Abstract
Background and Objectives
There are nearly 18 million family caregivers in the United States assisting an older adult in need of help. Identifying the caregivers in greatest need of support requires an understanding of the current social support networks available to family caregivers and whether specific groups of caregivers are at risk of having an insufficient support network.
Research Design and Methods
We collected personal network data from a nationally representative sample of 66 family caregivers to persons with dementia (PWDs) in the United States aged 18 and older, including information on network members’ support to the caregiver and help to the care recipient.
Results
We found four common caregiving network types: large networks with many helpers; large networks primarily supporting caregivers; small, dense networks supporting both caregivers and care recipient; and small networks providing little help to either caregiver or care recipient. Gender, income, and geographic proximity of caregiver to the care recipient were significantly associated with caregiver network type.
Discussion and Implications
This study suggests that there are different types of care and support networks available to caregivers to PWDs, and that the size and structure of networks vary considerably among demographic groups. As the population ages, a better understanding of the supports available to caregivers will be crucial for ensuring that caregivers are adequately supported, and caregiving needs of families are met.
Keywords: Caregiving, Cluster analysis, Social networks, Social support
Around 10,000 baby boomers turn 65 each day in the United States (Cohn & Taylor, 2010). By 2050, the number of people who will need assistance with everyday activities—for example, eating, bathing, meal preparation, and transportation—is expected to double (Frank, 2012). Family and friends, referred to hereafter as family caregivers, provide the vast majority of this care (Friedman et al., 2015), often at great financial, emotional, and physical expense (National Academies of Sciences, Engineering, and Medicine, 2016). Caregivers of persons with dementia (PWDs) face an especially great burden of care. This burden can be alleviated through a strong support system—a cohesive network of family and friends who provide support both to the care recipient and directly to the caregiver—yet there is little research examining these support networks. This is surprising given that stronger networks are related to better health outcomes (Smith & Christakis, 2008). And this may be particularly true for caregivers: because social networks change along with life transitions (Cornwell & Schafer, 2016), caregiving potentially puts caregivers at risk of social isolation and worsened health.
Despite the established importance of social ties to caregivers, there is little empirical work to date on the social networks of caregivers. The small literature on this topic focuses on either small samples of caregivers in countries outside the United States or older U.S. caregivers. For instance, the literature on the social networks of older adults has examined such topics as changes in older adults’ social networks and in the relationship between social networks and health (for a review, see Ayalon & Levkovich, 2018). Less work has focused on the networks of the family members assisting older adults directly. The literature that does exist focuses either on small samples of caregivers in countries outside the United States (Cañameras, 2015; Rodríguez-Madrid et al., 2018), on older U.S. caregivers (Roth, 2020), on caregiver networks within a closed community, such as assisted living communities or those attending local adult daycare centers (Ashida et al., 2017; Koehly et al., 2015; Marcum et al., 2020), or focuses explicitly on interventions to improve support (for a review, see Dam et al., 2016).
This study makes several contributions to the literature. One of the primary contributions is that we collect personal networks of family caregivers aged 18 and older from a nationally representative panel. In addition, we ask caregivers about both their own networks and those of the people to whom they provide care, for a more complete picture of the network surrounding the caregiver–care recipient dyad, including the direct support networks to the caregivers (caregiver networks) and the indirect support that caregivers receive through help provide to the care recipient (care recipient networks). Finally, while there are a handful of papers examining the characteristics and dynamics of caregiver networks, this is the first study to identify different network prototypes of caregivers.
Our approach uses personal networks to summarize the complexity of the support networks of caregivers and identify group differences in the size and structure of these networks. Social networks are important in the caregiving context because they provide the social resources that enhance or restrain access to help with everyday activities, contacts to medical care, and health information. Although sociocentric networks (Wasserman & Faust, 1994) are often referred to as the “gold standard” in social network analysis (Bettger, 2012), they require a defined population and defined specific relations. For instance, work on this topic using that approach has examined networks in assisted living communities or those attending local adult daycare centers (Ashida et al., 2017; Koehly et al., 2015; Marcum et al., 2020). However, caregiver networks among community-dwelling individuals are not easily bounded around one social context and are likely structured as separate networks that form around a focal person receiving caregiving support. For example, a study that initially used a sociocentric approach to sample caregivers of older adults from specific facilities in one geographic area resulted in an analysis of 30 separate networks (Marcum et al., 2020).
Personal Network Approach
A personal (egocentric) network approach is a better fit for the natural formation of caregiver networks. This approach has been used to define the variety of social ties around a sample of focal individuals and has been used to measure caregiver networks (Llopsis Cañameras, 2015; Rodríguez-Madrid et al., 2018). This is appropriate for caregivers of older adults with dementia because they are not necessarily part of a clearly defined network with other similar caregivers and they are tied to other types of people. The boundaries of caregiver networks are not only less defined, but they likely evolve over time. Caregivers can experience heightened social volatility due to loss of contact with people they interacted with prior to providing intensive care; their networks may shrink over time as caregiving requires more of their time and energy; and they may lose ties to network members whom they primarily socialized with, spending more time instead with other members of the older adult’s care network. They may also lose ties because of their need to rely on their extended network for support while they provide care, and this may cause network burnout. Therefore, a personal network approach is more appropriate for caregivers because they are at the center of an evolving configuration of social relationships rather than a member of a defined group.
Personal network interviews, whether performed in person or through surveys over the internet, can be used to produce raw network data for each focal individual that can be analyzed with data analysis techniques used for whole or complete network data (McCarty, 2002; Wasserman & Faust, 1994). Analysis of raw personal network data produces complex and correlated network variables to measure network composition and structure. Multivariate data reduction techniques, such as cluster analysis (Kaufman & Rousseeuw, 2009), can summarize these variables into a small number of common prototypes (Brandes et al., 2010; Giannella & Fischer, 2016; Green et al., 2012; Kennedy et al., 2011; Vacca, 2020; Wenger, 1991). While this approach is established in networks analysis, it has not been used previously to identify the social networks of caregivers.
