Abstract
PURPOSE:
To determine whether emergency department (ED) visit history prior to cancer diagnosis is associated with ED visit volume after cancer diagnosis.
METHODS:
This was a retrospective cohort study of adults (≥ 18 years) with an incident cancer diagnosis (excluding nonmelanoma skin cancers or leukemia) at an academic medical center between 2008 and 2018 and a safety-net hospital between 2012 and 2016. Our primary outcome was the number of ED visits in the first 6 months after cancer diagnosis, modeled using a multivariable negative binomial regression accounting for ED visit history in the 6-12 months preceding cancer diagnosis, electronic health record proxy social determinants of health, and clinical cancer-related characteristics.
RESULTS:
Among 35,090 patients with cancer (49% female and 50% non-White), 57% had ≥ 1 ED visit in the 6 months immediately following cancer diagnosis and 20% had ≥ 1 ED visit in the 6-12 months prior to cancer diagnosis. The strongest predictor of postdiagnosis ED visits was frequent (≥ 4) prediagnosis ED visits (adjusted incidence rate ratio [aIRR]: 3.68; 95% CI, 3.36 to 4.02). Other covariates associated with greater postdiagnosis ED use included having 1-3 prediagnosis ED visits (aIRR: 1.32; 95% CI, 1.28 to 1.36), Hispanic (aIRR: 1.12; 95% CI, 1.07 to 1.17) and Black (aIRR: 1.21; 95% CI, 1.17 to 1.25) race, homelessness (aIRR: 1.95; 95% CI, 1.73 to 2.20), advanced-stage cancer (aIRR: 1.30; 95% CI, 1.26 to 1.35), and treatment regimens including chemotherapy (aIRR: 1.44; 95% CI, 1.40 to 1.48).
CONCLUSION:
The strongest independent predictor for ED use after a new cancer diagnosis was frequent ED visits before cancer diagnosis. Efforts to reduce potentially avoidable ED visits among patients with cancer should consider educational initiatives that target heavy prior ED users and offer them alternative ways to seek urgent medical care.
INTRODUCTION
The literature on frequent emergency department (ED) use among the general patient population largely focuses on clinical characteristics (eg, mental health conditions)1-3 and indicators of social disadvantage (eg, social determinants of health [SDH])4 as predictors of ED use. Currently, health care systems largely rely on patients to triage the severity and urgency of their illness when they get sick and decide between going to the ED versus less expensive alternative sites of care, something patients may be ill-equipped to judge.
How to decide when and where to seek acute care when sick is even more challenging for patients with cancer. Adults newly diagnosed with cancer frequently visit the ED for nonemergent conditions because of side effects of their treatment and/or symptoms related to their underlying disease.5-10 This problem may be exacerbated by warnings to be alert to seemingly minor changes in condition: between 15% and 22% of patients with cancer have two or more ED visits made within 180 days of diagnosis.5,11
Even privately insured patients encounter administrative barriers in accessing timely, appropriate-site, and appropriate-specialty care.12 It follows that patients who have had poor prior experiences receiving a timely and complete evaluation in outpatient settings might learn to use the ED as a primary source of care. Other patients may not have enough health system savvy from the outset to be aware of and seek out less costly sites of acute care.
For a population-based cohort of patients with cancer in two health systems, we used longitudinally linked ED visits, including visits preceding the cancer diagnosis, to predict the factors influencing ED visits in the 6 months after a new cancer diagnosis. We hypothesized that ED visits post–cancer diagnosis would be associated with their pre–cancer diagnosis ED visit patterns, independent of other known drivers of acute care such as cancer- and treatment-related characteristics and SDH.
METHODS
Study Design, Population, and Setting
We conducted a retrospective analysis of comprehensive, longitudinally linked ED encounters from a regional health information exchange, the Dallas-Fort Worth Hospital Council Foundation (Foundation), which contains information on ED visits to > 80 hospitals in North Texas (all the nonfederal hospitals in a 100-mile radius of Dallas). We evaluated predictors of ED visits after a new cancer diagnosis across two different patient populations: patients with cancer treated at the University of Texas Southwestern Medical Center (University) and at the Parkland Health & Hospital System (Parkland), the safety-net integrated health system for Dallas County. We included patients who had an incident cancer diagnosis between 2008 and 2018 among the University population and between 2012 and 2016 among the Parkland population. For patients with synchronous diagnoses, we selected the highest-stage cancer. For patients with metachronous cancer diagnoses, we selected the first diagnosis and excluded subsequent diagnoses. We excluded patients with only nonmelanoma skin cancer because of lower ED use overall. We also excluded patients with leukemia because of prolonged inpatient stays for acute leukemia and frequent hospitalizations for relapse of disease,13 which make post–cancer diagnosis ED use difficult to compare with other cancers within a 6-month window.
Parkland is the primary provider of care for the under- and uninsured in Dallas County and is the sole provider of cancer care for the uninsured in the region. However, Parkland patients do visit EDs at other hospitals, which may not be captured by any single health system electronic health record (EHR). Among our University population, we have also found that two thirds of ED visits are made to other health systems and are not captured by the local EHR.14 Both health systems use the same EHR vendor (Epic, Verona, WI). Some University faculty physicians supervise trainees at Parkland, but the clinic staff providing acute care triage are exclusive to each health system. We linked patients from local cancer registries to the regional Foundation database, which collects information for approximately 12 million unique patients and their 65 million hospital encounters. Visit-level data are organized into a master patient index that assigns a unique identifier, allowing longitudinal tracking of patients over time to all hospitals in the Foundation database.
Using a combination of name, date of birth, zip code of residence, and medical record number, we matched patients to their unique Foundation identifiers. The Foundation database provided dates of ED arrival and discharge, name of hospital and health system, and discharge disposition (including died in ED, transferred to another hospital, observation stay, inpatient admission, and discharged home).
