frequency and emotional closeness and sleep duration (both self-reported and actigraph-measured).
Finally, we conducted further analyses to check the stability of our results by examining models with the full 11-item CES-D scale (including items for sleep quality and loneliness). Generally, results from this analysis were very similar to our findings based on the nine-item of CES-D scale. However, the indirect effect of parent–child emotional closeness on insomnia symptoms via depressive symptoms became marginally significant (B = −0.03, 95% CI = [−0.07 to 0.00]).
Discussion
This study examined the association between parent–child relationships and objective and subjective sleep characteristics among U.S. older adults. The investigation of depressive symptoms and loneliness contributed to a better understanding of psychological mechanisms linking parent–child relationships and sleep among older adults. The innovative design of the NSHAP actigraphy sleep data allowed for an in-depth investigation of the association between intergenerational relationships and two dimensions of sleep in later life. This study adds to the existing literature on the social determinants of sleep that previously focused mostly on subjective aspects of sleep among younger adults. Given the importance of sleep for overall well-being, examining whether psychosocial factors contributed to more healthy sleep may help identify intervention opportunities to enhance the welfare of older adults.
Overall, we found that emotional closeness with children was associated with objective measures of sleep among older adults. Specifically, older adults with closer relationships with their children showed less sleep fragmentation and a higher percentage of sleep. This finding was in line with earlier studies demonstrating the benefits of supportive social relationships for sleep outcomes among older adults (Ailshire & Burgard, 2012; Kent et al., 2015). Although results did not show significant associations between contact frequency and objective measures of sleep, contact frequency with children was directly related to older adults’ insomnia symptoms.
These findings raise questions about why emotional closeness directly benefited objectively measured sleep but not subjective evaluations of sleep, and why contact frequency was only associated with subjective reports of sleep but not objectively measured sleep. On the one hand, research has shown that frequent contacts with children are related to parents’ better daily mood (Fingerman et al., 2016), which is more strongly associated with subjective evaluations of sleep quality than actigraph-measured sleep, especially among healthy persons (Konjarski et al., 2018). Moreover, people may self-report poor sleep if they wake up in a bad mood, but they may actually have regular objective sleep (van den Berg et al., 2009; Lauderdale et al., 2008).
On the other hand, parent–child emotional closeness was more strongly associated with parents’ sleep than the frequency of contact with children. We found emotional closeness was both directly associated with objective sleep and indirectly related to subjective sleep among older parents. Unlike contact frequency which is a quantitative measure, emotional closeness measures the quality of parent–child relationships. Support from social network members consistently shows benefits for both objective and subjective sleep (Troxel et al., 2010). Our findings of different associations of parent–child closeness with the two dimensions of sleep cohere with a prior study on marital relationships and sleep (Chen et al., 2015). Chen et al. (2015) found that the benefits of marriage for older adults’ sleep were primarily driven by positive aspects of marital relationships, and such effects were more robust and evident for objective sleep characteristics than for subjective sleep quality. One possible explanation is that the benefits of positive family relationships for older adults’ sleep are best captured by objective sleep measures because actigraph-measured sleep characteristics are intrinsically more sensitive to small episodes of disruption during the night, which study respondents may not be aware of upon waking up. Thus, respondents may have enjoyed better sleep associated with positive family relations. However, their enhanced sleep quality was only recorded by the more sensitive actigraphy measures, while respondents may not be aware of and report small improvements in their subjective sleep quality.
Our findings regarding different associations between parent–child relationships (i.e., contact frequency and emotional closeness) and the two measures of sleep add to the literature. People may experience disrupted objective sleep but they are not aware of it and thus do not report this in their subjective evaluations of their sleep. Furthermore, it is likely that people report insomnia symptoms but nevertheless experienced normal levels of objective sleep. Many psychophysical factors, such as personality, mood, and memory, are likely related differently to the two dimensions of sleep and thus we see differences in the associations between parent–child relationships and objective and subjective indicators of sleep quantify and quality (Harvey & Tang, 2012). In summary, our study results demonstrate that parent–child relationships are related to different dimensions of sleep (i.e., objective and subjective). Future research should further explore the multidimensional feature of these sleep constructs when examining social determinants of sleep.
In addition, the research design for this study prevents us from making causal inferences regarding our results. Other studies also found conflicting results regarding social participation and older adult’s sleep quality using both cross-sectional and longitudinal designs (Chen et al., 2016). It is possible that more frequent contact contributes to better objective sleep over longer periods of time. Increased parent–child closeness may also lead to enhanced subjective sleep quality across longer observation periods. These possibilities should also be explored when longitudinal data of parent–child relations and sleep become available.
