Abstract
Globally, effective emergency response to disease outbreaks is usually affected by weak coordination. However, coordination using an incident management system (IMS) in line with a One Health approach involving human, environment, and animal health with collaborations between government and non-governmental agencies result in improved response outcome for zoonotic diseases such as Lassa fever (LF).
We provide an overview of the 2019 LF outbreak response in Nigeria using the IMS and One Health approach. The response was coordinated via ten Emergency Operation Centre (EOC) response pillars. Cardinal response activities included activation of EOC, development of an incident action plan, deployment of One Health rapid response teams to support affected states, mid-outbreak review and after-action review meetings.
Between 1st January and 29th December 2019, of the 5057 people tested for LF, 833 were confirmed positive from 23 States, across 86 Local Government Areas. Of the 833 confirmed cases, 650 (78%) were from hotspot States of Edo (36%), Ondo (26%) and Ebonyi (16%). Those in the age-group 21–40 years (47%) were mostly affected, with a male to female ratio of 1:1. Twenty healthcare workers were affected. Two LF naïve states Kebbi and Zamfara, reported confirmed cases for the first time during this period.
The outbreak peaked earlier in the year compared to previous years, and the emergency phase of the outbreak was declared over by epidemiological week 17 based on low national threshold composite indicators over a period of six consecutive weeks.
Multisectoral and multidisciplinary strategic One Health EOC coordination at all levels facilitated the swift containment of Nigeria's large LF outbreak in 2019. It is therefore imperative to embrace One Health approach embedded within the EOC to holistically address the increasing LF incidence in Nigeria.
Keywords: One Health, Lassa fever, Incident management system, Emergency operation centre
1. Introduction
Globally, effective emergency response to disease outbreak or events of public health importance is usually affected by weak multidiscipline and multi-sectoral coordination [1]. However, a well-coordinated incident management approach involving multiple stakeholders across human, environment and animal health sectors has been shown to yield better outbreak response outcomes particularly for zoonotic diseases [2]. The concept of One Health provides a platform for implementing joint response to infectious disease health threats such as Lassa fever (LF). The World Health Organisation (WHO) defines ‘One Health’ as an approach of designing and implementing programmes, policies, legislation, and research in which multiple sectors communicate and collaborate to achieve better public health outcomes [3].
The 2017 Joint External Evaluation (JEE) of the International Health Regulations (IHR) core capacities in Nigeria demonstrated critical gaps including absence of a national strategy for proper coordination and institutionalisation of One Health in the country [4]. To address some of the gaps identified in the JEE, the 5-year One Health Strategic Plan (2019–2023) was developed and launched in 2019. Implementing this strategy in incident management of a priority infectious disease outbreak in the country could be an effective way of demonstrating the utility of the One Health approach in improving public health outcomes and health system resilience [5].
Since 2016, there has been an increase in the number of reported LF cases from West Africa, especially with the large 2018 outbreak in Nigeria. This increase has mainly been attributed to the complex interplay of increasing human–rodent interactions, improved case detection, heightened awareness, availability of diagnostics and therapeutics, improved disease surveillance systems, and changing demographics as opposed to the initial speculation of the emergence of a new Lassa virus (LASV) variant [6].
In recent years, the deviation from the usual dry seasonal to incessant all year transmission suggests a shift in the epidemiology of the disease, although high transmission still occurs in the dry season between December and March [7]. Factors such as seasonal changes, urbanisation, poor environmental sanitation, deforestation and voluntary or involuntary migration may have contributed to the sustained increase in LASV transmission and spill-over into human populations [8,9].
Given the role of the human, animal, and environmental interface in the increasing transmission of LF, the need for a multi-sectoral One Health approach for surveillance, early detection of spill over into human populations, and rapid public health emergency response during outbreaks cannot be overemphasised [9]. Hence, following the upsurge in LF cases in the first three weeks of January 2019, the Nigeria Centre for Disease Control (NCDC) on January 22, 2019 activated the LF One Health Emergency Operation Centre (EOC) to ensure a holistic response and early containment of the outbreak. This paper provides an overview of the 2019 LF outbreak response in Nigeria using the One Health approach Incident Management System (IMS).