Current Study
This study adds to the literature on the social networks of family caregivers in three critical ways: (a) by collecting data in a nationally representative online panel study of adults in the United States aged 18 and older to identify family caregivers across the age spectrum and increase representativeness; (b) by measuring extended perceived caregiver networks, including strong connections and more distant “weaker” ties, which could inform strategic access to novel information and resources (Granovetter, 1977); (c) by identifying individuals who are not in the caregivers’ direct support networks but are available to provide indirect support through assistance to the caregiver and direct support to the care recipient (i.e., care recipient networks); and (d) by being the first study to identify different network prototypes specifically for caregivers.
We ask two primary research questions:
(1) What are the different types of social support networks available to caregivers to PWDs?
(2) What demographic and caregiving factors are correlated with each network type?
To answer these questions, we collected personal network data from a nationally representative online panel of family caregivers to PWDs in the United States aged 18 and older and ask them about their own networks and those of the PWD to whom they provide care. We use cluster analysis to help establish typologies of support and care networks (Brandes et al., 2010; Giannella & Fischer, 2016; Green et al., 2012; Kennedy et al., 2011; Vacca, 2020; Wenger, 1991) and examine demographic differences in network typologies.
Design and Methods
Data and Measures
We sampled panelists of the American Life Panel (ALP), a nationally representative online panel study of adults aged 18 and older and collected information on personal networks using EgoWeb 2.0, a specialized survey software for collecting and processing personal network data (http://egoweb.info). The ALP is a panel survey that consists of 6,000 U.S. individuals aged 18 and older who regularly take surveys over the internet. Since January 2006, the ALP has fielded more than 500 surveys on such topics as financial decision-making, retirement, health utilization, and voting preferences. The ALP has a good representation of the U.S. population, includes weights for population-level estimates, and has low rates of attrition over time (Pollard & Baird, 2017).
We conducted a pilot project to provide exploratory, empirical data on the personal networks of caregivers to older adults with dementia to examine the feasibility of collecting these data and to develop hypotheses for a larger study on social networks and caregiver burden. To identify family and friends providing unpaid care to a loved one, in November 2017, we screened about 2,500 ALP panelists who were part of the quarterly ALP Omnibus survey, and asked:
Do you provide unpaid care and assistance for, or manage the care of, a family member or friend 50 years or older who has an illness, injury or condition for which they require outside support? Unpaid care may include help with tasks such as personal care, bathing, dressing, feeding, giving medicines or treatments, transportation to doctors’ appointments, or arranging for services. This person does not need to live with you.
We then followed up with questions about their relationship to the care recipient and the condition(s) for which they are providing care. Four hundred forty panelists reported that they were providing care to a family member or friend aged 50 or older. In June/July 2018, we followed up with a subset of 150 panelists who reported that they were providing care to someone aged 50 or older with dementia by selecting dementia among a set of conditions or illnesses requiring care (n = 113), the vast majority of the sample, and a handful of others provided open-ended responses suggesting the presence of dementia (e.g., “early-stage dementia”). We re-screened the sample of 150 caregivers and conducted personal network interviews with the 66 panelists who reported that they are currently providing such care.
The personal network data collection instrument was designed to identify the broader support system available to dementia caregivers, including those providing direct social support to the caregiver and those available to provide caregiving support to the older adult with dementia. The interview included questions about the PWD (e.g., conditions and demographic characteristics), caregiver respondent (e.g., intensity of care and type of help provided), as well as questions about the network of people strongly connected to the caregiver and other people who were available to provide direct support to the PWD.
We used standard personal network interview techniques to measure the personal network of the respondent. Personal network interviews are conducted by asking a focal individual (referred to as the “ego”) to answer standardized questions about themselves and a list of people in their social environment (Crossley et al., 2015; McCarty et al., 2019; Perry et al., 2018). Caregivers first reported on demographic characteristics for themselves and the PWD to whom they provided care, including age (in years), ethnicity, and gender. Caregivers then reported how many years they have been providing care, how many hours they provide care per week, how far away they live from the PWD (in miles), and which types of support they provided (emotional, transportation, housework, financial, personal care, management of finances, and management of services). Caregiver household income was identified through responses provided to other recent ALP interviews.
To measure social network composition and structure, we first asked respondents to list people connected to themselves as well as to the PWD in order to capture a diversity of strong and weak ties available to provide direct or indirect support to the caregiver. We balanced the need to generate a sufficient number of network contacts against the increased respondent burden (Golinelli et al., 2010; McCarty, 2002) of adding each additional name by using a series of targeted questions asking respondents to list a specific number of types of people (“name generators”; Bidart & Charbonneau, 2011; Campbell & Lee, 1991; Marin & Hampton, 2007). Our goal was to elicit a list of people (referred to as “alters” in personal network terminology) connected to the caregiver either directly or indirectly through their connection to the PWD. The first question asked caregivers to name up to 10 people with whom they discussed things that were important to them. Three additional name generators asked them to name other people (up to five each) who either (a) provided them with support, (b) were in their household, or (c) were close to or provided unpaid support to the PWD. Once the respondent provided lists of names for each of these questions, we asked each network member if they provided support directly to the respondent (emotional, transportation, housework, or financial). Next, we asked respondents to indicate if each of the network members provided them with help providing support to the PWD and if the network members provided any support directly to the PWD (emotional, transportation, housework, financial, personal care, management of finances, and management of services). Finally, we asked respondents to rate how easy it would be to ask each alter for help or a break in providing support (ranging from 1 = “very difficult” to 4 = “very easy”) and used elsewhere (Ramchand et al., 2014).
