Abstract
Efferocytosis, the phagocytosis of apoptotic cells performed by both specialized phagocytes (such as macrophages) and non-specialized phagocytes (such as epithelial cells), is involved in tissue repair and homeostasis. Effective efferocytosis prevents secondary necrosis, terminates inflammatory responses, promotes self-tolerance and activates pro-resolving pathways to maintain homeostasis. When efferocytosis is impaired, apoptotic cells that could not be cleared in time aggregate, resulting in the necrosis of apoptotic cells and release of pro-inflammatory factors. In addition, defective efferocytosis inhibits the intracellular cholesterol reverse transportation pathways, which may lead to atherosclerosis, lung damage, non-alcoholic fatty liver disease and neurodegenerative diseases. The uncleared apoptotic cells can also release autoantigens, which can cause autoimmune diseases. Cancer cells escape from phagocytosis via efferocytosis. Therefore, new treatment strategies for diseases related to defective efferocytosis are proposed. This review illustrated the mechanisms of efferocytosis in multisystem diseases and organismal homeostasis and the pathophysiological consequences of defective efferocytosis. Several drugs and treatments available to enhance efferocytosis are also mentioned in the review, serving as new evidence for clinical application.
Keywords: efferocytosis, cardiovascular diseases, respiratory diseases, liver and intestine diseases, autoimmune diseases, neurodegenerative diseases
1. Introduction
Efferocytosis refers to the physiological process in which phagocytic cells clear apoptotic cells (ACs) (1). Phagocytosis involves both specialized phagocytes (such as macrophages) and non-specialized phagocytes (such as epithelial cells) (2).
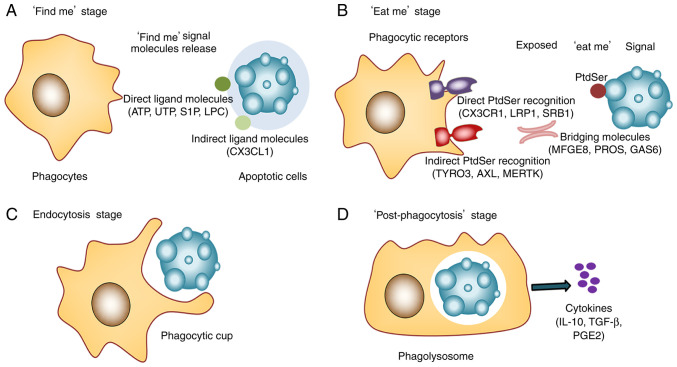
Efferocytosis can be divided into four stages (2) (Fig. 1): i) ‘Find me’ stage. Chemotactic factors induce macrophages to recognize and surround ACs. The ‘find me’ signal molecules released by ACs are recognized by homologous receptors on the surface of phagocytes, to induce the migration and recruitment of phagocytes to ACs (3). ii) ‘Eat me’ stage. Phagocytic receptors of macrophages recognize and bind to the ‘eat me’ signal molecules of ACs through bridging molecules. Following the programmed cell apoptosis, the ‘eat me’ signal molecule ligands on the AC surface are exposed, which can directly bind to the ‘eat me’ signal molecule receptors on the surface of phagocytes (4). Then, one end of the bridging molecules, as signal molecules related to efferocytosis, binds to the ligand of ‘eat me’ signal molecule of ACS and the other end binds to the receptor of the ‘eat me’ signal molecule on the surface of the phagocyte. Therefore, the phagocytes recognize and capture ACs in the direct ‘ligand-receptor’ binding form and the indirect ‘ligand-bridging molecule-receptor’ binding form (5). iii) Endocytosis stage. The ‘eat me’ signal molecules binding to phagocytic receptors activate the programmed cell removal system to form ‘a phagocytic cup’ and complete the endocytosis of ACs (6). iv) ‘Post-phagocytosis’ stage. Macrophages further digest and degrade apoptotic cell debris, activating multiple metabolic signaling pathways (7). After phagocytic cells engulf ACs, phagosomes are formed and then fuse with primary lysosomes to form phagolysosomes (8). When the phagolysosome matures, it begins to degrade ACs and release anti-inflammatory cytokines such as IL-10 and TGF-β (5).
Figure 1.
Four stages of efferocytosis. (A) ‘Find me’ stage. Chemotactic factors induce macrophages to recognize and surround ACs. The ‘find me’ signal molecules released by ACs are recognized by phagocytes, inducing the migration and recruitment of phagocytes to ACs. (B) ‘Eat me’ stage. Phagocytic receptors of macrophages recognize and bind to the ‘eat me’ signal molecules of ACs. (C) Endocytosis stage. Forming ‘a phagocytic cup’ completes the endocytosis of ACs. (D) ‘Post-phagocytosis’ stage. Macrophages further digest and degrade apoptotic cell debris, activating multiple metabolic signaling pathways. ATP, triphosphate nucleotides adenosine triphosphate; UTP, uridine-5′-triphosphate; S1P, sphingosine-1-phosphate; LPC, lyso-phosphatidylcholine; CX3CL1, CX3C chemokine ligand 1; CX3CR1, CX3C chemokine receptor 1; LRP1, low-density lipoprotein receptor related proteins 1; SRB1, scavenger receptor 1; MFGE8, milk fat globule-epidermal growth factor; ProS, protein S; PtdSer, phosphatidylserine; GAS6, growth arrest specific protein 6; TYRO3/AXL/MERTK, TAM receptors.
In efferocytosis, a number of molecules function to clear ACs promptly so that normal tissues cannot be damaged. First, the ‘find me’ signal molecules, consisting of direct ligand molecules and indirect signal molecules, are released after cell apoptosis. The direct ligand molecules include triphosphate nucleotides ATP, uridine-5′-triphosphate (9), lyso-phosphatidylcholine (10) and sphingosine-1-phosphate (11). The indirect signal molecules include CX3C chemokine ligand 1 (CX3CL1) protein (12). Second, the ‘find me’ signal is received by phagocytic cell receptors. Then the phagocytic receptors, including receptor G2 accumulation (13), CX3C chemokine receptor 1 (CX3CR1) (12), low-density lipoprotein receptor related proteins 1 (LRP1) (14) and scavenger receptor class B type 1 (SRB1), directly interact with ‘eat-me’ signal molecules on the surface of ACs, such as phosphatidylserine (PtdSer) (15), oxidized phospholipids and endoplasmic reticulum-resident protein calreticulin (16). The phagocytic receptors, such as Mer tyrosine protein kinase receptor (Mertk) (17), also interact with ‘eat-me’ signal molecules indirectly through bridging molecules (5). Extracellular bridging molecules link phagocytes with ACs, activate the phagocytic function of phagocytes and remove the ACs, such as milk fat globule-epidermal growth factor (MFGE8), serum complement C1q, transglutaminase 2, human growth arrest specific protein 6 (GAS6) and protein S (ProS) (17). These signaling molecules and extracellular bridging molecules are key to efferocytosis. In addition, the ‘not eat me’ signal in non-apoptotic cells prevents viable cells from being cleared by phagocytes. Among them, the best-known signal molecule is CD47 (18; Table I).
Table I.
Summary of efferocytosis related molecules.
| Author(s), year | Role in efferocytosis | Cell source | Molecules | (Refs.) |
|---|---|---|---|---|
| Elliott et al, 2009 | ‘Find me’ signal | Apoptotic cells | ATP, UTP | (9) |
| Lauber et al, 2003 | LPC | (10) | ||
| Gude et al, 2008 | S1P | (11) | ||
| Truman et al, 2008 | CX3CL1 | (12) | ||
| Peter et al, 2008 | Phagocytic cells | G2A | (13) | |
| Truman et al, 2008 | CX3CR1 | (12) | ||
| Gardai et al, 2005 | LRP1, | (14) | ||
| Gardai et al, 2005 | SRB1 | (14) | ||
| Elliott et al, 2009 | P2Y2 | (9) | ||
| Appelt et al, 2005 | ‘Eat me’ signal | Apoptotic cells | PtdSer | (15) |
| Nagata et al, 2010 | oxidized phospholipids, endoplasmic reticulum-resident protein calreticulin | (16) | ||
| Geng et al, 2017 | Phagocytic cells | TAM, TIM, TG2 | (17) | |
| Geng et al, 2017 | Bridging molecules | Apoptotic/phagocytic cell | MFGE8, GAS6, Pro S, serum complement C1q, Thbs1, Anx I | (17) |
| Ravichandran, 2010 | ‘Not eat me’ signal | Apoptotic cells | CD47, CD31 | (18) |
| Gheibi Hayat et al, 2019 | Phagocytic cells | SIRPα | (201) |
Anx I, Annexin I; ATP, triphosphate nucleotides adenosine triphosphate; CX3CL1, CX3C chemokine ligand 1; CX3CR1, CX3C chemokine receptor 1; GAS6, human growth arrest specific protein 6; G2A, receptor G2 accumulation; LPC, lyso-phosphatidylcholine; LRP1, low-density lipoprotein receptor related proteins 1; MFGE8, milk fat globule-epidermal growth factor; PtdSer, phosphatidylserine; ProS, protein S; P2Y2, purnoreceptor-2; SIRPα, signal regulatory protein alpha; SRB1, scavenger receptor 1; S1P, sphingosine-1-phosphate; TAM, TYRO3/Axl/MER tyrosine kinase receptor; TG2, transglutaminase 2; TIM, T cell immunoglobulin mucin; Thbs1, thrombospondin 1; UTP, uridine-5′-triphosphate.
Efferocytosis is essential for human health, because it can prevent the deleterious effects of cell necrosis, thus maintaining the tissue and organ homeostasis (19) and the normal immune response (20). Apart from preventing secondary necrosis, efferocytosis has three functions: Terminating inflammatory responses, promoting self-tolerance and activating pro-resolving pathways (21). Efferocytosis triggers the production of anti-inflammatory and tissue-reparative cytokines, while defective efferocytosis may lead to hyperinflammation and diseases (5).
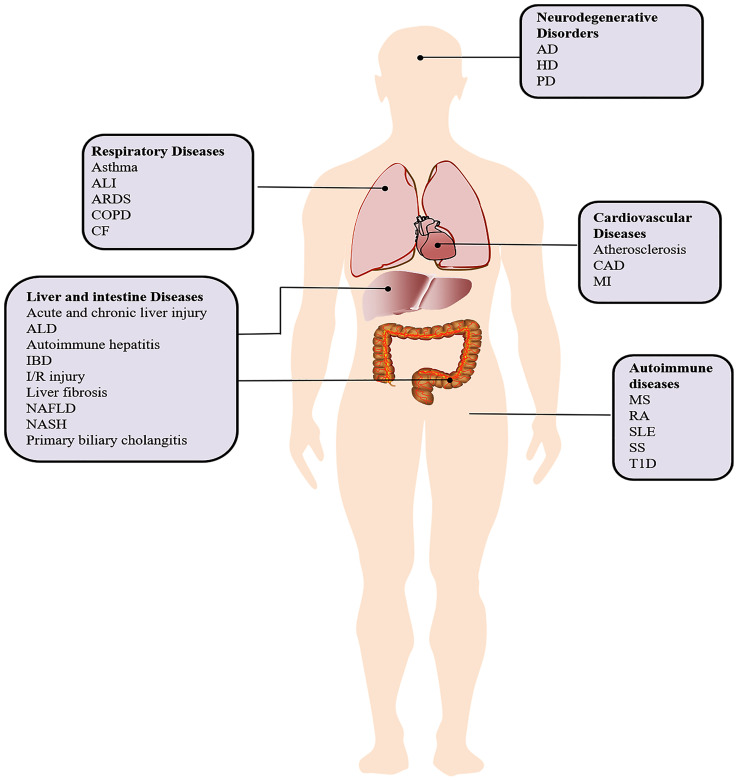
The present study summarized the current knowledge of efferocytosis and the links between efferocytosis and body homeostasis. Further, it reviewed the consequences of impaired efferocytosis in multisystem diseases (Fig. 2; Table II). Several drugs and treatments available to enhance efferocytosis are also mentioned to provide new evidence for clinical application.
Figure 2.
Efferocytosis in multisystem diseases. AD, Alzheimer's disease; ALD, alcoholic liver disease; ALI, acute lung injury; ARDS, acute respiratory distress syndrome; CAD, Coronary artery disease; CF, cystic fibrosis; COPD, chronic obstructive pulmonary disease; HD, Huntington's disease; IBD, inflammatory bowel disease; I/R injury, ischemia-reperfusion injury; MI, Myocardial infarction; MS, multiple sclerosis; NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis; PD, Parkinson's disease; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus; SS, Sjogren's syndrome; T1D, type 1 diabetes.
Table II.