2. Epidemiological overview of the 2019 Lassa fever outbreak
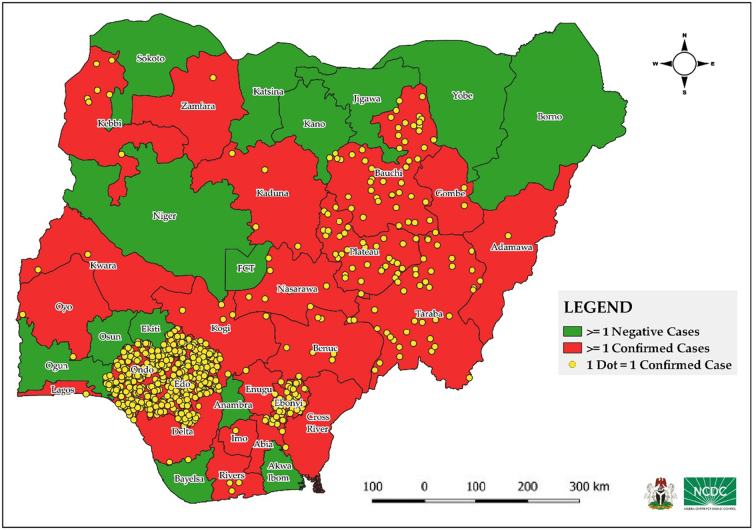
Between January 1 and December 29, 2019, a total of 5057 LF suspected cases were reported from 36 states and the Federal Capital Territory, of which 833 (16.6%) were laboratory confirmed cases, with 19 probable cases [10]. Deaths among confirmed cases were 174, with a case fatality rate (CFR) of 21%. Twenty-three States recorded at least one confirmed case across 86 local government areas (LGAs) Fig. 1. LF naïve states such as Kebbi and Zamfara reported confirmed cases for the first time.
Fig. 1.
Map Nigeria showing distribution of confirmed Lassa fever cases in Nigeria, 2019.
Majority (78%) of the confirmed cases were reported from Edo (37%), Ondo (34%) and Ebonyi (7%), the three historical “hotspot” States characterised by high incidence and prevalence with sustained all year-round transmission Fig. 2. Those in the age-group 21–40 years (47%) were majorly affected with a male to female ratio of 1:1. Twenty (3%) of total confirmed cases occurred among health care workers (HCWs). A total of 9379 contacts were identified from 21 States, of which 144 (1.5%) became symptomatic and 68 (0.7%) tested positive [10].
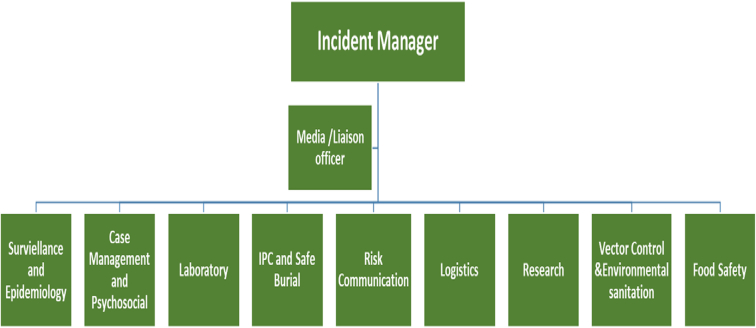
Fig. 2.
2019 National Lassa fever IMS structure.
3. Multi sectoral response using “One Health” EOC approach
3.1. Coordination
Following the rapid increase of LF cases reported in the first three weeks of 2019, a risk assessment was conducted and findings necessitated activation of a level two LF national EOC on January 22, 2019. The International Health Regulation (IHR) Annex 2 decision instrument was used to assess the outbreak , outcome of the assessment led to immediate notification of World Health Organisation (WHO) i in accordance with article 6 of the IHR 2005.