For each respondent, we calculated information on three domains: (a) type and intensity of support, (b) to whom support was provided, and (c) ease at which the caregiver could get help if needed. Type and intensity of support was calculated as the proportions of alters providing each type of support divided by the total number of alters named by the respondent. To whom support was provided included three variables capturing the proportions of alters who provided each type of support to caregivers, PWDs, or only to caregivers but not PWDs directly. Finally, for the ease at which the caregiver could get help if needed, we calculated sum scores of each of the difficulty ratings.
To measure network structure, we identified the number of alters named by each respondent to measure network size. We asked respondents to identify which network members knew each other and had regular contact. Respondents provided responses for their own contact with each alter, contact between each alter and the PWD, and contact between each unique alter–alter dyad. These responses provided the raw relationship data to calculate network density (proportion of actual connections of all possible connections).
Analyses
In order to classify the caregiver personal networks, we identified discrete types of networks using cluster analysis. We ran two clustering techniques—hierarchical and k-means clustering—using the statistical software R on a distance matrix of all standardized network measures (composition and structure). We used several clustering diagnostics across these two clustering techniques, in addition to examining the resulting cluster characteristics, to determine the best number of clusters that are meaningful. We first applied the hierarchical clustering procedure using Ward’s error sum of squares variance method using the “hclust” function in the R package “stats” (Murtagh & Legendre, 2014). We also ran the “NbClust” function in the R package “NbClust” with the “kmeans” method, which produces 26 indexes of cluster fit on a range of numbers of clusters and examined the distribution (Charrad et al., 2014). After examining a histogram of the cluster by a number of best fit diagnostics, we conducted several other diagnostics to identify the best number of clusters to analyze. We produced dendrograms to visually display the level of closeness when groups of observations split into separate clusters. We also produced elbow plots of the total within-cluster sum of squares to visually identify noticeable differences between a number of clusters as well as a silhouette plot. We used these measures of cluster fit to determine the significant peak in the number of clusters that corresponded with the highest number of best fits among all of the indices. More detail of these metrics as well as the plots are provided in Supplementary Materials. Finally, we evaluated the clusters identified by the various clustering evaluation packages for meaningfulness by comparing the means of variables within the clusters to the overall mean and standard deviation to identify the network characteristics that best characterize the networks. We subtracted the within-cluster means from the overall mean and divided by the overall standard deviation to produce z-scores. To interpret the cluster, we examined which z-scores were either at or above 0.5 or at or below −0.5 standard deviations above the overall mean.
We conducted bivariate tests to determine whether the clusters were associated with characteristics of the PWD, including analysis of variances (ANOVAs) for continuous variables and chi-square tests for categorical measures. We also tested cluster differences with multinomial logistic regression models using the “multinom” function in the R package “nnet.” Because of the exploratory aims of this pilot analysis, we report significant associations at both the 90% and 95% confidence levels and do not use survey weights. The demographic characteristics of the population (e.g., caregiver and PWD age, income, race, and gender) are comparable to those using weighted data.
Results
Table 1 provides descriptive results characterizing the caregiver respondents and the PWD to whom they provided care. The PWDs, who averaged around 85 years of age, were typically the parents (or parents-in-law) of the caregivers (84%). Caregivers were around 58 years old on average. Caregivers were primarily White (84%) and female (79%) and their household incomes averaged around $58,000. Caregivers reported providing close to 4 years of care to the PWD, on average, and spending close to 4 h per week providing this care. Caregivers and PWDs lived on average around 2 miles from each other with 26% living in the same household and 24% of PWD living in a medical center, nursing home, or other care facility. Caregivers provided a variety of types of support to PWD, most frequently emotional support (89%), followed by transportation (82%), financial management (70%), and housework (59%). A minority of caregivers reported providing personal care (45%), services management (41%), and direct financial assistance (27%).
Table 1.
Characteristics of Caregivers and Persons With Dementia (N = 66)
| Characteristic type | Overall (% or mean) |
|---|---|
| Caregiver mean age (mean, SD) | 57.62 (10.23) |
| PWD mean age (mean, SD) | 84.89 (9.45) |
| Caregiver–PWD relationship | |
| Child–parent (%) | 67 |
| Child–parent-in-law | 17 |
| Grandchild–grandparent | 5 |
| Spouses | 2 |
| Siblings | 2 |
| Other | 2 |
| Caregiver % White (%) | 84 |
| Caregiver % female (%) | 79 |
| Caregiver household income (thousands of $) | 58.06 (33.62) |
| Years providing care (mean, SD) | 3.83 (3.07) |
| Hours per week of caregiving (mean, SD) | 3.79 (1.74) |
| Live in the same household as PWD (%) | 26 |
| PWD lives in a care facility (%) | 24 |
| Distance between caregiver and PWD in miles (mean, SD) | 2.06 (1.95) |
| Mean count of types of support provided by caregivers (mean, SD) | 4.06 (1.45) |
| Type of support provided by the caregiver | |
| Emotional (%) | 89 |
| Transportation (%) | 82 |
| Housework (%) | 59 |
| Giving direct financial assistance (%) | 27 |
| Personal care (%) | 45 |
| Financial management (%) | 70 |
| Services management (%) | 41 |
Note: PWD = person with dementia.
After we examined the various metrics for best cluster fit (Supplementary Material), we considered two possible cluster solutions: the two-cluster solution and the four-cluster solution. The four-cluster solution produced the highest number of best fit metrics (10) from NbClust with the two-cluster solution next highest (8). The two-cluster solution had the highest silhouette width followed closely by the four-cluster solution. After examining these and other diagnostics, we also examined the meaningfulness of the distribution of z-scores for cluster solutions. We decided on the four-cluster solution as the best depiction of the data based on an iterative analysis of the cluster solutions and characteristics. The four-cluster solution produced qualitatively different clusters of caregiver networks, and the more precise division of clusters into smaller groups was a more desirable way to address our exploratory aims. We labeled each of the clusters based on which variables stood out when examining the z-scores, in particular those that characterized the amount and type of support received by caregivers.
