Abstract
Introduction and importance
Gastric pneumatosis with concurrent hepatic portal vein gas is an extremely rare condition in the adult population. It can be idiopathic or associated with well-known etiologies. Gastric outlet obstruction can progressively inflate the stomach and cause pneumatosis. Regarding abdominal signs and the presence of acute abdomen, management varies from just conservative to emergent surgical interventions.
Case presentation
We introduce an adult patient who presented to our hospital with weakness and dyspnea. After initial measures, unexpectedly we found intraabdominal free gas, concurrent gastric pneumatosis, and aeroportia. Due to the absence of positive abdominal signs, the patient was treated successfully without any surgical or endoscopic interventions.
Discussion
Gastric outlet obstruction is a well-known cause of gastric pneumatosis. Progressive dilation of the stomach due to pyloric stenosis is well-described both in infants and adult populations.
Conclusion
In stable patients, gastric drainage and correction of electrolyte disturbance are the only required treatment. However endoscopic and surgical interventions should be considered in unstable patients or those developing acute abdomen.
Keywords: Gastric pneumatosis, Aeroportia, Gastric outlet obstruction, Gastric emphysema, Pneumoperitoneum
Highlights
-
•
A 41-year-old man presented to us with weakness, fatigue, and electrolyte imbalance, and diagnosed as gastric pneumatosis.
-
•
Upper endoscopy showed a dilated stomach due to gastric outlet obstruction.
-
•
In the CT, gastric pneumatosis and portal vein gas were found.
-
•
After correction of electrolyte imbalance, we could treat the case without any surgical intervention.
-
•
Good clinical results and recovery of the patient were obtained.
1. Introduction
Gastric pneumatosis, also known as gastric emphysema is defined as the presence of air inside the stomach wall. A variety of known etiologies have been described in the literature including gastric outlet obstruction, trauma, severe vomiting, and ischemia [1]. This entity usually does not require surgical treatment because patients are hemodynamically stable and do not show any signs of acute abdomen [2]. It may be accompanied by some other nonspecific disorders such as the presence of air inside the biliary tree [3]. Hereby, we introduce an adult patient with repetitive vomiting and severe electrolyte disturbance who developed severe gastric pneumatosis associated with pneumobilia. We reported the case in line with the Surgical Case Report (SCARE) guidelines [4].
2. Case presentation
A 41-year-old man presented to our emergency department with weakness, fatigue, dyspnea, and a history of repetitive vomiting in the past few days. He also mentioned a history of weight loss in recent months without any other alarming symptoms. The patient was a heavy smoker and addicted to opioids and he had no positive findings in family history and physical examination. Due to his abnormal electrocardiogram (long QT-interval) he was admitted and initial blood tests were requested. Laboratory data showed severe electrolyte imbalances such as hyponatremia, hypokalemia, and compensated metabolic alkalosis (Table 1). Although chest x-ray was normal (Fig. 1), we performed a low-dose lung computed tomography (CT) due to the COVID-19 outbreak in the country. The results showed that both lungs were uninvolved but we found some gas in the abdominal cavity. Since the patient had no abdominal signs in physical examination, we decided to perform an abdominopelvic CT with IV and oral contrasts (Fig. 2, Fig. 3). Unexpectedly, we found a huge stomach that was extended to the level of the umbilicus. Also, there was some gas inside the stomach wall, biliary tree, and even abdominal cavity.
Table 1.
Laboratory findings.
| Laboratory variable | Before treatment | After treatment |
|---|---|---|
| Arterial blood gas | ||
| pH | 7.605 | 7.433 |
| pCO2 | 59.7 | 39.7 |
| HCO3− | 50.5 | 25.8 |
| Electrolytes | ||
| Potassium | 119 | 139 |
| Sodium | 2.0 | 4.1 |
Fig. 1.
Normal chest x-ray.
Fig. 2.
CT, axial views. Red arrows indicate gas inside the stomach wall or biliary tract. These three progressive views show the extent of stomach volume and pneumatosis. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
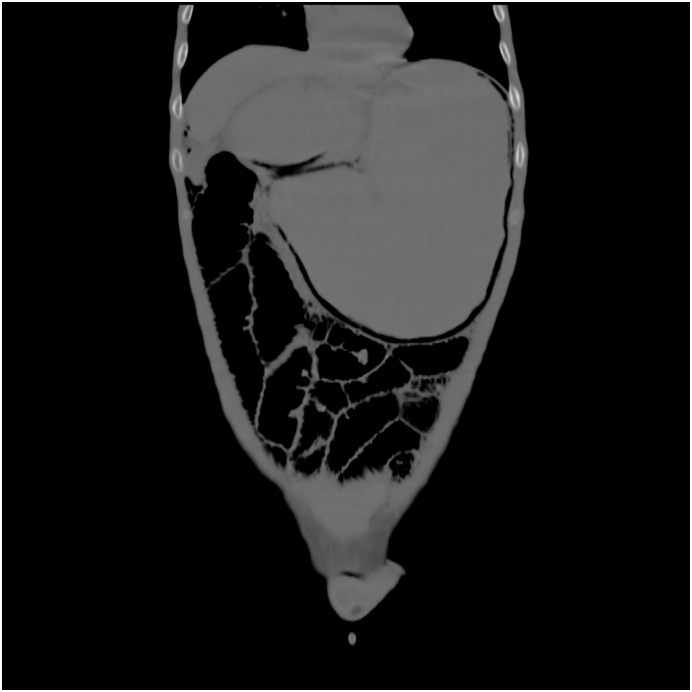
CT, coronal view shows a huge stomach with pneumatosis inside its wall.