The national EOC coordinated the implementation of several key activities via the ten response pillars: coordination, surveillance, case management, infection prevention and control/safe burial, laboratory, risk communication, logistics, food safety, environmental sanitation plus vector control, and research (Fig. 2). Leveraging on strong multisectoral and multipartner collaboration through a combination of technical and financial support, a One Health IMS coordinated response was mounted through the implementation of a transparent and accountable incident action plan (IAP). Resource mobilisation meetings were held with donors/partners to justify financial support for the outbreak response activities.
Multi-sectoral One Health national rapid response teams (RRT) comprising of epidemiologists, clinicians, data analysts, veterinarians, environmental health officers, risk communication officers, surveillance officers, and laboratorians were deployed to the seven majorly affected states to provide onsite technical support while other affected states were supported remotely. WHO Global Outbreak Alert Response Network (GOARN) deployed an epidemiologist while UK-Public Health Rapid Support Team (PHRST) deployed two epidemiologists to support the response.
State level One Health EOCs were activated with support from national RRT and partners for effective outbreak response coordination at the sub-national level. To ensure timely information sharing for action and effective monitoring of outbreak response, weekly teleconference meetings were held with the state EOCs and the treatment centres while weekly situation reports were developed and shared with stakeholders.
A mid-outbreak review meeting was conducted by epidemiological week eight, four weeks post outbreak emergency declaration to review the outbreak response activities and improve the identified gaps. Following decline in cases, the emergency phase of the outbreak was declared over by epidemiological week 17 in accordance with the established low national threshold composite indicators [11].
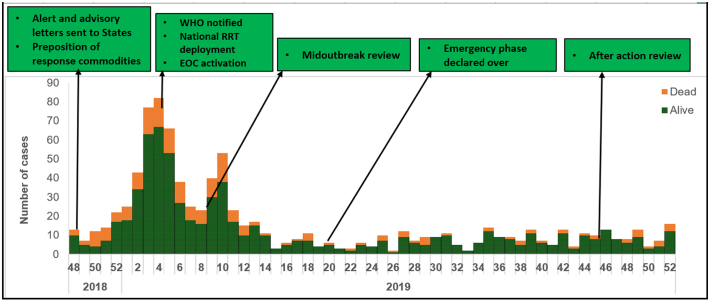
By epidemiological week 38, in line with the WHO IHR monitoring and evaluation framework, an outbreak after action review (AAR) meeting was convened with all key national and subnational stakeholders to share experiences, identify best practices, gaps and lessons learnt to strengthen subsequent preparedness and response measures to LF outbreak in Nigeria (Fig. 3).
Fig. 3.
Epidemic curve of 2019 Lassa fever outbreak in Nigeria with timeline of key response activities.
3.2. Case management and psychosocial support
Patients with suspected or confirmed LASV infections during outbreaks were managed in dedicated LF isolation wards with facilities for enhanced supportive care including dialysis and respiratory support. This decreases case fatality rate and healthcare associated infection. [8,12]. The case management pillar coordinates the management of confirmed cases in the designated treatment/isolation centres across the country. Ten new treatment centres were identified, assessed, and designated as LF treatment centres in addition to the existing twelve treatment centres in-country to cater for the increasing incidence of LF. Capacity building and sensitisation of healthcare workers and professional bodies were conducted to heighten LFindex of suspicion. In-depth investigation of 20 healthcare worker infections as well as review of LF associated deaths was conducted. In addition, the team reviewed and disseminated the case management guidelines to healthcare workers. Surge staff - physicians, nurses, laboratorians, and hygienists were deployed to the overwhelmed treatment centres and corresponding laboratories to support limited human resource capacity. Out-of-pocket payment for LF treatment in most treatment centres could also have affected the health seeking behaviour leading to delayed presentation with attendant mortalities.
Psychosocial support, a component of LF case management intended to provide holistic and improved quality of care for LF patients was introduced to help LF patients and their relatives overcome the fear and stigmatisation associated with the uncertainties of the disease [13].
