Graphical Abstract
Key words: COVID-19, Burnout, Nurses, Intensive care unit, Emergency department
Abstract
Introduction
This study aimed to assess (1) the prevalence of burnout risk among nurses working in intensive care units and emergency department before and during the coronavirus disease 2019 pandemic and (2) the individual and work-related associated factors.
Methods
Data were collected as part of a cross-sectional study on intensive care unit and emergency nurses in Belgium using 2 self-administered online questionnaires distributed just before the pandemic (January 2020, N = 422) and during the first peak of the pandemic (April 2020, N = 1616). Burnout was assessed with the Maslach Burnout Inventory scale.
Results
The overall prevalence of burnout risk was higher among emergency nurses than intensive care unit nurses but was not significantly different after the coronavirus disease 2019 pandemic (from 69.8% to 70.7%, χ² = 0.15, P = .68), whereas it increased significantly among intensive care unit nurses (from 51.2% to 66.7%, χ² = 23.64, P < .003). During the pandemic, changes in workload and the lack of personal protective equipment were significantly associated with a higher likelihood of burnout risk, whereas social support from colleagues and from superiors and management were associated with a lower likelihood of burnout risk. Several determinants of burnout risk were different between intensive care unit and emergency nurses.
Conclusion
Our findings indicate that nurses in intensive care unit and emergency department were at risk of burnout but their experience during the coronavirus disease 2019 pandemic was quite different. Therefore, it is important to implement specific measures for these 2 groups of nurses to prevent and manage their risk of burnout.
Contribution to Emergency Nursing Practice
• Nurses in many countries face high prevalence of burnout, particularly those working in intensive care units (ICUs) and emergency departments. The impact of the coronavirus disease 2019 (COVID-19) pandemic on their risk of burnout remains underdocumented.
• The COVID-19 pandemic had a greater impact on the burnout risk of ICU nurses than emergency nurses, although the latter had a higher prevalence of burnout risk. Several determinants of burnout risk were different between ICU and emergency nurses.
• It is important to implement interventions to prevent and manage burnout among ICU and emergency nurses. However, different individual and organizational determinants must be targeted for emergency nurses than for ICU nurses.
Introduction
Burnout is a psychological syndrome resulting from chronic exposure to emotional or psychological stressors at work and can be illustrated by a 3-dimensional model that involves emotional exhaustion (EE), depersonalization (DP), and reduced personal accomplishment (RPA).1 EE is characterized by an extreme lack of energy, DP is associated with the development of negative feelings and attitudes and a certain withdrawal from work, and RPA is characterized by a sense of loss of skills and professional effectiveness.2 A global consensus has identified EE as the central dimension of burnout.3 , 4
Nurses in many countries face a high prevalence of burnout, which may be related to the very nature of this profession that is considered to be physically and psychologically demanding. A meta-analysis on 61 studies in 49 countries worldwide showed that the pooled prevalence of burnout symptoms among nurses was 11.23%, with significant differences between countries and specialties.5 Burnout among nurses has multiple consequences. First, it has negative consequences on their professional practices, with a deleterious impact on the quality of care provided to patients and therefore on their safety, health, and recovery.4 , 6, 7, 8 Second, it has consequences for nurses themselves with a significant risk of developing physical and mental health problems4 , 6 such as fatigue, anxiety, sleep disorders,5 mental health disorders, heart disease, and metabolic syndromes.8 Third, it has a negative impact on the health care systems with a decrease in work performance,7 an increase in absenteeism at work and a phenomenon of staff turnover,7 , 8 and an increase in expenses related to recruitment and human resources.5
Some nurses are at a greater risk of burnout than others, and many studies have found several risk factors for burnout. On the one hand, individual risk factors include young age, sex, having an emotionally unstable or uncooperative personality, and having a low level of self-control and self-determination.7 , 9 , 10 On the other hand, risk factors related to the professional environment include the type of service in which the nurse works (ie, intensive care unit [ICU], emergency department, pediatric, and oncology), working in a technical environment, excessive workload, overtime worked, shift work, understaffing,7 , 10 performing acts for which one is underqualified or overqualified,11 having low decision-making autonomy,12 and a lack of social and organizational support from colleagues and from superiors and management.10 , 12 , 13
Profiles of nurses identified as at risk of burnout in the scientific literature are nurses working in the ICU and emergency departments. A meta-analysis published in 2020 highlighted that the prevalence of burnout was 14.36% among ICU nurses and 10.18% among emergency nurses.5 Some studies explained this higher prevalence by the fact that these nurses work in a very technical and stressful environment, with patients in critical health situations (ie, repeated exposure to suffering and death) and with a high physical and psychological demand.11 , 14
The working conditions of nurses, like other care professionals, fluctuate over time and are sensitive to external events such as natural disasters, conflicts, or epidemics. At the end of December 2019, China reported a pneumonia epidemic in Wuhan linked to a new coronavirus, the severe acute respiratory syndrome coronavirus 2, a virus responsible for the global coronavirus disease 2019 (COVID-19) pandemic announced on March 11, 2020, by the World Health Organization. In one year from December 2019 to January 4, 2021, there were 83 715 617 confirmed cases and 1 835 901 deaths worldwide.15 Frontline health care workers, such as ICU and emergency nurses, were particularly exposed to the consequences of this pandemic. They were heavily involved in the detection and treatment of patients with COVID-19.16 This exposure involved, among other things, working in a high-risk environment8 , 10 with a considerable increase in their workload,16 , 17 treating patients with COVID-19 with limited clinical knowledge14 , 18 and without any specific treatment available at the start of the pandemic,19 repeated exposure to suffering and death,20 working in a context of shortage of personal protective equipment (PPE),16 , 18 and being afraid of contracting and transmitting the virus.17
Some studies have shown that the COVID-19 pandemic had negative consequences on the well-being and mental health of nurses.13 , 19 , 20 However, few studies have analyzed the impact of the COVID-19 pandemic on the risk of burnout of nurses. A study in China found that between 43.5% and 62.0% of nurses had a moderate to high risk of burnout in the dimensions of DP, EE, and RPA during the COVID-19 pandemic.19 In addition, few studies have compared the situation during the COVID-19 pandemic with the situation before it. Finally, although ICU and emergency nurses were particularly exposed during the COVID-19 pandemic, very few studies specifically addressed the risk of burnout among them.