Outcome
Our primary outcome was the number of ED visits in the first 6 months (180 days) after a new diagnosis of cancer. ED visits that resulted in the initial pathology-confirmed cancer diagnosis were excluded.
Covariates
Our primary prespecified predictor of interest was ED use prior to cancer diagnosis, which we defined as the number of ED visits 6-12 months (181-365 days) before diagnosis. We categorized this variable as zero visits, 1-3 visits, or ≥ 4 visits. To be conservative, we did not use ED visits in the 0-6 months immediately before diagnosis, as they could potentially reflect early symptoms of the subsequently diagnosed cancer.
We prespecified additional predictors of postdiagnosis ED visits on the basis of our team's multidisciplinary expertise and from prior literature that were available in the EHR. These included a set of previously validated SDH variables (race and/or ethnicity, non–English language preference, insurance type at time of diagnosis, and homelessness),3,15-19 comorbidities at diagnosis (organized into Charlson Comorbidity Index),20,21 and clinical cancer-specific characteristics obtained from local cancer registries maintained by health systems that are Commission on Cancer-designated Academic Comprehensive Care, and National Cancer Institute-designated Comprehensive Cancer Programs (cancer type, whether advanced stage at diagnosis, and initial treatment modalities [chemotherapy, radiation therapy, surgery, and/or immunotherapy]).5,22 We categorized a patient as homeless if their address was listed as homeless shelter in the EHR at any point between 1 year (365 days) before or 6 months (180 days) after cancer diagnosis or if they received care with the homeless health care program during that period. Advanced stage was defined as stage IIIB or higher for lung cancer, stage III or higher for pancreatic cancer, and stage IV for all others except for brain cancer.5,23 Because our overall cohort consisted of patients from two distinct health systems spanning different time periods, we included the patient's health system (University or Parkland) and year of cancer diagnosis as covariates. The model was also adjusted for age, sex, and whether the patient died within 6 months (180 days) after cancer diagnosis.
Statistical Analysis
We first grouped ED visits and ED visit history into a patient-level data set and used descriptive statistics to characterize the patient cohort. Next, we applied a multivariable negative binomial regression to model the number of ED visits within the first 6 months after a new cancer diagnosis. We chose negative binomial regression because of overdispersion of the outcome variable. For improved interpretability, we used marginal effects methods to estimate adjusted postdiagnosis ED visit counts across key strata of interest.24
Sensitivity Analyses
To assess the robustness of our findings, we conducted a series of sensitivity analyses for the University and Parkland cohorts separately. First, we reran our analyses for each health system cohort separately. For both cohorts, we repeated analyses with (1) ED visit history 12-18 months prior to cancer diagnosis as the primary predictor, (2) added interaction terms between initial treatment modalities and cancer stage at diagnosis, (3) neighborhood education level included as a binary covariate (low v not low), and (4) excluded pre– and post–cancer diagnosis ED visits that resulted in hospitalization.
For the University cohort, we repeated analyses with neighborhood poverty level included as a binary covariate (high v not high). This was not done for the Parkland cohort because many patients were enrolled in low-income insurance programs at the county (charity assistance) or state level (Medicaid). We used validated measures to characterize census tracts as low education (≥ 25% of individuals older than age 25 years did not graduate high school) or high poverty (≥ 10% of households below poverty level).25-27
For the Parkland cohort, we repeated analyses with the addition of whether the patient listed a missing or nonsensical social security number as a proxy for undocumented immigration status as we hypothesized this could influence ED utilization. Social security numbers were not reliably identifiable in the University EHR.
Statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC) and Stata/SE 15.0 (StataCorp, College Station, TX). The University of Texas Southwestern Medical Center institutional review board approved this study (STU 112017-026 and 122017-042).
RESULTS
Patient Characteristics
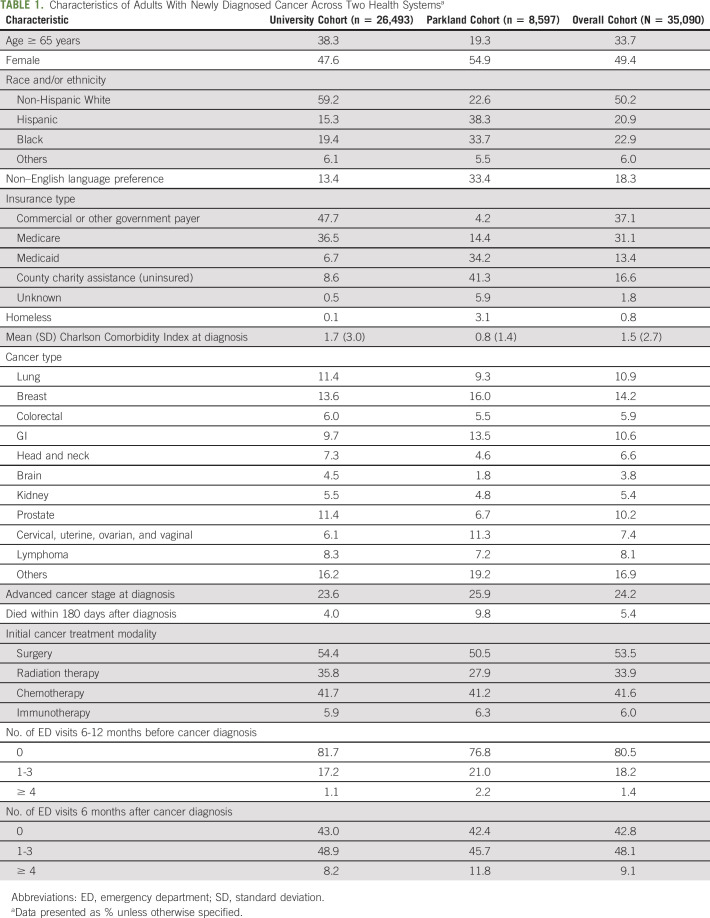
We matched 35,090 patients from the University and Parkland cancer registries to the Foundation database. Half (49.4%) were female, one-third (33.7%) were ≥ 65 years old, 18.3% had a non–English language preference, 30.0% were uninsured or enrolled in Medicaid at the time of diagnosis, and 0.8% were homeless. The most common cancers were breast (14.2%), lung (10.9%), GI (10.6%), prostate (10.2%), and colorectal (5.9%). Overall, one quarter (24.2%) of individuals had advanced-stage cancer at diagnosis, 41.6% had initial treatment regimens that included chemotherapy, and 5.4% died within 6 months after diagnosis.