Table 2 provides the overall means of the network variables used in the cluster analysis as well as the extreme z-scores that identify which variables best distinguish the clusters from each other cluster z-scores that were either at or above 0.5 or at or below −0.5 the overall mean. Examination of the extreme positive or negative z-score values enables us to characterize the four-cluster patterns: The networks of the caregivers in the four clusters can be described as follows: Direct Support: large, low density, primarily caregiver-supportive networks; Direct and Indirect Support: large dense networks supporting both caregivers and PWDs; Indirect Support: small dense networks primarily supporting the care recipient; and Low Support: small networks providing low support to both caregivers and PWDs.
Table 2.
Mean Characteristics of Variables Used in Cluster Analysis and Comparisons Within Overall Mean
| Cluster deviation from overall mean (z-scores ± 0.5 SD above/below mean)a | |||||
|---|---|---|---|---|---|
| Network measure | Overall mean (SD) (N = 66) | Direct (n = 19) | Direct and Indirect (n = 13) | Indirect (n = 19) | Low (n = 15) |
| Network density | 0.59 (0.25) | −0.85 | 0.71 | ||
| Network size | 8.68 (4.0) | 0.60 | 1.10 | −0.55 | −1.02 |
| Network proportion providing direct support to caregiver | |||||
| Emotional support | 0.53 (0.20) | 0.75 | −0.81 | ||
| Transportation | 0.25 (0.20) | −0.70 | 0.82 | ||
| Housework | 0.17 (0.18) | −0.58 | 0.79 | ||
| Financial | 0.54 (0.27) | 0.71 | −0.55 | ||
| Any direct support to caregiver | 0.70 (0.16) | 0.65 | 0.82 | −1.18 | |
| Network proportion providing support to persons with dementia | |||||
| Emotional support | 0.44 (0.21) | −0.51 | 1.00 | −0.90 | |
| Transportation | 0.24 (0.19) | −0.55 | 0.69 | 0.55 | −0.61 |
| Housework | 0.17 (0.18) | 0.62 | |||
| Financial | 0.14 (0.18) | −0.49 | 0.60 | ||
| Personal care | 0.16 (0.19) | 0.77 | −0.50 | ||
| Financial management | 0.12 (0.16) | 0.61 | |||
| Services management | 0.11 (0.15) | 0.70 | |||
| Help to respondent with caregiving | 0.31 (0.20) | −0.57 | 0.56 | 0.49 | |
| Any direct support to PWD | 0.50 (0.19) | −0.58 | 1.06 | 0.58 | −0.92 |
| Proportion of caregiver-only alters | 0.22 (0.20) | 1.04 | −0.82 | ||
| Help difficulty rating sumb | 14.91 (10.14) | 1.13 | −0.95 | ||
| Break difficulty rating suma,b | 12.55 (8.05) | 1.15 | −1.02 | ||
Note: PWD = person with dementia.
a z-scores calculated by subtracting overall mean from within-cluster mean and dividing by overall standard deviation. z-scores presented are either equal to or above 0.5 or equal to or below −0.5.
bDifficulty measures ranged from 1 = Very Difficult to 4 = Very Easy for each alter.
The “Direct” cluster included networks that provided a higher than average proportion of network members providing any type of support directly to caregivers as well as a higher average proportion providing direct financial support to caregivers compared to the overall proportion across all clusters. However, “Direct” networks did not provide support to caregivers for each type of support: a lower than average proportion of “Direct” network members provided transportation or housework support to caregivers, compared to overall. “Direct” networks provided less than average “any support” as well as less than average emotional, transportation, or financial support directly to the PWDs compared to the overall proportions. “Direct” networks contained a higher than average proportion of network members who only provided support to the caregiver compared to the overall proportion. The “Direct and Indirect” network cluster was larger than average and had higher average proportions of network members providing any support to the caregiver, including higher than average proportions providing emotional, transportation, and housework support. These network members also provided higher than the average of any type of support directly to the PWDs, including higher than average emotional, transportation, and housework support. The proportion of network members providing support to the respondent for caregiving was also higher than average and both help difficulty rating sums were higher than average, indicating higher than average ease in requesting help from the network. “Indirect” networks were smaller on average compared to overall network size and had a higher than average density. The proportion of network members providing any support to the PWD directly was higher than average, including higher than average transportation, financial, personal care, financial and service management, and support to the respondent for caregiving. There was a lower than average proportion of network members providing support to the caregiver only for “Indirect” networks compared to overall. The “Low Support” network cluster had smaller network size on average compared to overall and lower than average proportions providing any support to the caregiver (in particular, emotional and financial support) and the PWD (in particular, emotional, transportation, and personal care). The help difficulty rating sum scores were lower than average compared to overall, indicating higher than average difficulty for respondents asking for help from the network.