OBJECTIVES
The objectives of this cross-sectional study in the French-speaking part of Belgium were to assess (1) the prevalence of burnout risk among ICU and emergency nurses before and during the COVID-19 pandemic and (2) the individual and work-related associated factors during the pandemic.
Methods
STUDY DESIGN AND SETTING
A cross-sectional study was conducted on the risk of burnout among ICU and emergency nurses in the French-speaking part of Belgium. Two waves of open online survey were conducted. The first wave of the survey took place over a period of 4 weeks in January 2020, before the COVID-19 pandemic, the first case of COVID-19 in Belgium being identified on February 4, 2020. The second wave of the survey took place between April 21 and May 04, 2020. This period corresponded to the peak of the first wave of COVID-19 in Belgium. The Hospital Emergency Plan was launched on March 13, 2020, and the first peak of the pandemic took place in April with between 400 and 500 new hospitalizations per day.21 Data were collected online via a platform compliant with the General Data Protection Regulation and using a convenience sampling method. Limitations of the following sampling method will be further developed in the discussion. The self-administered online questionnaires were disseminated through different channels. First, the heads of nursing departments of the 50 French-speaking hospitals were contacted and invited to share the study with the emergency and ICU nurses of their staff. In addition, 2 French-speaking associations of critical care nurses (ie, working in the ICU and emergency department) sent the study to their members. Finally, the study was shared on social networks, mainly in online communities of Belgian critical care nurses. Cookies were used to assign a unique user identifier to each respondent and prevent multiple entries from the same individual. The usability and technical functionality of the online questionnaire were tested by 5 independent people before the survey was released. The number of items per page was limited to have the highest completion rate. The questionnaire consisted of 36 questions distributed over 9 pages.
PARTICIPANTS
A total of 442 ICU and emergency nurses completed the questionnaire in the first wave of the study and 1616 in the second. Because the questionnaire dissemination methods were the same in both waves, the larger sample size in the second wave of the study may be explained by the greater interest of nurses in the topic of the study in the context of the COVID-19 pandemic. The participation rate (ratio of unique visitors who agreed to participate to unique first survey page visitors) was 46% in the first wave of the study and 68% in the second wave. The completion rate (ratio of users who finished the survey to users who agreed to participate) was 82% in the first wave and 91% in the second.
VARIABLES AND MEASURES
The primary outcome of interest was the risk of burnout and was assessed with the Maslach Burnout Inventory (MBI) questionnaire. The MBI has a high reliability (Cronbach alpha > 0.70) and convergent validity to assess the different aspects of burnout among health care workers.2 , 22 The convergent validity was established by correlating individual MBI scores with outcomes such as job dissatisfaction and poor working conditions.2 , 23 The MBI is free to use and assesses the following dimensions of burnout: EE, DP, and RPA. We used the validated French version of the MBI, which is a 22-item questionnaire (9 items on EE, 5 items on DP, and 8 items on RPA). Each item is measured on a 7-point frequency scale from “never” (scored at 0) to “every day” (scored at 6) with the EE score ranging from 0 to 54, the DP score ranging from 0 to 30, and the RPA score ranging from 0 to 48. For the 2 dimensions EE and DP, the higher the scores, the higher the risk of burnout, whereas it is the contrary for the dimension of RPA. As suggested in the user manual, predetermined cutoff points were used to identify in each dimension individuals at high risk of burnout.1 The cutoff point for a high risk was ≥27 for EE, ≥10 for DP, and ≤33 for RPA. To estimate the overall prevalence of risk of burnout, we chose as in other studies that a person at high risk in at least one of the 3 dimensions can be considered at risk of burnout.24
Additional data were collected in the second wave of the study to assess the impact of the COVID-19 pandemic on the working conditions and risk of burnout of nurses. The objective was to collect variables to identify the explanatory factors of the risk of burnout and the groups at risk: age, sex, the seniority in the health care sector, the perceived workload during the COVID-19 pandemic, the availability of PPE for COVID-19, and the social support from colleagues and from superiors and management. To assess social support at work, we used the 2 subscales on social support from colleagues and from superiors and management of the French version of the Job Content Questionnaire.25 This questionnaire is considered to be the main validated instrument to assess job strain,12 and it is composed of 3 dimensions assessed separately: psychological demand, decision latitude, and social support at work. The 2 subscales on social support from colleagues and from superiors and management are respectively composed of 6 and 5 items. Each item is scored on a 4-point Likert-type scale with scores ranging from 1 (strongly disagree) to 4 (strongly agree). Therefore, the score for social support from colleagues ranges from 6 (low social support) to 24 (high social support) and from superiors and management from 5 (low social support) to 20 (high social support).
DATA ANALYSIS
Data were analyzed using IBM SPSS (IBM Corp, Armonk, NY). First, descriptive analyses were performed on the samples from the 2 waves. This study being cross-sectional and not longitudinal, it seemed important to compare the samples between the 2 waves. Second, descriptive analyses were performed on the prevalence of high risk of burnout in the 3 dimensions of the MBI (ie, EE, DP, and RPA) before the COVID-19 pandemic, then during the first peak of the pandemic, and separately for nurses working in the ICU and those working in the emergency department. Additional descriptive analyses were performed on data from the second wave of the study to describe the working conditions of nurses during the COVID-19 pandemic. The final objective was to assess the factors associated with the high risk of burnout during the pandemic, among ICU and emergency nurses separately, to identify common and different factors between the 2 groups. Therefore, multivariate logistic regression models were performed on the 3 dimensions of the risk of burnout separately for ICU and emergency nurses.
ETHICAL APPROVAL AND INFORMED CONSENT
Participation was voluntary and anonymous and did not involve any compensation. Informed consent was obtained from all participants. The Belgian Law does not require an approval from an Ethical Board for an online survey with the general population. However, the study is covered for privacy regulations. Participants were provided with the legal information relating to consent. All information related to respondents’ consent and the General Data Protection Regulation is available on request. This is in accordance with the Declaration of Helsinki and the law that is applicable, including the regulation 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC—General Data Protection Regulation. All methods were performed in accordance with the relevant Belgian guidelines and regulations.
