Abstract
Background: The COVID-19 pandemic generates negative psychological effects such as distress. Social influences on subjective distress associated with COVID-19 remain understudied in the Chinese context. Wuhan with its surrounding areas in Hubei province was not only the locale where first COVID-19 cases were detected in the world but was also the hardest hit across China. Data from Hubei provide a unique opportunity to investigate COVID-19-related subjective distress and its social correlates.
Methods: We use original data (N=3,465) from the General Social Survey on COVID-19 in Hubei, China, conducted in August 2020. Regression analysis is employed to examine the impact of socioeconomic status, family structure, and social policies on COVID-19-related subjective distress measured by the Impact of Event-Scale-Revised (IES-R).
Results: First, individuals with higher socioeconomic status are not more immune to distress, and actually it is those better-educated ones who are more distressed. Second, family structure influences distress. Divorced and widowed individuals are more prone to distress than those who are married or single. Those living with COVID-19-infected family members or living with a larger family are particularly more distressed. Third, stricter lockdown measures promote real and perceived protection and also increase individuals’ psychological distance from the disease, thereby reducing subjective distress.
Limitations: The sample is not totally random so we should use caution when generalizing the findings to the general population.
Conclusions: The findings contribute to our understanding of mental health disparity during the COVID-19 pandemic. Certain social groups are at a higher risk of distress than others.
Keywords: COVID-19, subjective distress, socioeconomic status, family, China
1. Introduction
The novel coronavirus (COVID-19) outbreak was first discovered in Wuhan, the capital city of China's Hubei province, where the initial cases were reported by Wuhan Municipal Health Commission on December 31, 2019 (Heymann, 2020). Coinciding with the emergence of COVID-19, massive human migration took place around Wuhan and other cities in Hubei province as individuals traveled back to their hometowns for the Chinese New Year holidays (Chen et al., 2020). In late January 2020, an increasing number of confirmed cases of COVID-19 infection were detected outside Wuhan (Backer et al., 2020). It only took 30 days for the COVID-19 epidemic to spread from Hubei to the rest of Mainland China. Since then the virus has been spreading quickly over the globe. Many countries have now been affected by COVID-19, which was declared by the World Health Organization (WHO) as a public health emergency of international concern on January 30, 2020 and a pandemic on March 11, 2020 (World Health Organization 2020). COVID-19 has led to millions of infected cases and hundreds of thousands of deaths globally (Cao et al., 2020; Liu et al., 2020; Usher, Durkin, and Bhullar, 2020). To contain the outbreak, countries took various lockdown measures to different extents, such as isolation of cases, contact tracing, community quarantine, travel bans, closing of schools, and social distancing. These measures are widely recommended worldwide to slow down and contain the spread of the virus, although the actual effectiveness of their implementation varies across countries and across social groups (Huynh, 2020; Jaja et al., 2020; Marchiori, 2020; O'Connell et al., 2020; Xie et al., 2020). The measures taken by China were among the most stringent, which kept tens of millions of people in isolation and affected many aspects of people's lives (Dandekar and Barbastathis, 2020; Qiu et al., 2020; Yang et al., 2020).
Emerging evidence has shown that the COVID-19 pandemic has negative psychological effects which can be widespread and long-lasting (Douglas et al., 2020; Holmes et al., 2020; Shanafelt, Ripp, and Trockel, 2020; Zhou and Guo, 2021). From a psychological perspective, pandemics engender life events associated with uncertainty, ambiguity, and loss of control, which are known to trigger emotional distress, so the level of distress in a population can significantly grow during a pandemic (Serafini et al., 2020). Distress impairs health, subjective well-being, and quality of life (Malone and Wachholtz, 2018). Recent survey studies in China found that many respondents suffered from psychological distress during the COVID-19 pandemic (Cao et al., 2020; Qiu et al., 2020). COVID-19-related distress is not evenly distributed in the population, however (Fitzpatrick et al., 2020). Psychological distress has a social dimension (Compton, Thompson, and Kaslow, 2005; Donev, 2005), and some social groups are more prone to distress than others. It remains an open empirical question how social factors aggravate or mitigate psychological distress during the COVID-19 pandemic.
To help fill this lacuna, we use original data from the General Social Survey on COVID-19 in Hubei, China, conducted in August 2020. Wuhan with its surrounding areas in Hubei province was not only the locale where first COVID-19 cases were reported in the world but was also the hardest hit across China.3 The data provide a unique opportunity to investigate how individuals with different social backgrounds experience distress differently at the epicenter of the COVID-19 pandemic. By highlighting the importance of social factors in shaping distress associated with COVID-19, this study sheds light on the mechanisms that may help inform distress-reducing interventions during this globally challenging time. It also broadly contributes to the emerging scholarship on social inequality in mental health during a pandemic.
2. Distress Associated with COVID-19
Psychological distress symptoms, defined as negative reactions to recent life difficulties or stressful situations, can impact people's long-term mental health (Massé et al., 1998; Roy et al., 2020; Usher, Durkin, and Bhullar, 2020). Intense psychological distress is a hallmark of mental disorders associated with poorer health outcomes and increased mortality risk, regardless of the population studied and health outcome examined (see Barry et al. 2020 for a systematic review). The COVID-19 pandemic triggers a wide variety of psychological problems including distress (Fernández et al., 2020, Qiu et al., 2020). While it is widely acknowledged that social factors shape health and stress disparities within a population (Adler and Newman, 2002), it remains largely unknown how social factors underlie the distribution of distress in a population during the COVID-19 pandemic. We highlight three sets of social factors that potentially influence different levels of distress within a society, including socioeconomic status, family structure, and social policy environment.
2.1. Socioeconomic Status
Socioeconomic status (SES) is a reliable predictor of health disparity. The negative relationship between SES and psychological distress is one of the most firmly established associations in the mental health literature (Kessler, 1982; Kosidou et al., 2011). Conventional SES measures include education, income, and occupation, and each of these measures captures a distinct aspect of SES. They may be correlated with each other but are not interchangeable (Shavers, 2007). Education and income are usually considered to be negatively associated with psychological distress, because they provide necessary resources for coping with stress in life (Chen et al., 2019; Sancakoğlu and Sayar, 2012). Disadvantaged SES has long been identified as a risk factor for mental health problems. Less income often directly causes stress stemming from economic hardship (Cockerham, 1990). Less educated individuals have higher levels of psychological distress because less education further deprives people of the problem-solving resources and knowledge needed to cope with stress (Ross & Van Willigen, 1997; Zhang et al., 2015). We thus expect that those with better education and greater income show lower levels of distress associated with COVID-19. Previous research suggested a limited role for occupation as a decisive condition leading to psychological distress. Instead, the structure of daily life plays a more important role in psychological distress compared with occupational structure (Marchand et al., 2005). Nevertheless, it is also possible that different occupations are associated with differential resources that can be utilized to cope with stress. Some occupations have higher prestige in society, provide more opportunities for social networking, and come with better benefits that are not measured by income (Vallas, Finlay, and Warton, 2009). Taken together, the existing literature seems to provide no clear clue about whether and which occupations are better at coping with COVID-19-related distress.