3.3. Infection prevention and control/safe and dignified burial
The Infection Prevention and Control (IPC) strategy allowed for outbreak response to be used for health systems strengthening. The response aimed at addressing issues related to increased index of suspicion, provision of IPC supplies and enforcement of the application of standard IPC precautions in all health facilities in the affected areas to minimize nosocomial infections.
IPC assessments were carried out in identified treatment centres and the national Viral Haemorrhagic Fever IPC guideline was reviewed and disseminated to healthcare workers. In addition to promoting the need for improved personal hygiene and safe burial practices, the concept of “IPC ring strategy” was also introduced in the hotspot LGAs. The ring strategy involved sensitisation of HCWs to have a high index of suspicion and adhere strictly to IPC measures irrespective of provisional diagnosis at identified health facilities in high-risk areas where LF cases were most likely to present. A mapping of health facilities in the three hotspot LGAs in the six highest burden states was also conducted as well as an assessment of the IPC capacity in these health facilities. The assessments will inform future strengthening/establishment of IPC programmes in these health facilities. Furthermore, subnational safe/dignified burial teams were established and trained using the national safe burial protocol to prevent further transmission of the infection through unsafe burial rites.
3.4. Surveillance
Continuous monitoring of LF outbreak indicators enabled early detection and transition to an emergency mode. Alert and epidemic threshold (composite) indicators were set after thorough analysis of historical data and once threshold was exceeded, triggered the activation of the EOC [11].
The surveillance outbreak response management and analysis system (SORMAS) which is a real-time national data management system was utilised in fifteen states including the three hotspot states - Edo, Ondo and Ebonyi to improve incident case reporting and investigation on LF [14]. Standard operating procedures on contact tracing and active case search were developed and used to train state surveillance officers. Weekly analysis of data for situation reports were conducted and reviewed by the EOC to inform the response and deployment of RRTs.
Intensified outbreak preparedness and response activities including enhanced surveillance were instituted across all states in the country, regardless of outbreak status to ensure all cases-at-risk, were rapidly detected, investigated, and reported.
Cross border active case searching in neighbouring country of Benin republic was conducted at Baruten and Saki LGA in Kwara, and Oyo states respectively, following the report of possible exportation of cases to Benin Republic, however no cases were detected [15].
Event based surveillance (EBS) signals on LF transmission, prevention and control as well as outbreak rumours were received from general public via phone calls, text messages, email and social media using 3 key receptors: Tatafo, the NCDC Connect Centre, and manual searches [16]. These alerts were escalated, investigated, and responded to via appropriate communication and notification channels.
3.5. Laboratory
The LF testing algorithm was standardised across the four LF testing laboratory network- Lagos university teaching hospital (LUTH), Irrua specialist teaching hospital (ISTH), Alex Ekwueme university teaching hospital (AEFUTHA) and National reference laboratory (NRL). A fifth LF testing laboratory in Nigeria was established in Ondo state through the support of Pan-African network for rapid, research, response and preparedness for infectious disease epidemics (PANDORA) to improve the result turnaround time. A national sample transportation framework from all state capitals to the reference LF testing laboratories was established to improve the result turnaround time; however, this framework was not extended to sample transportation from the LGAs/communities to the state capitals and this remains a great challenge. A total of 5057 samples were tested using real time polymerase chain reaction test in the five laboratories on the LF Laboratory testing network. Chain of custody forms were developed and training on sample triple packaging conducted for state laboratory focal persons to improve sample integrity. Overall, turnaround time from sample collection to result dissemination improved from median of 72 h in 2018 to 48 h in 2019. Genomic sequencing of positive LF samples was conducted during the outbreak to ascertain the predominant mode of transmission pattern which showed more of zoonotic spill-over and not of human-to-human transmission, contradicting the speculation of a possible new virus variant in circulation [17].