Results
SAMPLE CHARACTERISTICS
The comparison of the sample in the 2 waves of the study is presented in Table 1 . The samples in the 2 waves were not statistically different for the mean age (t = 3.89, P = .05) and for sex distribution (χ² = 0.461, P = .5). The mean age was approximately 35 years, and three-quarters of the sample were women. However, there was a significant difference between the 2 waves regarding the proportion of ICU and emergency nurses (χ² = 8.207, P = .004), with a higher proportion of ICU nurses in the second wave of the study. This difference was taken into account by analyzing these 2 groups separately.
TABLE 1.
Comparison of the sample in the 2 waves of the study
| Variables | First wave of the study: before the COVID-19 pandemic (N = 442) |
Second wave of the study: During the COVID-19 pandemic (N = 1616) |
t test/chi-square (P value) | ||
|---|---|---|---|---|---|
| Mean or n | SD or % | Mean or n | SD or % | ||
| Age, year, mean (SD) | 34.70 | 0.459 | 36.91 | 0.25 | 3.89 (.05) |
| Sex, female, n (%) | 345 | 78.1 | 1225 | 76.5 | 0.46 (.5) |
| Type of service, n (%) | |||||
| • ICU | 283 | 64 | 1149 | 71.1 | 8.21 (.004) |
| • Emergency nurse | 159 | 36 | 467 | 28.9 | |
COVID-19, coronavirus disease 2019; ICU, intensive care unit.
PREVALENCE OF HIGH RISK OF BURNOUT BEFORE AND DURING THE COVID-19 PANDEMIC AMONG NURSES WORKING IN THE ICU AND EMERGENCY DEPARTMENT
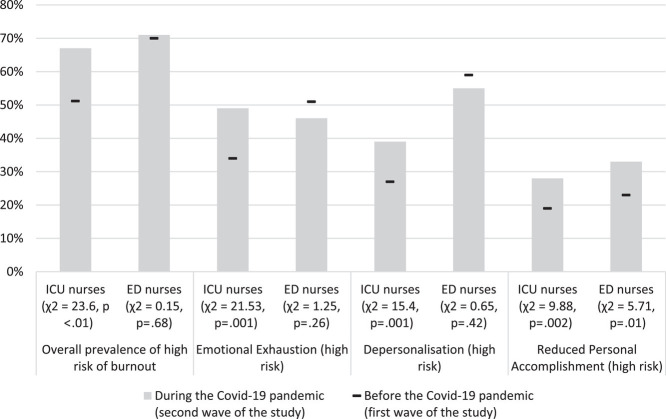
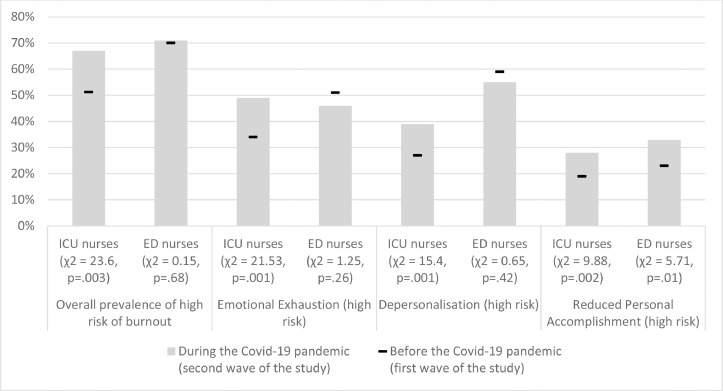
The prevalence of high risk of burnout before and during the COVID-19 pandemic among nurses working in the ICU and the emergency department is presented in the Figure . The overall prevalence of burnout risk was higher among emergency nurses than among ICU nurses before and also during the COVID-19 pandemic. Among emergency nurses, the prevalence remained stable over time (from 69.8% to 70.7%) and was not significantly different between the first and second waves of the study (χ² = 0.15, P = .68). Conversely, among ICU nurses, the prevalence has significantly increased after the COVID-19 pandemic (from 51.2% to 66.7%, χ² = 23.64, P < .003).
FIGURE.
Prevalence of high risk of burnout before and during the COVID-19 pandemic among nurses working in ICU and ED. COVID-19, coronavirus disease 2019; ICU, intensive care unit; ED, emergency department.
Regarding the different dimensions of burnout among ICU nurses, the most significant difference after the pandemic was observed on the high risk of EE, increasing from 33.6% to 48.9% (χ² = 21.53, P = .001). There was also a significant increase on the dimension of DP (high risk of DP, from 26.9% to 39.4%, χ² = 15.4, P = .001) and on the dimension of RPA (high risk of RPA, from 19.1% to 28.3%, χ² = 9.88, P = .002) after the COVID-19 pandemic.
Among emergency nurses, there was a significant difference after the COVID-19 pandemic on the high risk of RPA (5.71, P = .017) with an increase from 23.3% before to 33.4%, but not on the high risk of EE (χ² = 1.25, P = .26) and DP (χ² = 0.65, P = .42). For these last 2 dimensions, there was a slight decrease after the pandemic (high risk of EE from 50.9% to 45.8%; high risk of DP from 59.1% to 55.5%).
WORKING CONDITIONS OF NURSES WORKING IN THE ICU AND THE EMERGENCY DEPARTMENT DURING THE COVID-19 PANDEMIC
The working conditions of ICU and emergency nurses during the COVID-19 pandemic are presented in Table 2 . During the COVID-19 pandemic, the only significant difference between ICU and emergency nurses was on the perceived workload (χ² = 390.6, P < .001). Among ICU nurses, 89.1% reported an increased workload after the COVID-19 pandemic and 2.3% a decreased workload. In contrast, among emergency nurses, less than half (45.1%) reported an increase and 37% reported a decrease. The average seniority in the health care sector was not significantly different (t = 0.42, P = .06) between ICU nurses (13.96 years, SD = 0.32) and emergency nurses (13.57 years, SD = 0.47). In addition, approximately half of ICU (48.9%) and emergency nurses (51.4%) said they did not have sufficient PPE for COVID-19. Finally, ICU and emergency nurses reported fairly high social support from both their colleagues (18.5 of 24) and their superiors (14.8 of 20) during the COVID-19 pandemic.