2.2. Family Structure
A number of previous studies provide support for the relationship between perceived family support and mental health (e.g., Bauer et al., 2020; Cano et al., 2003; Cramer, 1991). The perception that social support from family members and friends would be available if needed helps mental health because it softens the appraisal of the situation and prevents the cascading of negative stress responses (Kawachi and Berkman, 2001). Family support is more important than friend support in reducing the deleterious effect of stressors on psychological distress (Bostean et al., 2019). During the COVID-19 lockdown it is found that lower satisfaction with the support from the family may lead to higher self-reported distress (Losada-Baltar et al., 2020). Family members represent a primary source of social support, especially during a lockdown. Family support has direct health-enhancing effects and may diminish the negative effects of stressors (Albrecht and Goldsmith, 2003). Being married and living with family members may provide important emotional and social support when social distancing is implemented and people are mostly confined to their homes during the COVID-19 pandemic. More family members potentially counteract the sense of isolation engendered by stringent social distancing and lockdown measures, thereby reducing distress.
2.3. Social Policy Environment
Social distancing and lockdown measures are commonly recommended during epidemics and pandemics. For instance, social distancing has widely been found to significantly reduce the number of influenza cases and delays the influenza peak (Ahmed et al., 2018). These measures are also the most recommended policies during the COVID-19 pandemic, and a wealth of emerging research has been examining how to promote their effective implementation in practice (Huynh, 2020; Jaja et al., 2020; Marchiori, 2020; O'Connell et al., 2020; Xie et al., 2020). The implementation of strict social distancing and lockdown measures may have two counteracting effects on psychological distress. On the one hand, these measures disrupt people's normal lifestyles and social interactions and also lead to perceived lack of social support, which may all exacerbate psychological distress (Gan et al., 2020; Sibley et al., 2020). For instance, Shanahan et al. (2020) found that COVID-19-related lifestyle disruptions were among the strongest correlates of young adults’ distress during the COVID-19 lockdown. This can be seen as the distress-inducing effect of COVID-19 lockdown measures. Some scholars thus called for intervention measures that would promote social connections in order to mitigate this distress-inducing effect of the COVID-19 lockdown (Sibley et al., 2020; Tull et al., 2020). On the other hand, it is also possible that stringent lockdown measures can offer individuals more perceived security and more confidence in the community's efficacy in tackling COVID-19, thereby reducing the level of psychological distress. The perception of better protection provided by the community has been shown to buffer the impact of stress and help people in social isolation cope with challenges psychologically (Jetten et al., 2011). Moreover, lockdown measures cut off interpersonal contact, restrict traffic and social activities, and construct a local safety “bubble” around the community. All these, consciously or subconsciously, increase individuals’ perceived “distance” of COVID-19 from their community. This increased psychological distance from COVID-19 reduces individuals’ subjective distress. The boosted sense of security and the increased psychological distance, taken together, can be seen as the distress-reducing effect of COVID-19 lockdown measures. Due to these potentially counteracting (distress-inducing and distress-reducing) effects, it remains to be empirically tested whether stricter lockdown measures increase or decrease psychological distress during the COVID-19 pandemic.
3. Data and Methods
The data are from the General Social Survey on COVID-19 in Hubei, China, which was conducted in August 2020 by Central China Normal University in Wuhan, Hubei province. Survey participants were not randomly selected but were recruited through the popular social media app “WeChat” (weixin). With the support from the Hubei Provincial Federation of Trade Unions, this survey reached a large population and finally collected information from as many as 25,465 participants aged between 16 and 70, who answered various questions about their experiences during the COVID-19 pandemic. Among them, 3,465 completed the mental health module and this sample of 3,465 individuals is analyzed in this study. This large sample size of 3,465 provides sufficient power to detecting statistical effects in multiple regression models, according to statistical power analyses (Faul et al., 2007; Green, 1991; Wilson VanVoorhis and Morgan, 2007). It is worth noting that the sampling was non-random so we should use caution when generalizing the findings to the general population. Nevertheless, this sampling made it possible to generate useful and timely information on a large sample in a short period of time when the COVID-19 pandemic was still evolving rapidly.
3.1. Dependent Variable
Subjective distress is measured by the widely used and well-established Impact of Event-Scale-Revised (IES-R) (Weiss and Marmar, 1997). The IES-R is a 22-item self-reported measure that assesses subjective distress caused by a certain traumatic event (in this case, COVID-19). Each item is rated on a 5-point scale ranging from 0 (“not at all”) to 4 (“always”). It is a revised version of the older version, the 15-item IES (Horowitz, Wilner, and Alvarez, 1979). A wealth of evidence has shown the IES-R to be a reliable and valid index of post-traumatic symptoms (Beck et al., 2008; Brunet et al., 2002). Our survey strictly followed the IES-R scheme and contained all the 22 items. Respondents were asked to indicate how much they felt distressed by COVID-19 during the past two weeks through the 22 items. The IES-R yields a total score ranging from 0 to 88, with a greater score indicating greater subjective distress related to COVID-19. This total score is used as the dependent variable of subjective distress. The Cronbach's alpha among the 22 items is extremely high (0.980), indicating good internal consistency and excellent reliability of the composite subjective distress measure. Table 1 displays the 22 items constituting the dependent variable.
Table 1.