More than half of the cohort (57.2%) had at least one ED visit in the 6 months after cancer diagnosis, whereas one-fifth (19.5%) had at least one ED visit in the 6-12 months prior to cancer diagnosis. Complete demographics, cancer-related characteristics, and ED visit counts are shown in Table 1.
TABLE 1.
Characteristics of Adults With Newly Diagnosed Cancer Across Two Health Systemsa
Predictors of ED Visits After Cancer Diagnosis
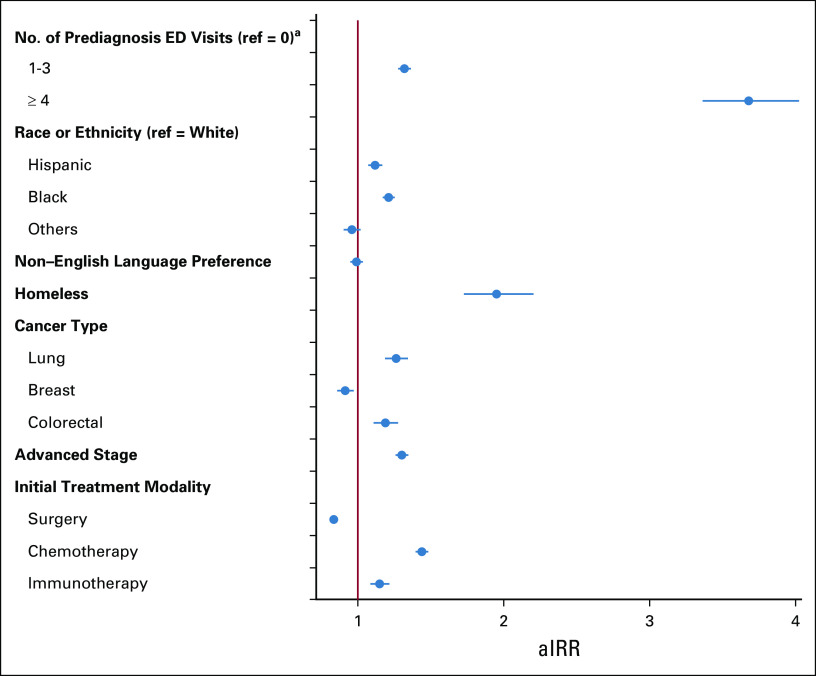
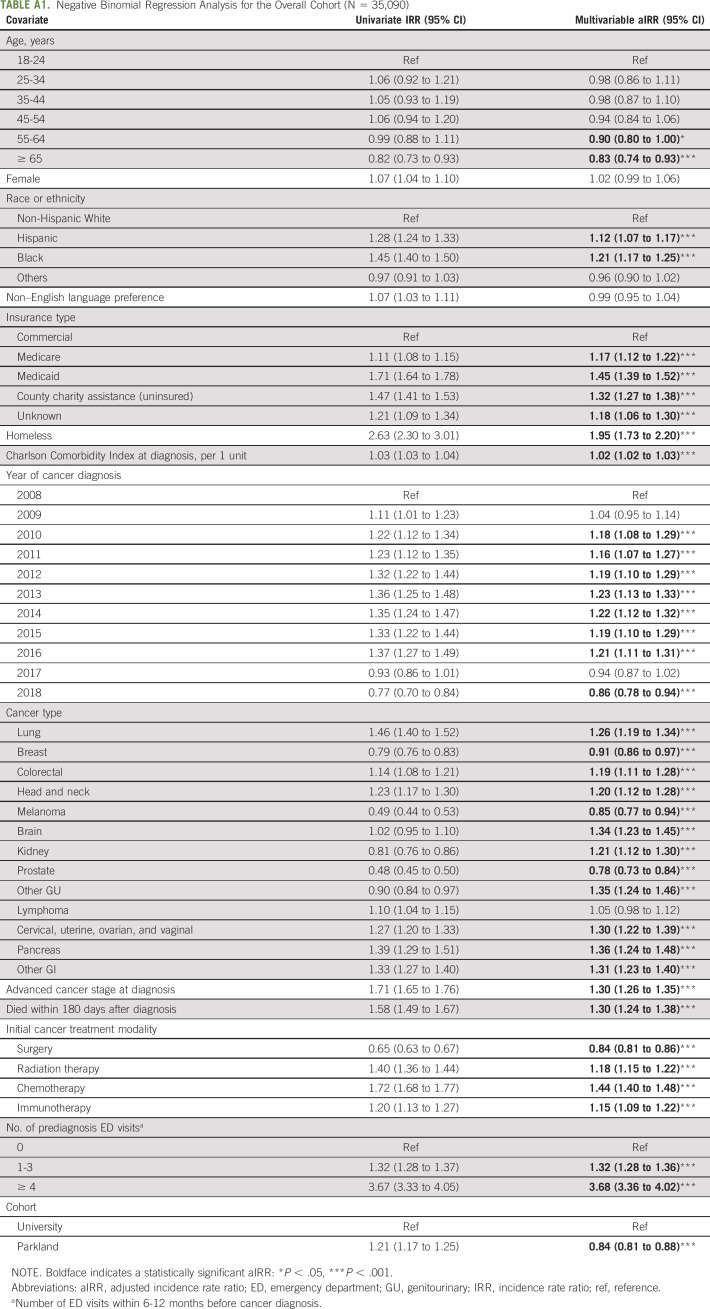
In our multivariable adjusted regression analysis, the strongest independent predictor of postdiagnosis ED visits was frequent (≥ 4) prediagnosis ED visits (adjusted incidence rate ratio [aIRR]: 3.68; 95% CI, 3.36 to 4.02) (Fig 1, Appendix Table A1, online only). Patients with 1-3 prediagnosis ED visits also had more ED visits following cancer diagnosis, although to a lesser extent (aIRR: 1.32; 95% CI, 1.28 to 1.36).
