Abstract
Background: This systematic review and meta-analysis aim to synthesize the extant literature reporting the effects of COVID-19 pandemic based on the pooled prevalence of depression among affected populations in Asia Pacific, as well as its risk factors.
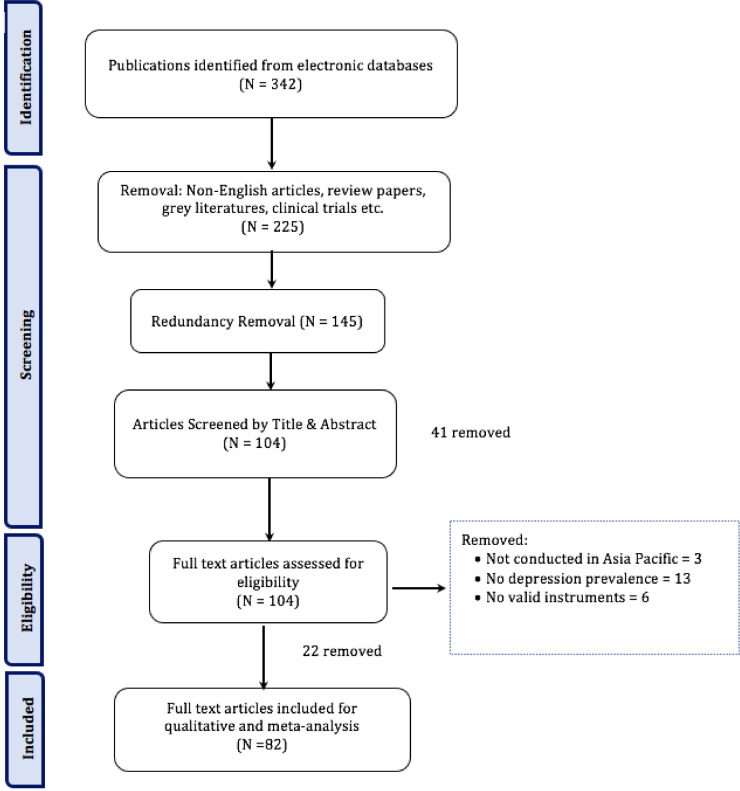
Method: A systematic review and meta-analysis approach was adopted as per the PRISMA guidelines, targeting articles published in PubMed, Google Scholar and Scopus from January 2021 to March 30, 2021. The screening resulted in 82 papers.
Results: The overall pooled depression prevalence among 201,953 respondents was 34% (95%CI, 29–38, 99.7%), with no significant differences observed between the cohorts, timelines, and regions (p > 0.05). Dominant risk factors found were fear of COVID-19 infection (13%), gender (i.e., females; 12%) and deterioration of underlying medical conditions (8.3%), regardless of the sub-groups. Specifically, fear of COVID-19 infection was the most reported risk factor among general population (k = 14) and healthcare workers (k = 8). Gender (k = 7) and increased workload (k = 7) were reported among healthcare workers whereas education disruption among students (k = 7).
Limitation: The review is limited to articles published in three electronic databases.
Conclusion The pandemic has caused depression among the populations across Asia Pacific, specifically among the general population, healthcare workers and students. Immediate attention and interventions from the concerned authorities are needed in addressing this issue.
Keywords: COVID-19, Depression, Asia Pacific, Systematic review, meta-analysis
1. Introduction
The Coronavirus disease 2019 (COVID-19) was first reported in December 2019 after a cluster of atypical cases of pneumonia was reported in Wuhan, China. It was subsequently characterized as a pandemic by the World Health Organization (WHO) on March 11, 2020 (World Health Organization, 2020). The latest data as of September 2021 indicate over 200 million1 positive cases worldwide, with 54.2 million2 cases in Asia Pacific region alone.
It has been widely reported that the on-going pandemic is compromising physical health, as well as mental health including elevated stress, anxiety, distress and depression caused by uncertainties, fear of COVID-19 infection, increasing work pressure, and lockdowns etc. (Le et al., 2020; Wong et al., 2021b). These adverse mental health effect has been observed worldwide, notably in the Asia Pacific region, dominantly in countries such as China where the first COVID-19 case was reported in 2019 (Hao et al., 2021; Peng et al., 2021; Yan et al., 2021). Currently, many countries in this region are experiencing a spike in daily positive cases, most of which linked to the highly transmissible Delta variant that was first detected in India.
Evidence exists showing elevated depression prevalence across the COVID-19 affected populations in Asia Pacific, for instance, Wong et al. (2021b) examined the level of mental health among Malaysian adults using different timelines ranging from May 2020 to September 2020, with results indicating depression prevalence to have increased overwhelmingly as the pandemic progressed. In fact, the authors found depression to have the highest prevalence (59.2%) compared to anxiety (55.1%) and stress (30.6%). Another study in China targeting the healthcare workers (HCWs) also reported a high depression prevalence of 50.9% (H. Wang et al., 2021a).
Studies have also reported depression prevalence among various cohorts including HCWs (Matsumoto et al., 2021; Young et al., 2021), general population (Liu et al., 2020; Veldhius et al., 2021), students (Wu et al., 2021a; R. Yadav et al., 2021b), and further identified risk factors contributing to increased depression (Tee et al., 2021; Wickens et al., 2021; Yan et al., 2021). Further, a search of the literature revealed meta-analytics indicating estimated pooled prevalence of depression of 22.8% among HCWs in Asian countries in May 2020 (Pappa et al., 2020) whilst another review among global HCWs conducted in November 2020 reported a higher overall prevalence of depression of 40% (Saragih et al., 2021).
As evidence shows that depression prevalence to have increased as the time progressed, there is a need to update and extend the literature to encompass more recent studies, particularly a year after the beginning of the COVID-19 pandemic across the affected population. This systematic review and meta-analysis aim to (a) analyze the pooled prevalence of depression among the affected populations in Asia Pacific, (b) compare the prevalence among the highly affected cohorts, and (c) identify the risk factors based on cohorts and regions.
2. Materials and method
The current review follows the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (Moher et al., 2009), and the protocol has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) to avoid duplication. The review is a sub-study of a much larger project, hence the steps presented in the subsequent sections are specifically for this review.
2.1. Search strategy
Scholarly publications related to COVID-19 and mental health were sought from three electronic databases, namely, PubMed, Google Scholar and Scopus, from January 2021 and March 2021. Numerous keywords manipulated with Boolean and wildcard operators were used in the search strategy, including “mental health and pandemic”, “mental health and C*”, “mental health and outbreak” and “mental health and epidemic”. In addition, specific keywords were also replaced (e.g., “mental health” with mental issues, stress*, depression, anxiety, emotion* and psycho*), resulting in more than 35 different combinations. This resulted in a total of 208 articles.