3.6. Risk Communication and social mobilisation
Risk communication, community mobilisation, and advocacy are comprehensive behaviour change and awareness creation strategy to support the reduction of LF transmission. In collaboration with private, public and civil society organisation, intensive risk communication activities were conducted via media appearances, press releases, advisories, stakeholders' advocacy to political, traditional and religious leaders. LF naïve states were prioritised with aggressive risk communication to improve the awareness. Sensitisation activities on LF transmission, prevention and control practices, environmental sanitation and safe food processing methods were conducted via social and traditional media platforms. NCDC convened a multisectoral content development meeting to review the existing LF information, education and communication (IEC) materials to reflect One Health messaging.
3.7. Logistics and supply chain management
Logistics and supply chain management is a critical aspect of emergency response. Response commodities such as medicines, personal protective equipment (PPE), guidelines, IEC materials and reagents were distributed across all 36 states and the Federal Capital Territory, treatment centres and laboratories. Stockout of response materials such medicines and PPEs were averted through effective forecasting and prepositioning of response commodities as component of outbreak preparedness measure. State Logistic focal persons were identified and trained on inventory management to ensure sustainability of supply chain framework at subnational level.
3.8. Research
Research was introduced as a pillar to the existing EOC response pillars following the large LF outbreak in 2018. With the support of the WHO, the national LF research Plan was developed the same year, with the aim to identify, facilitate and support the conduct of research that would improve knowledge about LF and inform appropriate, evidence-based prevention, response, and control activities of the disease [18]. An example would be a study conducted from the 2019 response on investigating the factors associated with delayed presentation to healthcare facilities of LF cases [19].
In January 2019, the NCDC convened the first Lassa Fever International Conference in Abuja, Nigeria, many questions were raised and the need to support further research on various aspects of LF was reiterated. In the same vein, the Nigeria Lassa Fever Research Consortium was inaugurated, consisting of treatment centres, academia, supporting partners and coordinated by the NCDC.
3.9. Environmental sanitation, food safety and vector control - Integrated One Health approach
Environmental Health and Animal health Interventions are pivotal for the prevention and control of zoonotic diseases. The exponential growth of human population, human encroachment on ecosystems, increased need for farming and exploration of wildlife sources of food, deforestation, and rapid urbanisation have increased the chances of human interaction with animals/wildlife and has resulted in a high risk of contracting zoonotic diseases [8].
Animal and environmental strategies for LF control include implementation of food safety and hygiene practices, environmental sanitation, LF animal surveillance and vector control measures such as use of rodenticides with active local community sensitization and engagement by the LGA environmental health officers and veterinary officers [20]. Using an integrated One Health approach, the pillar supported by WHO, conducted rodent control and community environmental sanitation in high burden Esako-West, Esan-West, Owo and Ose LGAs in Edo and Ondo states, the two major LF hotspot states; collaboratively led by the IPC and risk communication pillars aimed at interrupting the disease transmission pathway.
3.10. Military contribution to Lassa fever response
Effective coordination of public health emergencies involves linking public health practice with security authorities such as the military [4] . The Nigeria ministry of defense (MoD) though not a pillar in the LF EOC work closely with the LF technical working group in the LF response. Following reports of LF cases from the barracks, the LF EOC collaborated with the MoD to strengthen LF surveillance and intensify risk communication within the barracks to ensure early detection, diagnosis, prompt case management and contact tracing. To scale up the existing treatment centres and strengthen surge capacity, the NCDC identified and jointly assessed one military medical facility in each of Nigeria's six geopolitical zones for the purpose of diagnosis and treatment of LF cases.
4. Discussion
The One Health EOC response approach adopted in 2019 LF outbreak response leveraged on the lessons learnt from the large 2018 LF outbreak, led to significant improvement in the outbreak control evidenced by an early peak with a left-shift epidemic curve compared to previous years LF outbreaks. Furthermore, the One Health EOC provided opportunity to synergise the multisectoral response and coordinate collaborations from government and partners thus, the judicious utilization of limited available resources during the outbreak [21].