The 22 Survey Items Used in Measuring COVID-19-Related Subjective Distress.
| 1 | Any reminders brought uncomfortable feelings about COVID-19. |
|---|---|
| 2 | I had trouble staying asleep. |
| 3 | Other things kept making me think about COVID-19. |
| 4 | I thought about COVID-19 when I didn't mean to. |
| 5 | Pictures about COVID-19 popped into my mind. |
| 6 | I found myself acting or feeling affected by COVID-19. |
| 7 | I felt I was being surrounded by COVID-19. |
| 8 | I had dreams about COVID-19. |
| 9 | I avoided letting myself get upset by COVID-19. |
| 10 | I felt COVID-19 was surreal. |
| 11 | I tried to stay away from reminders about COVID-19. |
| 12 | I tried not to think about COVID-19. |
| 13 | I was aware that I still had a lot of feelings about COVID-19 and did not know how to handle them. |
| 14 | My feelings about COVID-19 were kind of numb. |
| 15 | I tried to remove COVID-19 from my memory. |
| 16 | I tried not to talk about COVID-19. |
| 17 | I felt irritable and angry. |
| 18 | I was jumpy and easily startled. |
| 19 | I had trouble falling asleep. |
| 20 | I had trouble concentrating. |
| 21 | Reminders caused me to have physical reactions. |
| 22 | I felt watchful and on guard. |
Notes: Each item is rated on a 5-point scale ranging from 0 (“not at all”) to 4 (“always”).
3.2. Independent Variables
We use education, income, and occupation, three conventional variables for measuring socioeconomic status (Shavers, 2007). Education is measured by the highest degree achieved and is on a 6-point scale including (1) elementary school or below, (2) junior middle school, (3) senior middle school or secondary vocational school, (4) junior college, (5) university, and (6) postgraduate education. Income is assessed by one's average monthly household income (in Chinese Yuan) in 2020 and is on a 16-point scale including (1) under 1,000, (2) 1,000-2,000, (3) 2,000-3,000, and up to (16) above 15,000. Occupation is captured by 7 occupational categories including (1) government (including the Communist Party) and public services, (2) state-owned or collective enterprises, (3) private enterprises, (4) social organizations, (5) self-employed, (6) other occupations, and (7) unemployed. We create a set of dummy variables representing different occupational categories.
Family structure is measured by marital status and the number of family members. The two variables capture important aspects of family structure (Brown, Manning, and Stykes, 2015). Marital status contains three categories, namely (1) single (never married), (2) married, and (3) divorced or widowed. The number of family members measures how many family members (including the respondent) currently live in the household.
Social policy environment is captured by the respondent's self-rated strictness of the lockdown measures taken by the local community, such as guarded entrances into the neighborhood, regular checks on households, taking residents’ body temperature regularly, keeping records of residents’ travel history, etc. While the government issued an overall lockdown order in Hubei, lockdown measures were largely carried out by local residential communities (Mei, 2020). The strictness of the lockdown measures’ implementation may vary from community to community. It is measured on a five-point scale ranging from (1) “not strict at all”, (2) “not very strict”, (3) “just so-so”, (4) “somewhat strict”, to (5) “very strict”.
In addition to these variables of major interest, we also control demographic variables including gender, age, ethnicity, residence type, and migrant status. Gender is a binary variable with male coded as 1 and female as 0. Age is measured in years.4 Ethnicity is measured as a binary variable, with the Han ethnicity coded as 1 and non-Han minority ethnicities as 0. Residence type is the respondent's household registration (or hukou) type, with rural coded as 1 and urban coded as 0. We also consider whether the respondent is a migrant currently living outside of their hometown. Migrant status is a binary variable, with 1 indicating a migrant and 0 not.
We further take into account whether respondents and their family members contracted COVID-19 (including both confirmed and suspected cases). Two variables are created accordingly. The variable of “self-infection” measures whether the respondent was infected with COVID-19, while the variable of “family-infection” captures whether anyone in the respondent's family was infected. Both variables are binary, with 1 indicating yes and 0 no.
3.3. Modeling Strategy
The dependent variable, subjective distress, is measured on a 0-88 point scale, so we use the ordinary least squares (OLS) model. We define Y as the level of subjective distress, and specify the model as follows. Here β is the coefficient and ε is the error term.
Y = β0 + β1Gender + β2Age + β3Ethnicity + β4Rural + β5Migrant +β6Education + β7Income + β8Occupation + β9Marital + β10Family + β11Policy + β12Self-Infection + β13Family-Infection + ε.
4. Results
4.1. Descriptive Statistics
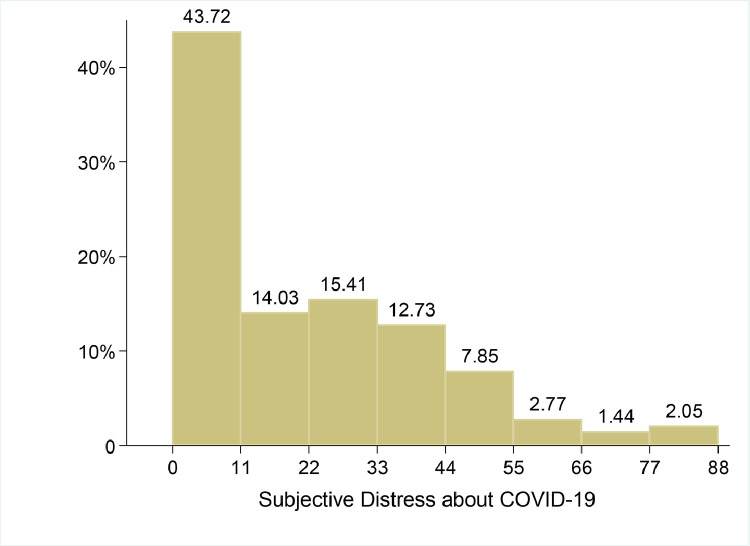
Table 2 presents the descriptive statistics of the variables used in the analysis. The average subjective distress score based on the IES-R is 20.05 (out of a total of 88). While generally a larger score indicates greater subjective distress, a score of 33 is sometimes used as the cut-off point to classify individuals as experiencing psychological distress above or below the clinical threshold (Creamer, Bell, Failla, 2003; Sullivan et al., 2009). There is much variation among individuals with respect to subjective distress about COVID-19. In particular, 26.84% of the respondents have scores above 33, thereby displaying clinically significant psychological distress symptoms. Fig. 1 shows the distribution of subjective distress about COVID-19 among the surveyed individuals.
Table 2.