TABLE 2.
Working conditions of ICU and emergency nurses during the COVID-19 pandemic (second wave of the study)
| Variables | ICU nurses (N = 1149) |
Emergency nurses (N = 467) |
t test/chi-square (P value) | ||
|---|---|---|---|---|---|
| Mean or n | SD or % | Mean or n | SD or % | ||
| Seniority in the health care sector, year, mean (SD) | 13.96 | 0.32 | 13.57 | 0.47 | 3.42 (.07) |
| The perceived workload during the COVID-19 epidemic was n (%) | |||||
| • Lower | 24 | 2.3 | 155 | 37.6 | 390.62 (<.001) |
| • The same | 88 | 8.5 | 71 | 17.2 | |
| • Greater | 920 | 89.1 | 186 | 45.1 | |
| Having sufficient protective equipment for COVID-19, n (%) | |||||
| • Yes | 550 | 51.1 | 209 | 48.6 | 0.75 (.39) |
| • No | 527 | 48.9 | 221 | 51.4 | |
| Social support from colleagues, from 6 (low) to 24 (high), mean (SD) | 18.59 | 0.09 | 18.59 | 0.14 | 0.06 (.81) |
| Social support from superiors, from 5 (low) to 20 (high), mean (SD) | 14.85 | 0.1 | 14.81 | 0.17 | 0.67 (.42) |
Descriptive statistics were performed after the exclusion of missing data.
ICU, intensive care unit; COVID-19, coronavirus disease 2019.
FACTORS ASSOCIATED WITH THE 3 DIMENSIONS OF THE RISK OF BURNOUT AMONG ICU AND EMERGENCY NURSES DURING THE COVID-19 PANDEMIC
The factors associated with the 3 dimensions of the risk of burnout among ICU and emergency nurses during the COVID-19 pandemic are presented in Table 3 .
TABLE 3.
Factors associated with the 3 dimensions of the risk of burnout during the COVID-19 pandemic among ICU and emergency nurses using multivariate logistic regression models (second wave of the study)
| Variables | High risk of EE, OR (95% CI) |
High risk of DP, OR (95% CI) |
High risk of RPA, OR (95% CI) |
|||
|---|---|---|---|---|---|---|
| ICU nurses | Emergency nurses | ICU nurses | Emergency nurses | ICU nurses | Emergency nurses | |
| Age, year | 1.04 (0.98-1.09) | 0.96 (0.89-1.05) | 0.94 (0.88-0.98)⁎ | 0.95 (0.88-1.04) | 0.97 (0.91-1.04) | 0.96 (0.87-1.05) |
| Sex (REF = women) | ||||||
| • Men | 0.86 (0.61-1.24) | 0.69 (0.41-1.18) | 2.81 (1.96-4.02)† | 3.87 (2.23-6.74)† | 0.84 (0.54-1.32) | 0.91 (0.50-1.64) |
| Seniority in the health care sector, year | 0.97 (0.92-1.02) | 1.02 (0.94-1.11) | 1.01 (0.95-1.08) | 0.99 (0.92-1.08) | 1.01 (0.95-1.08) | 1.17 (1.08-1.28)‡ |
| The perceived workload during the COVID-19 epidemic was | ||||||
| • Lower | 0.98 (0.27-3.54) | 1.01 (0.51-1.97) | 0.88 (0.21-3.63) | 1.41 (0.71-2.79) | 0.93 (0.17-4.93) | 1.80 (1.53-2.08)‡ |
| • The same | REF | REF | REF | REF | REF | REF |
| • Greater | 4.03 (2.10-7.72)† | 1.73 (0.89-3.36) | 2.44 (1.27-4.68)‡ | 1.70 (1.16-2.22)⁎ | 2.02 (0.90-4.55) | 1.56 (0.69-3.50) |
| Having sufficient protective equipment for COVID-19 (reference = yes) | ||||||
| • No | 1.81 (1.36-2.42)† | 1.75 (1.25-2.21)‡ | 1.28 (0.94-1.74) | 0.85 (0.52-1.38) | 1.14 (0.79-1.63) | 1.30 (0.75-2.23) |
| Social support from colleagues, from 6 (low) to 24 (high) | 0.93 (0.88-0.98)⁎ | 0.83 (0.75-0.92)‡ | 0.91 (0.86-0.97)‡ | 0.85 (0.77-0.95)‡ | 0.89 (0.83-0.96)‡ | 0.91 (0.82-1.02) |
| Social support from superiors, from 5 (low) to 20 (high) | 0.91 (0.87-0.97)‡ | 0.92 (0.85-1.01) | 0.96 (0.91-1.01) | 0.92 (0.84-1.01) | 0.92 (0.86-0.97)‡ | 0.94 (0.86-1.02) |
EE, emotional exhaustion; DP, depersonalization; RPA, reduced personal accomplishment; OR, odds ratio, CI, confidence interval.
P < .05.
P < .001.
P < .01.
Regarding the high risk of EE, the associated factors among ICU nurses were the perceived workload, whether or not they had PPE for COVID-19, and the social support from colleagues and from superiors and management. Among emergency nurses, the associated factors were whether or not they had PPE for COVID-19 and social support from colleagues. Among ICU nurses, having a higher workload during the COVID-19 pandemic significantly increased the odds (OR = 4.03, P < .001) of being at high risk of EE compared with having a stable workload. In addition, ICU nurses who reported not having enough PPE for COVID-19 were more likely (OR = 1.81, P < .001) to be at high risk of EE compared with those who reported having enough. Finally, high social support from colleagues (OR = 0.93, P < .05) and from superiors and management (OR = 0.91, P < .01) were significantly associated with lower odds of being at high risk of EE. Among emergency nurses, not having enough PPE for COVID-19 was also associated with an increased likelihood of high risk of EE (OR = 1.75, P < .01). Finally, emergency nurses reporting high social support from colleagues had lower odds of being at high risk of EE (OR = 0.83, P < .01).