To operationalise and institutionalise the One Health platform at the three tiers of government in zoonotic disease surveillance and outbreak response, the NCDC in collaboration with other ministries, departments, and agencies, developed a 5-year (2019–2023) strategic plan for One Health in Nigeria. This plan addresses the gaps identified in the Joint External Evaluation of the IHR core capacities. The plan reflects the shared commitment to enhance multi-sectoral collaborations in addressing human animal ecosystem public health challenges. If successfully implemented, the plan will institutionalise the One Health approach, address zoonotic diseases, enhance food safety and security, improve livelihoods of many Nigerians, and keep Nigeria heathier and safer [4,5].
Disease surveillance, outbreak investigation and immediate response activities are primarily the responsibilities of state governments; nevertheless, funding gaps at subnational levels negatively impact the implementation of the incident action plans. Dedicating a substantial budget line for public health emergencies at both national and subnational level is recommended to mitigate this challenge. The national level response was primarily funded by the Regional Disease Surveillance Systems Enhancement (REDISSE) project through the World Bank. The use of this fund at the subnational level could significantly improve preparedness and response in the States. Private sector participation in health emergency funding as part of corporate social responsibility should also be explored through strong advocacy.
The Nigeria Field Epidemiology Training Program (NFETP) is equally an important workforce development strategy that employs the One Health approach in training field epidemiologists. The programme is helping to advance the nation's goal of having at least one field epidemiologist to 200,000 population [22]. However, with the increasing need of a One Health RRT, the environment track should be incorporated in either the frontline or intermediate training programmes. Deployment of National RRT drawn from NCDC, inclusive of NFELTP residents/graduates, Federal Ministry of Agriculture and Rural Development (FMARD), Federal Ministry of Environment (FMoEnv) to the seven most affected states further reinforces the operationalisation of the One Health approach.
The Northeast humanitarian crisis was thought to complicate the response as three north east states: Taraba, Adamawa and Bauchi reported a significant proportion of confirmed cases by the epidemiological week 7 of 2019. Special attention was therefore channelled to controlling the outbreak in the Northeast due to the prevailing humanitarian crisis and deficient infection prevention and control [23].
Health workers are at risk of nosocomial LF infection with identified risks being the low index of suspicion among HCWs, inadequate IPC supplies and low adherence to the minimal standard IPC precautions [24]. The 2018 outbreak was heralded by cluster of cases among HCWs however, fewer HCWs were affected in the 2019 outbreak.
Implementation of continuous rodent control measures, enforcement of environmental sanitation and food safety practices; institutionalisation of infection prevention and control governance at all levels, introduction of free LF treatment and establishment of LF diagnostic laboratories in all geopolitical zones, establishment of EOC in all states in addition to timely release of adequate response funds, were critical recommendations from the AAR meeting to consolidate and institutionalise effective One Health IMS for LF in Nigeria.
5. Conclusion
In response to the large Lassa fever 2019 outbreak in Nigeria, the multisectoral and multidisciplinary strategic One Health EOC coordination at national and subnational levels facilitated the swift containment of the outbreak. From our perspective, an integrated One Health coordination mechanism using the IMS is currently the best fit-for-purpose approach to holistically address the increasing LF incidence in Nigeria.
Funding
No funding was received for this study.
Authorship contributions
Conceptualisation: CD-N Writing – original draft: CD-N. Writing – subsequent drafts, review and editing: CD-N, CLO, AO, RO, EE, TO, OO, EM, WU, MO, UA, NC, HB, GN, OI, YF, SW, AA, AI, MA, CA, LB, AA, GJ, CE, MS, ND, IO, MK, RO,CO, FM, CM, NU, FF, EA, NM, OA, Supervision: CLO, AO, EI, PN, and CI. All authors reviewed the article, contributed to interpretation, and approved the final version.
Declaration of Competing Interest
The authors declare there is no conflict of interest.
Acknowledgements
The authors would like to appreciate the hardwork, commitment and dedication of the National Lassa fever Emergency operations centre, the epidemiology teams of Nigerian State ministries of health, Lassa fever treatment centres and Lassa fever testing laboratory network towards the fight against LF.