2.2. Eligibility criteria
The Population, Issue of interest, Comparison, Outcome, and Study design (PICOS) (Liberati et al., 2009) approach was adopted to determine the eligibility criteria. The inclusion criteria were: (i) journals published between January 2021 and March 2021, (ii) written in English and targeting Asia Pacific (including multi-country studies), (iii) online surveys (cross-sectional, longitudinal etc.), (iv) the use of validated research instruments for mental health assessments, and (v) report prevalence of depression. Studies not meeting the PICOS criteria, gray literatures, book chapters, reviews and short communications, clinical trials, etc. were excluded. Four authors were involved in screening the articles, and further determining the suitability of the studies based on the titles and abstracts. In instances where the inclusion criteria were unclear, the reviewers checked the full text before a decision is made. This stage resulted in a total of 82 articles (see Fig. 1 ).
Fig. 1.
PRISMA flowchart.
2.3. Data extraction
Four authors independently performed the data extraction which involves the mapping of the articles in terms of quantity, characteristics and sources of evidence in accordance with the aim of this review. This includes details such as author, year, country, sample cohort, sample size, age, timeline of the study, scales/instrument, depression prevalence results and risk factors.
2.4. Quality assessment
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline that assesses cross-sectional studies for risk of bias was used to determine the quality of the articles (von Elm et al., 2007). According to STROBE, risk of bias is deemed to be low if the study reported sufficient data for quality assessment and fulfilled the criteria for the quality item, partial if incomplete data for the quality item were reported, or high if the study reported sufficient data for quality assessment but didn't fulfill the criteria for the quality item.
2.5. Statistical analysis
Statistical heterogeneity was assessed using (Higgins, 2003), in which proportions of 25%, 50%, and 75% indicate low, moderate, and high heterogeneity, respectively along with random-effects meta-analysis to pool the raw data. Between group analysis was done to examine the differences in the pooled prevalence between the cohorts (i.e., populations), regions, and timelines using a series of random-effects meta-analysis models. Cochran's Q test was used to compare the statistical significance of the subgroup differences (Wu et al., 2021a, b). All the results are considered significant at p < 0.05. Publication bias was assessed using the Egger's regression (Egger et al., 1997) and visual assessment of funnel plots. The analyses were done using JASP (0.14.1.0), an open-source tool for statistical analysis.
3. Results
3.1. Study characteristics
All the studies included in the systematic review and meta-analysis were conducted using online surveys, somewhat expected considering the worldwide lockdowns due to the COVID-19 pandemic. As shown in Table 1 , a vast majority of the studies were conducted in China (41%) as the virus was first detected in this nation, followed by the USA (15.7%). A further categorization of the countries based on the regions indicate slightly more than half of the studies were conducted in East Asia (50.6%), followed by North America (22.9%) and South Asia (18.1%). The top three cohorts were the general population (39.8%), (HCWs (27.7%), and students (18%). The rest of the cohorts include patients with pre-existing medical conditions (e.g., mental health disorder, cancer, COVID-19 etc.) with eight studies in total, one involving COVID-19 quarantined individuals (Kang et al., 2021), and one targeting children (Glynn et al., 2021). These cohorts were regrouped as Others for the between group analysis. As for the study instruments, the Patient Health Questionnaire (PHQ) and its variants emerged to be most popular (53%), followed by the Depression, Anxiety, and Stress Scale (DASS)−21 (18.1%) and Center for Epidemiological Studies Depression (CESD) (12%). The study timelines ranged between January and December 2020. The complete analysis can be found in Supplementary 1.
Table 1.
Study characteristics of the papers reviewed.
| Region | N (%) | Country | N (%) | Cohort | N (%) |
| East Asia | 41 (50.0) | China | 33 (40.2) | General Population | 32 (39.0) |
| Japan | 5 (6.1) | Healthcare Workers | 23 (28.1) | ||
| Hong Kong | 2 (2.4) | Students | 15 (18.3) | ||
| South Korea | 1 (1.2) | Others | 12 (14.6) | ||
| North America | 19 (23.2) | USA | 13 (15.9) | ||
| Canada | 6 (7.3) | Scale | |||
| South Asia | 15 (18.2) | Bangladesh | 7 (8.5) | PHQ | 43 (52.4) |
| India | 4 (4.9) | DASS −21 | 16 (19.5) | ||
| Nepal | 3 (3.7) | CESD | 10 (12.2) | ||
| Sri Lanka | 1 (1.2) | SDS | 5 (6.1) | ||
| HADS | 3 (3.7) | ||||
| Oceania | 4 (4.9) | Australia | 4 (4.89) | Others | 5 (6.1) |
| Southeast Asia | 3 (3.7) | Malaysia | 3 (3.7) |
Note: PHQ: Patient Health Questionnaire; DASS-21: Depression, Anxiety, and Stress Scale; CESD: Center for Epidemiological Studies Depression; SDS: Self-rating Depression Scale; HADS: Hospital Anxiety and Depression Scale; Others: Beck's Depression Inventory; Edinburgh Postpartum Depression Scale; Geriatric Depression Scale; Quick Inventory of Depressive Symptomatology; Short Mood and Feelings Questionnaire.
3.2. Publication bias
The visual assessment of the funnel plot indicates low publication bias (Supplementary 2), which was confirmed by the Egger's test (p = 0.249).
3.3. Quality assessment
All the studies fulfilled most of the criteria in the STROBE checklist (Supplementary 3). However, of these four did not specify timeline, 10 did not describe limitations, 43 did not provide sample size calculations, 47 had limited generalizability and 23 did not disclose information on financial support. This may justify the low-risk bias present in the studies as shown in the funnel plot (Supplementary 2).