FIG 1.
Key predictors of number of ED visits 6 months after cancer diagnosis. Shown are incidence rate ratios and 95% CIs of ED visits within 6 months after cancer diagnosis generated from a multivariable negative binomial regression adjusted for health system (Parkland v University), age, sex, race and/or ethnicity, language preference, insurance type, homelessness, Charlson Comorbidity Index at time of diagnosis, year of cancer diagnosis, cancer type, advanced cancer stage at diagnosis, death within 6 months of diagnosis, and initial cancer treatment modalities. Full model results are shown in Appendix Table A1. aNumber of ED visits within 6-12 months before cancer diagnosis. aIRR, adjusted incidence rate ratio; ED, emergency department; ref, reference.
SDH variables associated with greater postdiagnosis ED use included Hispanic (aIRR: 1.12; 95% CI, 1.07 to 1.17) and Black (aIRR: 1.21; 95% CI, 1.17 to 1.25) race and/or ethnicity, Medicaid (aIRR: 1.45; 95% CI, 1.39 to 1.52) and county charity assistance (aIRR: 1.32; 95% CI, 1.27 to 1.38) insurance types, and homelessness (aIRR: 1.95; 95% CI, 1.73 to 2.20). Non–English language preference was not significantly associated with postdiagnosis ED visits.
Among the clinical covariates, we observed greater postdiagnosis ED use for individuals with lung cancer (aIRR: 1.26; 95% CI, 1.19 to 1.34) and colorectal cancer (aIRR: 1.19; 95% CI, 1.11 to 1.28), advanced-stage cancer at diagnosis (aIRR: 1.30; 95% CI, 1.26 to 1.35), and initial treatment regimens that included chemotherapy (aIRR: 1.44; 95% CI, 1.40 to 1.48). Breast cancer was associated with fewer postdiagnosis ED visits (aIRR: 0.91; 95% CI, 0.86 to 0.97). Full model results for the overall cohort are shown in Appendix Table A1. Appendix Tables A2 and A3 (online only) contain full model results stratified by health system.
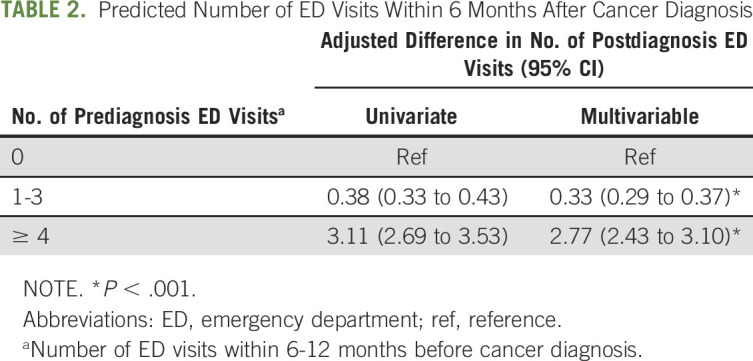
Marginally Adjusted ED Visit Counts
In our adjusted marginal effects analysis, patients with infrequent (1-3) and frequent (≥ 4) prediagnosis ED visits had 0.33 (95% CI, 0.29 to 0.37) and 2.77 (95% CI, 2.43 to 3.10) more postdiagnosis ED visits, respectively, than patients with zero prediagnosis ED visits (Table 2).
TABLE 2.