In our investigation of the psychological pathways linking parent–child relationships and parents’ sleep, we found that emotional closeness with children was indirectly associated with insomnia symptoms via older adults’ depressive symptoms. This result is consistent with previous studies examining psychological linkages between overall social relations and sleep among adult adults (Kent et al., 2015). In multigenerational families, older adults with closer relations with children had fewer depressive symptoms and fewer depressive symptoms are further related to better subjective sleep quality. This finding highlights the importance of considering family relations for older adults’ sleep health, as well as the need for appropriate psychological evaluation and intervention programs for older adults with sleep problems.
Limitations and Future Research Directions
Limitations of this study are acknowledged. First, causal inferences cannot be made in part because of the cross-sectional design. Also, omitted variables may potentially influence the association and/or the direction of the relationship between exposure and outcome variables. Second, this study considered the mean value of relationships with all reported children. Studies have shown substantial within-family variations in relationship quality across multiple parent–child ties (Ward, 2008). The aggregated parent–child relationships at the family level may be biased by the most favored or problematic tie. Thus, future research should investigate how relationships with each child are associated with parents’ sleep. Moreover, this study used the mean score of actigraphy measures across 3 days. Future studies using daily diary data or more repeated observations may provide better insights into the association between parent–child relationships and insomnia symptoms among older adults.
Conclusion
This study contributed to an increased understanding of social determinants of sleep by examining how parent–child relationships were related to objective and subjective sleep among U.S. older parents. Results of this study suggested emotional closeness with children was related to better objective sleep characteristics and fewer subjective insomnia symptoms for older parents. In addition, we found depressive symptoms as a psychological pathway linking parent–child closeness and older parents’ subjective sleep quality. Findings suggested that family counselors and physicians should consider the role of intergenerational relationships in improving sleep quality among older adults who have difficulties with sleeping.
Supplementary Material
Acknowledgments
We thank the National Opinion Research Center (NORC) for providing the National Social life, Health and Aging Project (NSHAP) data. The NSHAP data are publicly available through the National Archive of Computerized Data on Aging (https://www.icpsr.umich.edu/web/NACDA/series/706).
Funding
H. Wang acknowledges support from the National Institute on Aging (1R01AG060949); the Pennsylvania State University Population Research Institute, which is supported by an infrastructure grant by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2C-HD041025). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or other funding sources.
Conflict of Interest
None declared.
References
- Ailshire, J. A., & Burgard, S. A. (2012). Family relationships and troubled sleep among U.S. adults: Examining the influences of contact frequency and relationship quality. Journal of Health and Social Behavior, 53(2), 248–262. doi: 10.1177/0022146512446642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen, E. M., Malmgren, J. A., Carter, W. B., & Patrick, D. L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine, 10(2), 77–84. doi: 10.1016/S0749-3797(18)30622-6 [DOI] [PubMed] [Google Scholar]
- van den Berg, J. F., Miedema, H. M., Tulen, J. H., Hofman, A., Neven, A. K., & Tiemeier, H. (2009). Sex differences in subjective and actigraphic sleep measures: A population-based study of elderly persons. Sleep, 32(10), 1367–1375. doi: 10.1093/sleep/32.10.1367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo, J. T., Hawkley, L. C., Berntson, G. G., Ernst, J. M., Gibbs, A. C., Stickgold, R., & Hobson, J. A. (2002). Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science, 13(4), 384–387. doi: 10.1111/1467-9280.00469 [DOI] [PubMed] [Google Scholar]
- Chen, J.-H., Lauderdale, D. S., & Waite, L. J. (2016). Social participation and older adults’ sleep. Social Science and Medicine (1982), 149, 164–173. doi: 10.1016/j.socscimed.2015.11.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, J.-H., Waite, L. J., & Lauderdale, D. S. (2015). Marriage, relationship quality, and sleep among U.S. older adults. Journal of Health and Social Behavior, 56(3), 356–377. doi: 10.1177/0022146515594631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung, J. (2017). Social support, social strain, sleep quality, and actigraphic sleep characteristics: Evidence from a national survey of US adults. Sleep Health, 3(1), 22–27. doi: 10.1016/j.sleh.2016.10.003 [DOI] [PubMed] [Google Scholar]