Descriptive Statistics for Dependent and Independent Variables.
| Variables | Mean | Std. Dev. | Minimum | Maximum |
|---|---|---|---|---|
| Subjective distress about COVID-19 | 20.049 | 20.708 | 0 | 88 |
| Gender (male) | .529 | .499 | 0 | 1 |
| Age | 31.808 | 9.387 | 16 | 70 |
| Ethnicity (Han) | .959 | .198 | 0 | 1 |
| Residence type (rural) | .255 | .436 | 0 | 1 |
| Migrant | .261 | .439 | 0 | 1 |
| Education | 3.900 | 1.147 | 1 | 6 |
| Income | 5.084 | 2.932 | 1 | 16 |
| Occupation | ||||
| Public service | .143 | .350 | 0 | 1 |
| State-owned enterprise | .269 | .444 | 0 | 1 |
| Private enterprise | .333 | .471 | 0 | 1 |
| Social organization | .082 | .274 | 0 | 1 |
| Self-employed | .083 | .276 | 0 | 1 |
| Other | .037 | .189 | 0 | 1 |
| Unemployed | .053 | .224 | 0 | 1 |
| Marital status | ||||
| Single | .259 | .438 | 0 | 1 |
| Married | .718 | .450 | 0 | 1 |
| Divorced/widowed | .023 | .148 | 0 | 1 |
| Number of family members | 3.933 | 1.567 | 1 | 15 |
| Policy strictness | 4.326 | .933 | 1 | 5 |
| Self-infection | .020 | .141 | 0 | 1 |
| Family-infection | .032 | .176 | 0 | 1 |
Fig. 1.
Distribution of Subjective Distress about COVID-19 (IES-R Scores).
4.2. Results from Regression Analyses
Next, we conduct OLS regression analyses to examine the effects of social factors on subjective distress about COVID-19. The results from the regression models are presented in Table 3 . In Model 1, we include only major demographic variables. While gender and age show no significant effects, ethnicity, rural residence, and migrant status all display significant effects on subjective distress about COVID-19. Individuals of the Han ethnicity are significantly less distressed than those of other minority ethnicities. Rural residents display lower levels of distress than their urban counterparts. Migrants also show less distress, but the effect of migrant status disappears in the following models when socioeconomic status is taken into account.
Table 3.
Regression Analysis of Subjective Distress about COVID-19.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | |
|---|---|---|---|---|---|---|---|
| Gender (male) | .021 (.707) | -.320 (.747) | -.268 (.746) | -.420 (.746) | -.517 (.736) | ||
| Age | .022 (.038) | .024 (.042) | .029 (.046) | .043 (.047) | .061 (.046) | ||
| Ethnicity (Han) | -7.247⁎⁎⁎ (1.769) | -7.066⁎⁎⁎ (1.869) | -6.828⁎⁎⁎ (1.864) | -6.459⁎⁎ (1.863) | -4.918⁎⁎ (1.847) | -5.294⁎⁎ (1.750) | -.051⁎⁎ |
| Rural | -2.540⁎⁎ (.813) | -2.007* (.949) | -2.252* (.949) | -2.185* (.947) | -1.881* (.936) | -2.222⁎⁎ (.824) | -.047⁎⁎ |
| Migrant | -2.111⁎⁎ (.805) | -1.567 (.873) | -1.095 (.881) | -1.152 (.880) | -.867 (.869) | ||
| Education | .764* (.373) | .792* (.373) | .850* (.375) | .916* (.370) | .912⁎⁎ (.317) | .051⁎⁎ | |
| Income | .112 (.139) | .075 (.139) | .116 (.140) | .105 (.138) | |||
| Occupation | |||||||
| Public service | -.171 (1.979) | -.364 (1.975) | -.764 (1.975) | -.791 (1.950) | |||
| State-owned enterprise | .450 (1.866) | .339 (1.861) | .327 (1.858) | .385 (1.835) | |||
| Private enterprise | -.350 (1.792) | -.452 (1.788) | -.480 (1.785) | -.330 (1.763) | |||
| Social organization | 2.548 (2.104) | 2.066 (2.102) | 1.677 (2.102) | 1.508 (2.074) | |||
| Self-employed | 1.599 (2.095) | 1.119 (2.092) | 1.011 (2.089) | 1.334 (2.062) | |||
| Other | -1.924 (2.520) | -2.252 (2.512) | -2.549 (2.509) | -1.663 (2.479) | |||
| Marital status | |||||||
| Married | -.105 (1.001) | -.183 (1.000) | -.466 (.987) | ||||
| Divorced or widowed | 5.767* (2.602) | 5.393* (2.600) | 5.407* (2.566) | 5.293* (2.325) | .038* | ||
| Number of family members | 1.052⁎⁎⁎ (.240) | 1.025⁎⁎⁎ (.240) | .972⁎⁎⁎ (.237) | 1.062⁎⁎⁎ (.221) | .080⁎⁎⁎ | ||
| Policy strictness | -1.397⁎⁎ (.404) | -.866* (.404) | -.770* (.381) | -.033* | |||
| Self-infection | 6.938* (3.078) | 7.426* (2.975) | .050* | ||||
| Family-infection | 15.554⁎⁎⁎ (2.488) | 14.888⁎⁎⁎ (2.402) | .127⁎⁎⁎ | ||||
| Intercept | 27.493⁎⁎⁎ (2.184) | 24.691⁎⁎⁎ (3.101) | 19.859⁎⁎⁎ (3.278) | 24.656⁎⁎⁎ (3.554) | 18.836⁎⁎⁎ (3.563) | 20.370⁎⁎⁎ (2.720) | |
| R2 | .021 | .015 | .042 | .050 | .102 | .097 | .097 |
Notes: (1) numbers in parentheses are standard errors; (2) from 2-tailed tests, * P<.05; ** P<.01; *** P<.001; (3) the reference group for occupation is unemployed; (4) in Models 1-5 the reference group for marital status is single (never married), while in Model 6 and Model 7 the reference group for marital status becomes single (never married) and married; (5) Model 6 and Model 7 are the same regression model, with Model 6 reporting unstandardized coefficients and Model 7 reporting standardized coefficients.
In Model 2, we further incorporate socioeconomic variables including education, income, and a set of dummy variables representing various occupations with the unemployed as the reference group. The coefficient of education is significantly positive, indicating that more educated individuals are more prone to subjective distress. Income and occupation show no significant effects on subjective distress, though.
Model 3 adds individuals’ family variables including marital status and the number of family members living together. The single (never married) category is the reference group for marital status. Compared with single individuals, while married ones show no significant difference in subjective distress, divorced or widowed individuals are significantly more distressed. The coefficient of the number of family members is significantly positive, so living with more family members is significantly associated with a higher level of subjective distress.
In Model 4, we incorporate the strictness of the social measures against COVID-19 taken by the local community. Its coefficient is significantly negative so more strict measures reduce individuals’ subjective distress about COVID-19.
In Model 5, we further take into account the two variables measuring whether respondents and their family members were infected with COVID-19. Both variables show significantly positive effects. If one or their family members contracted COVID-19, they report significantly greater distress about COVID-19. Model 5 is the complete model that contains all the explanatory variables.