Regarding the high risk of DP, the associated factors among ICU nurses were age, sex, perceived workload, and social support from colleagues. For emergency nurses, the associated factors were sex, perceived workload, and social support from colleagues. In both groups, men (ICU, OR = 2.81, P < .001; ED, OR = 3.87, P < .001) and those reporting a higher workload since the COVID-19 pandemic (ICU, OR = 2.44, P < .01; ED, OR = 1.70; P < .05) were more likely to be at high risk of DP than women and those reporting a stable workload. In addition, ICU and emergency nurses with higher social support from colleagues had a lower likelihood (ICU, OR = 0.91, P < .01; ED, OR = 0.85, P < .01) of being at high risk of DP. Finally, among ICU nurses, older nurses had a lower likelihood (OR = 0.94, P < .05) of being at high risk of DP than younger nurses.
Regarding the high risk of RPA, the associated factors among ICU nurses were the social support from colleagues and from superiors and management. For emergency nurses, the associated factors were seniority in the health care sector and perceived workload. For ICU nurses, high social support from colleagues (OR = 0.89, P < .01) and from superiors and management (OR = 0.92, P < .01) were significantly associated with lower odds of being at high risk of RPA. Among emergency nurses, those with more seniority in the health care sector (OR = 1.17, P < .01) and those reporting a lower workload (OR = 1.80, P < .01) during the COVID-19 pandemic had higher odds of being at risk of RPA than emergency nurses with less seniority and reporting a stable workload.
Discussion
KEY RESULTS
The objectives of this study were to assess in Belgium (1) the prevalence of burnout risk among ICU and emergency nurses before and during the COVID-19 pandemic and (2) the individual and work-related associated factors during the pandemic. This study highlighted that the prevalence of burnout risk was high in both groups but overall higher in emergency nurses than in ICU nurses, before and during the COVID-19 pandemic. Half of ICU nurses were at risk of burnout before the pandemic, and this proportion significantly increased to 67% after the pandemic. Conversely among emergency nurses, 70% were at risk of burnout before the pandemic and this proportion did not change significantly after the pandemic. Therefore, we can note that the COVID-19 pandemic had a greater impact on the burnout risk of ICU nurses than emergency nurses, although the latter had a higher prevalence of burnout risk.
Regarding the determinants of the risk of burnout during the COVID-19 pandemic, several risk and protective factors were highlighted in this study. A change in workload was a significant risk factor but experienced differently by nurses in the ICU than in the emergency department. Among ICU nurses, 89.1% reported having an increase in their workload after the COVID-19 pandemic and this was a significant risk factor for EE and DP. However, among emergency nurses, 37% reported having a decrease in their workload after the pandemic and this was a significant risk factor for RPA. The lack of PPE for COVID-19 was reported by half of ICU and emergency nurses and was a significant risk factor for burnout. Having high social support from colleagues was a protective factor of burnout in both ICU and emergency nurses. In contrast, having high support from superiors and management was a protective factor only in ICU nurses.
INTERPRETATION
A recent meta-analysis on studies conducted before the COVID-19 pandemic showed that the prevalence of EE varied from 2% to 27% among ICU nurses and from 3% to 17% among emergency nurses.5 These figures are significantly lower than those of our study and different hypotheses can explain it. First, this difference can be explained by the Belgian context. In 2019 in Belgium, the average number of patients per nurse was 9.4, which is above international standards.26 In addition, a study conducted in Belgian hospitals highlighted that although the nurse-to-patient ratio in the ICU is set by national regulations at 1:3, the optimal ratio would rather be 1:1.5.27 This indicates, on the one hand, that there was a shortage of nurses in Belgium and, on the other hand, that they were facing a heavy workload that could increase their risk of burnout. Our results are consistent with a 2019 Belgian study on nurses working in general hospitals, which found that 36% had a high risk of EE, 32% a high risk of DP, and 31% a high risk of RPA.26 In addition, Belgium was strongly affected by the first wave of COVID-19 compared with other European countries. For example, in the first months of the pandemic, Belgium's hospitalization rate was nearly 12 times higher than that of France and its crude death rate from COVID-19 was almost twice as high.21 , 28 Second, although the MBI is a widely used instrument, there may be variations in the cutoff points used and these are not systematically reported, making comparisons of prevalence between studies complicated.5
So far, few studies have assessed the impact of the COVID-19 pandemic on the risk of burnout among nurses by comparing the situation during the pandemic with the situation before it. Our study highlighted a significant increase in the risk of burnout after the pandemic, in 3 dimensions of burnout among ICU nurses, and in the dimension of RPA among emergency nurses. In addition, our study found a higher risk of burnout among emergency nurses than among ICU nurses before and during the COVID-19 pandemic. This could be explained by the working conditions of emergency nurses because they work in an unpredictable environment in which they have to move from one emergency to another in a short time.4 In addition, emergency nurses are continually faced with acute illnesses and traumatic events and are often exposed to assault from patients.7 However, our study found that the COVID-19 pandemic had more impact on the burnout risk of ICU nurses than emergency nurses. Several elements can explain this difference between the 2 groups. Between March and June 2020, 1696 patients with COVID-19 were admitted to ICUs in Belgium.29 Therefore, the number of intensive care beds has been increased to 2000 with the opening of 800 new intensive care beds in this short period.30 These additional beds have led to major structural and organizational changes within the ICUs. For example, many nurses from other care units, such as the operating room, consultations, or even some hospitalization units, have been deployed in ICUs to supplement the workforce. However, these nurses had little or no experience working in ICUs, which resulted in an increase in the workload of ICU nurses. In addition to taking care of the most severe patients requiring the most technical care, ICU nurses also had to train their new colleagues and supervise them. In addition, patients with COVID-19 in ICUs considerably increase the workload of nurses because they are often critical, with many devices, requiring a lot of nursing care and high and long-term monitoring. A study in Belgium found that patients hospitalized in the ICU owing to COVID-19 require much more nursing time than patients without COVID-19 and that they needed a nurse-to-patient ratio of 1:1.31 Finally, ICU nurses were highly exposed to death because the mortality rate of patients with COVID-19 in the ICU at the end of the first wave of the pandemic in Belgium was 36%.30
Regarding the factors associated with the risk of burnout, many studies have found an association between the high workload in intensive care and emergency services and the increased risk of burnout of nurses working there.6 , 7 Studies conducted during the COVID-19 pandemic also reported that the increased workload during the pandemic led to an increase in burnout among nurses,14 , 16 which is consistent with the results of our study. However, our study also found an outcome that had rarely been documented so far; during the COVID-19 pandemic, a decrease in the workload among emergency nurses significantly increased the risk of RPA. Nearly half of the emergency nurses in our sample declared that they had a decreased workload during the pandemic, which could have led to the feeling that they were not very involved in the fight against the pandemic and the care of patients with COVID-19. This feeling can then lead to an increased risk of RPA.