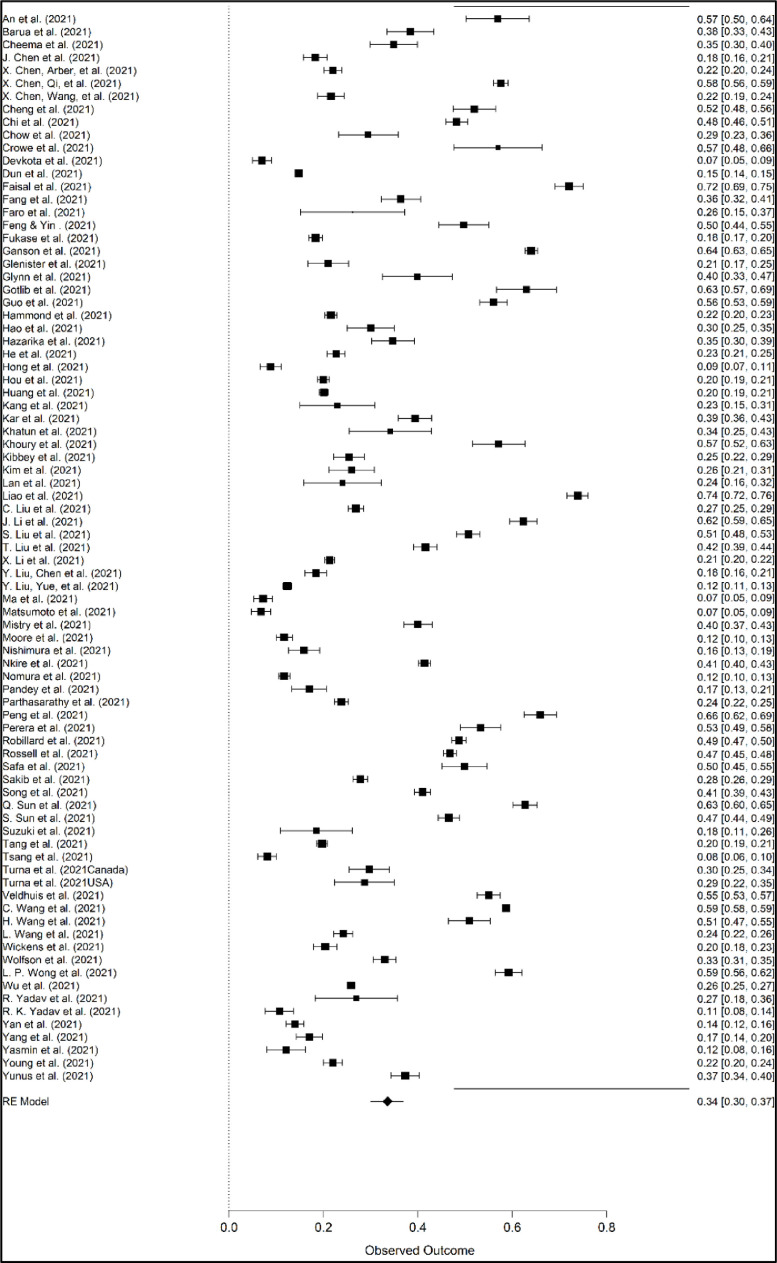
3.4. Depression prevalence
The prevalence of depression was analyzed in 82 studies, with 201, 953 respondents. The overall pooled prevalence of depression was 34% (95% CI: 29.0 –38.0%), ranging between 6.8% and 73.85% (Fig. 2 ). The I2 value of 99.7% also indicates a high degree of heterogeneity, a pattern that is commonly reported among systematic review and meta-analyses studies due to the varying methodologies, experimentations and scales adopted within each individual study (Böger et al., 2021; Levin et al., 2020; Wu et al., 2021b).
Fig. 2.
Forest plot for depression pooled prevalence.
3.5. Between group analysis
We performed between group analyses based on the cohorts, timelines and regions, and the results are shown in Table 2 .
Table 2.
Between group analyses.
| Categories | Number of Studies (k) | Pooled Prevalence | CI | I2 | Q | P-value | |
|---|---|---|---|---|---|---|---|
| Overall | Overall | 83 | 34 | 29–38 | 99.742 | ||
| Cohort | HCW | 23 | 34 | 29–39 | 99.431 | 0.254 | 0.968 |
| GP | 33 | 34 | 27–42 | 99.832 | |||
| Students | 15 | 34 | 25–42 | 99.838 | |||
| Others | 12 | 31 | 20–42 | 98.289 | |||
| Region | East Asia | 42 | 33 | 26–39 | 99.845 | 0.929 | 0.92 |
| South Asia | 15 | 32 | 24–41 | 99.281 | |||
| Southeast Asia | 3 | 42 | 24–60 | 98.55 | |||
| North America | 4 | 31 | 15–47 | 99.257 | |||
| Oceania | 19 | 36 | 27–45 | 99.458 | |||
| Timeline | Jan - Apr | 45 | 36 | 30–42 | 99.785 | 1.06 | 0.589 |
| May - Aug | 32 | 31 | 24–38 | 99.679 | |||
| Sept - Dec | 2 | 30 | 29–38 | 96.235 | |||
Note: HCW: Healthcare workers; GP: General population.
The pooled prevalence of depression among cohorts (k = 4, N = 83) for HCWs, General population, Students and Others were 34% (95% C1:29–39%), 34% (95% C1:27–42%), 34% (95% C1:25–42%) and 31% (95% C1:20–42%), respectively. The Q-statistics indicate no significant differences between the depression levels for each cohort (p > 0.05). A similar observation was noted for regions (k = 5, N = 83) with p > 0.05. Finally, the pooled prevalence of depression between different timelines (k = 3, N = 78) indicate most studies were conducted during the early phase of the outbreak (Jan - Mar 2020) resulting in a pooled prevalence of 36% CI 95% [30%; 42%]. However, no significant differences were observed between the timelines (p > 0.05). Results of the between group analysis are attached as Supplementary 4.
3.6. Risk factors
Dominant risk factors for depression revealed to be fear of COVID-19 infection (13%), gender (females, 12%) and deterioration of underlying medical conditions (8.3%). Others include income disruption, lack of social support, increased workload, job security, job burnout etc. Table 3 provides the details whereas the complete analysis is presented in Supplementary 5.
Table 3.
Risk factors for depression.
3.6.1. Risk factors between cohorts
Fear of COVID-19 infection (13%) emerged to be the most common risk factor for depression among all the cohorts (k = 33), especially within the general population (k = 14). As for the students, the disruption of education (k = 7) was identified as the most evident risk factor whilst the HCW listed gender (k = 7) and increased workload (k = 7) as risk factors apart from fear of COVID-19 infection (k = 8). Interestingly, among the COVID-19 infected cohort, the factor that was identified as a risk for depression was isolation and lack of community support (k = 2). Others include high stress levels (k = 4), lack of access to medical attention (k = 3), being away from family (k = 3), food security (k = 3), past trauma (k = 2), addictive behavior (k = 2), stigmatization (k = 2), sexuality (k = 1) and parental mental condition (k = 1).