Summary of efferocytosis related molecules and multisystem diseases.
| Author(s), year | Diseases | Molecules | (Refs.) |
|---|---|---|---|
| Fricker et al, 2012 | Alzheimer's disease | MFGE8 ↓ | (146) |
| Zheng et al, 2012 | Tyro3 ↓ | (145) | |
| Kojima et al, 2016 | Atherosclerosis | CD47 ↑ | (33) |
| Holden et al, 2019 | GAS6 ↓ | (202) | |
| Brophy et al, 2019 | LRP1 ↓ | (203) | |
| Ait-Oufella et al, 2008; Zhang et al, 2019; Thorp et al, 2008 | Mertk ↓ | (204–206) | |
| Ait-Oufella et al, 2007 | MFGE8 ↓ | (44) | |
| Boisvert et al, 2006 | TG2 ↓ | (207) | |
| Waterborg et al, 2018 | Arthritis | TAM receptors ↓ | (122) |
| Grabiec et al, 2017 | Asthma | Axl ↓ | (68) |
| Qi et al, 2013 | Autoimmune hepatitis | TAM receptors ↓ | (111) |
| Wan et al, 2013 | Cardiomyopathy | Mertk ↓ | (54) |
| Bosurgi et al, 2013 | Colon cancers | Axl ↓ | (101) |
| Akitake-Kawano et al, 2013 | GAS6 ↓ | (103) | |
| Bosurgi et al, 2013 | Mertk ↓ | (101) | |
| Llacuna et al, 2010 | Liver ischemia/reperfusion injury | GAS6 ↓ | (95) |
| Aziz et al, 2012 | Lung damage | MFGE8 ↓ | (69) |
| Gong et al, 2019 | Lupus nephritis | AXL ↑ | (208) |
| Gong et al, 2019 | GAS6 ↑ | (208) | |
| Gong et al, 2019 | Mertk ↑ | (208) | |
| Tworkoski et al, 2013 | Melanoma | Mertk ↑ | (209) |
| Demarest et al, 2013 | Tyro3 ↑ | (210) | |
| Tutusaus et al, 2020 | Non-alcoholic steatohepatitis | Mertk ↓ | (85) |
| Xie et al, 2015 | Non-small cell lung cancer | Mertk ↑ | (211) |
| Lew et al, 2020 | Retinal degeneration | Mertk ↓ | (177) |
| Walport et al, 1998 | Systemic lupus erythematosus | C1q ↓ | (212) |
| Huang et al, 2017 | MFGE8 ↑ | (213) | |
| Zhu et al, 2014 | Mertk ↑ | (214) | |
| Bertolaccini et al, 2003 | Pro S ↓ | (215) | |
| Ramirez-Ortiz et al, 2013 | SCARF1 ↓ | (120) | |
| Xiao et al, 2012 | TIM 1 ↓ | (119) | |
| Chen et al, 2015 | Sjogren's syndrome | GAS6 ↓ | (131) |
| Qin et al, 2015 | Axl ↓ | (132) | |
| Qin et al, 2015 | Tyro3 ↓ | (132) | |
| Peng and Elkon, 2011 | Type 1 diabetes mellitus | MFGE8 ↓ | (216) |
| Avilla et al, 2011 | Thyroid cancer | Axl ↑ | (217) |
| Avilla et al, 2011 | Tyro3 ↑ | (217) | |
| Bossi et al, 2014 | Wound healing | C1q ↓ | (180) |
GAS6, growth arrest specific protein 6; LRP1, low-density lipoprotein receptor related proteins 1; MFGE8, milk fat globule-epidermal growth factor; SCARF1, scavenger receptor class F, member 1; TAM receptors, Tyro3/Axl/Mertk; TG2, transglutaminase 2; TIM1, T-cell immunoglobulin and mucin domain-containing molecule 1.
2. Cardiovascular diseases
Studies on genome-wide association have discovered that common genetic variants in the chromosome 9p21 confer the risk of coronary artery disease, myocardial infarction (MI) (22) and ischemic stroke (23). The expression of calreticulin protein is reduced in the plaques of these allele carriers (24), while the area of the necrotic core and the number of ACs increase in the plaques of atherosclerosis (25). Calreticulin, located in the endoplasmic reticulum, serves a crucial role in cardiac embryogenesis. It affects cardiac development and myofibrillogenesis and is involved in the pathophysiology of several cardiac pathologies (26). Calreticulin binds to the ‘eat me’ ligand on the surface of ACs, activating LDLR4 on the surface of phagocytic cells and inducing phagocytosis (14). Therefore, the reduction of calreticulin protein of these allele carriers suppresses the ‘eat me’ signal and weakens the phagocytosis of ACs. This explains why efferocytosis is independent of traditional risk factors (such as hypertension, dyslipidemia, diabetes and smoking) of cardiovascular diseases (27).
Atherosclerosis, a major pathological basis for cardiovascular and cerebrovascular diseases, is also the key process in other diseases, such as chronic cerebral insufficiency and cerebral infarction. Atherosclerosis is considered to be a cholesterol storage disease and a lipid-driven inflammatory disease (28). Cholesterol loading is hypothesized to cause pro-inflammatory cytokine secretion and form intracellular cholesterol microcrystals that activate the inflammasome (29). In addition, cholesterol-laden macrophages are ‘foam cells’ that die easily and release their contents in advanced lesions and thereby can worsen the inflammatory status (30). As atherosclerosis is an inflammatory disease, various factors involved in the inflammatory response may be related to the formation of atherosclerotic plaques (31). TNF-α is elevated in the pro-inflammatory early-stage of atherosclerosis. TNF-α inhibits MFGE8, Mertk and LRP1 by activating the Toll-like receptor (TLR) (32) and upregulates CD47 expression to activate the ‘not eat me’ signal (33). TNF-α weakens the efferocytosis and prevents timely clearance of ACs, thereby aggravating the inflammatory response and further worsening atherosclerosis (34). The above reactions form a vicious circle. Therefore, the effect of efferocytosis is gradually impaired as the atherosclerotic plaque progresses.
In atherosclerosis, the clearance of ACs is essential to resolve inflammation. Efferocytosis promotes the resolution of inflammation in a stepwise manner. One step is to recognize and engulf ACs, which prevents AC accumulation and inflammatory agent secretion (35). The engulfment of ACs results in the acquisition of excess cellular materials such as lipids, carbohydrates, proteins and nucleic acids (36). Macrophages need to activate degradation and efflux pathways for increased metabolic load, which is crucial for inflammatory resolution and tissue repair (19). For instance, lipid metabolism activates the nuclear receptors peroxisome proliferator-activated receptor (PPAR) and liver X receptor (LXR)-α, helping release anti-inflammatory cytokines, such as IL-10 and TGF-β (37,38). Efferocytosis within the plaque is impaired when atherosclerotic plaque develops in the late stage (39). A study has confirmed that the ratio of apoptotic cell clearance is nineteen times higher in human tonsils as compared with human atherosclerotic plaques (40). Schrijvers et al (40) found more apoptotic cells outside lesional phagocytes in advanced human coronary artery lesions. Defective efferocytosis leads to post-apoptotic cellular necrosis and the release of proinflammatory factors (41). Failed AC clearance, increased inflammation (42) and worsened atherosclerosis (43,44) were found in mice lacking TIM-4, Mertk, MFGE8, or Pro S. As macrophage apoptosis accelerates under defective efferocytosis, the lipid-laden necrotic core enlarges with the progression of atherosclerotic plaques (45). Thinning fibrous cap, high-level inflammatory cytokines, apoptosis of intimal cells and expansion of the lipid-laden necrotic core all contribute to vulnerable plaques and acute coronary artery syndrome (46). The absence of efferocytosis signals also inhibits the subsequent intracellular cholesterol reverse transportation pathways (24), then promotes foam cell formation and initiates the development of atherosclerosis. C1q protects early atherosclerosis by promoting macrophage survival and improving the function of macrophage foam cells (47).
Effective efferocytosis can inhibit secondary cell necrosis and prevent dead cells from releasing inflammatory factors and toxic molecules, thereby slowing down atherosclerosis progression and reducing plaque vulnerability (32). Enhanced efferocytosis can reverse hypoxia in murine atherosclerosis to prevent necrotic core expansion (48). Natalicone ZB, the specific agonist of LXR, can facilitate efferocytosis, inhibit plaque formation and reduce the area of necrotic core (49). Conventional anti-atherosclerotic drugs, such as statins and non-steroidal PPAR γ agonists, can enhance efferocytosis in plaques (50,51). In atherosclerosis treatment, statin can reduce cholesterol and inflammation, repress the highly expressed Ras homologous gene family member A, a negative regulator of phagocytosis in atherosclerotic lesions (50).
Experimental results have confirmed the regulatory role of extracellular signal-regulated kinase 5 (ERK5) in macrophage phagocytosis. ERK5, one of the mitogen-activated protein kinases, can maintain macrophage phagocytosis and prevent atherosclerosis progression (32). In LDLR−/− mice, ERK5 gene knockout can aggravate atherosclerosis and inhibit the expression of efferocytosis-related proteins (52). ERK5 inhibitor can downregulate the phagocytosis of RAW264.7 cells in vitro (53). Thus, it can be concluded that regulating efferocytosis of macrophages through ERK5 can exert an anti-atherosclerosis effect.
Efferocytosis also serves a role in other cardiovascular diseases. In Wan et al (54), Mertk could clear apoptotic cardiomyocytes following MI, thus mitigating the progression to heart failure, while suppressed efferocytosis could increase infarct size, promote adverse ventricular remodeling and left ventricle functional deterioration after MI and ease the occurrence of cardiomyopathy.
These studies implicate that impaired efferocytosis can result in secondary necrosis, inflammation, cholesterol reverse disorder and thus lead to cardiovascular diseases, such as atherosclerosis and acute coronary artery syndrome. As a crucial modulator in cardiovascular diseases, efferocytosis is worthy of further investigation.
3. Respiratory diseases
Lung diseases are closely related to efferocytosis due to the complex inflammatory and immune responses. When lung inflammation occurs, neutrophils are quickly recruited to the airways. Following phagocytosis of pathogens, neutrophils undergo apoptosis. This process is regulated by multiple genes and multiple factors, such as LPS, TNF-α, Fas/Fas-L pathway, apoptotic genes, interleukins, interferons and Caspase protein (55). Phagocytosis clears apoptotic neutrophils to prevent the release of toxic substances and the subsequent damage to the surrounding tissues, thereby alleviating inflammation (55). Effective efferocytosis protects normal airways, alveolar structures and even the lung tissues (56). For example, Lee et al (57) found Mertk overexpression could attenuate bleomycin-induced lung injury in mice.
By contrast, due to impaired efferocytosis, the number of uncleared ACs increases, which prolongs inflammatory response in the mouse and human models of chronic obstructive pulmonary disease (COPD) and cystic fibrosis (CF) (58). COPD is characterized by chronic inflammation, extracellular matrix destruction and increased apoptosis of airway epithelial cells and neutrophils (59). The macrophage-mediated efferocytosis in the lungs of COPD patients weakens significantly, while efferocytosis strengthens in COPD patients who use statins (60).
Similarly, patients with CF or allergic asthma display protracted inflammation caused by defective efferocytosis (61,62). CF is a heritable disease with infection, airway inflammation and bronchiectasis (63). Sputa examination has shown more ACs in CF patients compared with those with chronic bronchitis (64). Asthma is a complex syndrome with airflow obstruction, bronchial hyper-responsiveness and airway inflammation (65). The resolution of ovalbumin-induced allergic airway inflammation is delayed in Mer-deficient mice (66). Targeting T-cell immunoglobulin and mucin domain-containing molecule (TIM) 1, a member of TIM receptor family, can modulate airway inflammation in mouse models of airway hyper-responsiveness (67). Grabiec et al (68) indicate that the deficiency of Axl receptor tyrosine kinase accelerates asthma progression by exaggerating airway inflammation. The prognosis of acute lung injury (ALI) in mouse models is also influenced by defective efferocytosis. MFGE8 deficient mice with lipopolysaccharide (LPS)-induced acute ALI showed increased inflammatory cytokines and decreased survival (69). Mertk can attenuate LPS-induced lung injury (70).
Common respiratory drugs, such as statins, macrolides and corticosteroids, can alleviate respiratory symptoms by enhancing efferocytosis. Macrolide antibiotics are reported to promote efferocytosis by upregulating the expression of bridging molecules such as collectins (71). These drugs have already been used to treat COPD, cystic fibrosis, or asthma (72). Mannose receptor may be a target of azithromycin to improve phagocytic ability (71). Azithromycin restores the phagocytic function of the airway macrophages by binding to PtdSer in COPD (73). Corticosteroids enhance efferocytosis by downregulating CD47-signal regulatory protein (SIRP) and upregulating Mertk (74). Glucocorticoids, the most commonly used drugs for asthma and COPD, enhance macrophage phagocytosis in vitro and restore the efferocytosis of macrophages in the airway of patients with asthma by regulating Mertk and Pro S (75,76). Grégoire et al (77) also found that blocking high mobility group box-1 (HMGB1) and activating AMP-activated protein kinase (AMPK) by metformin could enhance AC clearance and decrease lung inflammation in patients with acute respiratory distress syndrome (ARDS).
Several chronic lung diseases are characterized by an increased lung burden of uningested apoptotic cells and sustained lung inflammation (58). The efferocytic process favors tissue repair and inflammation suppression (78). Existing therapies such as corticosteroids, statins and macrolides may function in part by augmenting apoptotic cell clearance.
4. Liver and intestine diseases
Kupffer cells and other myeloid phagocytic cells, the most important hepatic efferocytes, are attracted into the liver to remove ACs after injury (79). Bukong et al (80) found that acute alcohol use could significantly impair the clearance of neutrophil extracellular traps by macrophages, which could contribute to prolonged liver inflammation and injury. Mediators released by neutrophils during NETosis can directly corrupt the recognition of apoptotic cells by phagocytes: HMGB1, for example, initiates pro-inflammatory signal whilst simultaneously preventing efferocytosis by obscuring PS recognition (81). In patients with alcoholic liver disease, alcohol and alcohol metabolites increase liver inflammation and steatosis (82). Wang et al (83) found alcohol inhibits MFGE8 gene expression and impairs efferocytosis and thus leading to hepatocyte necrosis, which explains why alcohol can cause liver damage from another perspective.
Defective efferocytosis also contributes to other liver diseases, such as fatty liver disease and primary biliary cholangitis (2). Following the phagocytosis of ACs, phagocytes increase cholesterol efflux activity to maintain lipid homeostasis. The engagement of PS receptors activates PPAR γ/δ and LXR, the regulators of cellular lipid homeostasis (37) and upregulates the phagocytic receptors, such as the TAM family, to accommodate to the increased cholesterol induced by phagocytosis (36,84). Excessive accumulation of fatty acids caused by defective efferocytosis triggers oxidative stress and lipid peroxidation, leading to liver cell death/apoptosis, inflammation, liver steatosis and even lipotoxic liver cell damage. GAS6 and Mertk can protect cultured primary mouse hepatocytes against lipid toxicity via protein kinase B (AKT)/signal transducers and activators of transcription 3 (STAT3) signaling (85). The enhanced oxidative stress response and the reactive oxygen species (ROS) expression in fatty liver tissues exacerbate non-alcoholic fatty liver disease (NAFLD) (86). Mertk can protect primary macrophages from oxidative stress-induced apoptosis (87). The significantly upregulated NLR family, pyrin domain containing 3 (NLRP3) inflammasome aggravates NAFLD greatly (88). However, a study showed that TIM4 reduced the inflammation in NAFLD by suppressing NLRP3 inflammasome (89). High-level hepatocyte apoptosis is found in non-alcoholic steatohepatitis (NASH) patients (90). The delayed removal of apoptotic liver cells can cause liver damage, inflammation and fibrosis (91). Liver fibrosis, the pathological result of various chronic liver diseases, is associated with the dysregulation and polarization of M1/M2 macrophages (92). Efferocytosis can alleviate liver fibrosis by stimulating M2 macrophage polarization (93). Rantakari et al (94) clearly showed that the absence of stabilin-1 aggravates fibrosis in chronic liver injury following CCl4 administration.