Conversely among ICU nurses, nearly 90% reported an increase in their workload after the pandemic and this increase was a major risk factor for burnout. Several actions can be implemented to manage the workload in the ICU. First, there is a need to increase the number of trained ICU nurses to increase the nurse-to-patient ratio. Currently, in Belgium, this ratio is legally set at 1:3 in the ICU but as previously explained the ratio for patients with COVID-19 should be close to 1:1.31 , 32 Unfortunately, Belgium faces, like many countries, a shortage of nurses. Some stakeholders even speak of a vicious circle, because this shortage exhausts the nurses who are at the bedside, leading to an escape from the profession and therefore a decrease in the number of active nurses. Therefore, it is essential to promote the nursing training and profession, to make it more attractive to students, and also to retain nurses already at the bedside.
Regarding the availability of PPE, approximately half of the sample of ICU and emergency nurses said they did not have enough during the first wave of COVID-19 in Belgium. At the start of the pandemic in Belgium, as in other countries, there was a shortage of PPE. This shortage has probably caused a feeling of insecurity among nurses and the fear of being infected but also of infecting patients and relatives. This could explain why the lack of PPE was associated with a higher risk of EE in ICU and emergency nurses. Similar results were found in a recent study in China.8
Our study also found that, during the COVID-19 pandemic, having a high social support from colleagues reduced the risk of burnout among ICU and emergency nurses. Having a high social support from superiors and management also reduced the risk of burnout, but only among ICU nurses. Previous studies have also shown that, during a pandemic, social support from colleagues and from superiors was a protective factor for burnout among health care workers.33 , 34 Other studies have found that greater social support from colleagues and superiors reduced the anxiety associated with COVID-19 among frontline nurses.18 , 19
LIMITATIONS
The main strength of this study is the use of data collected before and during the COVID-19 pandemic to assess the impact of the pandemic on the risk of burnout among emergency and ICU nurses. In addition, different potential determinants of the risk of burnout were assessed, some of which have been less studied in the context of the COVID-19 pandemic, such as social support from colleagues and from superiors and management. Finally, another strength of this study was the use of the MBI, which is a validated and widely used tool to assess the risk of burnout among health care workers. This study also has limitations. The first limitation is that it was a cross-sectional study; the 2 waves of surveys were conducted on similar populations, but we did not follow the same individuals over time. Therefore, we cannot study the impact of the pandemic on the risk of burnout at the individual level. Although the 2 samples were not statistically different in terms of age and sex (see Table 1), other unmeasured characteristics may be different between the 2 samples and may modify the association with the risk of burnout. The second limitation is that it was a convenience sample via an online survey with voluntary participation, which leads to possible selection bias. The nurses who responded were people who potentially wanted to share their difficulties and be heard, which could result in an overestimation of the risk of burnout. Information was sought in the Belgian national and regional registers on the characteristics of ICU and emergency nurses (eg, age and sex distribution) to assess the representativeness of the samples of the current study. However, this information is only partially available for nurses in Belgium, and the type of service (eg, emergency department and ICU) is not systematically recorded. Consequently, the representativeness of the samples could not be assessed or adjusted using weighting methods.
IMPLICATIONS FOR EMERGENCY CLINICAL CARE
This study highlighted that the COVID-19 pandemic had a greater impact on the burnout risk of ICU nurses than emergency nurses, although the latter had a higher prevalence of burnout risk. As explained previously, there are several elements that may explain the greater impact of the pandemic on ICU nurses. Between March and June 2020, 800 additional intensive care beds have been opened in Belgium, and these additional beds have led to major structural and organizational changes within the ICUs (eg, temporary deployment of the nurses from other departments). In addition, patients with COVID-19 in ICUs considerably increase the workload of nurses because they are often critical, with many devices, requiring a lot of nursing care and intensive and long-term monitoring. Finally, ICU nurses were highly exposed to death because the mortality rate of patients with COVID-19 in the ICU at the end of the first wave of the pandemic in Belgium was 36%.30
Regarding the determinants of the risk of burnout during the COVID-19 pandemic, several risk and protective factors for burnout were highlighted in this study. A change in workload after the COVID-19 pandemic was a significant risk factor but experienced differently by nurses in the ICU than in the emergency department. Most intensive care nurses reported having an increase in their workload as a result of the COVID-19 pandemic, and this increase was a significant risk factor for EE and DP. Conversely, among emergency nurses, almost 40% reported having a decrease in their workload after the pandemic, and it was a significant risk factor for RPA. The lack of PPE for COVID-19 was also a significant risk factor for burnout. Almost 50% of ICU and emergency nurses reported a lack of PPE, and it was a significant risk factor for EE in both groups. Having high social support from colleagues was a protective factor of burnout in both ICU and emergency nurses. In contrast, having high social support from superiors and management was a protective factor only in ICU nurses.