References
- 1.Olu O., Usman A., Woldetsadik S., Chamla D., Walker O. Lessons learnt from coordinating emergency health response during humanitarian crises: a case study of implementation of the health cluster in northern Uganda. Conflict Health [Internet] 2014 May 29;9(1):1–9. doi: 10.1186/1752-1505-9-1. http://www.conflictandhealth.com/content/9/1/1 [cited 2021 May 15]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.FAO, OIE, WHO . The Food and Agriculture Organization of the United Nations and The World Organisation for Animal Health and The World Health Organization; 2019. A Tripartite Guide to Addressing Zoonotic Diseases in Countries Taking a Multisectoral, One Health Approach. [Google Scholar]
- 3.WHO One Health [Internet] September, 2017. www.who.int/features/qa/one-health/en/https://www.who.int/news-room/q-a-detail/one-health [cited 2021 May 15]. Available from:
- 4.WHO . 2017. Joint External Evaluation of IHR Core Capacities Federal Republic of Nigeria. [Google Scholar]
- 5.Federal Ministry of Health . NCDC; 2019. Federal Ministry of Agriculture and Rural Development and, Federal Ministry of Environment. One Health Strategic Plan 2019–2023. [Google Scholar]
- 6.Ilori E.A., Frank C., Dan-Nwafor C.C., Ipadeola O., Krings A., Ukponu W., et al. Increase in lassa fever cases in Nigeria, January–March 2018. Emerg. Infect. Dis. 2019;25(5) doi: 10.3201/eid2505.181247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine . The National Academies. Microbial Threats to Health. National Academies Press; Washington, DC: 2003. Microbial Threats to Health: Emergence, Detection, and Response. [PubMed] [Google Scholar]
- 8.Asogun D.A., Günther S., Akpede G.O., Ihekweazu C., Zumla A. Vol. 33. Infectious Disease Clinics of North America; W.B. Saunders: 2019. Lassa Fever: Epidemiology, Clinical Features, Diagnosis, Management and Prevention; pp. 933–951. [DOI] [PubMed] [Google Scholar]
- 9.Tambo E., Adetunde O.T., Olalubi O.A. Infectious Diseases of Poverty. Vol. 7. BioMed Central Ltd; 2018. Re-emerging Lassa fever outbreaks in Nigeria: Re-enforcing “One Health” community surveillance and emergency response practice [Internet] p. 37.http://creativecommons.org/publicdomain/zero/1.0/ [cited 2021 May 15]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nigeria Centre for Disease Control . 2019. An update of Lassa fever outbreak in Nigeria for Week 52. [Google Scholar]
- 11.Ipadeola O., Furuse Y., de Gooyer T., Dan-Nwafor C., Namara G., Ilori E., et al. Determination of the emergency phase for response against endemic disease outbreak: a case of lassa fever outbreak in Nigeria. J. Global Health [Internet]. 2020 Dec 1;10(2):1–4. doi: 10.7189/jogh.10.020353. https://pubmed.ncbi.nlm.nih.gov/33110549/ [cited 2021 May 15]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CDC Lassa Fever | CDC [Internet] https://www.cdc.gov/vhf/lassa/index.html [cited 2021 May 15]. Available from:
- 13.Tobin EA, Akhere Asogun D, Okonofua M, Ogbaini-Emovon E, Efediyi G. A qualitative study of psychological support needs of family caregivers of hospitalized Lassa fever patients during an outbreak in an endemic state in Nigeria. Int. J. Psychol. Counsel., 12(4):115–23. Available from: http://www.academicjournals.org/IJPC.