3.6.2. Risk factors between regions
Dominant risk factors for countries within the Asian region (East Asia, South Asia, Southeast Asia) were fear of COVID-19 infection (k = 25), gender (k = 22) and deterioration of underlying medical conditions (k = 15). East Asia recorded the highest number of studies (k = 18) identifying fear of COVID-19 infection as a risk factor for depression. The major risk factors in North America and Oceania were age (k = 9), gender, fear of infection (k = 8) and income disruption/financial restraint (k = 6). Similar to risk factors between cohorts, the common risk factors identified within the Asia Pacific region was the fear of COVID-19 infection (k = 33), gender (k = 30) and deterioration in underlying medical conditions (k = 21).
4. Discussion
This systematic review and meta-analysis analyzed the pooled prevalence of depression among populations in Asia Pacific and identified its risk factors. Further analysis indicates depression was more common among women, younger adults, unmarried individuals, people with lower socioeconomic status, and those who were at high risk of COVID-19 infection (suspected/confirmed cases, living in a hard-hit area etc.). Furthermore, data indicates that increased familial and social support, as well as learning effective coping method aid in lowering the likelihood of depression.
Our overall pooled prevalence of depression (34%) was found to be in coherent with Wang et al. (2020) and Luo et al. (2020) who reported prevalence of 30% and 28%, respectively based on their meta-analyses on the general population. A further examination of the subgroups revealed no significant differences between the cohorts and depression prevalence, in line with Spoorthy et al. (2020). Studies related to mental health conditions of HCWs revealed that they were more likely to develop posttraumatic stress disorder compared to depression due to the conditions they had to deal with daily throughout this pandemic (Liu et al., 2020a; Spoorthy et al., 2020). Nevertheless, a deeper investigation needs to be administered to examine the non-differential levels of depression amongst HCWs and the general population to determine if the former is suppressing their emotions due to obligations of being front liners.
No significant differences were observed between regions as well with regards to the depression prevalence, although studies have revealed residents who are closer to ground zero tend to be at a higher risk of depression (DePierro et al., 2020; Han et al., 2021). This shows that the mental well-being of the population across Asia Pacific is affected similarly, regardless of the country of residence. This could also be attributed to different risk factors contributing to the decline in their mental health, such as living in isolation among residents in East Asia (Fang et al., 2021; Kang et al., 2021) and lack of access to medical attention as hospitals were full with COVID-19 patients for those within the Oceania region (Cheema et al., 2021; Glenister et al., 2021).
Fear of COVID-19 infection was found to be the most dominant risk factors, regardless of the cohorts, timelines, and regions. This was somewhat expected as new information regarding the virus was being discovered as it progressed (X. Chen et al., 2021b), coupled with the fear of the unknown that was further exacerbated by information overload due to a greater access to COVID-19 information through social media (Hong et al., 2021; Sakib et al., 2021; B. Ye et al., 2020a, b). The risk factor was also found to be commonly reported among HCWs, probably because they dealing with a virus they had minimal knowledge about with looming fear that they may infect their family members (Feng et al., 2021; Hammond et al., 2021; Matsumoto et al., 2021). Furthermore, the drastic increase in the number of patients as well as increased workload also led to an elevated depression among the HCWs (Crowe et al., 2021; Parthasarathy et al., 2021; Perera et al., 2021).
Students in Asia Pacific generally reported concern due to disruption to their education, a phenomenon not only evident among those at the tertiary level but also amongst students in secondary and primary levels as they were struggling to cope with online classes, and the challenges that come with it (Chi et al., 2021; Gotlib et al., 2021; Nishimura et al., 2021). Other concern include uncertainty towards their academic future and job prospects (Ma et al., 2021; Yunus et al., 2020).
Income disruption and financial strain were identified as risk factors among countries on the Pacific region of Asia Pacific (Ganson et al., 2021; Robillard et al., 2021; Wickens et al., 2021; Wolfson et al., 2021). In fact, recent report indicates that North American countries experienced income loss by 10.3% compared to those in Asia (6.6%) (International Labor Organization, 2021). Other risk factors identified include age (younger) and gender(female) (Glenister et al., 2021; Huang et al., 2021; Veldhuis et al., 2021). This is especially evident among the Asian countries and could be attributed to the cultural gendered roles and the biological means of women resulting in them handling stressful situations differently than men (Hidayati et al., 2020). This however warrants further investigation.
5. Conclusion, recommendation, and limitations
The systematic review and meta-analysis examined the pooled prevalence of depression among the affected populations in Asia Pacific and identified the risk factors leading to an increased depression. Further, between group analyses were conducted for the cohorts, regions and timelines. The review shows prevalence of depression due to the COVID-19 pandemic, regardless of the cohorts and regions. In fact, no significant differences were observed between the groups and the depression prevalence, indicating that the pandemic has hit the Asia Pacific populations hard, psychologically. Findings also revealed some common risk factors across the studies reviewed, with fear of COVID-19 infection to be highly reported. Unique risk factors were also found for the specific cohorts. The study provides evidence for the urgent need for attention and strategic interventions providing a holistic care to the affected populations.
The prevalence, cohorts and risk factors identified in this review provide insights into the populations with higher risk of depression, hence interventions can be tailored accordingly. For example, low-intensity psychosocial interventions such as social/family/peer support, education programs, computerized self-help Cognitive Behavioral Therapy (CBT) etc., can be initiated for people with milder depression whereas high-intensity interventions (i.e., formal psychological therapies) can be initiated for those with severe depression symptoms (NICE 2009). Further, other effective treatments such as task-shifting approaches with trained counsellors (Patel et al., 2017) should be considered as well. We, therefore, propose a variety of intervention approaches coupled with telehealth to target the affected populations in Asia Pacific.
We identify several limitations. Firstly, the articles were limited to three electronic databases, hence this may have resulted in the majority of the studies reviewed to over-represent general population and HCWs. Further, all the studies were based on online surveys, resulting in most of the samples studied to be urbanites with Internet connections, thus creating a selection bias in the populations studied. Also, all the studies assessed depression through self-reported questionnaires, and thus may have brought bias to an overestimation/underestimation of the prevalence of depression. A high heterogeneity rate was also observed in this study probably due to the various measurement instruments and scales adopted with varying cut-off points, cohorts as well as different regions across the Asia Pacific. Therefore, the results should be interpreted with caution. Further, a vast majority of the studies were from China (40%), thus probably contributing to the high heterogeneity in the results. This could also be attributed to the disproportionate sample populations investigated, instruments with varying cut-off points etc.