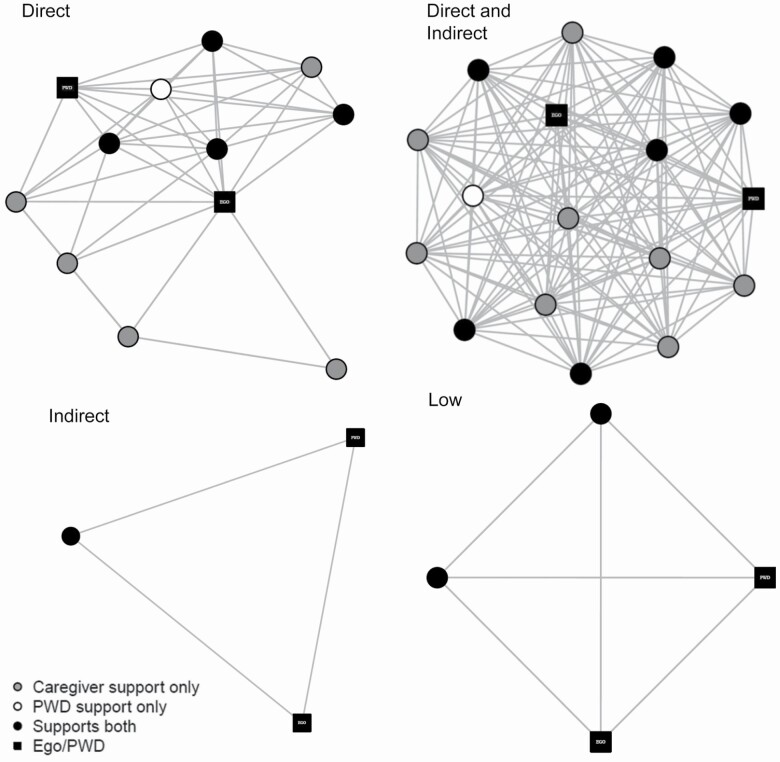
Examination of network diagrams also provides some intuitive insight into the differences between the four groups in terms of their size and structure. Figure 1 presents an example network for each of the four caregiver network types. Each of the diagrams depicts the caregiver, the PWD, and each of the members named by the caregiver in the personal network interview. Each person is represented by one network “node” and the people who the respondent identified as knowing each other are tied to each other with a network “edge.” The matrix of relationships among all network members (the raw network structure data) is visualized using a “spring-embedding” algorithm that clusters network members if they share common relationships and pushes apart those who are not directly or indirectly connected (Freeman, 2000). The caregivers and PWDs are represented by black squares. The other symbols in the graphs represent the network members named by the caregiver; colors indicate if they provided support to the caregiver only (gray circular), to the PWD only (white circular), or to both the caregiver and the PWD (black circular).
Figure 1.
Examples of caregiver personal networks for each of the four network types. Notes: Network members are represented by circles (graph “nodes”), the caregiver and persons with dementia (PWDs) are represented by black squares, and lines between nodes represent network members who know each other. The layout of the nodes, generated with the Fruchterman–Reingold force-directed placement algorithm, highlights structural characteristics of the network, such as density, the amount of lines between nodes, and size (the number of nodes). Composition among network members is highlighted by node color: gray circular nodes are those who were identified as having only provided support to the caregiver and not having provided support to the PWD; white circular nodes were those identified as having provided support to the PWD only and not support to the caregiver; black circular nodes were those who provided support to both caregiver and PWD.
Finally, we use the four clusters of caregivers identified in Table 2 and examine the demographic correlates of these four networks to compare the characteristics of caregivers who fall into each of the clusters on such factors as gender, age, race–ethnicity, proximity to PWD, total different types of care provided by the caregiver, years providing care, hours of care per week, and caregiver household income. Table 3 displays the results of these analyses and provides descriptive statistics of caregiver and PWD characteristics overall and within each of the four clusters, and results of tests of associations between average caregiver/PWD characteristics and cluster membership. Chi-square tests of association between cluster membership and the two categorical variables in the table, percent of respondents who were female, and percent caregiver with White race–ethnicity found a nonindependent relationship with gender but not ethnicity. “Indirect” had a very small percent of female caregivers (26) compared to the other clusters, in particular, “Direct” (79) and “Direct and Indirect” (93), and “Low Support” had a lower than average percent of female caregivers. For continuous measures, none of the ANOVA tests identified significant differences explaining the variance across clusters in percent of White caregivers. Each cluster was represented by a majority of White caregivers. However, the bivariate multinomial tests identified several significantly different caregiver characteristics between two or more clusters. Respondents in “Low Support” reported fewer total caregiving types than caregivers in “Direct” (relative risk ratio = 0.61, p < .06) and “Direct and Indirect” (relative risk ratio = 0.64, p = .09). “Low Support” caregivers also reported living a greater distance from the PWD than caregivers in “Indirect” (relative risk ratio = 1.44, p = .09). “Indirect” caregivers reported higher household income than caregivers in “Direct and Indirect” (relative risk ratio = 1.14, p = .02) and “Low Support” (relative risk ratio = 1.12, p = .03).
Table 3.
Characteristics of Caregivers and PWD and Bivariate Tests for Significant Differences Among and Between Clusters
| Caregiver and PWD Characteristics | Overall (N = 66) | Direct (N = 19) | Direct and Indirect (n = 13) | Indirect (n = 19) | Low (n = 15) |
|---|---|---|---|---|---|
| Caregiver mean age | 57.62 (10.23) | 54.32 | 59.31 | 59.26 | 58.27 |
| PWD mean age | 84.89 (9.45) | 86.68 | 82.31 | 86.26 | 83.13 |
| Caregiver % White (N, %) | 54 (81.81) | 16 (84.21) | 10 (76.92) | 15 (78.94) | 13 (86.68) |
| Caregiver % female (N, %) | 41 (62.12)*** | 15 (79.95) | 12 (92.31) | 5 (26.32) | 9 (60.00) |
| Total different types of care provided by caregiver | 4.06 (1.45) | 4.37a,* | 4.08 | 4.26a,* | 3.40b,c,* |
| Years providing care | 3.83 (3.07) | 3.39 | 3.19 | 4.18 | 4.47 |
| Distance between caregiver and PWD (in miles) | 2.06 (1.95) | 2.37 | 1.62 | 1.47a,** | 2.80c,** |
| Hours per week of caregiving | 3.79 (1.74) | 4.05 | 3.85 | 3.68 | 3.53 |
| Caregiver household income (thousands of $) | 58.06 (33.62) | 59.61 | 50.73c,** | 65.50a,d,** | 53.00c,,** |
Note: PWD = person with dementia.
aMultinomial model reference cluster “Low.”
bMultinomial model reference “Direct.”
cMultinomial model reference cluster “Indirect.”
dMultinomial model reference cluster “Direct and Indirect.”