Predicted Number of ED Visits Within 6 Months After Cancer Diagnosis
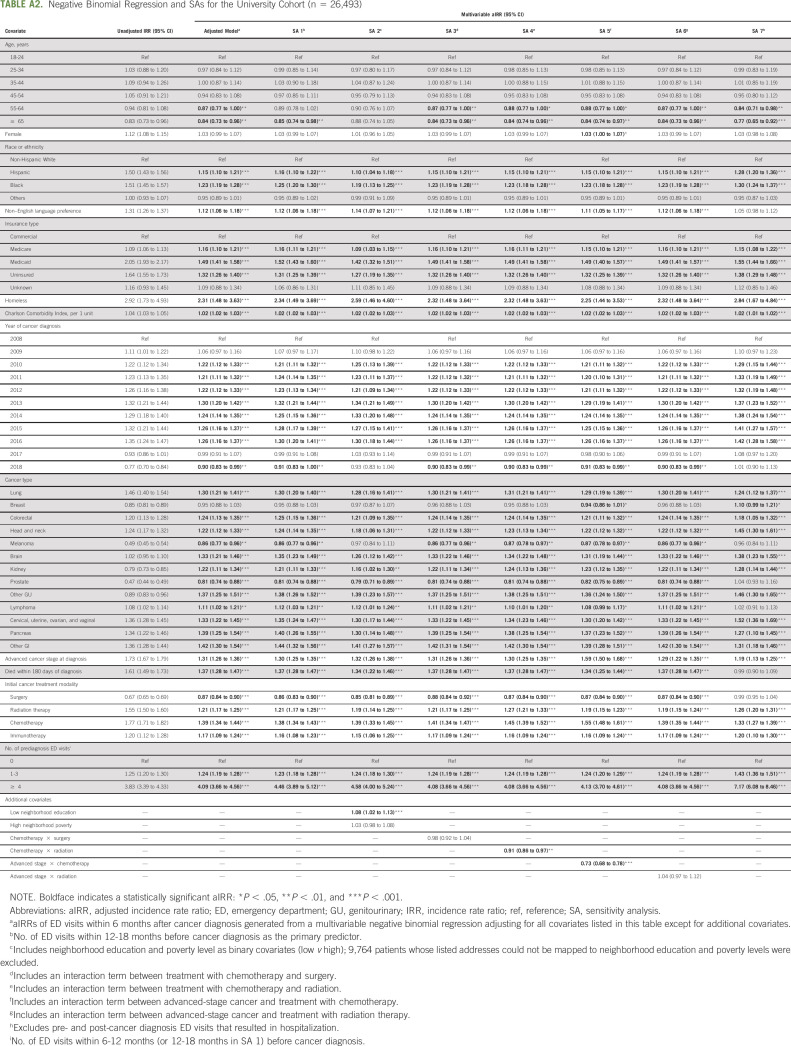
Sensitivity Analyses
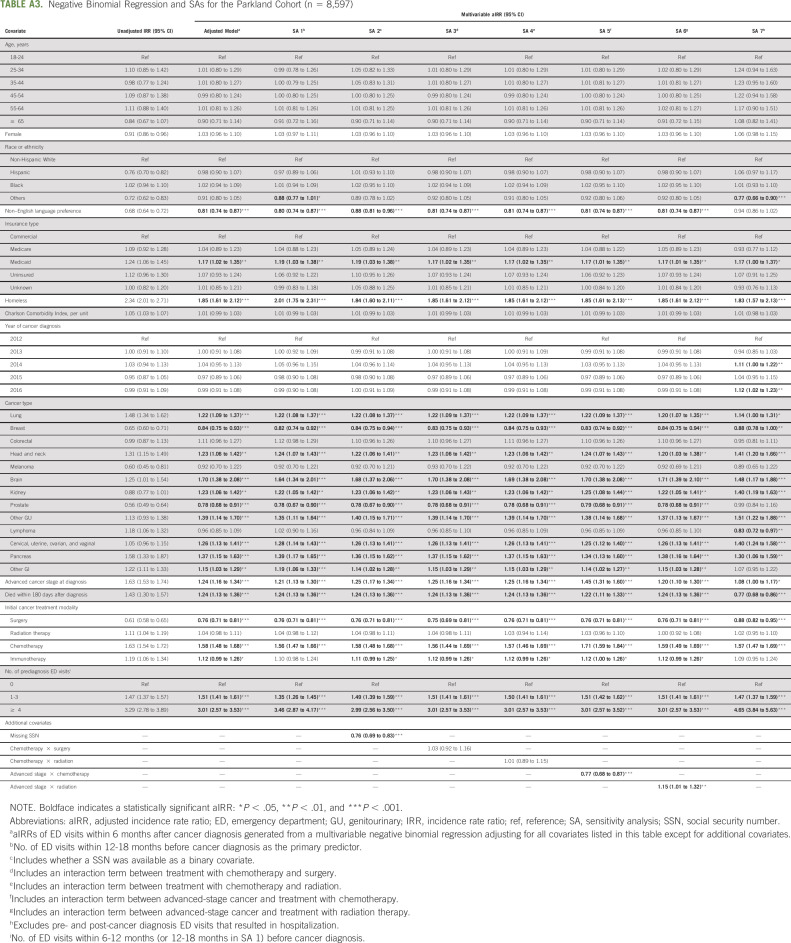
Our findings were not substantively changed when modeled for the two health system cohorts separately, nor in sensitivity analyses that (1) used ED visit history 12-18 months prior to cancer diagnosis as the primary predictor, (2) included interaction terms between initial treatment modalities and cancer stage, (3) adjusted for neighborhood education level, (4) excluded pre– and post–cancer diagnosis ED visits that resulted in hospitalization, (5) adjusted for neighborhood poverty level, and (6) adjusted for whether a social security number was missing in the EHR. See Appendix Tables A2 and A3 for complete sensitivity analysis results.
DISCUSSION
In this retrospective analysis of 35,090 adults with newly diagnosed cancer across two health systems with diverse populations, we identified a strong association between ED use before cancer diagnosis and ED use after cancer diagnosis. Patients with frequent (≥ 4) ED visits in the 6 months prior to cancer diagnosis averaged nearly three more postdiagnosis ED visits than patients with zero prediagnosis ED visits. Our estimates are likely conservative because we excluded ED visits in the 6 months leading up to cancer diagnosis. Furthermore, our results were robust to a number of sensitivity analyses. We also confirmed known risk factors of postdiagnosis ED visits such as minority race and/or ethnicity, homelessness, advanced-staged cancer, and treatment regimens including chemotherapy and radiation therapy.28-30
Our most practice- and policy-relevant finding is the strength of a patient's prior ED visit history in predicting ED visits in the first 6 months after an incident cancer diagnosis. Adding to prior studies that identified prior acute care use as a predictor of acute care use after initiation of chemotherapy or radiation therapy,29-33 our study sampled a diverse population of patients (half non-White), including patients without insurance and who had not undergone chemotherapy or radiation therapy, and accounted for SDH variables. Frequent prediagnosis ED visits was by far the strongest predictor of postdiagnosis ED visit volume, with a predictive impact that nearly doubled those of the strongest clinical or SDH predictors. Recognizing that sociodemographic and cancer-related factors are often beyond the control of a patient or health system, and that many ED visits may be clinically necessary, frequent prediagnosis ED use may be a marker for potentially modifiable ED-seeking behavior. Although we account only for certain SDH measurable in the EHR, prediagnosis ED use was also strongly predictive for the University cohort. We would not expect the prevalence of only the unmeasured proxy SDH to be disproportionately higher in the University cohort. Although some faculty physicians practice at the University and supervise at Parkland as well, we have low concern for correlation between the health systems given that clinic staff that provide acute care triage advice work exclusively at one health system.