TIM4 and GAS6 are critical proteins in the resolution of hepatic ischemia-reperfusion injury (95). The administration of recombinant GAS6 can protect GAS6-knockout mice from fulminant hepatic failure (96). GAS6 also protects primary mouse hepatocytes from hypoxia-induced cell death through AKT phosphorylation and diminishes inflammatory cytokines in vitro (95). In acute and chronic liver injury, the elevated Galectin-3 expression can facilitate phagocytosis via Mertk (97). Triantafyllou et al (98) demonstrate that Mertk+ macrophage, as a novel hepatoprotective target, can promote resolution responses and quell tissue-destructive responses following acute liver injury.
Phagocytic clearance of ACs also serves a role in intestinal inflammatory disorders. In the acute phase of murine experimental colitis, MFGE8 expression decreases in inflamed colons (99). However, recombinant MFGE8 ameliorates colitis by reducing inflammation and improving disease parameters, suggesting that it may be a useful therapeutic agent for colitis (99). A number of studies indicate that the receptor tyrosine kinases Axl and Mertk can promote the resolution of inflammation, serving as a potential therapeutic target for inflammatory bowel disease (IBD) (100–102). Compared with wild-type mice, Axl−/−Mertk−/−mice and GAS6−/− mice are more sensitive to dextran sulfate sodium, presenting with more severe colitis signs and more weight loss (101,103).
Effective efferocytosis prevents apoptotic or necrotic cells from forming cell debris that can induce liver and intestine damage (81,104). Efferocytosis serves a role in liver diseases by regulating lipid metabolism, inflammation and polarization (81). Also, since efferocytosis promotes the resolution of inflammation, it can be used to treat intestinal inflammatory disorders (104).
5. Autoimmune diseases
A large number of cells undergo apoptosis during the development and homeostasis of the body (105). There are two main pathways of apoptosis, extrinsic or death receptor pathway and intrinsic or mitochondrial pathway, which have been identified (106). Patients with autoimmune diseases show high levels of apoptotic cells, partly attributed to the massive apoptosis in phagocytes or in tissue cells, such as glomerular cell, epidermal keratinocytes and T cells (107). Efficient AC clearance maintains immune homeostasis by eliminating auto-antigens, as well as producing anti-inflammatory and immunosuppressive signals (3). By contrast, under defective efferocytosis, ACs cannot be removed in time (108). As a result, uncleared ACs may rupture and release harmful contents such as autoantigens, thus promoting immune response and resulting in autoimmune diseases, such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), type 1 diabetes (T1D) and multiple sclerosis (MS) (109). Genetic evidence from mouse studies has demonstrated that failed or delayed efferocytosis might cause immune system disorders and the release of auto-antigens (110). TAM triple-knockout mice can develop autoimmune hepatitis at the age of six months, with rising transaminases and titers of autoantibodies to antinuclear antigen (111).
SLE damages multiple organs, such as the skin, joints, kidney, lungs, nervous system, heart and blood vessels (112). Autoantibodies against nuclear antigens, such as antinuclear antibodies and anti-double-stranded DNA (dsDNA), are found in SLE patients (113). Macrophages from SLE patients possess a weaker capability to engulf ACs (114). Defective clearance of ACs has been demonstrated to promote the autoantibody production in vivo (115). An analysis of 50 SLE patients indicates that GAS6/ProS-TAM system is associated with the disease activity of SLE in several ways (116). Several PS receptors and PS opsonins serve an essential role in efferocytosis, chronic inflammation and age-dependent autoimmunity. TAM triple (Mertk−/−, Axl−/−, Tyro3−/−) knockout mice develop a poly-autoimmune syndrome resembling SLE, with elevated titers of autoantibodies, uncontrolled B and T cell proliferation and lymphocyte accumulation (117). Similarly, TIM4-deficient mice, with hyperactivated T and B cells, develop autoantibodies to dsDNA, a specific antibody to SLE (118). Furthermore, knockouts of TIM-1 (119), scavenger receptor class F member 1 (SCARF1) (120) and CD300f (121) all share a common phenotype with SLE-like autoimmunity. These observations are evidenced by the defective AC clearance as an etiological cause of SLE.
The site of RA inflammation contains uncleared ACs, suggesting that RA is related to impaired efferocytosis. Waterborg et al (122) show that the deficiency of Axl and Mertk worsens arthritis in mice, whereas overexpressing their ligands ProS1 and GAS6 to activate these receptors can ameliorate arthritis. Other studies have demonstrated that activating LXR/PPAR γ exerts therapeutic effects on the mouse model with inflammatory arthritis (123–125).
T1D is a T cell-mediated autoimmune disorder with insulin deficiency and hyperglycemia (126). Inefficient clearance of apoptotic pancreatic cells may aggravate inflammation and necrosis, thus accelerating the release of autoantigens (127). Defective wound healing is a characteristic of patients with T1D. Due to incomplete phagocytosis, dead cells accumulate at the wound site, which leads to inflammation and retard wound healing (128). Das et al (129) demonstrate that MFGE8−/− mice develop systemic inflammation and MFGE8 exerts a potential therapeutic effect on diabetic wound.
Sjogren's syndrome (SS) is a chronic, progressive autoimmune disease, with dry mouth and eyes as the most frequent symptoms. The accumulation of ACs and a type I interferon signature have been observed in patients with SS and mouse models. The function of TAMs in efferocytosis and interferon response dampening is impaired in SS (130). Chen et al (131) found that decreased plasma GAS6 concentration is associated with SS and thus GAS6 may be a novel independent risk factor for SS. Similarly, another study shows that the level of Tyro3 and Axl was decreased in SS patients (132). These findings suggest that efferocytosis may be associated with disease activity or inflammation in SS.
Glucocorticoids, the most widely-used anti-inflammatory drugs, are used to treat SLE by promoting AC clearance and alleviating inflammation in an MFGE8-dependent way (133). Glucocorticoids can also upregulate Mer (134) and increase the expression of annexin A1 and lipoxin A receptors (135,136). Long-term effects of glucocorticoids are reported to be dependent on PPARγ (137).
When efferocytosis fails, ACs can rupture and release cellular materials. Then the released cellular materials stimulate inflammatory and immunogenic reactions, which are likely to trigger an autoimmune response (138). Glucocorticoids treat autoimmune diseases by promoting efferocytosis, which provides more ideas for future treatment (139).
6. Neurodegenerative disorders
Phagocytosis in the brain is accomplished by microglia, a resident macrophage in the brain and spinal cord. The central nervous system also requires efficient efferocytosis to achieve homeostasis by clearing the dying cells and preventing the spillover of proinflammatory and neurotoxic molecules (140). Defective efferocytosis may lead to multiple neurodegenerative disorders, such as Alzheimer's disease (AD), Parkinson's disease (PD) and Huntington's disease. Excessive ACs have been detected in patients with neurodegenerative diseases (141). MFGE8, an endogenous protective factor, regulates microglial phagocytosis of apoptotic neurons and inhibits inflammation (142). In the central nervous system of mice, microglial cells lacking Mertk fail to clear ineffective synaptic connections, thus impairing hippocampal development and propagating neuronal damage (143).
AD is characterized by the accumulation of hyperphosphorylated protein tau and amyloid β (Aβ) (144). Zheng et al (145) found that Aβ generation is significantly decreased by Tyro3 receptor overexpression in the cell model. A significant increase of amyloid plaques in the hippocampus and plaque-associated clusters of astroglia has been detected in a Tyro3−/− AD transgenic mouse model (145). Neuroinflammation serves a key role in AD development and progression. The expression of MFGE8, an anti-inflammatory agent, decreases in a mouse model of AD (146). Evidence suggests that MFGE8 can suppress A1 astrocytes and regulate microglia M1/M2 alteration to prevent the death of neurons and oligodendrocytes by regulating NF-κB and PI3K-AKT (147,148). Recombinant MFGE8 may have the potential to treat chronic inflammation in AD, through inhibiting MAPK and NF-κB signaling pathways (149).
PD is a progressive neurological disorder characterized by α-synuclein deposit (150). Dysregulated microglia phagocytosis has been recognized in PD and defective phagocytosis has also been observed in the monocytes of patients with PD (151). In PD models, CX3CR1−/− mice show microglial neurotoxicity (152). Studies also reveal that microglia phagocytosed and cleared cellular debris of degenerating neurons through C1q-mediated pathway and scavenger receptors (153,154). In the central nervous system, microglial phagocytic function is supported by bridging proteins (such as MFGE8 or Pro S) and TAM-receptor kinases (such as Axl and Mer) to clear PS-exposing neurons (155,156). The study of Nakashima et al (157) suggests that MFGE8 may prevent PD by reversing the reduced mesencephalic dopamine neurons. Chronic neuroinflammation is also crucial in PD. Ghahremani et al (158) conclude that efferocytosis can change the macrophage phenotype into anti-inflammatory phenotype.
In conclusion, neuronal apoptotic debris is cleared by phagocytic cells through efferocytosis. Then the release of proinflammatory and antigenic autoimmune constituents is inhibited, which enhances the neuronal survival and axonal regeneration. The tremendous therapeutic potential of efferocytosis for neurodegenerative diseases requires further preclinical development.
7. Tumors
Efferocytosis also serves an essential role in tumors. Apoptotic cell clearance can have deleterious consequences within the tumor microenvironment, potentially affecting the natural progression of the disease and cancer treatments. Efferocytosis can help generate a tumor-tolerant, immunosuppressive tumor micro-environment (159). In the tumor microenvironment, tumor-associated macrophages, which are largely polarized to the M2-like phenotype through PPAR-γ and LXR-α, exert pro-tumor effects by promoting angiogenesis, suppressing T cell infiltration and cytotoxic T cell function, remodeling extracellular matrix to promote invasion and metastasis of cancer cells and suppressing the immune system (160–162). Efferocytosis upregulates TAM receptor expression to promote macrophage polarization towards an immunosuppressive phenotype (163). Namely, the escape of malignant cells is supported by TAM-mediated efferocytosis, negative regulation of dendritic cell activity and dysregulated production of chemokines. MerTK overexpression has been found in a number of human cancers, including myeloid and lymphoblastic leukemia, melanoma and gliomas (164–166). Thus, TAM receptors on macrophages serve as exciting targets for cancer therapy by effecting macrophage phenotype and efferocytosis (167). A growing amount of evidence suggests that efferocytosis in the tumor microenvironment accelerates tumor progression, which provides new ideas for tumor treatment. For example, the blockade of PtdSer interacting with the efferocytosis of phagocytes sufficiently can inhibit tumor progression and metastasis (168). Studies demonstrate that Axl and Mer contribute to cell survival, migration, invasion, metastasis and chemosensitivity, which can be used as therapeutic targets (169–171).
Cancer cells have been found to escape from phagocytosis by upregulating ‘don't eat me’ molecules on their surface (172). Willingham et al (173) found that CD47 was highly expressed in ovarian, breast, colon, bladder, glioblastoma, hepatocellular carcinomas and prostate tumor cells; a high level of CD47 mRNA expression was associated with a decreased survival. Anti-CD47 antibodies can promote phagocytosis, inhibit tumor growth and prevent tumor metastasis. The anti-CD47 antibodies enhance cancer cell phagocytosis via inhibiting the SIRPα axis in anti-cancer therapy (174). These results suggest CD47 as a therapeutic target for solid tumors. Combing anti-CD47 antibodies and tumor-targeting therapies can achieve higher anti-cancer efficacies.
Other studies support that the enhanced efferocytosis can exert anti-tumor effects. A previous study has revealed that multiple myeloma is associated with reduced efferocytosis by monocytes (175). Some studies have demonstrated that the loss of Axl, Mertk and GAS6 can promote colon cancer (101,103). Axl, Mertk and GAS6 can limit inflammation and reduce the risk of inflammation-associated colorectal cancer (176). The above evidence suggest the double edge sword role of efferocytosis in tumor. Therefore, the specific mechanism of efferocytosis in tumor requires further clarification.
8. Discussion
Efferocytosis can maintain homeostasis in biological evolution. Efferocytosis not only serves a role in the above-mentioned diseases, but also affects other diseases, such as skin diseases, retinal degeneration and wound healing. Loss of the phagocytosis receptor Mertk causes overt retinal degeneration (177). The protein CCN1 is a critical opsonin in skin injury by acting as a bridging molecule in neutrophil efferocytosis (178). Abnormal activation of complement-mediated phagocytosis also affects retinal diseases, such as glaucoma and age-related macular degeneration (179). C1q is found to stimulate endothelial cells proliferation and migration and to promote tube formation and sprouting of new vessels (180). C1q may represent a valuable therapeutic agent for wound healing. The critical role of efferocytosis in multisystem diseases provides new directions for the prevention and treatment of these diseases. More extensive and in-depth studies are needed to clarify the pathophysiological mechanism of efferocytosis in diseases.
Traditional Chinese medicine, which features multi-components, multi-targets, multi-pathways and multi-effects, shows clear advantages in the treatment of diseases (181). Therefore, research on the role of traditional Chinese medicine in regulating efferocytosis promises a new direction of therapy development. More and more studies are being carried out on natural products for efferocytosis regulation.
Our previous studies (182–184) demonstrate the key role of efferocytosis in the development of atherosclerosis and the regulatory effect of efferocytosis on atherosclerosis. Guan Xin Kang (GXK), a formula designed by our research group and composed of Astragalus, Salvia, Leonurus, Trichosanthes kirilowii, Pinellia ternate and Scallions white, can improve the pathological changes in thoracic aorta, increase the phagocytosis rate of splenic macrophages and upregulate the protein expression of thrombospondin 1 (182) and TAM receptors (Tyro3/Axl/Mertk) in LDLR−/− mouse (184). The expression of Mertk protein in RAW264.7 cells can be upregulated by sera medicated with GXK (183). The above results indicate that efferocytosis regulation may be effective in treating atherosclerosis. Treatment with catechins in rats can result in anti-atherogenic properties (185). Kaempferol, luteolin, ellagic acid and berberine can upregulate SR-BI expression and further inhibit ox-LDL uptake in macrophages (186–189). Caffeic acid and ferulic acid possess anti-atherogenic properties by enhancing HDL-mediated cholesterol efflux from the macrophages (190). These natural products, which have been proved to inhibit foam cell formation via efferocytosis (191), are potential drugs to improve cardiovascular diseases.