*p < .1, **p < .05; ***Chi-square test.
Discussion and Implications
Nearly 18 million family and friends in the United States are currently providing care to older adults because of limitations in their physical, mental, or cognitive functioning (National Academies of Sciences, Engineering, and Medicine, 2016), and solutions to help and support them are desperately needed.
To identify the caregivers in greatest need of support, we first need a better understanding of the current social support networks available to family caregivers and whether specific groups of caregivers are at risk of having an insufficient support network. Network analysis is valuable for examining the connections that cross perceived boundaries of home or neighborhood situations. For family caregivers, support networks serve two crucial functions: the first is to provide emotional, financial, and other supports to the caregivers. The other function is to help the caregiver by providing direct care to the care recipient. This pilot study is the first to examine a broad sample of caregivers to people with dementia across the age spectrum and for a nationally representative sample. We use cluster analysis to help establish typologies of support and care networks. The personal network data collection instrument was designed to identify the broader support system available to dementia caregivers, including those providing direct social support to the caregiver and those available to provide caregiving support to the older adult with dementia. We found four common caregiving networks: large networks, primarily supporting caregivers (“Direct”); large networks with many helpers of caregivers and PWDs (“Direct and Indirect”); small, dense networks supporting PWDs mainly (“Indirect”); and small networks providing little help to either caregiver or PWD with dementia (“Low”). Gender, income, and geographic proximity of caregiver to the care recipient were associated with care network typologies.
We build on prior work that is focused either on older adults’ networks or on caregivers’ networks by examining the joint networks of caregivers and the PWDs to whom they provide care. That is, in addition to collecting detailed information on the direct support available to caregivers, we also ask about other people who provide care or support to only the PWD. Our network typologies suggest that while some networks are mostly focused on caregivers, others are centered on the care recipient and the caregiving tasks being provided to them.
This work has implications for informing the development of caregiving interventions that incorporate social network-based interventions that have been successful with other populations—for example, technology-based interventions that use personalized network visualizations to trigger strategies for altering networks (e.g., dropping ties, connecting disconnected ties, spending more time with supportive network members; Bouris et al., 2013; Kennedy et al., 2011, 2016, 2018; Osilla et al., 2016; Yoon, 2011). Empirical data on the correlates and consequences of network configurations are needed to customize network interventions that can help dementia caregivers reconfigure their networks and lower inefficiencies in care coordination. A recent review of support interventions for caregivers of PWD identified only a small number of successful support interventions that explicitly targeted the social networks of caregivers (Dam et al., 2016). One of these, a small pilot study that tested a “Network therapy” intervention approach with caregivers of PWD in which caregivers manually mapped out their social networks (Cohen et al., 1998). This study demonstrated promising results of increased caregiver coping and network activation, which supports the use of network visualizations as a caregiver support tool. Enhancing this approach with web-based technology for capturing and visualizing social networks and informed by a greater empirical grounding in the social network characteristics of caregivers over time would enable this promising approach to reach the growing population of PWD caregivers.
This work has several limitations. First, the network data were generated through interviews with caregivers about their perception of their immediate social environment of support for themselves and the PWD. We did not receive self-reports from the other members of the network about the support they provided to the PWD or the focal caregiver. Our personal network approach differed from what is often referred to as the “gold standard” of network data collection—sociocentric networks—where all network members are interviewed. However, this type of network is less appropriate for caregiver networks in the community, which do not necessarily have a well-defined sampling frame from which to recruit network members. Providing care to a PWD may also trigger accelerated network change more than other network types because of the strain on social relationships that caregiving may cause. While the sociocentric approach has been used elsewhere with caregivers of PWD, it has been confined to specific care facilities in a specific geographic area (Ashida et al., 2017; Koehly et al., 2015; Marcum et al., 2020). Our personal network approach enabled a diverse sample of respondents across the United States. Another limitation is that, although we assess the networks of care recipients along with the caregivers, we do not separately interview care recipients. This means that information on care recipients is provided by the caregivers based on their perceptions. This could mean that we are missing members of the care recipients’ network with whom are unknown to the caregiver. However, given that care recipients are older and have dementia, direct interviews were not feasible and proxy reporting by a close family member is common in other studies of older adults with dementia. Also, interventions for caregivers would primarily target their perceptions of their network environment; therefore, directly measuring the perception of their social networks may be more relevant than a more “objective” measurement of network composition and structure. Finally, because this was a pilot study with a small sample size, we had limited representation of minority race–ethnic groups and younger caregivers who may have different network typologies. Future work is needed to expand this sample and examine whether different network typologies are associated with different health and well-being outcomes for caregivers and the family members to whom they provide care.
This pilot study was a first step to identifying different types of caregiver network typologies and their demographic correlates, but there is further work to do to better understand differences in caregiver networks and implications for health outcomes. Next steps for this work could include expanding and diversifying the sample and collecting data over time to examine how networks change as caregiver roles become more/less intense and/or cease completely. It is also important to examine whether and how network profiles may be associated with caregiver/recipient health and well-being outcomes. For instance, this approach can be used to examine how different joint network profiles may be related to the health and well-being outcomes for caregivers and PWDs, as well as whether having well-supported caregivers have spillover effects on care recipient outcomes.