Instead of specifying a model with certain variables ex ante, we next apply the stepwise (forward) modeling procedure to the modeling. We model the process and let the stepwise model selection technique to select significant variables into the final model. This resultant model (Model 6) confirms the findings from the previous models. Significant influences on subjective distress about COVID-19 are identified in ethnicity, rural (versus urban) residence, education, being divorced or widowed (versus being single or married), the number of family members, the strictness of local measures against COVID-19, and infection with COVID-19 of oneself or their family members.
To compare the relative importance of these significant variables, we estimate another model that reports standardized coefficients. We first rescale all variables and transform them into standardized scores (with a mean of zero and a variance of one). Then we re-estimate Model 6 with these standardized variables. The results are presented in Model 7. Standardized variables are unit-free. By comparing standardized coefficients, we can examine which explanatory variables have greater effects. Among the significant variables, the effects of family members’ infection and the number of family members living together stand out, outranking all the other variables. Family appears to be particularly influential in shaping one's subjective distress about COVID-19.
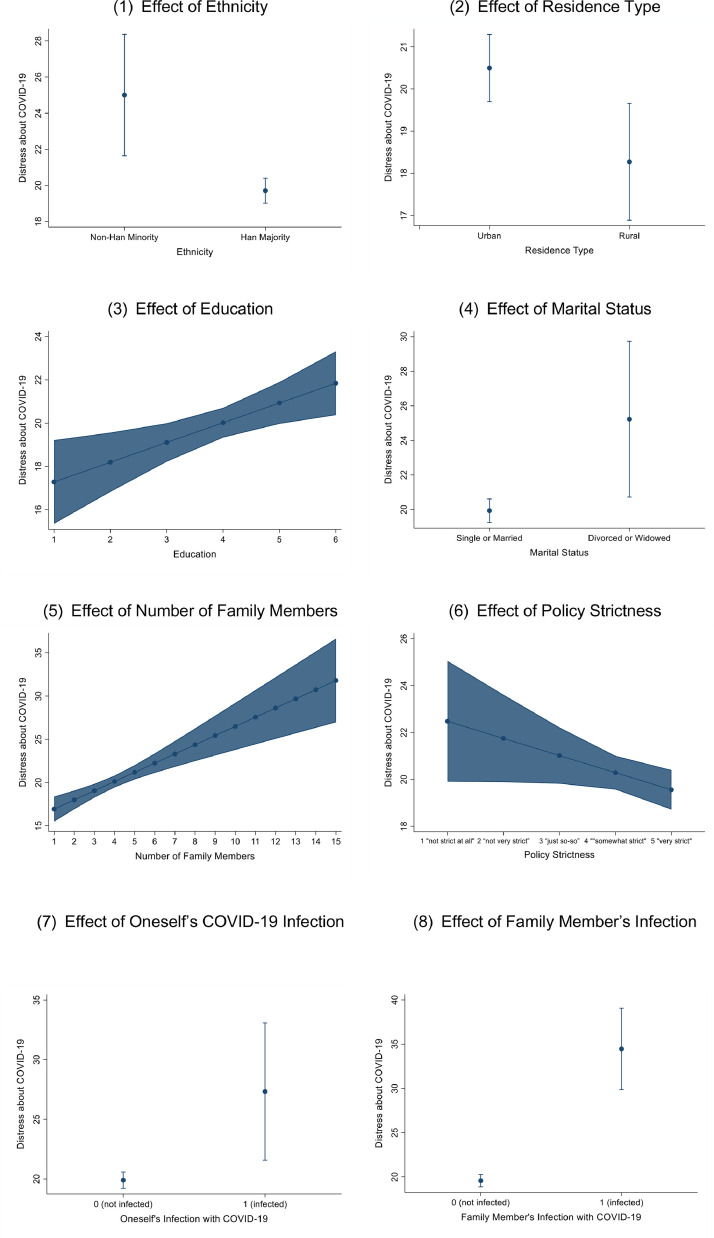
Based on Model 6 in Table 3, we calculate and visualize in Fig. 2 the significant influences on subjective distress (the IES-R score), when holding all other variables at their mean values.
Fig. 2.
Visualization of the Statistically Significant Effects (with 95% Confidence Intervals) on Subjective Distress about COVID-19 (IES-R Scores) Note: The figures are derived from Model 6 in Table 3 (with all other explanatory variables held at their mean values).
Fig. 2(1) compares the average distress score between the Han and the non-Han ethnical groups. When all other explanatory variables are held at their mean values, the average distress score of the Han group is 19.71, whereas that of the non-Han group is 25.01. This group difference is statistically significant.
Fig. 2(2) illustrates the average distress score between rural and urban residents. The average distress score is significantly higher among urban residents (20.50) than among rural residents (18.27).
Fig. 2(3) shows the distress-increasing effect of education on subjective distress. As one's education increases, the average distress score becomes significantly higher. For instance, individuals with only elementary school education or below (coded as 1) have an average distress score of 17.28, compared with an average score of 21.85 among those with postgraduate education (coded as 6).
Fig. 2(4) is the comparison of single or married individuals with divorced or widowed individuals. While the average distress score of the former group is 19.93, the average score of the latter group is as high as 25.22. There is a significant gap of more than 5 between the two groups.
Fig. 2(5) tracks the significant distress-increasing effect of family size. The average distress score is 16.93 for those living alone (i.e., the family size is 1), and it increases to 18.00, 20.12, 22.24, and 24.37 for those whose family size is 2, 4, 6, 8, respectively.
Fig. 2(6) visualizes how the average distress score changes with the strictness of the lockdown measures taken by the local community. The average distress score is significantly lower where the lockdown measures are stricter. When the lockdown measures are not strict at all (coded as 1), the average distress score is 22.48. In contrast, the average distress score is only 19.56 when the lockdown measures are very strict (coded as 5).
Fig. 2(7) displays the significant distress-increasing effect of the respondent being infected with COVID-19. When the respondent is not infected, the average distress score is 19.90, but the score is as high as 27.33 among those infected with the virus.
Fig. 2(8) depicts the significant distress-increasing effect of the respondent's family member being infected with COVID-19. Without anyone in the family being infected, the average distress score is 18.57. By comparison, the average distress score is as high as 34.46 for those who have someone infected with COVID-19 in their family.