- 14.Tom-Aba D., Silenou B.C., Doerrbecker J., Fourie C., Leitner C., Wahnschaffe M., et al. The surveillance outbreak response management and analysis system (SORMAS): digital health global goods maturity assessment. JMIR Public Health Surv. [Internet]. 2020 Apr 1;6(2) doi: 10.2196/15860. [cited 2021 May 15]. Available from: /pmc/articles/PMC7221633/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kakai C.G., Okunromade O.F., Dan-Nwafor C.C., Chabi A.I.B., Martial G.T.P., Dalhat M.M., et al. Vol. 18. Health Security. Mary Ann Liebert Inc; 2020. Improving Cross-Border Preparedness and Response: Lessons Learned from 3 Lassa Fever Outbreaks Across Benin, Nigeria, and Togo, 2017–2019 [Internet] pp. S105–S112.https://pubmed.ncbi.nlm.nih.gov/32004125/ [cited 2021 May 15]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beebeejaun K., Elston J., Oliver I., Ihueze A., Ukenedo C., Aruna O., et al. Emerging Infectious Diseases. Centers for Disease Control and Prevention (CDC) Vol. 27. 2021. Evaluation of national event-based surveillance, nigeria, 2016–2018; pp. 694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guy Baele ARTIC Network 2019 Lassa virus sequencing in Nigeria - Final field report (75 samples) - Lassa virus / Lassa virus Nigeria 2019 - Virological [Internet] https://virological.org/t/2019-lassa-virus-sequencing-in-nigeria-final-field-report-75-samples/291 [cited 2021 May 15]. Available from:
- 18.Olayinka A.T., Dan Nwafor C., Akano A., Jan K., Ebhodaghe B., Elimian K., et al. Research as a pillar of lassa fever emergency response: Lessons from nigeria [Internet] Pan African Med. J. 2020;Vol. 37:1–5. doi: 10.11604/pamj.2020.37.179.26425. https://www.panafrican-med-journal.com/content/article/37/179/full African Field Epidemiology Network. [cited 2021 May 15]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chandra N.L., Bolt H., Dan-Nwafor C., Ipadeola O., Ilori E., Namara G., et al. Factors associated with delayed presentation to healthcare facilities for Lassa fever cases, Nigeria 2019: a retrospective cohort study. BMC Infect. Dis. [Internet]. 2021 Dec 1;21(1):1–11. doi: 10.1186/s12879-021-05822-4. [cited 2021 May 15]. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mari Saez A., Cherif Haidara M., Camara A., Kourouma F., Sage M., Magassouba N., et al. Rodent control to fight Lassa fever: Evaluation and lessons learned from a 4-year study in Upper Guinea. PLoS Neglect. Trop. Dis. [Internet]. 2018 Nov 1;12(11) doi: 10.1371/journal.pntd.0006829. e0006829. Available from. [Cited 2021 May 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nyatanyi T., Wilkes M., McDermott H., Nzietchueng S., Gafarasi I., Mudakikwa A., et al. Implementing one health as an integrated approach to health in Rwanda. BMJ Global Health [Internet]. 2017 Feb 1;2(1):121. doi: 10.1136/bmjgh-2016-000121. http://gh.bmj.com/ [cited 2021 May 15]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nigeria Centre for Disease Control National action plan for health security federal republic of Nigeria 2018–2022 [Internet] https://ncdcnaija.azurewebsites.net/themes/common/files/establishment/5e88f9e22d2b4e4563b527005c8a0c43.pdf [cited 2021 Feb 15]. Available from:
- 23.Bishara D.B., Oladipo S., Lawi M., Ini N., Collins O., Chima O.E. 2019. An Assessment of Hand Hygiene in Healthcare Facilities in Protracted Crisis Environment. [Google Scholar]
- 24.Dan-Nwafor C.C., Ipadeola O., Smout E., Ilori E., Adeyemo A., Umeokonkwo C., et al. A cluster of nosocomial Lassa fever cases in a tertiary health facility in Nigeria: description and lessons learned, 2018. Int. J. Infect. Dis. [Internet]. 2019 Jun 1;83:88–94. doi: 10.1016/j.ijid.2019.03.030. https://pubmed.ncbi.nlm.nih.gov/30930184/ [cited 2021 May 15]. Available from: [DOI] [PubMed] [Google Scholar]