Our work suggests that there are different types of support/care networks available to caregivers and that there is variation by sociodemographic characteristics in terms of which type is most common. As the population ages, a better understanding of the supports available to caregivers and which caregivers may be left with insufficient supports will be crucial for ensuring the health and well-being of older adults and their families.
Funding
This work was supported by the National Institutes of Health under grant R01AG066194 (PI: E. M. Friedman) and by pilot project funding through the RAND Center for the Study of Aging which is supported by the National Institutes of Health (P30AG012815, PI: M. Hurd).
Conflict of Interest
None declared.
Author Contributions
The authors contributed equally and are listed in alphabetical order.
Supplementary Material
References
- Ashida, S., Marcum, C. S., & Koehly, L. M. (2017). Unmet expectations in Alzheimer’s family caregiving: Interactional characteristics associated with perceived under-contribution. The Gerontologist, 58(2), e46–e55. doi: 10.1093/geront/gnx141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayalon, L., & Levkovich, I. (2018). A systematic review of research on social networks of older adults. The Gerontologist, 59(3), e164–e176. doi: 10.1093/geront/gnx218 [DOI] [PubMed] [Google Scholar]
- Bettger, J. P. (2012). Foreword: The social environment supporting elder health: An exploration of social ties, networks, and resources. Family & Community Health, 35(4), 274–275. doi: 10.1097/FCH.0b013e3182685130 [DOI] [Google Scholar]
- Bidart, C., & Charbonneau, J. (2011). How to generate personal networks: Issues and tools for a sociological perspective. Field Methods, 23(3), 266–286. doi: 10.1177/1525822x11408513 [DOI] [Google Scholar]
- Bouris, A., Voisin, D., Pilloton, M., Flatt, N., Eavou, R., Hampton, K., Kuhns, L. M., Eder, M., & Schneider, J. A. (2013). Project nGage: Network supported HIV care engagement for younger black men who have sex with men and transgender persons. Journal of AIDS & Clinical Research, 4, 1000236. doi: 10.4172/2155-6113.1000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandes, U., Lerner, J., Lubbers, M. J., McCarty, C., Molina, J. L., & Nagel, U. (2010). Recognizing modes of acculturation in personal networks of migrants. Procedia—Social and Behavioral Sciences, 4, 4–13. doi: 10.1016/j.sbspro.2010.07.478 [DOI] [Google Scholar]
- Campbell, K. E., & Lee, B. A. (1991). Name generators in surveys of personal networks. Social Networks, 13(3), 203–221. doi: 10.1016/0378-8733(91)90006-F [DOI] [Google Scholar]
- Cañameras, J. L. (2015). La enfermedad de Alzheimer desde el análisis de redes sociales. GRAFO Working Papers, 4, 31–47. doi: 10.5565/rev/grafowp.15 [DOI] [Google Scholar]
- Charrad, M., Ghazzali, N., Boiteau, V., & Niknafs, A. (2014). NbClust package: Finding the relevant number of clusters in a dataset. Journal of Statistical Software, 61, 1–36. [Google Scholar]
- Cohen, C. A., Blumberger, C., Zucchero-Sarracini, C., Letts, L., & Marshall, L. (1998). Network therapy: A unique intervention for dementia caregivers. Aging & Mental Health, 2(4), 343–345. doi: 10.1080/13607869856605 [DOI] [Google Scholar]
- Cohn, D., & Taylor, P. (2010). Baby boomers approach 65—Glumly.Pew Research Center.https://www.pewsocialtrends.org/2010/12/20/baby-boomers-approach-65-glumly/ [Google Scholar]
- Cornwell, B., & Schafer, M. H. (2016). Social networks in later life. In George L. K. & Ferraro K. F. (Eds.), Handbook of aging and the social sciences (pp. 181–201). Elsevier. doi: 10.1016/B978-0-12-417235-7.00009-3 [DOI] [Google Scholar]
- Crossley, N., Bellotti, E., Edwards, G., Everett, M. G., Koskinen, J., & Tranmer, M. (2015). Social network analysis for ego-nets. SAGE. doi: 10.4135/9781473911871 [DOI] [Google Scholar]
- Dam, A. E., de Vugt, M. E., Klinkenberg, I. P., Verhey, F. R., & van Boxtel, M. P. (2016). A systematic review of social support interventions for caregivers of people with dementia: Are they doing what they promise? Maturitas, 85, 117–130. doi: 10.1016/j.maturitas.2015.12.008 [DOI] [PubMed] [Google Scholar]
- Frank, R. G. (2012). Long-term care financing in the United States: Sources and institutions. Applied Economic Perspectives and Policy, 34(2), 333–345. doi: 10.1093/aepp/pps016 [DOI] [Google Scholar]
- Freeman, L. C. (2000). Visualizing social networks. Journal of Social Structure, 1(1), 4. [Google Scholar]
- Friedman, E. M., Shih, R. A., Langa, K. M., & Hurd, M. D. (2015). US prevalence and predictors of informal caregiving for dementia. Health Affairs (Project Hope), 34(10), 1637–1641. doi: 10.1377/hlthaff.2015.0510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannella, E., & Fischer, C. S. (2016). An inductive typology of egocentric networks. Social Networks, 47, 15–23. doi: 10.1016/j.socnet.2016.02.003 [DOI] [Google Scholar]
- Golinelli, D., Ryan, G., Green, H. D., Kennedy, D. P., Tucker, J. S., & Wenzel, S. L. (2010). Sampling to reduce respondent burden in personal network studies and its effect on estimates of structural measures. Field Methods, 22(3), 217–230. doi: 10.1177/1525822X10370796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granovetter, M. S. (1977). The strength of weak ties Social networks. In Leinhardt S. (Ed.), Social networks: A developing paradigm (pp. 347–367). Elsevier. doi: 10.1016/B978-0-12-442450-0.50025-0 [DOI] [Google Scholar]