- Fingerman, K. L., Kim, K., Birditt, K. S., & Zarit, S. H. (2016). The ties that bind: Midlife parents’ daily experiences with grown children. Journal of Marriage and Family, 78(2), 431–450. doi: 10.1111/jomf.12273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman, K. L., Sechrist, J., & Birditt, K. (2013). Changing views on intergenerational ties. Gerontology, 59(1), 64–70. doi: 10.1159/000342211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould, C. E., Karna, R., Jordan, J., Kawai, M., Hirst, R., Hantke, N., Pirog, S., Cotto, I., Schussler-Fiorenza Rose, S. M., Beaudreau, S. A., & O’Hara, R. (2018). Subjective but not objective sleep is associated with subsyndromal anxiety and depression in community-dwelling older adults. The American Journal of Geriatric Psychiatry, 26(7), 806–811. doi: 10.1016/j.jagp.2018.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner, M. A., Patel, N. P., Gehrman, P. R., Xie, D., Sha, D., Weaver, T., & Gooneratne, N. (2010). Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Medicine, 11(5), 470–478. doi: 10.1016/j.sleep.2009.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulia, K. K., & Kumar, V. M. (2018). Sleep disorders in the elderly: A growing challenge. Psychogeriatrics, 18(3), 155–165. doi: 10.1111/psyg.12319 [DOI] [PubMed] [Google Scholar]
- Hall, M. H. (2010). Behavioral medicine and sleep: Concepts, measures, and methods. In Steptoe A. (Ed.), Handbook of behavioral medicine (pp. 749–765). Springer. [Google Scholar]
- Harvey, A. G., & Tang, N. K. (2012). (Mis)perception of sleep in insomnia: A puzzle and a resolution. Psychological Bulletin, 138(1), 77–101. doi: 10.1037/a0025730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley, L. C., & Cacioppo, J. T. (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley, L. C., Preacher, K. J., & Cacioppo, J. T. (2010). Loneliness impairs daytime functioning but not sleep duration. Health Psychology, 29(2), 124–129. doi: 10.1037/a0018646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, J. M., Song, Y., Fung, C. H., Dzierzewski, J. M., Mitchell, M. N., Jouldjian, S., Josephson, K. R., Alessi, C. A., & Martin, J. L. (2018). Measuring sleep in vulnerable older adults: A comparison of subjective and objective sleep measures. Clinical Gerontologist, 41(2), 145–157. doi: 10.1080/07317115.2017.1408734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, M. E., Waite, L. J., Hawkley, L. C., & Cacioppo, J. T. (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. doi: 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackowska, M., Ronaldson, A., Brown, J., & Steptoe, A. (2016). Biological and psychological correlates of self-reported and objective sleep measures. Journal of Psychosomatic Research, 84, 52–55. doi: 10.1016/j.jpsychores.2016.03.017 [DOI] [PubMed] [Google Scholar]
- Jenkins, C. D., Stanton, B.-A., Niemcryk, S. J., & Rose, R. M. (1988). A scale for the estimation of sleep problems in clinical research. Journal of Clinical Epidemiology, 41(4), 313–321. doi: 10.1016/0895-4356(88)90138-2 [DOI] [PubMed] [Google Scholar]
- Kahn, M., Sheppes, G., & Sadeh, A. (2013). Sleep and emotions: Bidirectional links and underlying mechanisms. International Journal of Psychophysiology, 89(2), 218–228. doi: 10.1016/j.ijpsycho.2013.05.010 [DOI] [PubMed] [Google Scholar]
- Kent, R. G., Uchino, B. N., Cribbet, M. R., Bowen, K., & Smith, T. W. (2015). Social relationships and sleep quality. Annals of Behavioral Medicine, 49(6), 912–917. doi: 10.1007/s12160-015-9711-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline, R. B. (2016). Principles and practice of structural equation modeling (4th ed.). The Guilford Press. [Google Scholar]
- Konjarski, M., Murray, G., Lee, V. V., & Jackson, M. L. (2018). Reciprocal relationships between daily sleep and mood: A systematic review of naturalistic prospective studies. Sleep Medicine Reviews, 42, 47–58. doi: 10.1016/j.smrv.2018.05.005 [DOI] [PubMed] [Google Scholar]
- Koropeckyj-Cox, T. (2002). Beyond parental status: Psychological well-being in middle and old age. Journal of Marriage and Family, 64(4), 957–971. doi: 10.1111/j.1741-3737.2002.00957.x [DOI] [Google Scholar]
- Krueger, P. M., & Friedman, E. M. (2009). Sleep duration in the United States: A cross-sectional population-based study. American Journal of Epidemiology, 169(9), 1052–1063. doi: 10.1093/aje/kwp023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landry, G. J., Best, J. R., & Liu-Ambrose, T. (2015). Measuring sleep quality in older adults: A comparison using subjective and objective methods. Frontiers in Aging Neuroscience, 7, 166. doi: 10.3389/fnagi.2015.00166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale, D. S., Chen, J.-H., Kurina, L. M., Waite, L. J., & Thisted, R. A. (2017). Sleep duration and health among older adults: Associations vary by how sleep is measured. Journal Epidemiology and Community Health, 70(4), 361–366. doi: 10.1136/jech-2015-206109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale, D. S., Knutson, K. L., Yan, L. L., Liu, K., & Rathouz, P. J. (2008). Self-reported and measured sleep duration: How similar are they? Epidemiology, 19(6), 838–845. doi: 10.1097/EDE.0b013e318187a7b0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale, D. S., Schumm, L. P., Kurina, L. M., McClintock, M., Thisted, R. A., Chen, J.-H., & Waite, L. (2014). Assessment of sleep in the national social life, health, and aging project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(Suppl. 2), 125–133. doi: 10.1093/geronb/gbu092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J. H., Chopik, W. J., & Schiamberg, L. B. (2017). Longitudinal associations between marital quality and sleep quality in older adulthood. Journal of Behavioral Medicine, 40(5), 821–831. doi: 10.1007/s10865-017-9850-2 [DOI] [PubMed] [Google Scholar]