There are also several natural products that can regulate macrophage activation, recruitment and polarization to reduce inflammation, attenuate lipid accumulation and improve insulin sensitivity in NASH treatment, such as sparstolonin B (192), berberine (193) and celastrol (194). Baicalin promotes macrophage polarization to the M2-type in mice with IBD by enhancing the phagocytosis and efferocytosis of macrophages (195,196). Polysaccharides from Ganoderma lucidum modulate microglial phagocytosis to attenuate neuroinflammation (197). An increasing number of natural products, such as pycnogenol (198), polysaccharides from the roots of Sanguisorba officinalis (199) and tea polysaccharides (200), enhance the phagocytic function of macrophages and could be used to treat diseases.
Having fewer adverse effects and multi-target properties, natural products are prospective medicinal components for the treatment of multi-system diseases in the future. Therefore, more research is needed to explore the mechanism of Chinese medicine that can regulate efferocytosis and provide reliable basis for disease treatment.
Acknowledgements
Not applicable.
Glossary
Abbreviations
- ACs
apoptotic cells
- AD
Alzheimer's disease
- AKT
protein kinase B
- ALI
acute lung injury
- AMPK
AMP-activated protein kinase
- ARDS
acute respiratory distress syndrome
- ATP
adenosine triphosphate
- Aβ
amyloid β protein
- CF
cystic fibrosis
- COPD
chronic obstructive pulmonary disease
- CX3CL1
CX3C chemokine ligand 1
- CX3CR1
CX3C chemokine receptor 1
- dsDNA
anti-double-stranded DNA
- ERK5
extracellular signal-regulated kinase 5
- GAS6
growth arrest specific protein 6
- GXK
Guan Xinkang
- HMGB1
high mobility group box-1
- IBD
inflammatory bowel disease
- LPC
lyso-phosphatidylcholine
- LRP1
low-density lipoprotein receptor related proteins 1
- LXR
liver X receptor
- Mertk
Mer tyrosine protein kinase receptor
- MFGE8
milk fat globule-epidermal growth factor 8
- MI
myocardial infarction
- NAFLD
non-alcoholic fatty liver disease
- NASH
non-alcoholic steatohepatitis
- NLRP3
NLR family, pyrin domain containing 3
- PD
Parkinson's disease
- PPAR
peroxisome proliferator receptor
- ProS
Protein S
- PtdSer
phosphatidylserine
- RA
rheumatoid arthritis
- ROS
reactive oxygen species
- SCARF1
scavenger receptor class F member 1
- SLE
systemic lupus erythematosus
- SRB1
scavenger receptor 1
- SS
Sjogren's syndrome
- T1D
type 1 diabetes
- TAM
TYRO3/Axl/MER tyrosine kinase receptor
- TIM
T-cell immunoglobulin and mucin domain-containing molecule
Funding Statement
The present review was supported by the Natural Science Foundation of China (grant nos. 81873117).
Availability of data and materials
Data sharing is not applicable to this article, as no data sets were generated or analyzed during the current study.
Authors' contributions
YZ conceptualized the review, performed the literature search and drafted the manuscript. YW and JD helped to draft and revise the manuscript. PL edited and revised the paper. All authors have read and approved the final version of the manuscript to be published.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Thorp E, Tabas I. Mechanisms and consequences of efferocytosis in advanced atherosclerosis. J Leukoc Biol. 2009;86:1089–1095. doi: 10.1189/jlb.0209115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boada-Romero E, Martinez J, Heckmann BL, Green DR. The clearance of dead cells by efferocytosis. Nat Rev Mol Cell Biol. 2020;21:398–414. doi: 10.1038/s41580-020-0232-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trahtemberg U, Mevorach D. Apoptotic cells induced signaling for immune homeostasis in macrophages and dendritic cells. Front Immunol. 2017;8:1356. doi: 10.3389/fimmu.2017.01356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Segawa K, Nagata S. An apoptotic ‘Eat Me’ Signal: Phosphatidylserine exposure. Trends Cell Biol. 2015;25:639–650. doi: 10.1016/j.tcb.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Kourtzelis I, Hajishengallis G, Chavakis T. Phagocytosis of apoptotic cells in resolution of inflammation. Front Immunol. 2020;11:553. doi: 10.3389/fimmu.2020.00553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freeman SA, Grinstein S. Phagocytosis: Receptors, signal integration and the cytoskeleton. Immunol Rev. 2014;262:193–215. doi: 10.1111/imr.12212. [DOI] [PubMed] [Google Scholar]
- 7.Doran AC, Yurdagul A, Jr, Tabas I. Efferocytosis in health and disease. Nat Rev Immunol. 2020;20:254–267. doi: 10.1038/s41577-019-0240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levin R, Grinstein S, Canton J. The life cycle of phagosomes: Formation, maturation and resolution. Immunol Rev. 2016;273:156–179. doi: 10.1111/imr.12439. [DOI] [PubMed] [Google Scholar]
- 9.Elliott MR, Chekeni FB, Trampont PC, Lazarowski ER, Kadl A, Walk SF, Park D, Woodson RI, Ostankovich M, Sharma P, et al. Nucleotides released by apoptotic cells act as a find-me signal to promote phagocytic clearance. Nature. 2009;461:282–286. doi: 10.1038/nature08296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lauber K, Bohn E, Krober SM, Xiao YJ, Blumenthal SG, Lindemann RK, Marini P, Wiedig C, Zobywalski A, Baksh S, et al. Apoptotic cells induce migration of phagocytes via caspase-3-mediated release of a lipid attraction signal. Cell. 2003;113:717–730. doi: 10.1016/S0092-8674(03)00422-7. [DOI] [PubMed] [Google Scholar]
- 11.Gude DR, Alvarez SE, Paugh SW, Mitra P, Yu J, Griffiths R, Barbour SE, Milstien S, Spiegel S. Apoptosis induces expression of sphingosine kinase 1 to release sphingosine-1-phosphate as a ‘come-and-get-me’ signal. FASEB J. 2008;22:2629–2638. doi: 10.1096/fj.08-107169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Truman LA, Ford CA, Pasikowska M, Pound JD, Wilkinson SJ, Dumitriu IE, Melville L, Melrose LA, Ogden CA, Nibbs R, et al. CX3CL1/fractalkine is released from apoptotic lymphocytes to stimulate macrophage chemotaxis. Blood. 2008;112:5026–5036. doi: 10.1182/blood-2008-06-162404. [DOI] [PubMed] [Google Scholar]
- 13.Peter C, Waibel M, Radu CG, Yang LV, Witte ON, Schulze-Osthoff K, Wesselborg S, Lauber K. Migration to apoptotic ‘find-me’ signals is mediated via the phagocyte receptor G2A. J Biol Chem. 2008;283:5296–5305. doi: 10.1074/jbc.M706586200. [DOI] [PubMed] [Google Scholar]
- 14.Gardai SJ, McPhillips KA, Frasch SC, Janssen WJ, Starefeldt A, Murphy-Ullrich JE, Bratton DL, Oldenborg PA, Michalak M, Henson PM. Cell-surface calreticulin initiates clearance of viable or apoptotic cells through trans-activation of LRP on the phagocyte. Cell. 2005;123:321–334. doi: 10.1016/j.cell.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 15.Appelt U, Sheriff A, Gaipl US, Kalden JR, Voll RE, Herrmann M. Viable, apoptotic and necrotic monocytes expose phosphatidylserine: Cooperative binding of the ligand Annexin V to dying but not viable cells and implications for PS-dependent clearance. Cell Death Differ. 2005;12:194–196. doi: 10.1038/sj.cdd.4401527. [DOI] [PubMed] [Google Scholar]
- 16.Nagata S, Hanayama R, Kawane K. Autoimmunity and the clearance of dead cells. Cell. 2010;140:619–630. doi: 10.1016/j.cell.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 17.Geng K, Kumar S, Kimani SG, Kholodovych V, Kasikara C, Mizuno K, Sandiford O, Rameshwar P, Kotenko SV, Birge RB. Requirement of gamma-carboxyglutamic acid modification and phosphatidylserine binding for the activation of Tyro3, Axl and Mertk receptors by growth arrest-specific 6. Front Immunol. 2017;8:1521. doi: 10.3389/fimmu.2017.01521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ravichandran KS. Find-me and eat-me signals in apoptotic cell clearance: Progress and conundrums. J Exp Med. 2010;207:1807–1817. doi: 10.1084/jem.20101157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tajbakhsh A, Rezaee M, Kovanen PT, Sahebkar A. Efferocytosis in atherosclerotic lesions: Malfunctioning regulatory pathways and control mechanisms. Pharmacol Ther. 2018;188:12–25. doi: 10.1016/j.pharmthera.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Yoon KW. Dead cell phagocytosis and innate immune checkpoint. BMB Rep. 2017;50:496–503. doi: 10.5483/BMBRep.2017.50.10.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tajbakhsh A, Farahani N, Gheibihayat SM, Mirkhabbaz AM, Savardashtaki A, Hamblin MR, Mirzaei H. Autoantigen-specific immune tolerance in pathological and physiological cell death: Nanotechnology comes into view. Int Immunopharmacol. 2021;90:107177. doi: 10.1016/j.intimp.2020.107177. [DOI] [PubMed] [Google Scholar]
- 22.Helgadottir A, Thorleifsson G, Manolescu A, Gretarsdottir S, Blondal T, Jonasdottir A, Jonasdottir A, Sigurdsson A, Baker A, Palsson A, et al. A common variant on chromosome 9p21 affects the risk of myocardial infarction. Science. 2007;316:1491–1493. doi: 10.1126/science.1142842. [DOI] [PubMed] [Google Scholar]
- 23.Smith JG, Melander O, Lövkvist H, Hedblad B, Engström G, Nilsson P, Carlson J, Berglund G, Norrving B, Lindgren A. Common genetic variants on chromosome 9p21 confers risk of ischemic stroke: A large-scale genetic association study. Circ Cardiovasc Genet. 2009;2:159–164. doi: 10.1161/CIRCGENETICS.108.835173. [DOI] [PubMed] [Google Scholar]
- 24.Kojima Y, Downing K, Kundu R, Miller C, Dewey F, Lancero H, Raaz U, Perisic L, Hedin U, Schadt E, et al. Cyclin-dependent kinase inhibitor 2B regulates efferocytosis and atherosclerosis. J Clin Invest. 2019;129:2164. doi: 10.1172/JCI129277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leeper NJ, Raiesdana A, Kojima Y, Kundu RK, Cheng H, Maegdefessel L, Toh R, Ahn GO, Ali ZA, Anderson DR, et al. Loss of CDKN2B promotes p53-dependent smooth muscle cell apoptosis and aneurysm formation. Arterioscler Thromb Vasc Biol. 2013;33:e1–e10. doi: 10.1161/ATVBAHA.112.300399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martinho-Dias D, Leite-Moreira A, Castro-Chaves P. Calreticulin in the heart: From embryological development to cardiac pathology. Curr Mol Med. 2016;16:12–22. doi: 10.2174/1566524016666151222142816. [DOI] [PubMed] [Google Scholar]
- 27.Cunnington MS, Keavney B. Genetic mechanisms mediating atherosclerosis susceptibility at the chromosome 9p21 locus. Curr Atheroscler Rep. 2011;13:193–201. doi: 10.1007/s11883-011-0178-z. [DOI] [PubMed] [Google Scholar]
- 28.Bäck M, Yurdagul A, Jr, Tabas I, Öörni K, Kovanen PT. Inflammation and its resolution in atherosclerosis: mediators and therapeutic opportunities. Nat Rev Cardiol. 2019;6:389–406. doi: 10.1038/s41569-019-0169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, Abela GS, Franchi L, Nuñez G, Schnurr M, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464:1357–1361. doi: 10.1038/nature08938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tabas I, Bornfeldt KE. Macrophage phenotype and function in different stages of atherosclerosis. Circ Res. 2016;118:653–667. doi: 10.1161/CIRCRESAHA.115.306256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 32.Tabas I. Macrophage death and defective inflammation resolution in atherosclerosis. Nat Rev Immunol. 2010;10:36–46. doi: 10.1038/nri2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kojima Y, Volkmer JP, McKenna K, Civelek M, Lusis AJ, Miller CL, Direnzo D, Nanda V, Ye J, Connolly AJ, et al. CD47-blocking antibodies restore phagocytosis and prevent atherosclerosis. Nature. 2016;536:86–90. doi: 10.1038/nature18935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martinet W, Schrijvers DM, De Meyer GR. Necrotic cell death in atherosclerosis. Basic Res Cardiol. 2011;106:749–760. doi: 10.1007/s00395-011-0192-x. [DOI] [PubMed] [Google Scholar]
- 35.Tabas I. 2016 Russell Ross memorial lecture in vascular biology: Molecular-cellular mechanisms in the progression of atherosclerosis. Arterioscler Thromb Vasc Biol. 2017;37:183–189. doi: 10.1161/ATVBAHA.116.308036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Han CZ, Ravichandran KS. Metabolic connections during apoptotic cell engulfment. Cell. 2011;147:1442–1445. doi: 10.1016/j.cell.2011.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.A-Gonzalez N, Bensinger SJ, Hong C, Beceiro S, Bradley MN, Zelcer N, Deniz J, Ramirez C, Díaz M, Gallardo G, et al. Apoptotic cells promote their own clearance and immune tolerance through activation of the nuclear receptor LXR. Immunity. 2009;31:245–258. doi: 10.1016/j.immuni.2009.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mukundan L, Odegaard JI, Morel CR, Heredia JE, Mwangi JW, Ricardo-Gonzalez RR, Goh YP, Eagle AR, Dunn SE, Awakuni JU, et al. PPAR-delta senses and orchestrates clearance of apoptotic cells to promote tolerance. Nat Med. 2009;15:1266–1272. doi: 10.1038/nm.2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Festuccia WT, Pouliot P, Bakan I, Sabatini DM, Laplante M. Myeloid-specific Rictor deletion induces M1 macrophage polarization and potentiates in vivo pro-inflammatory response to lipopolysaccharide. PLoS One. 2014;9:e95432. doi: 10.1371/journal.pone.0095432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schrijvers DM, De Meyer GR, Kockx MM, Herman AG, Martinet W. Phagocytosis of apoptotic cells by macrophages is impaired in atherosclerosis. Arterioscler Thromb Vasc Biol. 2005;25:1256–1261. doi: 10.1161/01.ATV.0000166517.18801.a7. [DOI] [PubMed] [Google Scholar]