5. Discussion and Conclusion
This study examined social influences, such as socioeconomic status, family structure, and social policy environment, on subjective distress associated with COVID-19 based on original survey data from China's hardest hit Hubei province. In terms of socioeconomic status, we find that the results are not always consistent with the general literature on social inequality in mental health. It is commonly believed that individuals with better education, more income, and more prestigious occupations have richer resources in coping with stress, so they are expected to report less distress (Chen et al., 2019; Fegert et al., 2020). Contrary to this expectation, our findings suggest that better educated individuals are actually more distressed. A possible explanation is that more educated individuals are more informed of the severity of the COVID-19 pandemic and thus feel greater distress. Income and occupation show no significant effect. These findings align with newly emerging evidence that higher socioeconomic status does not necessarily reduce people's distress about COVID-19 (O'Connell et al., 2020).
The results also find family to be among the most influential factors in shaping one's subjective distress about COVID-19. Divorced or widowed individuals are significantly more distressed than those who are single or married. Divorced and widowed family structure is particularly prone to greater subjective distress during the COVID-19 pandemic. Existing stress (stemming from going through a divorce or losing one's spouse) present in divorced or widowed families makes COVID-19 more distressing. The effects of family members’ infection and the number of family members living together are two most impactful influences, among all the variables analyzed. Those who are living with COVID-19-infected family members or with a large family have to take care of and worry about more people during the COVID-19 pandemic, which increases their psychological distress. Notably, family members’ infection with COVID-19 is even more stressful than one's own infection, according to the results. Additionally, COVID-19 spreads from person to person so those who live with infected family members or with a larger family have a greater chance of contracting the virus, which aggravates subjective distress. The high human-to-human transmissibility of COVID-19 puts individuals with a larger family into a greater danger of being infected, as they come into contact with more people (Van Bavel et al., 2020). Higher infection risks are associated with greater worries about COVID-19 (O'Connell et al., 2020). Hence, during the COVID-19 pandemic larger families may not necessarily reduce distress as they normally do in many other circumstances; to the contrary, they may elevate the risk and bring about greater subjective distress.
With respect to social policy environment, the results here show that the distress-reducing effect of stringent lockdown measures outstrips the distress-inducing effect. Strict measures close off local communities and disrupt normal social interactions. However, these measures promote people's confidence in the local community's efficacy in tackling the spread of the virus. Lockdown measures were employed and proved effective in previous epidemics, especially the 2013 SARS outbreak (Wilder-Smith, Chiew, and Lee, 2020). Moreover, these measures cut off interpersonal connections with the outside world and increase individuals’ perceived “remoteness” of COVID-19 from their community (Trope and Liberman, 2010; Zheng et al., 2020). The enhanced sense of security and the increased psychological distance from COVID-19 both reduce individuals’ subjective distress.
Although this analysis is conducted in the Chinese context based on a large dataset from Hubei province, the findings here contribute to our general understanding of mental health disparity across social groups during a public health crisis such as a pandemic. Certain groups are at a higher risk of negative mental health outcomes than others. First, higher socioeconomic status does not automatically provide better protection from psychological distress during a pandemic. There are usually health disparities resulting from socioeconomic inequalities in a society under normal circumstances (Fiscella and Williams, 2004). During a highly contagious pandemic, however, all socioeconomic groups face a universally challenging situation and higher socioeconomic status does not lessen people's worry about the prevalent health threat. Second, some family structures such as divorced and widowed families are particularly vulnerable to distress related to a pandemic. In addition, fast human-to-human transmission of a virus, which is a defining feature of a pandemic, potentially turns larger families, a source of more supportive resources in normal times, into a distress-inducing burden. Individuals with larger families and, in particular, those who have family members infected with the virus encounter more distressing challenges. Third, more and more countries or communities affected by a pandemic choose to take various quarantine and lockdown measures in order to prevent and contain the spread of the disease. Despite their disruptions of normal lifestyles and social connections, these measures actually have positive mental health effects such as an enhanced sense of protection and an increased psychological distance from the immediate danger, thereby lowering people's psychological distress. Their distress-reducing benefits outweigh their distress-inducing influences.
With the numbers of confirmed cases and deaths still surging, the COVID-19 pandemic continues posing a daunting challenge and causing significant disruptions to lives and communities around the globe. In this period of uncertainty and fear, it is likely that psychological distress will continue to grow and become more widespread. This study serves as a call for more data collection and empirical research to further advance our understanding about psychological well-being and its social correlates during this pandemic. In particular, we see three critical directions for this future research. First, research based on more representative data will help improve the reliability of statistical inferences and thus produce more generalizable knowledge. Second, cross-country comparisons can shed light on how COVID-19 induces distress differently under differing social contexts. The current literature on COVID-19 is often based on data from one country and cross-country studies will certainly be a valuable addition. Third, longitudinal data and research are better able to reveal the causal, rather than associational, relationship between social factors and COVID-19-related distress. Longitudinal studies will generate insight into how individuals with certain social characteristics develop distress over time. Taken together, only with a better understanding of the social correlates of COVID-19-related distress, can we be better equipped to alleviate the negative psychological effects of COVID-19.
Author contributions
Wei Guo acquired funding. Min Zhou and Wei Guo designed the study, analyzed the data, and wrote the manuscript. Wei Guo and Min Zhou have approved the final manuscript.
Conflict of Interest
None to declare.
Acknowledgements
None.
Footnotes
This work was supported by the National Social Science Fund of China (NSSFC) under Grant No. 20VYJ039, the National Natural Science Foundation of China under Grant No. 71921003, the Insight Grant from the Social Sciences and Humanities Research Council (SSHRC) of Canada, and the Early Career Lansdowne Scholar Award from the University of Victoria. The authors thank Professor Ping Fu, the dean of the School of Sociology of Central China Normal University, who generously share the data with us. Direct all correspondence to Wei Guo, Department of Social Work and Social Policy, School of Social and Behavioral Sciences, Nanjing University, Jiangsu Province, 210023, P. R. China.
The numbers of confirmed cases and deaths in Hubei province account for more than 80% and more than 95% of China's totals, respectively, as of August 2020. There are also large disparities in mortality rates between Wuhan (>3%), different regions of Hubei province (about 2.9% on average), and across the other provinces of China (about 0.7% on average) (Ji et al., 2020).
The effect of age on subjective distress may not be linear but curvilinear (Jorm, 2000) so we also tried a quadratic term of age (or age-squared) in the regression model which showed no significant effect.