- Green, H. D.Jr, Tucker, J. S., Wenzel, S. L., Golinelli, D., Kennedy, D. P., Ryan, G. W., & Zhou, A. J. (2012). Association of childhood abuse with homeless women’s social networks. Child Abuse & Neglect, 36(1), 21–31. doi: 10.1016/j.chiabu.2011.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman, L., & Rousseeuw, P. J. (2009). Finding groups in data: An introduction to cluster analysis. John Wiley & Sons. [Google Scholar]
- Kennedy, D. P., Green, H. D.Jr, McCarty, C., & Tucker, J. (2011). Non-experts’ recognition of structure in personal network data. Field Methods, 23(3), 287–206. doi: 10.1177/1525822X11399702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy, D. P., Hunter, S. B., Chan Osilla, K., Maksabedian, E., Golinelli, D., & Tucker, J. S. (2016). A computer-assisted motivational social network intervention to reduce alcohol, drug and HIV risk behaviors among Housing First residents. Addiction Science & Clinical Practice, 11(1), 4. doi: 10.1186/s13722-016-0052-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy, D. P., Osilla, K. C., Hunter, S. B., Golinelli, D., Maksabedian Hernandez, E., & Tucker, J. S. (2018). A pilot test of a motivational interviewing social network intervention to reduce substance use among housing first residents. Journal of Substance Abuse Treatment, 86, 36–44. doi: 10.1016/j.jsat.2017.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehly, L. M., Ashida, S., Schafer, E. J., & Ludden, A. (2015). Caregiving networks—Using a network approach to identify missed opportunities. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70(1), 143–154. doi: 10.1093/geronb/gbu111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llopsis Cañameras, J. (2015). La enfermedad de Alzheimer desde el análisis de redes sociales. GRAFO Working Papers, 4(2), 31–47. doi: 10.5565/rev/grafowp.15 [DOI] [Google Scholar]
- Marcum, C. S., Ashida, S., & Koehly, L. M. (2020). Primary caregivers in a network context. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(1), 125–136. doi: 10.1093/geronb/gbx165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin, A., & Hampton, K. N. (2007). Simplifying the personal network name generator. Field Methods, 19(2), 163–193. doi: 10.1177/1525822X06298588 [DOI] [Google Scholar]
- McCarty, C. (2002). Structure in personal networks. Journal of Social Structure, 3(1), 20. [Google Scholar]
- McCarty, C., Lubbers, M. J., Vacca, R., & Molina, J. L. (2019). Conducting personal network research: A practical guide. Guilford Press. [Google Scholar]
- Murtagh, F., & Legendre, P. (2014). Ward’s hierarchical agglomerative clustering method: Which algorithms implement Ward’s criterion? Journal of Classification, 31(3), 274–295. doi: 10.1007/s00357-014-9161-z [DOI] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2016). Families caring for an aging America. The National Academies Press.https://www.johnahartford.org/images/uploads/reports/Family_Caregiving_Report_National_Academy_of_Medicine_IOM.pdf [PubMed] [Google Scholar]
- Osilla, K. C., Kennedy, D. P., Hunter, S. B., & Maksabedian, E. (2016). Feasibility of a computer-assisted social network motivational interviewing intervention for substance use and HIV risk behaviors for housing first residents. Addiction Science & Clinical Practice, 11(1), 14. doi: 10.1186/s13722-016-0061-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry, B. L., Pescosolido, B. A., & Borgatti, S. P. (2018). Egocentric network analysis: Foundations, methods, and models. Cambridge University Press. doi: 10.1017/9781316443255 [DOI] [Google Scholar]
- Pollard, M., & Baird, M.. (2017). The RAND American life panel: Technical description. RAND Corporation. doi: 10.7249/RR1651 [DOI] [Google Scholar]
- Ramchand, R., Tanielian, T., Fisher, M. P., Vaughan, C. A., Trail, T. E., Batka, C., Voorhies, P., Robbins, M. W., Robinson, E., & Ghosh-Dastidar, B. (2014). Hidden heroes: America’s military caregivers. RAND Corporation. doi: 10.7249/RR499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Madrid, M. N., Del Río-Lozano, M., Fernandez-Peña, R., Jiménez-Pernett, J., García-Mochón, L., Lupiañez-Castillo, A., & García-Calvente, M. (2018). Gender differences in social support received by informal caregivers: A personal network analysis approach. International Journal of Environmental Research and Public Health, 16(1), 91. doi: 10.3390/ijerph16010091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth, A. R. (2020). Informal caregiving and network turnover among older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(7), 1538–1554. doi: 10.1093/geronb/gby139 [DOI] [PubMed] [Google Scholar]
- Smith, K. P., & Christakis, N. A. (2008). Social networks and health. Annual Reviews of Sociology, 34, 405–429. doi: 10.1146/annurev.soc.34.040507.134601 [DOI] [Google Scholar]
- Vacca, R. (2020). Structure in personal networks: Constructing and comparing typologies. Network Science (Cambridge University Press), 8(2), 142–167. doi: 10.1017/nws.2019.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman, S., & Faust, K. (1994). Social network analysis: Methods and applications. Cambridge University Press. [Google Scholar]
- Wenger, G. C. (1991). A network typology: From theory to practice. Journal of Aging Studies, 5(2), 147–162. doi: 10.1016/0890-4065(91)90003-B [DOI] [Google Scholar]
- Yoon, S. A. (2011). Using social network graphs as visualization tools to influence peer selection decision-making strategies to access information about complex socioscientific issues. Journal of the Learning Sciences, 20(4), 549–588. doi: 10.1080/10508406.2011.563655 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.