- 41.Yurdagul A, Jr, Subramanian M, Wang X, Crown SB, Ilkayeva OR, Darville L, Kolluru GK, Rymond CC, Gerlach BD, Zheng Z, et al. Macrophage metabolism of apoptotic cell-derived arginine promotes continual efferocytosis and resolution of injury. Cell Metab. 2020;31:518–533.e10. doi: 10.1016/j.cmet.2020.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kimani SG, Geng K, Kasikara C, Kumar S, Sriram G, Wu Y, Birge RB. Contribution of defective PS recognition and efferocytosis to chronic inflammation and autoimmunity. Front Immunol. 2014;5:566. doi: 10.3389/fimmu.2014.00566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cai B, Thorp EB, Doran AC, Sansbury BE, Daemen MJ, Dorweiler B, Spite M, Fredman G, Tabas I. MerTK receptor cleavage promotes plaque necrosis and defective resolution in atherosclerosis. J Clin Invest. 2017;127:564–568. doi: 10.1172/JCI90520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ait-Oufella H, Kinugawa K, Zoll J, Simon T, Boddaert J, Heeneman S, Blanc-Brude O, Barateau V, Potteaux S, Merval R, et al. Lactadherin deficiency leads to apoptotic cell accumulation and accelerated atherosclerosis in mice. Circulation. 2007;115:2168–2177. doi: 10.1161/CIRCULATIONAHA.106.662080. [DOI] [PubMed] [Google Scholar]
- 45.Schrijvers DM, De Meyer GR, Herman AG, Martinet W. Phagocytosis in atherosclerosis: Molecular mechanisms and implications for plaque progression and stability. Cardiovasc Res. 2007;73:470–480. doi: 10.1016/j.cardiores.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 46.Virmani R, Burke AP, Kolodgie FD, Farb A. Vulnerable plaque: The pathology of unstable coronary lesions. J Interv Cardiol. 2002;15:439–446. doi: 10.1111/j.1540-8183.2002.tb01087.x. [DOI] [PubMed] [Google Scholar]
- 47.Pulanco MC, Cosman J, Ho MM, Huynh J, Fing K, Turcu J, Fraser DA. Complement protein C1q enhances macrophage foam cell survival and efferocytosis. J Immunol. 2017;198:472–480. doi: 10.4049/jimmunol.1601445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marsch E, Theelen TL, Demandt JA, Jeurissen M, van Gink M, Verjans R, Janssen A, Cleutjens JP, Meex SJ, Donners MM, et al. Reversal of hypoxia in murine atherosclerosis prevents necrotic core expansion by enhancing efferocytosis. Arterioscler Thromb Vasc Biol. 2014;34:2545–2553. doi: 10.1161/ATVBAHA.114.304023. [DOI] [PubMed] [Google Scholar]
- 49.Gui Y, Yao S, Yan H, Hu L, Yu C, Gao F, Xi C, Li H, Ye Y, Wang Y. A novel small molecule liver X receptor transcriptional regulator, nagilactone B, suppresses atherosclerosis in apoE-deficient mice. Cardiovasc Res. 2016;112:502–514. doi: 10.1093/cvr/cvw183. [DOI] [PubMed] [Google Scholar]
- 50.Salman H, Bergman M, Djaldetti M, Bessler H. Hydrophobic but not hydrophilic statins enhance phagocytosis and decrease apoptosis of human peripheral blood cells in vitro. Biomed Pharmacother. 2008;62:41–45. doi: 10.1016/j.biopha.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 51.Ivanova EA, Myasoedova VA, Melnichenko AA, Orekhov AN. Peroxisome proliferator-activated receptor (PPAR) gamma agonists as therapeutic agents for cardiovascular disorders: Focus on atherosclerosis. Curr Pharm Des. 2017;23:1119–1124. doi: 10.2174/1381612823666161118145850. [DOI] [PubMed] [Google Scholar]
- 52.Heo KS, Cushman HJ, Akaike M, Woo CH, Wang X, Qiu X, Fujiwara K, Abe J. ERK5 activation in macrophages promotes efferocytosis and inhibits atherosclerosis. Circulation. 2014;130:180–191. doi: 10.1161/CIRCULATIONAHA.113.005991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang J, Liu P. Effects of ERK5 inhibitors on macrophages efferocytosis and the expression of ProS and Axl. Journal of Jinan University (Natural Science & Medicine Edition) 2018;39:93–98. (In Chinese) [Google Scholar]
- 54.Wan E, Yeap XY, Dehn S, Terry R, Novak M, Zhang S, Iwata S, Han X, Homma S, Drosatos K, et al. Enhanced efferocytosis of apoptotic cardiomyocytes through myeloid-epithelial-reproductive tyrosine kinase links acute inflammation resolution to cardiac repair after infarction. Circ Res. 2013;113:1004–1012. doi: 10.1161/CIRCRESAHA.113.301198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fox S, Leitch AE, Duffin R, Haslett C, Rossi AG. Neutrophil apoptosis: Relevance to the innate immune response and inflammatory disease. J Innate Immun. 2010;2:216–227. doi: 10.1159/000284367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hodge S, Tran HB, Hamon R, Roscioli E, Hodge G, Jersmann H, Ween M, Reynolds PN, Yeung A, Treiberg J, Wilbert S. Nonantibiotic macrolides restore airway macrophage phagocytic function with potential anti-inflammatory effects in chronic lung diseases. Am J Physiol Lung Cell Mol Physiol. 2017;312:L678–Ll687. doi: 10.1152/ajplung.00518.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee YJ, Lee SH, Youn YS, Choi JY, Song KS, Cho MS, Kang JL. Preventing cleavage of Mer promotes efferocytosis and suppresses acute lung injury in bleomycin treated mice. Toxicol Appl Pharmacol. 2012;263:61–72. doi: 10.1016/j.taap.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 58.McCubbrey AL, Curtis JL. Efferocytosis and lung disease. Chest. 2013;143:1750–1757. doi: 10.1378/chest.12-2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lareau SC, Fahy B, Meek P, Wang A. Chronic obstructive pulmonary disease (COPD) Am J Respir Crit Care Med. 2019;199:P1–P2. doi: 10.1164/rccm.1991P1. [DOI] [PubMed] [Google Scholar]
- 60.Noda N, Matsumoto K, Fukuyama S, Asai Y, Kitajima H, Seki N, Matsunaga Y, Kan-O K, Moriwaki A, Morimoto K, et al. Cigarette smoke impairs phagocytosis of apoptotic neutrophils by alveolar macrophages via inhibition of the histone deacetylase/Rac/CD9 pathways. Int Immunol. 2013;25:643–650. doi: 10.1093/intimm/dxt033. [DOI] [PubMed] [Google Scholar]
- 61.Krysko O, Vandenabeele P, Krysko DV, Bachert C. Impairment of phagocytosis of apoptotic cells and its role in chronic airway diseases. Apoptosis. 2010;15:1137–1146. doi: 10.1007/s10495-010-0504-x. [DOI] [PubMed] [Google Scholar]
- 62.Simpson JL, Gibson PG, Yang IA, Upham J, James A, Reynolds PN, Hodge S, AMAZES Study Research Group Impaired macrophage phagocytosis in non-eosinophilic asthma. Clin Exp Allergy. 2013;43:29–35. doi: 10.1111/j.1365-2222.2012.04075.x. [DOI] [PubMed] [Google Scholar]
- 63.Stanton BF. Cystic fibrosis. Pediatr Clin North Am. 2016;63:xv. doi: 10.1016/j.pcl.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 64.Vandivier RW, Fadok VA, Ogden CA, Hoffmann PR, Brain JD, Accurso FJ, Fisher JH, Greene KE, Henson PM. Impaired clearance of apoptotic cells from cystic fibrosis airways. Chest. 2002;121((Suppl 3)):S89. doi: 10.1378/chest.121.3_suppl.89S. [DOI] [PubMed] [Google Scholar]
- 65.Mishra V, Banga J, Silveyra P. Oxidative stress and cellular pathways of asthma and inflammation: Therapeutic strategies and pharmacological targets. Pharmacol Ther. 2018;181:169–182. doi: 10.1016/j.pharmthera.2017.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Felton JM, Lucas CD, Dorward DA, Duffin R, Kipari T, Vermeren S, Robb CT, MacLeod KG, Serrels B, Schwarze J, et al. Mer-mediated eosinophil efferocytosis regulates resolution of allergic airway inflammation. J Allergy Clin Immunol. 2018;142:1884–1893.e6. doi: 10.1016/j.jaci.2018.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Freeman GJ, Casasnovas JM, Umetsu DT, DeKruyff RH. TIM genes: A family of cell surface phosphatidylserine receptors that regulate innate and adaptive immunity. Immunol Rev. 2010;235:172–189. doi: 10.1111/j.0105-2896.2010.00903.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grabiec AM, Denny N, Doherty JA, Happonen KE, Hankinson J, Connolly E, Fife ME, Fujimori T, Fujino N, Goenka A, et al. Diminished airway macrophage expression of the Axl receptor tyrosine kinase is associated with defective efferocytosis in asthma. J Allergy Clin Immunol. 2017;140:1144–1146.e4. doi: 10.1016/j.jaci.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 69.Aziz M, Matsuda A, Yang WL, Jacob A, Wang P. Milk fat globule-epidermal growth factor-factor 8 attenuates neutrophil infiltration in acute lung injury via modulation of CXCR2. J Immunol. 2012;189:393–402. doi: 10.4049/jimmunol.1200262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Choi JY, Park HJ, Lee YJ, Byun J, Youn YS, Choi JH, Woo SY, Kang JL. Upregulation of Mer receptor tyrosine kinase signaling attenuated lipopolysaccharide-induced lung inflammation. J Pharmacol Exp Ther. 2013;344:447–458. doi: 10.1124/jpet.112.199778. [DOI] [PubMed] [Google Scholar]
- 71.Hodge S, Hodge G, Jersmann H, Matthews G, Ahern J, Holmes M, Reynolds PN. Azithromycin improves macrophage phagocytic function and expression of mannose receptor in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2008;178:139–148. doi: 10.1164/rccm.200711-1666OC. [DOI] [PubMed] [Google Scholar]
- 72.Yamaryo T, Oishi K, Yoshimine H, Tsuchihashi Y, Matsushima K, Nagatake T. Fourteen-member macrolides promote the phosphatidylserine receptor-dependent phagocytosis of apoptotic neutrophils by alveolar macrophages. Antimicrob Agents Chemother. 2003;47:48–53. doi: 10.1128/AAC.47.1.48-53.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hodge S, Hodge G, Brozyna S, Jersmann H, Holmes M, Reynolds PN. Azithromycin increases phagocytosis of apoptotic bronchial epithelial cells by alveolar macrophages. Eur Respir J. 2006;28:486–495. doi: 10.1183/09031936.06.00001506. [DOI] [PubMed] [Google Scholar]
- 74.Xiong Z, Leme AS, Ray P, Shapiro SD, Lee JS. CX3CR1+ lung mononuclear phagocytes spatially confined to the interstitium produce TNF-α and IL-6 and promote cigarette smoke-induced emphysema. J Immunol. 2011;186:3206–3214. doi: 10.4049/jimmunol.1003221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.McColl A, Bournazos S, Franz S, Perretti M, Morgan BP, Haslett C, Dransfield I. Glucocorticoids induce protein S-dependent phagocytosis of apoptotic neutrophils by human macrophages. J Immunol. 2009;183:2167–2175. doi: 10.4049/jimmunol.0803503. [DOI] [PubMed] [Google Scholar]
- 76.Zizzo G, Hilliard BA, Monestier M, Cohen PL. Efficient clearance of early apoptotic cells by human macrophages requires M2c polarization and MerTK induction. J Immunol. 2012;189:3508–3520. doi: 10.4049/jimmunol.1200662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Grégoire M, Uhel F, Lesouhaitier M, Gacouin A, Guirriec M, Mourcin F, Dumontet E, Chalin A, Samson M, Berthelot LL, et al. Impaired efferocytosis and neutrophil extracellular trap clearance by macrophages in ARDS. Eur Respir J. 2018;52:1702590. doi: 10.1183/13993003.02590-2017. [DOI] [PubMed] [Google Scholar]
- 78.Grabiec AM, Hussell T. The role of airway macrophages in apoptotic cell clearance following acute and chronic lung inflammation. Semin Immunopathol. 2016;38:409–423. doi: 10.1007/s00281-016-0555-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Krenkel O, Tacke F. Liver macrophages in tissue homeostasis and disease. Nat Rev Immunol. 2017;17:306–321. doi: 10.1038/nri.2017.11. [DOI] [PubMed] [Google Scholar]