We suspect that patients with prior frequent ED use are exhibiting a behavior reinforced by interactions with the health care system. Patients that frequently visit the ED may find certain features of ED visits favorable to the alternatives (eg, urgent clinic visit), and some may be unaware of alternatives altogether. Although ED visits are accompanied by longer visit times34 and higher cost-sharing,35,36 the ED is open 24 hours, does not require a scheduled appointment, does not rely on patients to determine the severity of their own medical condition, and is the only site of guaranteed evaluation and clinical stabilization regardless of ability to pay.37 Health systems might use this information to develop educational initiatives that target heavy prior ED users and offer them alternative ways to seek urgent medical advice.
To date, policy efforts discouraging patients from inappropriate ED visits have relied on post hoc financial penalties, with some insurers requiring higher cost-sharing for ED visits that, with the benefit of hindsight, are deemed avoidable.38,39 Health care providers and policymakers keen on reducing ED visits among patients with cancer should be careful not to ignore that the patient's decision to visit the ED is made under a great deal of uncertainty. Efforts to reduce ED use by patients with cancer should include strategies to educate patients about the best ways to judge how and where to receive care when sick (eg, urgent telephone advice and ED v outpatient cancer urgent care visit) with a sensitivity to understanding a patient's prior experiences. Although cancer centers often provide instructions about when to call, come to the clinic, or go to the ED, more in-depth educational approaches may be needed for the subgroup of patients who are avid ED users prior to cancer diagnosis. Existing 24-hour telephone triage lines could be emphasized, as well as ED alternatives such as oncology urgent care clinics.40 Such an effort may be more effective and patient-centered than issuing post hoc financial penalties.
Our findings should be interpreted in the context of several limitations. First, this is an observational study, and there may be unmeasured confounders affecting our results. We were unable to adjust for presenting complaint, which prior studies have shown is closely tied to acute care use.28,41,42 However, we carefully adjusted for many of the important predictors of illness severity and reliably measurable SDH. Second, of the original 9,050 Parkland patients and 31,048 University patients, 448 Parkland (5.0%) and 4,555 University (14.7%) patients were not matched to the Foundation database. Most patients were likely unmatched because of data entry errors and discrepancies. Some patients may not have matched because of recent in-migration to the region. However, a selective lack of prediagnosis ED visits would tend to underestimate the magnitude of our prediagnosis ED visit predictor. It is also possible that the matching process combined two different patients with the same names, dates of birth, and zip codes of residence, which would bias our results in both directions. We suspect the frequency of this type of mismatch to be exceedingly low given the multiple levels of detail used to match patients. Third, we did not distinguish which ED visits after cancer diagnosis could have been avoidable—addressable in either an outpatient or specialized oncology urgent care clinic. As to the generalizability of our findings, we captured a broad array of cancer types within two distinct health systems with diverse patient populations over a 10-year time span. Conducting similar analyses across a wider geographic range would only be possible with a specific subset of insured enrollees (eg, Medicare fee-for-service) rather than our all-ages, population-level analysis and would exclude uninsured patients. Additionally, the EHR-based measures of SDH that we used are much less widely available in national-level administrative data sets. However, our findings may not be completely reflective of patients who had synchronous or metachronous cancers.
As part of efforts to reduce potentially avoidable ED visits among a population at high risk, we should take care to understand the behavioral and experiential components of patients seeking acute care. Frequent ED use prior to cancer diagnosis may serve as a surrogate marker that we can use to identify patients likely to have frequent postdiagnosis ED visits. Further research is needed to understand the reasons that underpin patient decisions to seek ED care prior to cancer diagnosis, including qualitative studies exploring the philosophy of seeking on-demand care, cultural and/or community norms, and previous experiences with the health care system. Health systems will also need to provide more timely and patient-friendly sick care telephone advice and accessible ED alternatives such as specialized oncology urgent care clinics.
ACKNOWLEDGMENT
We are grateful to the Dallas-Fort Worth Hospital Council Education and Research Foundation, which contributed a portion of the data, although it did not have a role in the design or conduct of the study.
APPENDIX
TABLE A1.
Negative Binomial Regression Analysis for the Overall Cohort (N = 35,090)
TABLE A2.
Negative Binomial Regression and SAs for the University Cohort (n = 26,493)
TABLE A3.
Negative Binomial Regression and SAs for the Parkland Cohort (n = 8,597)
Arthur S. Hong
Honoraria: Medscape (I)
Consulting or Advisory Role: Janssen (I), AbbVie (I)
Speakers' Bureau: Janssen (I), AbbVie (I)
Travel, Accommodations, Expenses: Janssen (I), AbbVie (I)
D. Mark Courtney
Stock and Other Ownership Interests: Attune Medical
Consulting or Advisory Role: Nabriva Therapeutics
John V. Cox
Employment: University of Texas Southwestern Medical Center—Simmons Cancer Center
Leadership: Parkland Health System
Stock and Other Ownership Interests: Amgen, Medfusion, Merck, Pfizer, Johnson & Johnson
Honoraria: Association of Community Cancer Centers, American College of Physicians, National Comprehensive Cancer Network, National Academies of Science Engineering Medicine
Research Funding: US Oncology
Travel, Accommodations, Expenses: American College of Physicians, Association of Community Cancer Centers, National Comprehensive Cancer Network
Other Relationship: Mary Crowley Research Center, ASCO, Texas Oncology
Uncompensated Relationships: National Committee for Quality Assurance
No other potential conflicts of interest were reported.