References
- Adler N.E., Newman K. Vol. 21. Health Affairs; 2002. pp. 60–76. (Socioeconomic disparities in health: Pathways and policies). [DOI] [PubMed] [Google Scholar]
- Ahmed F., Zviedrite N., Uzicanin A. Effectiveness of workplace social distancing measures in reducing influenza transmission: A systematic review. BMC Public Health. 2018;18(1):518. doi: 10.1186/s12889-018-5446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albrecht T.L., Goldsmith D.J. Lawrence Erlbaum Associates Publishers; New Jersey: 2003. Social support, social networks, and health. In T. L. Thompson, A. M. Dorsey, K. I. Miller, and R. Parrott (Eds.), Handbook of health communication (p. 263-284) [Google Scholar]
- Backer J.A., Klinkenberg D., Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance. 2020 doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry V., Stout M.E., Lynch M.E., Mattis S., Tran D.Q., Antun A., Kempton C.L. The effect of psychological distress on health outcomes: A systematic review and meta-analysis of prospective studies. Journal of Health Psychology. 2020;25(2):227–239. doi: 10.1177/1359105319842931. [DOI] [PubMed] [Google Scholar]
- Bauer L.L., Seiffer B., Deinhart C., Atrott B., Sudeck G., Hautzinger M., Wolf S. Associations of exercise and social support with mental health during quarantine and social-distancing measures during the COVID-19 pandemic: A cross-sectional survey in Germany. medRxiv. 2020 doi: 10.1101/2020.07.01.20144105. [DOI] [Google Scholar]
- Beck J.G., Grant D.M., Read J.P., Clapp J.D., Coffey S.F., Miller L.M., Palyo S.A. The Impact of Event Scale – Revised: Psychometric properties in a sample of motor vehicle accident survivors. Journal of Anxiety Disorders. 2008;22(2):187–198. doi: 10.1016/j.janxdis.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostean G., Andrade F.C.D., Viruell-Fuentes E.A. Neighborhood stressors and psychological distress among US Latinos: Measuring the protective effects of social support from family and friends. Stress and Health. 2019;35(2):115–126. doi: 10.1002/smi.2843. [DOI] [PubMed] [Google Scholar]
- Brown S.L., Manning W., Stykes J.B. Family structure and child well-being: Integrating family complexity. Journal of Marriage and Family. 2015;77(1):177–190. doi: 10.1111/jomf.12145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet A., St-Hilaire A., Jehel L., King S. Validation of the French version of the Impact of Event Scale – Revised. Canadian Journal of Psychiatry. 2002;20:174–182. doi: 10.1177/070674370304800111. [DOI] [PubMed] [Google Scholar]
- Cano A., Scaturo D.J., Sprafkin R.P., Lantinga L.J., Fiese B.H., Brand F. Family support, self-rated health, and psychological distress. Primary Care Companion to The Journal of Clinical Psychiatry. 2003;5(3):111–117. doi: 10.4088/pcc.v05n0302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer D. Social support and psychological distress in women and men. British Journal of Medical Psychology. 1991;64(2):147–158. doi: 10.1111/j.2044-8341.1991.tb01652.x. [DOI] [PubMed] [Google Scholar]
- Chen R., Kessler R.C., Sadikova E., NeMoyer A., Sampson N.A., Alvarez K., Alegría M. Racial and ethnic differences in individual-level and area-based socioeconomic status and 12-month DSM-IV mental disorders. Journal of Psychiatric Research. 2019;119:48–59. doi: 10.1016/j.jpsychires.2019.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Yang J., Yang W., Wang C., Bärnighausen T. COVID-19 control in China during mass population movements at New Year. The Lancet. 2020;395(10226):764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockerham W.C. A test of the relationship between race, socioeconomic status, and psychological distress. Social Science & Medicine. 1990;31(12):1321–1326. doi: 10.1016/0277-9536(90)90071-y. [DOI] [PubMed] [Google Scholar]
- Compton M.T., Thompson N.J., Kaslow N.J. Social environment factors associated with suicide attempt among low-income African Americans: The protective role of family relationships and social support. Social Psychiatry and Psychiatric Epidemiology. 2005;40(3):175–185. doi: 10.1007/s00127-005-0865-6. [DOI] [PubMed] [Google Scholar]
- Creamer M., Bell R., Failla S. Psychometric properties of the Impact of Event Scale – Revised. Behavior Research and Therapy. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Dandekar, R., and Barbastathis, G. 2020. Neural Network aided quarantine control model estimation of COVID spread in Wuhan, China. arXiv preprint arXiv:2003.09403.
- Donev D. Hans Jacobs Publishing Company; Lage: 2005. Social networks and social support as determinants of health. In: Georgieva L, Burazeri G (Eds), Health determinants in the scope of new public health: Handbook for teachers, researchers and health professionals (pp. 531-548) [Google Scholar]
- Douglas M., Katikireddi S.V., Taulbut M., McKee M., McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369 doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A.G., Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health. 2020;14:1–11. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández R.S., Crivelli L., Guimet N.M., Allegri R.F., Pedreira M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. Journal of Affective Disorders. 2020;277:75–84. doi: 10.1016/j.jad.2020.07.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K., Williams D.R. Health disparities based on socioeconomic inequities: implications for urban health care. Academic Medicine. 2004;79(12):1139–1147. doi: 10.1097/00001888-200412000-00004. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Drawve G., Harris C. Facing new fears during the COVID-19 pandemic: The State of America's mental health. Journal of Anxiety Disorders. 2020;75 doi: 10.1016/j.janxdis.2020.102291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan Y., Ma J., Wu J., Chen Y., Zhu H., Hall B.J. Immediate and delayed psychological effects of province-wide lockdown and personal quarantine during the COVID-19 outbreak in China. Psychological Medicine. 2020 doi: 10.1017/S0033291720003116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green S.B. How many subjects does it take to do a regression analysis? Multivariate Behavioral Research. 1991;26(3):499–510. doi: 10.1207/s15327906mbr2603_7. [DOI] [PubMed] [Google Scholar]
- Heymann D.L. Data sharing and outbreaks: Best practice exemplified. The Lancet. 2020;395(10223):469–470. doi: 10.1016/S0140-6736(20)30184-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huynh T.L.D. Does culture matter social distancing under the COVID-19 pandemic? Safety Science. 2020;130 doi: 10.1016/j.ssci.2020.104872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaja I.F., Anyanwu M.U., Iwu Jaja C.J. Social distancing: How religion, culture and burial ceremony undermine the effort to curb COVID-19 in South Africa. Emerging Microbes & Infections. 2020;9(1):1077–1079. doi: 10.1080/22221751.2020.1769501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jetten J., Haslam C., Haslam S.A. Taylor and Francis; Oxford, United Kingdom: 2011. The social cure: Identity, health and wellbeing. [Google Scholar]
- Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. The Lancet Global Health. 2020;8(4):e480. doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm A. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychological Medicine. 2000;30(1):11–22. doi: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- Kawachi I., Berkman L.F. Social ties and mental health. Journal of Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C. A disaggregation of the relationship between socioeconomic status and psychological distress. American Sociological Review. 1982;47(6):752–764. [PubMed] [Google Scholar]
- Kosidou K., Dalman C., Lundberg M., Hallqvist J., Isacsson G., Magnusson C. Socioeconomic status and risk of psychological distress and depression in the Stockholm Public Health Cohort: A population-based study. Journal of Affective Disorders. 2011;134(1-3):160–167. doi: 10.1016/j.jad.2011.05.024. [DOI] [PubMed] [Google Scholar]
- Liu Y.C., Kuo R.L., Shih S.R. COVID-19: The first documented coronavirus pandemic in history. Biomedical Journal. 2020 doi: 10.1016/j.bj.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada-Baltar A., Jiménez-Gonzalo L., Gallego-Alberto L., Pedroso-Chaparro M.D.S., Fernandes-Pires J., Márquez-González M. “We're staying at home”. Association of self-perceptions of aging, personal and family resources and loneliness with psychological distress during the lock-down period of COVID-19. The Journals of Gerontology: Series B. 2020 doi: 10.1093/geronb/gbaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malone C., Wachholtz A. The relationship of anxiety and depression to subjective well-being in a mainland Chinese sample. Journal of Religion and Health. 2018;57(1):266–278. doi: 10.1007/s10943-017-0447-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchand A., Demers A., Durand P. Do occupation and work conditions really matter? A longitudinal analysis of psychological distress experiences among Canadian workers. Sociology of Health & Illness. 2005;27(5):602–627. doi: 10.1111/j.1467-9566.2005.00458.x. [DOI] [PubMed] [Google Scholar]
- Marchiori, M. 2020. COVID-19 and the social distancing paradox: Dangers and solutions. arXiv:2005.12446v1. https://arxiv.org/abs/2005.12446v1.
- Massé R., Poulin C., Dassa C., Lambert J., Bélair S., Battaglini A. The structure of mental health: Higher-order confirmatory factor analyses of psychological distress and well-being measures. Social Indicators Research. 1998;45(1-3):475–504. [Google Scholar]
- Mei C. Policy style, consistency and the effectiveness of the policy mix in China's fight against COVID-19. Policy and Society. 2020;39(3):309–325. doi: 10.1080/14494035.2020.1787627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connell, K., Berluti, K., Rhoads, S. A., and Marsh, A. 2020. Reduced social distancing during the COVID-19 pandemic is associated with antisocial behaviors in an online United States sample. https://doi.org/10.31234/osf.io/ezypg. [DOI] [PMC free article] [PubMed]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross C.E., Van Willigen M. Education and the subjective quality of life. Journal of Health and Social Behavior. 1997;38(3):275–297. [PubMed] [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety and perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sancakoğlu S., Sayar M.K. Relation between socioeconomic status and depression, anxiety, and self-esteem in early adolescents. Yeni Symposium. 2012;50(4):207–220. [Google Scholar]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM: An International Journal of Medicine. 2020 doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. Jama. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- Shanahan L., Steinhoff A., Bechtiger L., Murray A.L., Nivette A., Hepp U., Eisner M. Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine. 2020 doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavers V.L. Measurement of socioeconomic status in health disparities research. Journal of the National Medical Association. 2007;99(9):1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Sibley C.G., Greaves L.M., Satherley N., Wilson M.S., Overall N.C., Lee C.H., Houkamau C.A. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. American Psychologist. 2020;75(5):618–630. doi: 10.1037/amp0000662. [DOI] [PubMed] [Google Scholar]
- Sullivan M.J.L., Thibault P., Simmonds M.J., Milioto M., Cantin A-P., Velly A.M. Pain, perceived injustice and the persistence of post-traumatic stress symptoms during the course of rehabilitation for whiplash injuries. PAIN. 2009;145:325–331. doi: 10.1016/j.pain.2009.06.031. [DOI] [PubMed] [Google Scholar]
- Trope Y., Liberman N. Construal-level theory of psychological distance. Psychological Review. 2010;117(2):440–463. doi: 10.1037/a0018963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K., Richmond J.R., Rose J.P., Gratz K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Research. 2020 doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher K., Durkin J., Bhullar N. The COVID-19 pandemic and mental health impacts. International Journal of Mental Health Nursing. 2020;29(3):315–318. doi: 10.1111/inm.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallas S.P., Finlay W., Warton A.S. Oxford University Press; 2009. New Sociology of Work: Structures and Inequalities. [Google Scholar]
- Van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Drury J. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020 doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Weiss D.S., Marmar C.R. Guilford Press; New York: 1997. “The impact of event scale – revised.” Pp. 399-411 in Assessing Psychological Trauma and PTSD, edited by Wilson, J. P. and Keane, T. M. [Google Scholar]
- Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? The Lancet Infectious Diseases. 2020;20(5):e102–e107. doi: 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson VanVoorhis C.R., Morgan B.L. Understanding power and rules of thumb for determining sample sizes. The Quantitative Methods for Psychology. 2007;3(2):43–50. [Google Scholar]
- World Health Organization. 2020. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020 (No. WHO/2019-nCoV/MentalHealth/2020.1). World Health Organization.
- Xie K., Liang B., Dulebenets M.A., Mei Y. The impact of risk perception on social distancing during the COVID-19 pandemic in China. International Journal of Environmental Research and Public Health. 2020;17(17):6256. doi: 10.3390/ijerph17176256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Zeng Z., Wang K., Wong S.S., Liang W., Zanin M., Liang J. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. Journal of Thoracic Disease. 2020;12(3):165–174. doi: 10.21037/jtd.2020.02.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W., Chen H., Feng Q. Education and psychological distress of older Chinese: Exploring the longitudinal relationship and its subgroup variations. Journal of Aging and Health. 2015;27(7):1170–1198. doi: 10.1177/0898264315577589. [DOI] [PubMed] [Google Scholar]
- Zheng L., Miao M., Lim J., Li M., Nie S., Zhang X. Is lockdown bad for social anxiety in COVID-19 regions? A national study in the SOR perspective. International Journal of Environmental Research and Public Health. 2020;17(12):4561. doi: 10.3390/ijerph17124561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou M., Guo W. Social Factors and Worry Associated with COVID-19: Evidence from a Large Survey in China. Social Science & Medicine. 2021;277113934 doi: 10.1016/j.socscimed.2021.113934. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]