- 80.Bukong TN, Cho Y, Iracheta-Vellve A, Saha B, Lowe P, Adejumo A, Furi I, Ambade A, Gyongyosi B, Catalano D, et al. Abnormal neutrophil traps and impaired efferocytosis contribute to liver injury and sepsis severity after binge alcohol use. J Hepatol. 2018;69:1145–1154. doi: 10.1016/j.jhep.2018.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Horst AK, Tiegs G, Diehl L. Contribution of macrophage efferocytosis to liver homeostasis and disease. Front Immunol. 2019;10:2670. doi: 10.3389/fimmu.2019.02670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rocco A, Compare D, Angrisani D, Sanduzzi Zamparelli M, Nardone G. Alcoholic disease: Liver and beyond. World J Gastroenterol. 2014;20:14652–14659. doi: 10.3748/wjg.v20.i40.14652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang X, Bu HF, Zhong W, Asai A, Zhou Z, Tan XD. MFG-E8 and HMGB1 are involved in the mechanism underlying alcohol-induced impairment of macrophage efferocytosis. Mol Med. 2013;19:170–182. doi: 10.2119/molmed.2012.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Roszer T, Menendez-Gutierrez MP, Lefterova MI, Alameda D, Núñez V, Lazar MA, Fischer T, Ricote M. Autoimmune kidney disease and impaired engulfment of apoptotic cells in mice with macrophage peroxisome proliferator-activated receptor gamma or retinoid X receptor alpha deficiency. J Immunol. 2011;186:621–631. doi: 10.4049/jimmunol.1002230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tutusaus A, de Gregorio E, Cucarull B, Cristóbal H, Aresté C, Graupera I, Coll M, Colell A, Gausdal G, Lorens JB, et al. A functional role of GAS6/TAM in nonalcoholic steatohepatitis progression implicates AXL as therapeutic target. Cell Mol Gastroenterol Hepatol. 2020;9:349–368. doi: 10.1016/j.jcmgh.2019.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ashraf NU, Sheikh TA. Endoplasmic reticulum stress and Oxidative stress in the pathogenesis of Non-alcoholic fatty liver disease. Free Radic Res. 2015;49:1405–1418. doi: 10.3109/10715762.2015.1078461. [DOI] [PubMed] [Google Scholar]
- 87.Anwar A, Keating AK, Joung D, Sather S, Kim GK, Sawczyn KK, Brandão L, Henson PM, Graham DK. Mer tyrosine kinase (MerTK) promotes macrophage survival following exposure to oxidative stress. J Leukoc Biol. 2009;86:73–79. doi: 10.1189/jlb.0608334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mridha AR, Wree A, Robertson AAB, Yeh MM, Johnson CD, Van Rooyen DM, Haczeyni F, Teoh NC, Savard C, Ioannou GN, et al. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J Hepatol. 2017;66:1037–1046. doi: 10.1016/j.jhep.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liu W, Bai F, Wang H, Liang Y, Du X, Liu C, Cai D, Peng J, Zhong G, Liang X, et al. Tim-4 inhibits NLRP3 inflammasome via the LKB1/AMPKα pathway in macrophages. J Immunol. 2019;203:990–1000. doi: 10.4049/jimmunol.1900117. [DOI] [PubMed] [Google Scholar]
- 90.El Bassat H, Ziada DH, Hasby EA, Nagy H, Abo Ryia MH. Apoptotic and anti-apoptotic seromarkers for assessment of disease severity of non-alcoholic steatohepatitis. Arab J Gastroenterol. 2014;15:6–11. doi: 10.1016/j.ajg.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 91.de Alwis NM, Day CP. Non-alcoholic fatty liver disease: The mist gradually clears. J Hepatol. 2008;48((Suppl 1)):S104–S112. doi: 10.1016/j.jhep.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 92.Yao Q, Li S, Li X, Wang F, Tu C. Myricetin modulates macrophage polarization and mitigates liver inflammation and fibrosis in a murine model of nonalcoholic steatohepatitis. Front Med (Lausanne) 2020;7:71. doi: 10.3389/fmed.2020.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yang M, Liu J, Piao C, Shao J, Du J. ICAM-1 suppresses tumor metastasis by inhibiting macrophage M2 polarization through blockade of efferocytosis. Cell Death Dis. 2015;6:e1780. doi: 10.1038/cddis.2015.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rantakari P, Patten DA, Valtonen J, Karikoski M, Gerke H, Dawes H, Laurila J, Ohlmeier S, Elima K, Hübscher SG, et al. Stabilin-1 expression defines a subset of macrophages that mediate tissue homeostasis and prevent fibrosis in chronic liver injury. Proc Natl Acad Sci USA. 2016;113:9298–9303. doi: 10.1073/pnas.1604780113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Llacuna L, Bárcena C, Bellido-Martín L, Fernández L, Stefanovic M, Marí M, García-Ruiz C, Fernández-Checa JC, García de Frutos P, Morales A. Growth arrest-specific protein 6 is hepatoprotective against murine ischemia/reperfusion injury. Hepatology. 2010;52:1371–1379. doi: 10.1002/hep.23833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lafdil F, Chobert MN, Deveaux V, Zafrani ES, Mavier P, Nakano T, Laperche Y, Brouillet A. Growth arrest-specific protein 6 deficiency impairs liver tissue repair after acute toxic hepatitis in mice. J Hepatol. 2009;51:55–66. doi: 10.1016/j.jhep.2009.02.030. [DOI] [PubMed] [Google Scholar]
- 97.Caberoy NB, Alvarado G, Bigcas JL, Li W. Galectin-3 is a new MerTK-specific eat-me signal. J Cell Physiol. 2012;227:401–407. doi: 10.1002/jcp.22955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Triantafyllou E, Pop OT, Possamai LA, Wilhelm A, Liaskou E, Singanayagam A, Bernsmeier C, Khamri W, Petts G, Dargue R, et al. MerTK expressing hepatic macrophages promote the resolution of inflammation in acute liver failure. Gut. 2018;67:333–347. doi: 10.1136/gutjnl-2016-313615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Otani A, Ishihara S, Aziz MM, Oshima N, Mishima Y, Moriyama I, Yuki T, Amano Y, Ansary MM, Kinoshita Y. Intrarectal administration of milk fat globule epidermal growth factor-8 protein ameliorates murine experimental colitis. Int J Mol Med. 2012;29:349–356. doi: 10.3892/ijmm.2011.866. [DOI] [PubMed] [Google Scholar]
- 100.Rothlin CV, Leighton JA, Ghosh S. Tyro3, Axl and Mertk receptor signaling in inflammatory bowel disease and colitis-associated cancer. Inflamm Bowel Dis. 2014;20:1472–1480. doi: 10.1097/MIB.0000000000000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bosurgi L, Bernink JH, Delgado Cuevas V, Gagliani N, Joannas L, Schmid ET, Booth CJ, Ghosh S, Rothlin CV. Paradoxical role of the proto-oncogene Axl and Mer receptor tyrosine kinases in colon cancer. Proc Natl Acad Sci USA. 2013;110:13091–13096. doi: 10.1073/pnas.1302507110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Steiner CA, Rodansky ES, Johnson LA, Berinstein JA, Cushing KC, Huang S, Spence JR, Higgins PDR. AXL is a potential target for the treatment of intestinal fibrosis. Inflamm Bowel Dis. 2021;27:303–316. doi: 10.1093/ibd/izaa169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Akitake-Kawano R, Seno H, Nakatsuji M, Kimura Y, Nakanishi Y, Yoshioka T, Kanda K, Kawada M, Kawada K, Sakai Y, Chiba T. Inhibitory role of Gas6 in intestinal tumorigenesis. Carcinogenesis. 2013;34:1567–1574. doi: 10.1093/carcin/bgt069. [DOI] [PubMed] [Google Scholar]
- 104.Shankman LS, Fleury ST, Evans WB, Penberthy KK, Arandjelovic S, Blumberg RS, Agaisse H, Ravichandran KS. Efferocytosis by Paneth cells within the intestine. Curr Biol. 2021;31:2469–2476.e5. doi: 10.1016/j.cub.2021.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fuchs Y, Steller H. Programmed cell death in animal development and disease. Cell. 2011;147:742–758. doi: 10.1016/j.cell.2011.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Biermann M, Maueröder C, Brauner JM, Chaurio R, Janko C, Herrmann M, Muñoz LE. Surface code-biophysical signals for apoptotic cell clearance. Phys Biol. 2013;10:065007. doi: 10.1088/1478-3975/10/6/065007. [DOI] [PubMed] [Google Scholar]
- 107.Yang F, He Y, Zhai Z, Sun E. Programmed cell death pathways in the pathogenesis of systemic lupus erythematosus. J Immunol Res. 2019;2019:3638562. doi: 10.1155/2019/3638562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tajbakhsh A, Rezaee M, Barreto GE, Moallem SA, Henney NC, Sahebkar A. The role of nuclear factors as ‘Find-Me’/alarmin signals and immunostimulation in defective efferocytosis and related disorders. Int Immunopharmacol. 2020;80:106134. doi: 10.1016/j.intimp.2019.106134. [DOI] [PubMed] [Google Scholar]
- 109.Silva MT, do Vale A, dos Santos NM. Secondary necrosis in multicellular animals: An outcome of apoptosis with pathogenic implications. Apoptosis. 2008;13:463–482. doi: 10.1007/s10495-008-0187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Muñoz LE, Lauber K, Schiller M, Manfredi AA, Herrmann M. The role of defective clearance of apoptotic cells in systemic autoimmunity. Nat Rev Rheumatol. 2010;6:280–289. doi: 10.1038/nrrheum.2010.46. [DOI] [PubMed] [Google Scholar]
- 111.Qi N, Liu P, Zhang Y, Wu H, Chen Y, Han D. Development of a spontaneous liver disease resembling autoimmune hepatitis in mice lacking tyro3, axl and mer receptor tyrosine kinases. PLoS One. 2013;8:e66604. doi: 10.1371/journal.pone.0066604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mills JA. Systemic lupus erythematosus. N Engl J Med. 1994;330:1871–1879. doi: 10.1056/NEJM199406303302608. [DOI] [PubMed] [Google Scholar]
- 113.Yaniv G, Twig G, Shor DB, Furer A, Sherer Y, Mozes O, Komisar O, Slonimsky E, Klang E, Lotan E, et al. A volcanic explosion of autoantibodies in systemic lupus erythematosus: A diversity of 180 different antibodies found in SLE patients. Autoimmun Rev. 2015;14:75–79. doi: 10.1016/j.autrev.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 114.Huang WN, Tso TK, Wu HC, Yang HF, Tsay GJ. Impaired phagocytosis of apoptotic cell material in serologically active clinically quiescent patients with systemic lupus erythematosis. Int J Rheum Dis. 2016;19:1310–1316. doi: 10.1111/1756-185X.12826. [DOI] [PubMed] [Google Scholar]
- 115.Sakamoto K, Fukushima Y, Ito K, Matsuda M, Nagata S, Minato N, Hattori M. Osteopontin in Spontaneous Germinal Centers inhibits apoptotic cell engulfment and promotes Anti-Nuclear antibody production in Lupus-Prone Mice. J Immunol. 2016;197:2177–2186. doi: 10.4049/jimmunol.1600987. [DOI] [PubMed] [Google Scholar]
- 116.Recarte-Pelz P, Tàssies D, Espinosa G, Hurtado B, Sala N, Cervera R, Reverter JC, de Frutos PG. Vitamin K-dependent proteins GAS6 and Protein S and TAM receptors in patients of systemic lupus erythematosus: Correlation with common genetic variants and disease activity. Arthritis Res Ther. 2013;15:R41. doi: 10.1186/ar4199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lu Q, Lemke G. Homeostatic regulation of the immune system by receptor tyrosine kinases of the Tyro 3 family. Science. 2001;293:306–311. doi: 10.1126/science.1061663. [DOI] [PubMed] [Google Scholar]
- 118.Rodriguez-Manzanet R, Sanjuan MA, Wu HY, Quintana FJ, Xiao S, Anderson AC, Weiner HL, Green DR, Kuchroo VK. T and B cell hyperactivity and autoimmunity associated with niche-specific defects in apoptotic body clearance in TIM-4-deficient mice. Proc Natl Acad Sci USA. 2010;107:8706–8711. doi: 10.1073/pnas.0910359107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Xiao S, Brooks CR, Zhu C, Wu C, Sweere JM, Petecka S, Yeste A, Quintana FJ, Ichimura T, Sobel RA, et al. Defect in regulatory B-cell function and development of systemic autoimmunity in T-cell Ig mucin 1 (Tim-1) mucin domain-mutant mice. Proc Natl Acad Sci USA. 2012;109:12105–12110. doi: 10.1073/pnas.1120914109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ramirez-Ortiz ZG, Pendergraft WF, III, Prasad A, Byrne MH, Iram T, Blanchette CJ, Luster AD, Hacohen N, El Khoury J, Means TK. The scavenger receptor SCARF1 mediates the clearance of apoptotic cells and prevents autoimmunity. Nat Immunol. 2013;14:917–926. doi: 10.1038/ni.2670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tian L, Choi SC, Murakami Y, Allen J, Morse HC, III, Qi CF, Krzewski K, Coligan JE. p85α recruitment by the CD300f phosphatidylserine receptor mediates apoptotic cell clearance required for autoimmunity suppression. Nat Commun. 2014;5:3146. doi: 10.1038/ncomms4146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Waterborg CEJ, Koenders MI, van Lent PLEM, van der Kraan PM, van de Loo FAJ. Tyro3/Axl/Mertk-deficient mice develop bone marrow edema which is an early pathological marker in rheumatoid arthritis. PLoS One. 2018;13:e0205902. doi: 10.1371/journal.pone.0205902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Park MC, Kwon YJ, Chung SJ, Park YB, Lee SK. Liver X receptor agonist prevents the evolution of collagen-induced arthritis in mice. Rheumatology (Oxford) 2010;49:882–890. doi: 10.1093/rheumatology/keq007. [DOI] [PubMed] [Google Scholar]
- 124.Huang Y, Fu X, Lyu X, Xu Z, He Z, Zhang Y, Zeng Y, He F, Huang G. Activation of LXR attenuates collagen-induced arthritis via suppressing BLyS production. Clin Immunol. 2015;161:339–347. doi: 10.1016/j.clim.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 125.Zhu X, Chen F, Lu K, Wei A, Jiang Q, Cao W. PPARγ preservation via promoter demethylation alleviates osteoarthritis in mice. Ann Rheum Dis. 2019;78:1420–1429. doi: 10.1136/annrheumdis-2018-214940. [DOI] [PubMed] [Google Scholar]