DISCLAIMER
The content is solely the responsibility of the authors and does not necessarily represent the official views of Texas Health Resources, the University of Texas Southwestern Medical Center, the National Institutes of Health, or the Agency for Healthcare Research and Quality. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
SUPPORT
Supported by the Texas Health Resources Clinical Scholars Program, the National Center for Advancing Translational Sciences of the National Institutes of Health (UL1TR001105), the Agency for Healthcare Research and Quality (R24HS022418), the National Cancer Institute Cancer Center Support Grant (1P30CA142543), and the Clinician Scientist Development Grant from the American Cancer Society (CSDG-20-023-01-CPHPS).
A.S.H. and D.Q.N. contributed equally to this work as first co-authors.
AUTHOR CONTRIBUTIONS
Conception and design: Arthur S. Hong, Danh Q. Nguyen, Simon Craddock Lee, D. Mark Courtney, Ethan A. Halm
Financial support: Arthur S. Hong, Ethan A. Halm
Administrative support: Arthur S. Hong, John W. Sweetenham, John V. Cox
Provision of study materials or patients: Arthur S. Hong
Collection and assembly of data: Arthur S. Hong, Danh Q. Nguyen, Hannah Fullington
Data analysis and interpretation: Arthur S. Hong, Danh Q. Nguyen, John W. Sweetenham, Navid Sadeghi, John V. Cox
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Prior Frequent Emergency Department Use as a Predictor of Emergency Department Visits After a New Cancer Diagnosis
The following represents disclosure information provided by the authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Arthur S. Hong
Honoraria: Medscape (I)
Consulting or Advisory Role: Janssen (I), AbbVie (I)
Speakers' Bureau: Janssen (I), AbbVie (I)
Travel, Accommodations, Expenses: Janssen (I), AbbVie (I)
D. Mark Courtney
Stock and Other Ownership Interests: Attune Medical
Consulting or Advisory Role: Nabriva Therapeutics
John V. Cox
Employment: University of Texas Southwestern Medical Center—Simmons Cancer Center
Leadership: Parkland Health System
Stock and Other Ownership Interests: Amgen, Medfusion, Merck, Pfizer, Johnson & Johnson
Honoraria: Association of Community Cancer Centers, American College of Physicians, National Comprehensive Cancer Network, National Academies of Science Engineering Medicine
Research Funding: US Oncology
Travel, Accommodations, Expenses: American College of Physicians, Association of Community Cancer Centers, National Comprehensive Cancer Network
Other Relationship: Mary Crowley Research Center, ASCO, Texas Oncology
Uncompensated Relationships: National Committee for Quality Assurance
No other potential conflicts of interest were reported.
REFERENCES
- 1.Weilburg JB, Wong HJ, Sistrom CL, et al. : Behavioral health factors as predictors of emergency department use in the high-risk, high-cost Medicare population Psychiatr Serv 69:1230–1237, 2018 [DOI] [PubMed] [Google Scholar]
- 2.Pines J, Zocchi MS, Larbi A, et al. : Geospatial and clinical factors associated with frequent emergency department use at a Washington DC Safety Net Hospital J Health Care Poor Underserved 31:471–490, 2020 [DOI] [PubMed] [Google Scholar]
- 3.Niedzwiecki MJ, Sharma PJ, Kanzaria HK, et al. : Factors associated with emergency department use by patients with and without mental health diagnoses JAMA Netw Open 1:e183528, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uscher-Pines L, Pines J, Kellerman A, et al. : Deciding to visit the emergency department for non-urgent conditions: A systematic review of the literature Am J Manag Care 19:47–59, 2013 [PMC free article] [PubMed] [Google Scholar]
- 5.Hong AS, Sadeghi N, Harvey V, et al. : Characteristics of emergency department visits and select predictors of hospitalization for adults with newly diagnosed cancer in a safety-net health system J Oncol Pract 15:e490–e500, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Panattoni L, Fedorenko C, Greenwood-Hickman MA, et al. : Characterizing potentially preventable cancer- and chronic disease–related emergency department use in the year after treatment initiation: A regional study J Oncol Pract 14:e176–e185, 2018 [DOI] [PubMed] [Google Scholar]
- 7.Manzano J-GM, Luo R, Elting LS, et al. : Patterns and predictors of unplanned hospitalization in a population-based cohort of elderly patients with GI cancer J Clin Oncol 32:3527–3533, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rivera DR, Gallicchio L, Brown J, et al. : Trends in adult cancer–related emergency department utilization JAMA Oncol 3:e172450, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mayer DK, Travers D, Wyss A, et al. : Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina J Clin Oncol 29:2683–2688, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uscher-Pines L, Pines J, Kellermann A, et al. : Emergency department visits for nonurgent conditions: Systematic literature review Am J Manag Care 19:47–59, 2013 [PMC free article] [PubMed] [Google Scholar]
- 11.Lash R, Bell J, Bold R, et al. : Emergency department use by recently diagnosed cancer patients in California J Community Support Oncol 15:95–102, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hendren S, Chin N, Fisher S, et al. : Patients' barriers to receipt of cancer care, and factors associated with needing more assistance from a patient navigator J Natl Med Assoc 103:701–710, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathematic Policy Research : Admissions and Emergency Department Visits for Patients Receiving Outpatient Chemotherapy, Version 2.0. Princeton, NJ, Mathematica Policy Research, 2018 [Google Scholar]