Author's contribution
Balakrishnan - designed the study, screening, visualization, drafting manuscript, manuscript revision; Ng - designed the study, screening, drafted the manuscript; Wandeep - article search, data extraction and screening; Kumanan - article search, data extraction and screening; Lek - article search, data extraction and screening.
Funding
We received no funding for this study.
Declaration of competing interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgement
None
Footnotes
https://www.worldometers.info/coronavirus/
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.11.048.
Appendix. Supplementary materials
References
- An R., Chen X., Wu Y., Liu J., Deng C., Liu Y., Guo H. A survey of postpartum depression and health care needs among Chinese postpartum women during the pandemic of COVID-19. Arch. Psychiatr. Nurs. 2021;35(2):172–177. doi: 10.1016/j.apnu.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barua L., Zaman M.S., Omi F.R., Faruque M. Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: a cross-sectional study. F1000Research. 2020:9. doi: 10.12688/f1000research.27189.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böger B., Fachi M.M., Vilhena R.O., Cobre A.F., Tonin F.S., Pontarolo R. Systematic review with meta-analysis of the accuracy of diagnostic tests for COVID-19. Am. J. Infect. Control. 2021;49(1):21–29. doi: 10.1016/j.ajic.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheema M., Mitrev N., Hall L., Tiongson M., Ahlenstiel G., Kariyawasam V. Depression, anxiety and stress among patients with inflammatory bowel disease during the COVID-19 pandemic: australian national survey. BMJ Open Gastroenterol. 2021;8(1) doi: 10.1136/bmjgast-2020-000581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Liu X., Wang D., Jin Y., He M., Ma Y., Zhao X., Song S., Zhang L., Xiang X. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc. Psychiatry Psychiatr. Epidemiol. 2021;56(1):47–55. doi: 10.1007/s00127-020-01954-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Wang L., Liu L., Jiang M., Wang W., Zhou X., Shao J. Factors associated with psychological distress among patients with breast cancer during the COVID-19 pandemic: a cross-sectional study in Wuhan, China. Support. Care Cancer. 2021:1–10. doi: 10.1007/s00520-021-05994-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C., Wang H.-y., Ebrahimi O.V. Adjustment to a “new normal:” Coping flexibility and mental health issues during the COVID-19 pandemic. Front. Psychiatry. 2021;12:353. doi: 10.3389/fpsyt.2021.626197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi X., Liang K., Chen S.T., Huang Q., Huang L., Yu Q., Jiao C., Guo T., Stubbs B., Hossain M.M. Problemas de salud mental en adolescentes chinos durante el COVID-19: importancia de la nutrición y la actividad física. Int. J. Clin. Health Psychol. 2021 doi: 10.1016/j.ijchp.2020.100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe S., Howard A.F., Vanderspank-Wright B., Gillis P., McLeod F., Penner C., Haljan G. The effect of COVID-19 pandemic on the mental health of Canadian critical care nurses providing patient care during the early phase pandemic: a mixed method study. Intensive Crit. Care Nurs. 2021;63 doi: 10.1016/j.iccn.2020.102999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePierro J., Lowe S., Katz C. Lessons learned from 9/11: mental health perspectives on the COVID-19 pandemic. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.113024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devkota H.R., Sijali T.R., Bogati R., Ahmad M., Shakya K.L., Adhikary P. The impact of COVID-19 on mental health outcomes among hospital fever clinic attendants across Nepal: a cross-sectional study. PLoS ONE. 2021;16(3) doi: 10.1371/journal.pone.0248684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dun Y., Ripley-Gonzalez J.W., Zhou N., Li Q., Chen M., Hu Z., Zhang W., Thomas R.J., Olson T.P., Liu J. The association between prior physical fitness and depression in young adults during the COVID-19 pandemic—A cross-sectional, retrospective study. PeerJ. 2021;9:e11091. doi: 10.7717/peerj.11091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faisal R.A., Jobe M.C., Ahmed O., Sharker T. Mental health status, anxiety, and depression levels of Bangladeshi university students during the COVID-19 pandemic. Int. J. Ment. Health Addict. 2021:1–16. doi: 10.1007/s11469-020-00458-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang X.-.H., Wu L., Lu L.-.S., Kan X.-.H., Wang H., Xiong Y.-.J., Ma D.-.C., Wu G.-.C. Mental health problems and social supports in the COVID-19 healthcare workers: a Chinese explanatory study. BMC Psychiatry. 2021;21(1):1–8. doi: 10.1186/s12888-020-02998-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faro J.M., Mattocks K.M., Nagawa C.S., Lemon S.C., Wang B., Cutrona S.L., Sadasivam R.S. Physical activity, mental health, and technology preferences to support cancer survivors during the COVID-19 pandemic: cross-sectional study. JMIR Cancer. 2021;7(1):e25317. doi: 10.2196/25317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng L., Yin R. Social support and hope mediate the relationship between gratitude and depression among front-line medical staff during the pandemic of COVID-19. Front. Psychol. 2021;12:579. doi: 10.3389/fpsyg.2021.623873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukase Y., Ichikura K., Murase H., Tagaya H. Depression, risk factors, and coping strategies in the context of social dislocations resulting from the second wave of COVID-19 in Japan. BMC Psychiatry. 2021;21(1):1–9. doi: 10.1186/s12888-021-03047-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganson K.T., Tsai A.C., Weiser S.D., Benabou S.E., Nagata J.M. Job insecurity and symptoms of anxiety and depression among US young adults during COVID-19. J. Adolesc. Health. 2021;68(1):53–56. doi: 10.1016/j.jadohealth.2020.10.008. [DOI] [PubMed] [Google Scholar]