- 126.Noble JA. Immunogenetics of type 1 diabetes: A comprehensive review. J Autoimmun. 2015;64:101–112. doi: 10.1016/j.jaut.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 127.Rodriguez-Fernandez S, Pujol-Autonell I, Brianso F, Perna-Barrull D, Cano-Sarabia M, Garcia-Jimeno S, Villalba A, Sanchez A, Aguilera E, Vazquez F, et al. Phosphatidylserine-liposomes promote tolerogenic features on dendritic cells in human type 1 diabetes by apoptotic mimicry. Front Immunol. 2018;9:253. doi: 10.3389/fimmu.2018.00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Khanna S, Biswas S, Shang Y, Collard E, Azad A, Kauh C, Bhasker V, Gordillo GM, Sen CK, Roy S. Macrophage dysfunction impairs resolution of inflammation in the wounds of diabetic mice. PLoS One. 2010;5:e9539. doi: 10.1371/journal.pone.0009539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Das A, Ghatak S, Sinha M, Chaffee S, Ahmed NS, Parinandi NL, Wohleb ES, Sheridan JF, Sen CK, Roy S. Correction of MFG-E8 resolves inflammation and promotes cutaneous wound healing in diabetes. J Immunol. 2016;196:5089–5100. doi: 10.4049/jimmunol.1502270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Witas R, Peck AB, Ambrus JL, Nguyen CQ. Sjogren's syndrome and TAM receptors: A possible contribution to disease onset. J Immunol Res. 2019;2019:4813795. doi: 10.1155/2019/4813795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Chen CH, Chen HC, Chang CC, Peng YJ, Lee CH, Shieh YS, Hung YJ, Lin YF. Growth arrest-specific 6 protein in patients with Sjögren syndrome: Determination of the plasma level and expression in the labial salivary gland. PLoS One. 2015;10:e0139955. doi: 10.1371/journal.pone.0139955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Qin B, Wang J, Ma N, Yang M, Fu H, Liang Y, Huang F, Yang Z, Zhong R. The association of Tyro3/Axl/Mer signaling with inflammatory response, disease activity in patients with primary Sjögren's syndrome. Joint Bone Spine. 2015;82:258–263. doi: 10.1016/j.jbspin.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 133.Lauber K, Keppeler H, Munoz LE, Koppe U, Schröder K, Yamaguchi H, Krönke G, Uderhardt S, Wesselborg S, Belka C, et al. Milk fat globule-EGF factor 8 mediates the enhancement of apoptotic cell clearance by glucocorticoids. Cell Death Differ. 2013;20:1230–1240. doi: 10.1038/cdd.2013.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zagórska A, Través PG, Lew ED, Dransfield I, Lemke G. Diversification of TAM receptor tyrosine kinase function. Nat Immunol. 2014;15:920–928. doi: 10.1038/ni.2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Elliott MR, Ravichandran KS. Clearance of apoptotic cells: Implications in health and disease. J Cell Biol. 2010;189:1059–1070. doi: 10.1083/jcb.201004096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Maderna P, Yona S, Perretti M, Godson C. Modulation of phagocytosis of apoptotic neutrophils by supernatant from dexamethasone-treated macrophages and annexin-derived peptide Ac(2–26) J Immunol. 2005;174:3727–3733. doi: 10.4049/jimmunol.174.6.3727. [DOI] [PubMed] [Google Scholar]
- 137.Majai G, Sarang Z, Csomós K, Zahuczky G, Fésüs L. PPARgamma-dependent regulation of human macrophages in phagocytosis of apoptotic cells. Eur J Immunol. 2007;37:1343–1354. doi: 10.1002/eji.200636398. [DOI] [PubMed] [Google Scholar]
- 138.Kawano M, Nagata S. Efferocytosis and autoimmune disease. Int Immunol. 2018;30:551–558. doi: 10.1093/intimm/dxy055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Tait AS, Butts CL, Sternberg EM. The role of glucocorticoids and progestins in inflammatory, autoimmune and infectious disease. J Leukoc Biol. 2008;84:924–931. doi: 10.1189/jlb.0208104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wolf SA, Boddeke HW, Kettenmann H. Microglia in physiology and disease. Annu Rev Physiol. 2017;79:619–643. doi: 10.1146/annurev-physiol-022516-034406. [DOI] [PubMed] [Google Scholar]
- 141.Radi E, Formichi P, Battisti C, Federico A. Apoptosis and oxidative stress in neurodegenerative diseases. J Alzheimers Dis. 2014;42((Suppl 3)):S125–S152. doi: 10.3233/JAD-132738. [DOI] [PubMed] [Google Scholar]
- 142.Fuller AD, Eldik LJ. MFG-E8 regulates microglial phagocytosis of apoptotic neurons. J Neuroimmune Pharmacol. 2008;3:246–256. doi: 10.1007/s11481-008-9118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ji R, Tian S, Lu HJ, Lu Q, Zheng Y, Wang X, Ding J, Li Q, Lu Q. TAM receptors affect adult brain neurogenesis by negative regulation of microglial cell activation. J Immunol. 2013;191:6165–6177. doi: 10.4049/jimmunol.1302229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ramachandran G, Udgaonkar JB. Mechanistic studies unravel the complexity inherent in tau aggregation leading to Alzheimer's disease and the tauopathies. Biochemistry. 2013;52:4107–4126. doi: 10.1021/bi400209z. [DOI] [PubMed] [Google Scholar]
- 145.Zheng Y, Wang Q, Xiao B, Lu Q, Wang Y, Wang X. Involvement of receptor tyrosine kinase Tyro3 in amyloidogenic APP processing and β-amyloid deposition in Alzheimer's disease models. PLoS One. 2012;7:e39035. doi: 10.1371/journal.pone.0039035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Fricker M, Neher JJ, Zhao JW, Théry C, Tolkovsky AM, Brown GC. MFG-E8 mediates primary phagocytosis of viable neurons during neuroinflammation. J Neurosci. 2012;32:2657–2666. doi: 10.1523/JNEUROSCI.4837-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Xu X, Zhang A, Zhu Y, He W, Di W, Fang Y, Shi X. MFG-E8 reverses microglial-induced neurotoxic astrocyte (A1) via NF-κB and PI3K-Akt pathways. J Cell Physiol. 2018;234:904–914. doi: 10.1002/jcp.26918. [DOI] [PubMed] [Google Scholar]
- 148.Shi X, Cai X, Di W, Li J, Xu X, Zhang A, Qi W, Zhou Z, Fang Y. MFG-E8 selectively inhibited Aβ-induced microglial M1 polarization via NF-κB and PI3K-Akt pathways. Mol Neurobiol. 2017;54:7777–7788. doi: 10.1007/s12035-016-0255-y. [DOI] [PubMed] [Google Scholar]
- 149.Xu X, Cai X, Zhu Y, He W, Wu Q, Shi X, Fang Y, Pei Z. MFG-E8 inhibits Aβ-induced microglial production of cathelicidin-related antimicrobial peptide: A suitable target against Alzheimer's disease. Cell Immunol. 2018;331:59–66. doi: 10.1016/j.cellimm.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 150.Kalia LV, Kalia SK, McLean PJ, Lozano AM, Lang AE. α-Synuclein oligomers and clinical implications for Parkinson disease. Ann Neurol. 2013;73:155–169. doi: 10.1002/ana.23746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gardai SJ, Mao W, Schüle B, Babcock M, Schoebel S, Lorenzana C, Alexander J, Kim S, Glick H, Hilton K, et al. Elevated alpha-synuclein impairs innate immune cell function and provides a potential peripheral biomarker for Parkinson's disease. PLoS One. 2013;8:e71634. doi: 10.1371/journal.pone.0071634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cardona AE, Pioro EP, Sasse ME, Kostenko V, Cardona SM, Dijkstra IM, Huang D, Kidd G, Dombrowski S, Dutta R, et al. Control of microglial neurotoxicity by the fractalkine receptor. Nat Neurosci. 2006;9:917–924. doi: 10.1038/nn1715. [DOI] [PubMed] [Google Scholar]
- 153.Depboylu C, Schäfer MK, Arias-Carrión O, Oertel WH, Weihe E, Höglinger GU. Possible involvement of complement factor C1q in the clearance of extracellular neuromelanin from the substantia nigra in Parkinson disease. J Neuropathol Exp Neurol. 2011;70:125–132. doi: 10.1097/NEN.0b013e31820805b9. [DOI] [PubMed] [Google Scholar]
- 154.Michelakakis H, Xiromerisiou G, Dardiotis E, Bozi M, Vassilatis D, Kountra PM, Patramani G, Moraitou M, Papadimitriou D, Stamboulis E, et al. Evidence of an association between the scavenger receptor class B member 2 gene and Parkinson's disease. Mov Disord. 2012;27:400–405. doi: 10.1002/mds.24886. [DOI] [PubMed] [Google Scholar]
- 155.Cahoy JD, Emery B, Kaushal A, Foo LC, Zamanian JL, Christopherson KS, Xing Y, Lubischer JL, Krieg PA, Krupenko SA, et al. A transcriptome database for astrocytes, neurons and oligodendrocytes: A new resource for understanding brain development and function. J Neurosci. 2008;28:264–278. doi: 10.1523/JNEUROSCI.4178-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Fourgeaud L, Través PG, Tufail Y, Leal-Bailey H, Lew ED, Burrola PG, Callaway P, Zagórska A, Rothlin CV, Nimmerjahn A, Lemke G. TAM receptors regulate multiple features of microglial physiology. Nature. 2016;532:240–244. doi: 10.1038/nature17630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Nakashima Y, Miyagi-Shiohira C, Noguchi H, Omasa T. The healing effect of human milk fat Globule-EGF factor 8 protein (MFG-E8) in A rat model of Parkinson's disease. Brain Sci. 2018;8:167. doi: 10.3390/brainsci8090167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ghahremani Piraghaj M, Soudi S, Ghanbarian H, Bolandi Z, Namaki S, Hashemi SM. Effect of efferocytosis of apoptotic mesenchymal stem cells (MSCs) on C57BL/6 peritoneal macrophages function. Life Sci. 2018;212:203–212. doi: 10.1016/j.lfs.2018.09.052. [DOI] [PubMed] [Google Scholar]
- 159.Werfel TA, Cook RS. Efferocytosis in the tumor microenvironment. Semin Immunopathol. 2018;40:545–554. doi: 10.1007/s00281-018-0698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Jetten N, Verbruggen S, Gijbels MJ, Post MJ, De Winther MP, Donners MM. Anti-inflammatory M2, but not pro-inflammatory M1 macrophages promote angiogenesis in vivo. Angiogenesis. 2014;17:109–118. doi: 10.1007/s10456-013-9381-6. [DOI] [PubMed] [Google Scholar]
- 161.Han Q, Shi H, Liu F. CD163(+) M2-type tumor-associated macrophage support the suppression of tumor-infiltrating T cells in osteosarcoma. Int Immunopharmacol. 2016;34:101–106. doi: 10.1016/j.intimp.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 162.Finkernagel F, Reinartz S, Lieber S, Adhikary T, Wortmann A, Hoffmann N, Bieringer T, Nist A, Stiewe T, Jansen JM, et al. The transcriptional signature of human ovarian carcinoma macrophages is associated with extracellular matrix reorganization. Oncotarget. 2016;7:75339–75352. doi: 10.18632/oncotarget.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Yeh HW, Chiang CF, Chen PH, Su CC, Wu YC, Chou L, Huang RY, Liu SY, Shieh YS. Axl involved in mineral trioxide aggregate induces macrophage polarization. J Endod. 2018;44:1542–1548. doi: 10.1016/j.joen.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 164.Graham DK, Salzberg DB, Kurtzberg J, Sather S, Matsushima GK, Keating AK, Liang X, Lovell MA, Williams SA, Dawson TL, et al. Ectopic expression of the proto-oncogene Mer in pediatric T-cell acute lymphoblastic leukemia. Clin Cancer Res. 2006;12:2662–2669. doi: 10.1158/1078-0432.CCR-05-2208. [DOI] [PubMed] [Google Scholar]
- 165.Wang Y, Moncayo G, Morin P, Jr, Xue G, Grzmil M, Lino MM, Clément-Schatlo V, Frank S, Merlo A, Hemmings BA. Mer receptor tyrosine kinase promotes invasion and survival in glioblastoma multiforme. Oncogene. 2013;32:872–882. doi: 10.1038/onc.2012.104. [DOI] [PubMed] [Google Scholar]
- 166.Schlegel J, Sambade MJ, Sather S, Moschos SJ, Tan AC, Winges A, DeRyckere D, Carson CC, Trembath DG, Tentler JJ, et al. MERTK receptor tyrosine kinase is a therapeutic target in melanoma. J Clin Invest. 2013;123:2257–2267. doi: 10.1172/JCI67816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Myers KV, Amend SR, Pienta KJ. Targeting Tyro3, Axl and MerTK (TAM receptors): Implications for macrophages in the tumor microenvironment. Mol Cancer. 2019;18:94. doi: 10.1186/s12943-019-1022-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bondanza A, Zimmermann VS, Rovere-Querini P, Turnay J, Dumitriu IE, Stach CM, Voll RE, Gaipl US, Bertling W, Pöschl E, et al. Inhibition of phosphatidylserine recognition heightens the immunogenicity of irradiated lymphoma cells in vivo. J Exp Med. 2004;200:1157–1165. doi: 10.1084/jem.20040327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Linger RM, Keating AK, Earp HS, Graham DK. Taking aim at Mer and Axl receptor tyrosine kinases as novel therapeutic targets in solid tumors. Expert Opin Ther Targets. 2010;14:1073–1090. doi: 10.1517/14728222.2010.515980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sawabu T, Seno H, Kawashima T, Fukuda A, Uenoyama Y, Kawada M, Kanda N, Sekikawa A, Fukui H, Yanagita M, et al. Growth arrest-specific gene 6 and Axl signaling enhances gastric cancer cell survival via Akt pathway. Mol Carcinog. 2007;46:155–164. doi: 10.1002/mc.20211. [DOI] [PubMed] [Google Scholar]
- 171.Lee-Sherick AB, Eisenman KM, Sather S, McGranahan A, Armistead PM, McGary CS, Hunsucker SA, Schlegel J, Martinson H, Cannon C, et al. Aberrant Mer receptor tyrosine kinase expression contributes to leukemogenesis in acute myeloid leukemia. Oncogene. 2013;32:5359–5368. doi: 10.1038/onc.2013.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Brightwell RM, Grzankowski KS, Lele S, Eng K, Arshad M, Chen H, Odunsi K. The CD47 ‘don't eat me signal’ is highly expressed in human ovarian cancer. Gynecol Oncol. 2016;143:393–397. doi: 10.1016/j.ygyno.2016.08.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Willingham SB, Volkmer JP, Gentles AJ, Sahoo D, Dalerba P, Mitra SS, Wang J, Contreras-Trujillo H, Martin R, Cohen JD, et al. The CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. Proc Natl Acad Sci USA. 2012;109:6662–6667. doi: 10.1073/pnas.1121623109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chao MP, Alizadeh AA, Tang C, Myklebust JH, Varghese B, Gill S, Jan M, Cha AC, Chan CK, Tan BT, et al. Anti-CD47 antibody synergizes with rituximab to promote phagocytosis and eradicate non-Hodgkin lymphoma. Cell. 2010;142:699–713. doi: 10.1016/j.cell.2010.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Liang YY, Schwarzinger I, Simonitsch-Klupp I, Agis H, Oehler R. Impaired efferocytosis by monocytes in multiple myeloma. Oncol Lett. 2018;16:409–416. doi: 10.3892/ol.2018.8620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Terzić J, Grivennikov S, Karin E, Karin M. Inflammation and colon cancer. Gastroenterology. 2010;138:2101–2114.e5. doi: 10.1053/j.gastro.2010.01.058. [DOI] [PubMed] [Google Scholar]