In addition to the negative impact on workers’ health, health care worker burnout has a negative impact on the entire health care system and patient care outcomes. Therefore, policy makers and health managers should provide adequate evidence-based interventions. Several studies have highlighted the importance of implementing interventions at the organizational (eg, appropriate staffing and provision of protective equipment) and individual level (eg, debriefing sessions and social support).35 , 36 In terms of staffing, some countries have guidelines for nurse-to-patient ratios, depending on the type of service or patient profile. In the context of a pandemic, one possibility would be to adapt these guidelines and increase the nurse-to-patient ratio. At the individual level, debriefing techniques are probably the most documented interventions to manage the risk of burnout. Individual or group debriefing is an information-sharing and event-handling session that is considered good practice after a disaster or adverse event.37 , 38 After a stressful and traumatic event such as the death of patients with COVID-19, a debriefing session within 24 hours could be beneficial for nurses to prevent burnout and other stress-related disorders.39 Finally, our study showed that strengthening the social support from colleagues and from superiors and management could reduce the risk of burnout among ICU and emergency nurses. For the social support of colleagues, it is possible to strengthen team spirit with interventions such as the granting of breaks to promote informal exchanges between colleagues, the provision of a relaxation room, or the organization of team building. Regarding support from superiors and management, it is possible to set up daily team meetings and systematic debriefing exchanges between the team manager and the nurses. However, for these strategies to be effective, it is essential to target nurses at risk of burnout. This study showed that nurses who experienced a decrease in their workload after the COVID-19 pandemic were also at high risk of burnout; therefore, they should not be overlooked when it comes to interventions.
Conclusions
This study found that ICU and emergency nurses had high burnout risk prevalence before and during the COVID-19 pandemic. Although emergency nurses had a higher prevalence before and during the COVID-19 pandemic, this study found that ICU nurses were more affected by the pandemic. Indeed, the prevalence of burnout risk was stable among emergency nurses whereas it increased among ICU nurses after the pandemic. This result suggests the need for routine, nonpandemic-specific interventions for emergency nurses and more pandemic-specific interventions for ICU nurses.
In the context of the COVID-19 pandemic, different risk factors for burnout have been highlighted such as changes in workload or lack of PPE and protective factors such as social support from colleagues and from superiors and management. However, these factors may have a different influence on the 2 groups of nurses, so it is important to assess them to better target the interventions to be implemented at the individual and organizational levels. For example, most ICU nurses reported an increased workload after the pandemic, and this was a risk factor for burnout. Conversely, nearly half of emergency nurses reported a decreased workload, and it was a risk factor for RPA.
Given that the COVID-19 pandemic continues to rage worldwide, it would be relevant to conduct additional studies to analyze the evolution after more than a year of the risk of burnout among nurses and long-term associated factors. In addition, further studies should include open-ended questions so that participants can voice their concerns. Finally, we suggest collecting data related to any deployment during the pandemic, to investigate the stress arising from a new work environment.
Author Disclosures
Conflicts of interest: none to report.
Acknowledgment
The authors gratefully acknowledge the nurses who took part in the study.
Biographies
Sarah Butera is a Faculty of Public Health, Université Catholique de Louvain; and Nurse, Centre Hospitalier Interrégional Edith-Cavell, Brussels, Belgium. ORCID identifier:https://orcid.org/0000-0001-9647-4961
Natacha Brasseur is Faculty of Public Health, Université Catholique de Louvain; and Nurse, Cliniques universitaires Saint-Luc, Brussels, Belgium. ORCID identifier:https://orcid.org/0000-0003-0883-0554
Nataly Filion is Professor, Haute Ecole Léonard de Vinci, Brussels, Belgium. ORCID identifier:https://orcid.org/0000-0001-9382-0347
Arnaud Bruyneel is PhD Candidate, Health Economics, Hospital Management and Nursing Research Department, School of Public Health, Université Libre de Bruxelles, Brussels, Begium; and Nurse, SIZ Nursing, A Society of Intensive Care Nurses, Belgium. ORCID identifier:https://orcid.org/0000-0002-0432-9474. Twitter: @arnaudbruyneel
Pierre Smith is PhD Post Doctoral Researcher, Institute of Health and Society (IRSS), Université catholique de Louvain; and Department of Epidemiology and Public Health, Sciensano, Brussels, Belgium. ORCID identifier:https://orcid.org/0000-0003-3178-9924. Twitter: @pierres65618260
REFERENCES
- 1.Maslach C, Jackson SE, Leiter MP, Schaufeli W, Schwab RL. Mind Garden; 1986. Maslach Burnout Inventory Manual, General Survey, Human Services Survey, Educators Survey and Scoring Guides. [Google Scholar]
- 2.Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 3.Maslach C, Leiter MP. Early predictors of job burnout and engagement. J Appl Psychol. 2008;93(3):498–512. doi: 10.1037/0021-9010.93.3.498. [DOI] [PubMed] [Google Scholar]
- 4.Adriaenssens J, De Gucht V, Maes S. Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int J Nurs Stud. 2015;52(2):649–661. doi: 10.1016/j.ijnurstu.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Woo T, Ho R, Tang A, Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J Psychiatr Res. 2020;123:9–20. doi: 10.1016/j.jpsychires.2019.12.015. [DOI] [PubMed] [Google Scholar]
- 6.Chuang CH, Tseng PC, Lin CY, Lin KH, Chen YY. Burnout in the intensive care unit professionals: a systematic review. Medicine (Baltimore) 2016;95(50):e5629. doi: 10.1097/MD.0000000000005629. doi:1097/MD.0000000000005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gómez-Urquiza JL, De la Fuente-Solana EI, Albendin-Garcia L, Vargas-Pecino C, Ortega-Campos EM, Cañadas-De la Fuente GA. Prevalence of burnout syndrome in emergency nurses: a meta-analysis. Crit Care Nurse. 2017;37(5):e1–e9. doi: 10.4037/ccn2017508. [DOI] [PubMed] [Google Scholar]