- Glenister K.M., Ervin K., Podubinski T. Detrimental health behaviour changes among females living in rural areas during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2021;18(2):722. doi: 10.3390/ijerph18020722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn L.M., Davis E.P., Luby J.L., Baram T.Z., Sandman C.A. A predictable home environment may protect child mental health during the COVID-19 pandemic. Neurobiol. Stress. 2021;14 doi: 10.1016/j.ynstr.2020.100291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib I.H., Borchers L.R., Chahal R., Gifuni A.J., Teresi G.I., Ho T.C. Early life stress predicts depressive symptoms in adolescents during the COVID-19 pandemic: the mediating role of perceived stress. Front. Psychol. 2021;11:3864. doi: 10.3389/fpsyg.2020.603748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo W.-.P., Min Q., Gu W.-.W., Yu L., Xiao X., Yi W.-.B., Li H.-.L., Huang B., Li J.-.L., Dai Y.-.J. Prevalence of mental health problems in frontline healthcare workers after the first outbreak of COVID-19 in China: a cross-sectional study. Health Qual. Life Outcomes. 2021;19(1):1–10. doi: 10.1186/s12955-021-01743-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond N.E., Crowe L., Abbenbroek B., Elliott R., Tian D.H., Donaldson L.H., Fitzgerald E., Flower O., Grattan S., Harris R. Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers' depression, anxiety, and stress levels. Aust. Crit. Care. 2021;34(2):146–154. doi: 10.1016/j.aucc.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X., Chen S., Bi K., Yang Z., Sun P. Depression following COVID-19 lockdown in severely, moderately, and mildly impacted areas in China. Front Psychiatry. 2021;12:154. doi: 10.3389/fpsyt.2021.596872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao W., Tang Q., Huang X., Ao L., Wang J., Xie D. Analysis of the prevalence and influencing factors of depression and anxiety among maintenance dialysis patients during the COVID-19 pandemic. Int. Urol. Nephrol. 2021;53(7):1453–1461. doi: 10.1007/s11255-021-02791-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazarika M., Das S., Bhandari S.S., Sharma P. The psychological impact of the COVID-19 pandemic and associated risk factors during the initial stage among the general population in India. Open J. Psychiatry Allied Sci. 2021;12(1):31. doi: 10.5958/2394-2061.2021.00009.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Q., Ren J., Wang G., Zhang J., Xiang J., He D. Psychological effects of the COVID-19 outbreak on nurses working in tertiary women’s and children’s hospitals from Sichuan, China: a cross-sectional study. Int. J. Disaster Risk Reduct. 2021;58 doi: 10.1016/j.ijdrr.2021.102188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hidayati I., Tan W., Yamu C. How gender differences and perceptions of safety shape urban mobility in Southeast Asia. Transp. Res. Part F: Traffic Psychol. Behav. 2020;73:155–173. [Google Scholar]
- Higgins J.P.T. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong W., Liu R.D., Ding Y., Fu X., Zhen R., Sheng X. Social media exposure and college students’ mental health during the outbreak of COVID-19: the mediating role of rumination and the moderating role of mindfulness. Cyberpsychol. Behav. Soc. Netw. 2021;24(4):282–287. doi: 10.1089/cyber.2020.0387. [DOI] [PubMed] [Google Scholar]
- Hou W.K., Lee T.M.-C., Liang L., Li T.W., Liu H., Ettman C.K., Galea S. Civil unrest, COVID-19 stressors, anxiety, and depression in the acute phase of the pandemic: a population-based study in Hong Kong. Soc. Psychiatry Psychiatr. Epidemiol. 2021:1–10. doi: 10.1007/s00127-021-02037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Labor Organization. (2021). Retrieved from https://www.ilo.org/wcmsp5/groups/public/—dgreports/—dcomm/documents/briefingnote/wcms_767028.pdf.
- Kang E., Lee S.Y., Kim M.S., Jung H., Kim K.H., Kim K.-.N., Park H.Y., Lee Y.J., Cho B., Sohn J.H. The psychological burden of COVID-19 stigma: evaluation of the mental health of isolated mild condition COVID-19 patients. J. Korean Med. Sci. 2021;36(3) doi: 10.3346/jkms.2021.36.e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kar N., Kar B., Kar S. Stress and coping during COVID-19 pandemic: result of an online survey. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury J.E., Atkinson L., Bennett T., Jack S.M., Gonzalez A. COVID-19 and mental health during pregnancy: the importance of cognitive appraisal and social support. J. Affect. Disord. 2021;282:1161–1169. doi: 10.1016/j.jad.2021.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kibbey M.M., Fedorenko E.J., Farris S.G. Anxiety, depression, and health anxiety in undergraduate students living in initial US outbreak “hotspot” during COVID-19 pandemic. Cogn. Behav. Ther. 2020:1–13. doi: 10.1080/16506073.2020.1853805. [DOI] [PubMed] [Google Scholar]
- Kim S.C., Quiban C., Sloan C., Montejano A. Predictors of poor mental health among nurses during COVID-19 pandemic. Nursing Open. 2021;8(2):900–907. doi: 10.1002/nop2.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan F.-.Y., Suharlim C., Kales S.N., Yang J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the USA. Occup. Environ. Med. 2021;78(4):237–243. doi: 10.1136/oemed-2020-106774. [DOI] [PubMed] [Google Scholar]
- Le, H.T., Lai, A.J.X., Sun, J., Hoang, M.T., Vu, L.G., Pham, H.Q., Nguyen, T.H., Tran, B.X., Latkin, C.A., Le, X.T.T., Nguyen, T.T., Pham, Q.T., Ta, N.T.K., Nguyen, Q.T., Ho, R.C.M., & Ho, C.S.H. (2020). Anxiety and Depression Among People Under the Nationwide Partial Lockdown in Vietnam. Front. Public Health, 8. https://doi.org/10.3389/fpubh.2020.589359. [DOI] [PMC free article] [PubMed]
- Levin A.T., Hanage W.P., Owusu-Boaitey N., Cochran K.B., Walsh S.P., Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur. J. Epidemiol. 2020:1–16. doi: 10.1007/s10654-020-00698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Xu J., Zhou H., You H., Wang X., Li Y., Liang Y., Li S., Ma L., Zeng J. Working conditions and health status of 6,317 front line public health workers across five provinces in China during the COVID-19 epidemic: a cross-sectional study. BMC Public Health. 2021;21(1):1–14. doi: 10.1186/s12889-020-10146-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Liu C., Liu D., Huang N., Fu M., Ahmed J.F., Zhang Y., Wang X., Wang Y., Shahid M., Guo J. The Combined Impact of Gender and Age on Post-traumatic Stress Symptoms, Depression, and Insomnia During COVID-19 Outbreak in China. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.620023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xu Y., Cai L., Ma S., Wang Y., Cai Z., Du H., Li R. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J. Psychiatr. Res. 2021;137:393–400. doi: 10.1016/j.jpsychires.2021.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., Idris S., Zhang Y., Zewen L., Wali A., Ji Y., Pan Q., Baloch Z. The impact of COVID-19 pandemic outbreak on education and mental health of Chinese children aged 7–15 years: an online survey. BMC Pediatr. 