- 177.Lew DS, Mazzoni F, Finnemann SC. Microglia inhibition delays retinal degeneration due to MerTK phagocytosis receptor deficiency. Front Immunol. 2020;11:1463. doi: 10.3389/fimmu.2020.01463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Jun JI, Kim KH, Lau LF. The matricellular protein CCN1 mediates neutrophil efferocytosis in cutaneous wound healing. Nat Commun. 2015;6:7386. doi: 10.1038/ncomms8386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Borucki DM, Toutonji A, Couch C, Mallah K, Rohrer B, Tomlinson S. Complement-mediated microglial phagocytosis and pathological changes in the development and degeneration of the visual system. Front Immunol. 2020;11:566892. doi: 10.3389/fimmu.2020.566892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Bossi F, Tripodo C, Rizzi L, Bulla R, Agostinis C, Guarnotta C, Munaut C, Baldassarre G, Papa G, Zorzet S, et al. C1q as a unique player in angiogenesis with therapeutic implication in wound healing. Proc Natl Acad Sci USA. 2014;111:4209–4214. doi: 10.1073/pnas.1311968111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Wang J, Wong YK, Liao F. What has traditional Chinese medicine delivered for modern medicine? Expert Rev Mol Med. 2018;20:e4. doi: 10.1017/erm.2018.3. [DOI] [PubMed] [Google Scholar]
- 182.Wei J, Wang J, Ma G, Liu P. Effects of Guanxinkang on efferocytosis of spleen macrophages in LDLR-/-mice. Academic Journal of Shanghai University of Traditional Chinese Medicine. 2018;32:56–61. (In Chinese) [Google Scholar]
- 183.Wang J, Mao M, Deng B, Liu P. Effects of Guanxinkang medicated serum on MerTK expression in RAW264.7 macrophages. Academic Journal of Shanghai University of Traditional Chinese Medicine. 2018;32:45–48. (In Chinese) [Google Scholar]
- 184.Wang J, Liu P. Effects of Guanxinkang and its separate prescriptions on TAM receptor expression in peritoneal macrophages of LDLR−/− atherosclerotic mice. Lishizhen Medicine and Materia Medica Research. 2018;29:2326–2328. (In Chinese) [Google Scholar]
- 185.Susanti E, Ratnawati R, Aulani A, Rudijanto A. Catechins green tea upregulates the expression of ABCA1, ABCG1 and SRB1 in rats induced atherogenic diet. J Appl Pharma Sci. 2019;9:91–97. doi: 10.7324/JAPS.2019.90313. [DOI] [Google Scholar]
- 186.Li XY, Kong LX, Li J, He HX, Zhou YD. Kaempferol suppresses lipid accumulation in macrophages through the downregulation of cluster of differentiation 36 and the upregulation of scavenger receptor class B type I and ATP-binding cassette transporters A1 and G1. Int J Mol Med. 2013;31:331–338. doi: 10.3892/ijmm.2012.1204. [DOI] [PubMed] [Google Scholar]
- 187.Kim MS, Kim DS, Kim HS, Kang SW, Kang YH. Inhibitory effects of luteolin on transendothelial migration of monocytes and formation of lipid-laden macrophages. Nutrition. 2012;28:1044–1054. doi: 10.1016/j.nut.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 188.Park SH, Kim JL, Lee ES, Han SY, Gong JH, Kang MK, Kang YH. Dietary ellagic acid attenuates oxidized LDL uptake and stimulates cholesterol efflux in murine macrophages. J Nutr. 2011;141:1931–1937. doi: 10.3945/jn.111.144816. [DOI] [PubMed] [Google Scholar]
- 189.Guan S, Wang B, Li W, Guan J, Fang X. Effects of berberine on expression of LOX-1 and SR-BI in human macrophage-derived foam cells induced by ox-LDL. Am J Chin Med. 2010;38:1161–1169. doi: 10.1142/S0192415X10008548. [DOI] [PubMed] [Google Scholar]
- 190.Uto-Kondo H, Ayaori M, Ogura M, Nakaya K, Ito M, Suzuki A, Takiguchi S, Yakushiji E, Terao Y, Ozasa H, et al. Coffee consumption enhances high-density lipoprotein-mediated cholesterol efflux in macrophages. Circ Res. 2010;106:779–787. doi: 10.1161/CIRCRESAHA.109.206615. [DOI] [PubMed] [Google Scholar]
- 191.Ford HZ, Zeboudj L, Purvis GSD, Ten Bokum A, Zarebski AE, Bull JA, Byrne HM, Myerscough MR, Greaves DR. Efferocytosis perpetuates substance accumulation inside macrophage populations. Proc Biol Sci. 2019;286:20190730. doi: 10.1098/rspb.2019.0730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Dattaroy D, Seth RK, Das S, Alhasson F, Chandrashekaran V, Michelotti G, Fan D, Nagarkatti M, Nagarkatti P, Diehl AM, Chatterjee S. Sparstolonin B attenuates early liver inflammation in experimental NASH by modulating TLR4 trafficking in lipid rafts via NADPH oxidase activation. Am J Physiol Gastrointest Liver Physiol. 2016;310:G510–525. doi: 10.1152/ajpgi.00259.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Zhang X, Zhao Y, Zhang M, Pang X, Xu J, Kang C, Li M, Zhang C, Zhang Z, Zhang Y, et al. Structural changes of gut microbiota during berberine-mediated prevention of obesity and insulin resistance in high-fat diet-fed rats. PLoS One. 2012;7:e42529. doi: 10.1371/journal.pone.0042529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Luo D, Guo Y, Cheng Y, Zhao J, Wang Y, Rong J. Natural product celastrol suppressed macrophage M1 polarization against inflammation in diet-induced obese mice via regulating Nrf2/HO-1, MAP kinase and NF-κB pathways. Aging (Albany NY) 2017;9:2069–2082. doi: 10.18632/aging.101302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lai YS, Putra RBDS, Aui SP, Chang KT. M2C polarization by baicalin enhances efferocytosis via upregulation of MERTK receptor. Am J Chin Med. 2018;46:1899–1914. doi: 10.1142/S0192415X18500957. [DOI] [PubMed] [Google Scholar]
- 196.Zhu W, Jin Z, Yu J, Liang J, Yang Q, Li F, Shi X, Zhu X, Zhang X. Baicalin ameliorates experimental inflammatory bowel disease through polarization of macrophages to an M2 phenotype. Int Immunopharmacol. 2016;35:119–126. doi: 10.1016/j.intimp.2016.03.030. [DOI] [PubMed] [Google Scholar]
- 197.Cai Q, Li Y, Pei G. Polysaccharides from Ganoderma lucidum attenuate microglia-mediated neuroinflammation and modulate microglial phagocytosis and behavioural response. J Neuroinflammation. 2017;14:63. doi: 10.1186/s12974-017-0839-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Wu TF, Hsu CY, Huang HS, Chou SP, Wu H. Proteomic analysis of pycnogenol effects in RAW 264.7 macrophage reveals induction of cathepsin D expression and enhancement of phagocytosis. J Agric Food Chem. 2007;55:9784–9791. doi: 10.1021/jf070453o. [DOI] [PubMed] [Google Scholar]
- 199.Tong H, Mao D, Zhai M, Zhang Z, Sun G, Jiang G. Macrophage activation induced by the polysaccharides isolated from the roots of Sanguisorba officinalis. Pharm Biol. 2015;53:1511–1515. doi: 10.3109/13880209.2014.991834. [DOI] [PubMed] [Google Scholar]
- 200.Wang H, Wei G, Liu F, Banerjee G, Joshi M, Bligh SW, Shi S, Lian H, Fan H, Gu X, Wang S. Characterization of two homogalacturonan pectins with immunomodulatory activity from green tea. Int J Mol Sci. 2014;15:9963–9978. doi: 10.3390/ijms15069963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Gheibi Hayat SM, Bianconi V, Pirro M, Sahebkar A. Efferocytosis: Molecular mechanisms and pathophysiological perspectives. Immunol Cell Biol. 2019;97:124–133. doi: 10.1111/imcb.12206. [DOI] [PubMed] [Google Scholar]
- 202.Holden RM, Hétu MF, Li TY, Ward EC, Couture LE, Herr JE, Christilaw E, Adams MA, Johri AM. Circulating Gas6 is associated with reduced human carotid atherosclerotic plaque burden in high risk cardiac patients. Clin Biochem. 2019;64:6–11. doi: 10.1016/j.clinbiochem.2018.11.018. [DOI] [PubMed] [Google Scholar]
- 203.Brophy ML, Dong Y, Tao H, Yancey PG, Song K, Zhang K, Wen A, Wu H, Lee Y, Malovichko MV, et al. Myeloid-specific deletion of epsins 1 and 2 reduces atherosclerosis by preventing LRP-1 downregulation. Circ Res. 2019;124:e6–e19. doi: 10.1161/CIRCRESAHA.118.313028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Ait-Oufella H, Pouresmail V, Simon T, Blanc-Brude O, Kinugawa K, Merval R, Offenstadt G, Lesèche G, Cohen PL, Tedgui A, Mallat Z. Defective mer receptor tyrosine kinase signaling in bone marrow cells promotes apoptotic cell accumulation and accelerates atherosclerosis. Arterioscler Thromb Vasc Biol. 2008;28:1429–1431. doi: 10.1161/ATVBAHA.108.169078. [DOI] [PubMed] [Google Scholar]
- 205.Zhang Y, Wang Y, Zhou D, Zhang LS, Deng FX, Shu S, Wang LJ, Wu Y, Guo N, Zhou J, Yuan ZY. Angiotensin II deteriorates advanced atherosclerosis by promoting MerTK cleavage and impairing efferocytosis through the AT1R/ROS/p38 MAPK/ADAM17 pathway. Am J Physiol Cell Physiol. 2019;317:C776–C787. doi: 10.1152/ajpcell.00145.2019. [DOI] [PubMed] [Google Scholar]
- 206.Thorp E, Cui D, Schrijvers DM, Kuriakose G, Tabas I. Mertk receptor mutation reduces efferocytosis efficiency and promotes apoptotic cell accumulation and plaque necrosis in atherosclerotic lesions of apoe−/− mice. Arterioscler Thromb Vasc Biol. 2008;28:1421–1428. doi: 10.1161/ATVBAHA.108.167197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Boisvert WA, Rose DM, Boullier A, Quehenberger O, Sydlaske A, Johnson KA, Curtiss LK, Terkeltaub R. Leukocyte transglutaminase 2 expression limits atherosclerotic lesion size. Arterioscler Thromb Vasc Biol. 2006;26:563–569. doi: 10.1161/01.ATV.0000203503.82693.c1. [DOI] [PubMed] [Google Scholar]
- 208.Gong S, Xu Z, Liu Y, Xing L, Ma J, Yu C, Liu X, Jia X, Xie R, Sui M. Plasma sMer, sAxl and GAS6 levels correlate with disease activity and severity in lupus nephritis. Eur J Clin Invest. 2019;49:e13064. doi: 10.1111/eci.13064. [DOI] [PubMed] [Google Scholar]
- 209.Tworkoski KA, Platt JT, Bacchiocchi A, Bosenberg M, Boggon TJ, Stern DF. MERTK controls melanoma cell migration and survival and differentially regulates cell behavior relative to AXL. Pigment Cell Melanoma Res. 2013;26:527–541. doi: 10.1111/pcmr.12110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Demarest SJ, Gardner J, Vendel MC, Ailor E, Szak S, Huang F, Doern A, Tan X, Yang W, Grueneberg DA, et al. Evaluation of Tyro3 expression, Gas6-mediated Akt phosphorylation and the impact of anti-Tyro3 antibodies in melanoma cell lines. Biochemistry. 2013;52:3102–3118. doi: 10.1021/bi301588c. [DOI] [PubMed] [Google Scholar]
- 211.Xie S, Li Y, Li X, Wang L, Yang N, Wang Y, Wei H. Mer receptor tyrosine kinase is frequently overexpressed in human non-small cell lung cancer, confirming resistance to erlotinib. Oncotarget. 2015;6:9206–9219. doi: 10.18632/oncotarget.3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Walport MJ, Davies KA, Botto M. C1q and systemic lupus erythematosus. Immunobiology. 1998;199:265–285. doi: 10.1016/S0171-2985(98)80032-6. [DOI] [PubMed] [Google Scholar]
- 213.Huang W, Wu J, Yang H, Xiong Y, Jiang R, Cui T, Ye D. Milk fat globule-EGF factor 8 suppresses the aberrant immune response of systemic lupus erythematosus-derived neutrophils and associated tissue damage. Cell Death Differ. 2017;24:263–275. doi: 10.1038/cdd.2016.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Zhu H, Sun X, Zhu L, Hu F, Shi L, Li Z, Su Y. The expression and clinical significance of different forms of Mer receptor tyrosine kinase in systemic lupus erythematosus. J Immunol Res. 2014;2014:431896. doi: 10.1155/2014/431896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Bertolaccini ML, Sanna G, Ralhan S, Gennari LC, Merrill JT, Khamashta MA, Hughes GR. Antibodies directed to protein S in patients with systemic lupus erythematosus: Prevalence and clinical significance. Thromb Haemost. 2003;90:636–641. doi: 10.1160/TH03-03-0151. [DOI] [PubMed] [Google Scholar]
- 216.Peng Y, Elkon KB. Autoimmunity in MFG-E8-deficient mice is associated with altered trafficking and enhanced cross-presentation of apoptotic cell antigens. J Clin Invest. 2011;121:2221–2241. doi: 10.1172/JCI43254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Avilla E, Guarino V, Visciano C, Liotti F, Svelto M, Krishnamoorthy G, Franco R, Melillo RM. Activation of TYRO3/AXL tyrosine kinase receptors in thyroid cancer. Cancer Res. 2011;71:1792–1804. doi: 10.1158/0008-5472.CAN-10-2186. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article, as no data sets were generated or analyzed during the current study.