According to these findings, a nasogastric tube was inserted immediately and about 2 l of gastric juice was drained. Also, electrolyte disturbance was corrected properly. Due to the absence of abdominal tenderness, we just observed the patient. Upper gastrointestinal endoscopy was performed during his first days of admission and the diagnosis was gastric outlet obstruction due to inflammation; then, biopsies were taken. Conservative management with a high dose of intravenous pantoprazole was performed. The patient could eat orally on the third day and was discharged with appropriate oral medications.
3. Discussion
Gastric pneumatosis is a rare clinical entity and is defined as the presence of air inside the stomach wall. It may be associated with portal venous gas or pneumoperitoneum [5]. Although it is well-described in infants and in the context of hypertrophic pyloric stenosis [6], there are fewer reports associated with this condition in the adult population. Diagnosis is usually made by CT scan and the presence of air in the gastric wall. Because of its silent course and absence of peritoneal signs, it is usually treated conservatively, and surgical exploration is rarely needed.
There are some major well-known causes for this disorder such as gastric outlet obstruction, trauma, or ischemia. Gastric outlet obstruction can be secondary to other conditions like malignancy, pyloric stenosis, volvulus and also duodenal stenosis [7]. The pathophysiology of this disease is not known precisely. However, excessive dilation of the stomach seems to allow air to enter its wall. It can rupture into the peritoneal cavity and develop peritonitis or it can penetrate microscopically without the development of acute abdomen. Also, it can move into the biliary tree via different routes [8]. Noninvasive management is almost always recommended [2], [3], [5]; however, endoscopic treatment has been described well by some authors [9]. According to a comparative review conducted in 2018, the short-term prognosis of conservative management seems to be good and further imaging and endoscopic follow-ups are recommended [1].
4. Conclusion
Gastric emphysema with concurrent hepatic portal vein gas seems to be a benign intra-abdominal condition. In hemodynamically stable patients, it rarely requires surgical treatment and can be managed conservatively. Also, if the underlying condition is recognized, it is better to treat that entity. If gastric outlet obstruction is the major cause of gastric emphysema, endoscopic follow-ups should be considered.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of the journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Funding
The authors did not receive any financial support for this report.
Guarantor
Dr. Manoochehr Ebrahimian.
Research registration number
Not applicable.
CRediT authorship contribution statement
ME: Study design. SR: Case presentation. NG: Data gathering and writing manuscript.
All authors read and approved the final manuscript.
Declaration of competing interest
The authors declared no potential conflict of interests with respect to the research, authorship, and/or publication of this article.
Acknowledgments
None.
Contributor Information
Manoochehr Ebrahimian, Email: manoochehrebrahimian@sbmu.ac.ir.
Negin Ghayebi, Email: negin.gh71@gmail.com.
Seyed Parviz Rezaee, Email: dr.parvizrezaee@gmail.com.
References
- 1.Inayat F., Zafar F., Zaman M.A., Hussain Q. Gastric emphysema secondary to severe vomiting: a comparative review of 14 cases. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2018-226594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Y.-G., Dai M.-S. Man with nausea and vomiting. Ann. Emerg. Med. 2012;60(2):250. doi: 10.1016/j.annemergmed.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Pichon L., Poncelet P.A. Perigastric and portal venous gas induced by vomiting. J. Belg. Soc. Radiol. 2020;104(1):75. doi: 10.5334/jbsr.2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., et al. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Allaparthi S.B., Anand C.P. Acute gastric dilatation: a transient cause of hepatic portal venous gas-case report and review of the literature. Case Rep. Gastrointest. Med. 2013;2013 doi: 10.1155/2013/723160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Travadi J.N., Patole S.K., Simmer K. Gastric pneumatosis in neonates: revisited. J. Paediatr. Child Health. 2003;39(7):560–562. doi: 10.1046/j.1440-1754.2003.00220.x. [DOI] [PubMed] [Google Scholar]
- 7.Pauli E.M., Tomasko J.M., Jain V., Dye C.E., Haluck R.S. Multiply recurrent episodes of gastric emphysema. Case reports in surgery. 2011;2011 doi: 10.1155/2011/587198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Misro A., Sheth H. Diagnostic dilemma of gastric intramural air. Ann.R.Coll.Surg.Engl. 2014;96(7):e11–e13. doi: 10.1308/003588414X13946184901128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Honda H., Ikeya T., Kashiwagi E., Okada S., Fukuda K. Successful emergency endoscopic treatment of gastric outlet obstruction due to gastric bezoar with gastric pneumatosis. Case Rep. Gastroenterol. 2017;11(3):718–723. doi: 10.1159/000484130. [DOI] [PMC free article] [PubMed] [Google Scholar]