2021;21(1):1–8. doi: 10.1186/s12887-021-02550-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto Y., Fujino J., Shiwaku H., Miyajima M., Doi S., Hirai N., Jitoku D., Takagi S., Tamura T., Maruo T. Factors affecting mental illness and social stress in hospital workers treating COVID-19: paradoxical distress during pandemic era. J. Psychiatr. Res. 2021;137:298–302. doi: 10.1016/j.jpsychires.2021.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistry S.K., Ali A.M., Hossain M.B., Yadav U.N., Ghimire S., Rahman M.A., Irfan N.M., Huque R. Exploring depressive symptoms and its associates among Bangladeshi older adults amid COVID-19 pandemic: findings from a cross-sectional study. Soc. Psychiatry Psychiatr. Epidemiol. 2021:1–11. doi: 10.1007/s00127-021-02052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore S.E., Wierenga K.L., Prince D.M., Gillani B., Mintz L.J. Disproportionate impact of the COVID-19 pandemic on perceived social support, mental health and somatic symptoms in sexual and gender minority populations. J. Homosex. 2021;68(4):577–591. doi: 10.1080/00918369.2020.1868184. [DOI] [PubMed] [Google Scholar]
- NICE . National Institute for Health and Care Excellence; 2009. Overview | Depression in adults: Recognition and Management | Guidance | NICE. (2009, October 28)https://www.nice.org.uk/guidance/cg90 [PubMed] [Google Scholar]
- Nishimura Y., Ochi K., Tokumasu K., Obika M., Hagiya H., Kataoka H., Otsuka F. Impact of the COVID-19 pandemic on the psychological distress of medical students in Japan: cross-sectional survey study. J. Med. Internet Res. 2021;23(2):e25232. doi: 10.2196/25232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkire N., Mrklas K., Hrabok M., Gusnowski A., Vuong W., Surood S., Abba-Aji A., Urichuk L., Cao B., Greenshaw A.J. COVID-19 pandemic: demographic predictors of self-isolation or self-quarantine and impact of isolation and quarantine on perceived stress, anxiety, and depression. Front. Psychiatry. 2021:12. doi: 10.3389/fpsyt.2021.553468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomura K., Minamizono S., Maeda E., Kim R., Iwata T., Hirayama J., Ono K., Fushimi M., Goto T., Mishima K. Cross-sectional survey of depressive symptoms and suicide-related ideation at a Japanese national university during the COVID-19 stay-home order. Environ. Health Prev. Med. 2021;26(1):1–9. doi: 10.1186/s12199-021-00953-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey A., Sharma C., Chapagain R.H., Devkota N., Ranabhat K., Pant S., Adhikari K. Stress, anxiety, depression and their associated factors among health care workers during COVID-19 pandemic in Nepal. J. Nepal Health Res. Counc. 2021;18:655–660. doi: 10.33314/jnhrc.v18i4.3190. [DOI] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parthasarathy R., Jaisoorya T., Thennarasu K., Murthy P. Mental health issues among health care workers during the COVID-19 pandemic–a study from India. Asian J. Psychiatr. 2021;58 doi: 10.1016/j.ajp.2021.102626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Weobong B., Weiss H.A., Anand A., Bhat B., Katti B., Dimidjian S., Araya R., Hollon S.D., King M., Vijayakumar L., Park A.L., McDaid D., Wilson T., Velleman R., Kirkwood B.R., Fairburn C.G. The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. Lancet North Am. Ed. 2017;389(10065):176–185. doi: 10.1016/s0140-6736(16)31589-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng X., Meng X.-.Y., Li L., Hu C., Liu W., Liu Z., Ma X., Xu D., Xing Z., Zhu Z. Psychological effects of COVID-19 on ICU healthcare workers: an online cross-sectional study in China. Front. Public Health. 2021;9:39. doi: 10.3389/fpubh.2021.603273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera B., Wickramarachchi B., Samanmalie C., Hettiarachchi M. Psychological experiences of healthcare professionals in Sri Lanka during COVID-19. BMC Psychol. 2021;9(1):1–9. doi: 10.1186/s40359-021-00526-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashid M., Alam M., Talukder A., Rahman Razu S., Ward P.R., Ali M. Mental health of physicians during COVID-19 outbreak in Bangladesh: a web-based cross-sectional survey. Front. Public Health. 2021;9:10. doi: 10.3389/fpubh.2021.592058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robillard R., Daros A.R., Phillips J.L., Porteous M., Saad M., Pennestri M.-.H., Kendzerska T., Edwards J.D., Solomonova E., Bhatla R. Emerging New Psychiatric Symptoms and the Worsening of Pre-existing Mental Disorders during the COVID-19 Pandemic: a Canadian Multisite Study: nouveaux symptômes psychiatriques émergents et détérioration des troubles mentaux préexistants durant la pandémie de la COVID-19: une étude canadienne multisite. Canad. J. Psychiatry. 2021 doi: 10.1177/0706743720986786. 0706743720986786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossell S.L., Neill E., Phillipou A., Tan E.J., Toh W.L., Van Rheenen T.E., Meyer D. An overview of current mental health in the general population of Australia during the COVID-19 pandemic: results from the COLLATE project. Psychiatry Res. 2021;296 doi: 10.1016/j.psychres.2020.113660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safa F., Anjum A., Hossain S., Trisa T.I., Alam S.F., Rafi M.A., Podder V., Koly K.N., Azad D.T., Ahmad W.U. Immediate psychological responses during the initial period of the COVID-19 pandemic among Bangladeshi medical students. Child Youth Serv. Rev. 2021;122 doi: 10.1016/j.childyouth.2020.105912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakib N., Akter T., Zohra F., Bhuiyan A.I., Mamun M.A., Griffiths M.D. Fear of COVID-19 and depression: a comparative study among the general population and healthcare professionals during COVID-19 pandemic crisis in Bangladesh. Int. J. Ment. Health Addict. 2021:1–17. doi: 10.1007/s11469-020-00477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saragih I.D., Tonapa S.I., Saragih I.S., Advani S., Batubara S.O., Suarilah I., Lin C.J. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int. J. Nurs. Stud. 2021;121 doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song S., Yang X., Yang H., Zhou P., Ma H., Teng C., Chen H., Ou H., Li J., Mathews C.A. Psychological resilience as a protective factor for depression and anxiety among the public during the outbreak of COVID-19. Runing Title: protective factor of the public during COVID-19. Front. Psychol. 2020;11:4104. doi: 10.3389/fpsyg.2020.618509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoorthy M.S., Pratapa S.K., Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Q., Qin Q., Basta M., Chen B., Li Y. Psychological reactions and insomnia in adults with mental health disorders during the COVID-19 outbreak. BMC Psychiatry. 2021;21(1):1–10. doi: 10.1186/s12888-020-03036-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki K., Numao A., Komagamine T., Haruyama Y., Kawasaki A., Funakoshi K., Fujita H., Suzuki S., Okamura M., Shiina T. Impact of the COVID-19 Pandemic on the Quality of Life of Patients with Parkinson’s Disease and Their Caregivers: a Single-Center Survey in Tochigi Prefecture. J. Parkinsons. Dis. 2021:1–10. doi: 10.3233/JPD-212560. (Preprint) [DOI] [PubMed] [Google Scholar]