- 8.Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J Clin Nurs. 2020;29(21-22):4217–4226. doi: 10.1111/jocn.15454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cañadas-De la Fuente GA, Vargas C, San Luis C, Garcia I, Cañadas GR, De la Fuente EI. Risk factors and prevalence of burnout syndrome in the nursing profession. Int J Nurs Stud. 2015;52(1):240–249. doi: 10.1016/j.ijnurstu.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020;277:347–357. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karanikola M, Giannakopoulou M, Mpouzika M, Kaite CP, Tsiaousis GZ, Papathanassoglou ED. Dysfunctional psychological responses among intensive care unit nurses: a systematic review of the literature. Rev Esc Enferm USP. 2015;49(5):847–857. doi: 10.1590/S0080-623420150000500020. [DOI] [PubMed] [Google Scholar]
- 12.Niedhammer I, Ganem V, Gendrey L, David S, Degioanni S. Propriétés psychométriques de la version française des échelles de la demande psychologique, de la latitude décisionnelle et du soutien social du “Job Content Questionnaire” de Karasek: résultats de l'enquête nationale SUMER. Sante Publique. 2006;18(3):413–427. doi: 10.3917/spub.063.0413. [DOI] [PubMed] [Google Scholar]
- 13.Hu D, Kong Y, Li W, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalmedicine. 2020;24 doi: 10.1016/j.eclinm.2020.100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.An Y, Yang Y, Wang A, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. WHO coronavirus (COVID-19) dashboard. Published January 2021. Accessed October 1, 2021. https://Covid19.who.int
- 16.Spoorthy M, Pratapa S, Mahant S. Mental health problems faced byhealthcare workers due to the COVID-19 pandemic-a review. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sampaio F, Sequeira C, Teixeira L. Impact of COVID-19 outbreak on nurses’ mental health: a prospective cohort study. Environ Res. 2021;194 doi: 10.1016/j.envres.2020.110620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Labrague L, De Los, Santos J. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28(7):1653–1661. doi: 10.1111/jonm.13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guixia L, Hui Z. A study on burnout of nurses in the period of COVID-19. Psychol Behav Sci. 2020;9(3):31–36. doi: 10.11648/j.pbs.20200903.12. [DOI] [Google Scholar]
- 20.Giusti EM, Pedroli E, D'Aniello GE, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. 2020;11:1684. doi: 10.3389/fpsyg.2020.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sciensano. COVID-19-epidemiologische situatie. Published March 2020. Accessed October 1, 2021. https://covid-19.sciensano.be/nl/covid-19-epidemiologische-situatie
- 22.Kovess-Masfety V, Saunder L. Le burnout: historique, mesures et controverses. Arch Mal Prof Environ. 2017;78(1):16–23. doi: 10.1016/j.admp.2016.01.007. [DOI] [Google Scholar]
- 23.Poghosyan L, Aiken L, Sloane D. Factor structure of the Maslach Burnout Inventory: an analysis of data from large scale cross-sectional surveys of nurses from eight countries. Int J Nurs Stud. 2009;46(7):894–902. doi: 10.1016/j.ijnurstu.2009.03.004. Published correction appears in Int J Nurs Stud. 2014;51(10):1416-1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rotenstein L, Torre M, Ramos M, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karasek R, Kawakami N, Brisson C, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 26.Heede Koen VD, Luk B, Dorien B, et al. Safe nurse staffing levels in acute-hospitals. Belgian Health Care Knowledge Centre. Published 2019. Accessed October 1, 2021; https://kce.fgov.be/fr/dotation-infirmière-pour-des-soins-plus-sûrs-dans-les-hôpitaux-aigus
- 27.Bruyneel A, Tack J, Droguet M, et al. Measuring the nursing workload in intensive care with the Nursing Activities Score (NAS): a prospective study in 16 hospitals in Belgium. J Crit Care. 2019;54:205–211. doi: 10.1016/j.jcrc.2019.08.032. [DOI] [PubMed] [Google Scholar]
- 28.Les données relatives Au COVID-19 en France. Data.gouv.f. Published March 2020. Accessed October 1, 2021. https://www.data.gouv.fr/fr/datasets/donnees-relatives-a-lepidemie-de-covid-19-en-france-vue-densemble/
- 29.Van Beckhoven D, Duysburgh E, Montourcy M, et al. Sciensano; Bruxelles, Belgique: 2020. Points clés de la surveillance des patients hospitalisés atteints d'une infection COVID-19 confirmée: résultats jusqu'au 14 juin 2020. Numéro dépôt légalD/2020/14.440/65. [Google Scholar]
- 30.Taccone F, Van Goethem N, De Pauw R, et al. The role of organizational characteristics on the outcome of COVID-19 patients admitted to the ICU in Belgium. Lancet Reg Health Eur. 2021;3 doi: 10.1016/j.lanepe.2020.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bruyneel A, Gallani M, Tack J, et al. Impact of COVID-19 on nursing time in intensive care units in Belgium. Intensive Crit Care Nurs. 2021;62 doi: 10.1016/j.iccn.2020.102967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lucchini A, Giani M, Elli S, Villa S, Rona R, Foti G. Nursing Activities Score is increased in COVID-19 patients. Intensive Crit Care Nurs. 2020;59 doi: 10.1016/j.iccn.2020.102876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cabarkapa S, Nadjidai S, Murgier J, Ng C. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. Brain Behav Immun Health. 2020;8 doi: 10.1016/j.bbih.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cotel A, Golu F, Pantea Stoian A, et al. Predictors of burnout in healthcare workers during the COVID-19 pandemic. Healthcare (Basel) 2021;9(3):304. doi: 10.3390/healthcare9030304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duncan D. What the COVID-19 pandemic tells us about the need to develop resilience in the nursing workforce. Nurs Manag (Harrow) 2020;27(3):22–27. doi: 10.7748/nm.2020.e1933. [DOI] [PubMed] [Google Scholar]
- 36.Nelson S, Lee-Winn A. The mental turmoil of hospital nurses in the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S126–S127. doi: 10.1037/tra0000810. [DOI] [PubMed] [Google Scholar]
- 37.Fisher MEM, Oudshoorn A. Debriefing for professional practice placements in nursing: a concept analysis. Nurs Educ Perspect. 2019;40(4):199–204. doi: 10.1097/01.NEP.0000000000000487. [DOI] [PubMed] [Google Scholar]
- 38.Plowe K. Increasing resiliency: a focus for clinical conferencing /group debriefing in nursing education. Nurse Educ Pract. 2020;49 doi: 10.1016/j.nepr.2020.102882. [DOI] [PubMed] [Google Scholar]
- 39.Schmidt M, Haglund K. Debrief in emergency departments to improve compassion fatigue and promote resiliency. J Trauma Nurs. 2017;24(5):317–322. doi: 10.1097/JTN.0000000000000315. [DOI] [PubMed] [Google Scholar]