- 14.Hong AS, Froehlich T, Hobbs SC, et al. : Impact of a cancer urgent care clinic on regional emergency department visits J Oncol Pract 15:e501–e509, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen OK, Makam AN, Clark C, et al. : Predicting all-cause readmissions using electronic health record data from the entire hospitalization: Model development and comparison J Hosp Med 11:473–480, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amarasingham R, Velasco F, Xie B, et al. : Electronic medical record-based multicondition models to predict the risk of 30 day readmission or death among adult medicine patients: Validation and comparison to existing models BMC Med Inform Decis Mak 15:39, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amarasingham R, Moore BJ, Tabak YP, et al. : An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data Med Care 48:981–988, 2010 [DOI] [PubMed] [Google Scholar]
- 18.Njeru JW, St. Sauver JL, Jacobson DJ, et al. : Emergency department and inpatient health care utilization among patients who require interpreter services BMC Health Serv Res 15:214, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doran KM, Kunzler NM, Mijanovich T, et al. : Homelessness and other social determinants of health among emergency department patients J Soc Distress Homeless 25:71–77, 2016 [Google Scholar]
- 20.Charlson ME, Pompei P, Ales KL, et al. : A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation J Chronic Dis 40:373–383, 1987 [DOI] [PubMed] [Google Scholar]
- 21.Deyo RA, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases J Clin Epidemiol 45:613–619, 1992 [DOI] [PubMed] [Google Scholar]
- 22.Sutradhar R, Barbera L: Comparing an artificial neural network to logistic regression for predicting ED visit risk among patients with cancer: A population-based cohort study J Pain Symptom Manage 60:1–9, 2020 [DOI] [PubMed] [Google Scholar]
- 23.Brooks GA, Li L, Uno H, et al. : Acute hospital care is the chief driver of regional spending variation in Medicare patients with advanced cancer Health Aff 33:1793–1800, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams R: Using stata's margins command to estimate and interpret adjusted predictions and marginal effects Stata J 12:308–331, 2016 [Google Scholar]
- 25.Krieger N: Overcoming the absence of socioeconomic data in medical records: Validation and application of a census-based methodology Am J Public Health 82:703–710, 1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trivedi AN, Zaslavsky AM, Schneider EC, et al. : Relationship between quality of care and racial disparities in Medicare health plans JAMA 296:1998–2004, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Krieger N, Chen JT, Waterman PD, et al. : Race/ethnicity, gender, and monitoring socioeconomic gradients in health: A comparison of area-based socioeconomic measures—The public health disparities geocoding project Am J Public Health 93:1655–1671, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sutradhar R, Rostami M, Barbera L: Patient-reported symptoms improve performance of risk prediction models for emergency department visits among patients with cancer: A population-wide study in Ontario using administrative data J Pain Symptom Manage 58:745–755, 2019 [DOI] [PubMed] [Google Scholar]
- 29.Daly B, Gorenshteyn D, Nicholas KJ, et al. : Building a clinically relevant risk model: Predicting risk of a potentially preventable acute care visit for patients starting antineoplastic treatment JCO Clin Cancer Inform 4:275–289, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hong JC, Eclov NCW, Dalal NH, et al. : System for high-intensity evaluation during radiation therapy (SHIELD-RT): A prospective randomized study of machine learning–directed clinical evaluations during radiation and chemoradiation J Clin Oncol 38:3652–3661, 2020 [DOI] [PubMed] [Google Scholar]
- 31.Brooks GA, Uno H, Aiello Bowles EJ, et al. : Hospitalization risk during chemotherapy for advanced cancer: Development and validation of risk stratification models using real-world data JCO Clin Cancer Inform 3:1–10, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grant RC, Moineddin R, Yao Z, et al. : Development and validation of a score to predict acute care use after initiation of systemic therapy for cancer JAMA Netw Open 2:e1912823, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ko M, Lee Y, Chen C, et al. : Prevalence of and predictors for frequent utilization of emergency department Medicine 94:e1205, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaiser Health News : As ER wait times grow, more patients leave against medical advice https://khn.org/news/as-er-wait-times-grow-more-patients-leave-against-medical-advice/
- 35.Narang AK, Nicholas LH: Out-of-pocket spending and financial burden among Medicare beneficiaries with cancer JAMA Oncol 3:757, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramsey SD, Bansal A, Fedorenko CR, et al. : Financial insolvency as a risk factor for early mortality among patients with cancer J Clin Oncol 34:980–986, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Medicare & Medicaid Services : Emergency medical treatment & labor act (EMTALA) https://www.cms.gov/regulations-and-guidance/legislation/emtala/
- 38.Anthem Blue Cross Blue Shield : The right care at the right time and right place https://www11.anthem.com/shared/noapplication/f1/s0/t0/pw_g318734.pdf?refer=ahpprovider&state=oh
- 39.Gillespie L: Emergency or not? Ky. Medicaid changes will penalize for unnecessary ER visits 89.3 WFPL News Louisville, February 21, 2018https://wfpl.org/new-non-emergency-visit-penalty-kicks-in-july-1-for-kentucky-medicaid/ [Google Scholar]
- 40.Waters TM, Kaplan CM, Graetz I, et al. : Patient-centered medical homes in community oncology practices: Changes in spending and care quality associated with the COME HOME experience J Oncol Pract 15:e56–e64, 2019 [DOI] [PubMed] [Google Scholar]
- 41.Harrison JM, Stella PJ, Lavasseur B, et al. : Toxicity-related factors associated with use of services among community oncology patients J Oncol Pract 12:e818–e827, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.El Majzoub I, Qdaisat A, Chaftari PS, et al. : Association of emergency department admission and early inpatient palliative care consultation with hospital mortality in a comprehensive cancer center Support Care Cancer 27:2649–2655, 2019 [DOI] [PubMed] [Google Scholar]