- Tang S., Xiang M., Cheung T., Xiang Y.-.T. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J. Affect. Disord. 2021;279:353–360. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tee M., Wang C., Tee C., Pan R., Reyes P.W., Wan X., Anlacan J., Tan Y., Xu L., Harijanto C., Kuruchittham V., Ho C., Ho R. Impact of the COVID-19 pandemic on physical and mental health in lower and upper middle-income Asian countries: a comparison between the Philippines and China. Front. Psychiatry. 2021;11 doi: 10.3389/fpsyt.2020.568929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang S., Avery A.R., Duncan G.E. Fear and depression linked to COVID-19 exposure A study of adult twins during the COVID-19 pandemic. Psychiatry Res. 2021;296 doi: 10.1016/j.psychres.2020.113699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turna J., Zhang J., Lamberti N., Patterson B., Simpson W., Francisco A.P., Bergmann C.G., Van Ameringen M. Anxiety, depression and stress during the COVID-19 pandemic: results from a cross-sectional survey. J. Psychiatr. Res. 2021;137:96–103. doi: 10.1016/j.jpsychires.2021.02.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veldhuis C.B., Nesoff E.D., McKowen A.L.W., Rice D.R., Ghoneima H., Wootton A.R., Papautsky E.L., Arigo D., Goldberg S., Anderson J.C. Addressing the critical need for long-term mental health data during the COVID-19 pandemic: changes in mental health from April to September 2020. Prev. Med. 2021;146 doi: 10.1016/j.ypmed.2021.106465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies*. Bull. World Health Organ. 2007;85(11):867–872. doi: 10.2471/blt.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Dai X., Yao Z., Zhu X., Jiang Y., Li J., Han B. The prevalence and risk factors for depressive symptoms in frontline nurses under COVID-19 pandemic based on a large cross-sectional study using the propensity score-matched method. BMC Psychiatry. 2021;21(1):1–10. doi: 10.1186/s12888-021-03143-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Kala M.P., Jafar T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS ONE. 2020;15(12) doi: 10.1371/journal.pone.0244630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Shi L., Que J., Lu Q., Liu L., Lu Z., Xu Y., Liu J., Sun Y., Meng S. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol. Psychiatry. 2021:1–10. doi: 10.1038/s41380-021-01019-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickens C.M., Hamilton H.A., Elton-Marshall T., Nigatu Y.T., Jankowicz D., Wells S. Household-and employment-related risk factors for depressive symptoms during the COVID-19 pandemic. Canad. J. Public Health. 2021;112(3):391–399. doi: 10.17269/s41997-020-00472-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson J.A., Garcia T., Leung C.W. Food insecurity is associated with depression, anxiety, and stress: evidence from the early days of the COVID-19 pandemic in the United States. Health Equity. 2021;5(1):64–71. doi: 10.1089/heq.2020.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong L.P., Alias H., Md Fuzi A.A., Omar I.S., Mohamad Nor A., Tan M.P., Baranovich D.L., Saari C.Z., Hamzah S.H., Cheong K.W. Escalating progression of mental health disorders during the COVID-19 pandemic: evidence from a nationwide survey. PLoS ONE. 2021;16(3) doi: 10.1371/journal.pone.0248916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Tao S., Zhang Y., Li S., Ma L., Yu Y., Sun G., Li T., Tao F. Geographic distribution of mental health problems among Chinese college students during the COVID-19 pandemic: nationwide, web-based survey study. J. Med. Internet Res. 2021;23(1):e23126. doi: 10.2196/23126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav R., Yadav P., Kumar S.S., Kumar R. Assessment of Depression, Anxiety, and Sleep Disturbance in COVID-19 Patients at Tertiary Care Center of North India. J. Neurosci. Rural. Pract. 2021;12(02):316–322. doi: 10.1055/s-0040-1722811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan T., Zhizhong W., Jianzhong Z., Yubo Y., Jie L., Junjun Z., Guangtian L. Depressive and anxiety symptoms among people under quarantine during the COVID-19 epidemic in China: a cross-sectional study. Front. Psychiatry. 2021;12:9. doi: 10.3389/fpsyt.2021.566241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Xiao Y., Liu Y., Li Q., Shan C., Chang S., Jen P.H.-S. Mental Health and Psychological Impact on Students with or without Hearing Loss during the Recurrence of the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health. 2021;18(4):1421. doi: 10.3390/ijerph18041421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasmin S., Alam M.K., Ali F.B., Banik R., Salma N. Psychological Impact of COVID-19 Among People from the Banking Sector in Bangladesh: a Cross-Sectional Study. Int. J. Ment. Health Addict. 2021:1–15. doi: 10.1007/s11469-020-00456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye B., Zhou X., Im H., Liu M., Wang X.Q., Yang Q. Epidemic rumination and resilience on college students’ depressive symptoms during the COVID-19 pandemic: the mediating role of fatigue. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.560983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young K.P., Kolcz D.L., O'Sullivan D.M., Ferrand J., Fried J., Robinson K. Health care workers’ mental health and quality of life during COVID-19: results from a mid-pandemic, national survey. Psychiatr. Serv. 2021;72(2):122–128. doi: 10.1176/appi.ps.202000424. [DOI] [PubMed] [Google Scholar]
- Yunus W.M.A.W.M., Badri S.K.Z., Panatik S.A., Mukhtar F. The unprecedented movement control order (Lockdown) and factors associated with the negative emotional symptoms, happiness, and work-life balance of malaysian university students during the coronavirus disease (COVID-19) Pandemic. Front. Psychiatry. 2020:11. doi: 10.3389/fpsyt.2020.566221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.