- Lippman, S., Gardener, H., Rundek, T., Seixas, A., Elkind, M. S. V., Sacco, R. L., Wright, C. B., & Ramos, A. R. (2017). Short sleep is associated with more depressive symptoms in a multi-ethnic cohort of older adults. Sleep Medicine, 40, 58–62. doi: 10.1016/j.sleep.2017.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lye, D. N. (1996). Adult child–parent relationships. Annual Review of Sociology, 22, 79–102. doi: 10.1146/annurev.soc.22.1.79 [DOI] [Google Scholar]
- Mikulincer, M., & Shaver, P. R. (2005). Attachment security, compassion, and altruism. Current Directions in Psychological Science, 14(1), 34–38. doi: 10.1111/j.0963-7214.2005.00330.x [DOI] [Google Scholar]
- Miner, B., & Kryger, M. H. (2017). Sleep in the aging population. Sleep Medicine Clinics, 12(1), 31–38. doi: 10.1016/j.jsmc.2016.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel, N. P., Grandner, M. A., Xie, D., Branas, C. C., & Gooneratne, N. (2010). “Sleep disparity” in the population: Poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health, 10, 475. doi: 10.1186/1471-2458-10-475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin, L. I. (2010). The life course and the stress process: Some conceptual comparisons. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65(2), 207–215. doi: 10.1093/geronb/gbp106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reczek, C., & Zhang, Z. (2016). Parent–child relationships and parent psychological distress: How do social support, strain, dissatisfaction, and equity matter? Research on Aging, 38(7), 742–766. doi: 10.1177/0164027515602315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teo, A. R., Choi, H., Andrea, S. B., Valenstein, M., Newsom, J. T., Dobscha, S. K., & Zivin, K. (2015). Does mode of contact with different types of social relationships predict depression in older adults? Evidence from a nationally representative survey. Journal of the American Geriatrics Society, 63(10), 2014–2022. doi: 10.1111/jgs.13667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits, P. A. (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145–161. doi: 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- Tosi, M., & Grundy, E. (2019). Intergenerational contacts and depressive symptoms among older parents in Eastern Europe. Aging and Mental Health, 23(6), 686–692. doi: 10.1080/13607863.2018.1442412 [DOI] [PubMed] [Google Scholar]
- Troxel, W. M., Buysse, D. J., Hall, M., & Matthews, K. A. (2009). Marital happiness and sleep disturbances in a multi-ethnic sample of middle-aged women. Behavioral Sleep Medicine, 7(1), 2–19. doi: 10.1080/15402000802577736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel, W. M., Buysse, D. J., Monk, T. H., Begley, A., & Hall, M. (2010). Does social support differentially affect sleep in older adults with versus without insomnia? Journal of Psychosomatic Research, 69(5), 459–466. doi: 10.1016/j.jpsychores.2010.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite, L. J., Cagney, K. A., Dale, W., Huang, E., Laumann, E. O., McClintock, M. K., O’Muircheartaigh, C. A., Schumm, L. P., & Cornwell, B. (2019). National Social Life, Health, and Aging Project (NSHAP): Wave 2 and Partner Data Collection, 2010–2011. Inter-university Consortium for Political and Social Research [distributor], 2019-06-19. doi: 10.3886/ICPSR34921.v4 [DOI] [Google Scholar]
- Wang, H., Kim, K., Burr, J. A., & Wu, B. (2020). Longitudinal associations between parent–child relationship quality and insomnia for aging parents: The mediating role of depressive symptoms. Social Science and Medicine, 253, 112972. doi: 10.1016/j.socscimed.2020.112972 [DOI] [PubMed] [Google Scholar]
- Ward, R. A. (2008). Multiple parent–adult child relations and well-being in middle and later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(4), 239–247. doi: 10.1093/geronb/63.4.s239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, R., Deane, G., & Spitze, G. (2014). Life-course changes and parent-adult child contact. Research on Aging, 36(5), 568–602. doi: 10.1177/0164027513510325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai, L., Zhang, H., & Zhang, D. (2015). Sleep duration and depression among adults: A meta-analysis of prospective studies. Depression and Anxiety, 32(9), 664–670. doi: 10.1002/da.22386 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.