Abstract
Background
Various procedures exist to augment or reconstruct the Achilles tendon (AT) in patients suffering from chronic pathologies. The aim of this study is to assess patient reported outcomes and satisfaction following single incision FHL augmentation using a short tendon harvest with interference screw fixation.
Methods
This is a multicentre case series where postoperative patient reported outcome and satisfaction scores were collected on 30 patients. Outcome measures included EQ-5D, EQ-VAS, Achilles Tendon Rupture Scores (ATRS), and satisfaction scores. Scores were also collected on the unaffected limbs for comparison.
Results
Mean patient age was 61 years (range 40–79, SD 11). Mean EQ-5D index value was 0.750 (0.100–1.00, SD 0.238), and mean EQ-VAS score was 74 (36–99, SD 15), at a mean follow-up of 57 months (4–118, SD 32). For patients with ≥24 months’ follow-up, a mean deficit of 16 ATRS points was found between the operated and unaffected limb. Overall satisfaction was over 86%. In cases of chronic AT rupture, younger age and increasing time from initial injury to surgery were predictors of greater residual deficit. No serious complications or failures occurred.
Conclusions
FHL augmentation using short tendon harvest and interference screw fixation is a safe treatment option. It appears to take at least 24 months to functionally recover following this procedure, and despite a residual function deficit, there is a high level of patient satisfaction. Further studies are required to determine optimal patient selection and timing of surgery.
Keywords: Flexor hallucis longus (FHL), Tendon transfer, Tendo Achilles, Reconstruction, Augmentation
1. Introduction
Acute Achilles tendon (AT) ruptures are usually amenable to conservative treatment, with favourable outcomes being reported when diagnosed and treated promptly.1 However, as many as 10–25% of acute AT ruptures can initially remain undiagnosed due to misdiagnosis or delayed presentation, resulting in a chronic rupture.2,3 Failure of conservative treatment can also result in an acute rupture becoming chronic. Achilles tendinopathy itself can be a chronic problem in patients of all ages where degeneration and ruptures are a common part of disease progression.4 In cases of chronic AT rupture or recalcitrant tendinopathy, reconstruction or augmentation may be required to improve patient symptoms and restore function.5, 6, 7, 8
A variety of surgical techniques have been described for AT reconstruction and augmentation. These include V–Y advancement, turn-down flaps, flexor hallucis longus (FHL), flexor digitorum longus (FDL), peroneus brevis (PB) transfer, as well as a variety of autograft, allograft and synthetic graft options.9, 10, 11, 12, 13, 14, 15, 16 FHL transfer has gained popularity with some now considering this to be the gold standard for reconstruction and augmentation. FHL transfer has several advantages; it is easily harvested due to its proximity to the AT, has clinically insignificant donor site morbidity, can be performed with less exposure minimising risk of neurovascular injury and wound healing complications, and has a very low reported failure rate.6,17, 18, 19
The original method of FHL transfer was first described by Hansen in 1991.18 Various modifications to the procedure have since been described, including single versus double incisions, short versus long graft, route of tendon graft, method of fixation, and open versus endoscopic approach. FHL transfer is often performed to augment a separate Achilles tendon repair or reconstructive procedure, but can also be performed as a standalone procedure.20 When performed as a standalone procedure, the FHL transfer can function as both a reconstruction and augment if interwoven with the proximal and distal Achilles stump, or function purely as an augment if only fixed distally.
The aim of this study is to assess our patient reported outcomes and satisfaction following FHL augmentation for chronic AT pathologies using a single incision ‘short harvest’ technique.20 This technique has been shown to have favourable outcomes for both the treatment of tendinopathy and chronic AT rupture.21, 22, 23, 24
2. Methods
2.1. Study design
This is a multicentre case series involving patients undergoing single incision FHL augmentation for chronic AT pathologies at 3 centres, performed by 2 Consultant Foot & Ankle surgeons, using identical methods. All consecutively treated patients over a 10-year period from 2010 to February 2020 were identified from operative databases and considered for inclusion. All patients were contacted by telephone during the month of July 2020, and invited to complete a questionnaire assessing their current health, patient reported outcome measures and patient satisfaction. The questionnaire was designed for self-completion and included clear written instructions. As preoperative scores were not routinely collected, the questionnaire included assessment of the unaffected limb for comparison, and satisfaction scores that assessed changes in symptoms and function following surgery. Questionnaires were sent and returned using the patient's preferred method (e-mail or post). Patients who were not contactable by telephone following 3 separate attempts were not sent questionnaires. Patient demographics and details regarding diagnosis and treatment were collected from electronic healthcare records. This study was authorised by the Research and Development departments for Service Evaluation and thus ethical committee review was not required.
2.2. Surgical technique
The procedure is performed with patient in the ‘recovery’ or prone position, under general anaesthesia and thigh tourniquet, using an open technique with a single posteromedial incision. A short harvest of the FHL tendon (approximately 1 inch) is performed though the same incision. The deep compartment fascia is released to allow posterior migration of the muscle belly. A whip stitch is placed on the tendon and the diameter measured. A bone tunnel is made close to the Achilles tendon insertion from the dorsomedial surface of the calcaneal tuberosity and directed plantar-laterally. The harvested FHL tendon is passed through the tunnel and tensioned distally until the FHL muscle belly comes into contact with the mouth of the tunnel. An appropriately sized BioComposite Tenodesis Screw (Arthrex, Naples, FL) is used to secure the tendon in the tunnel. In AT rupture cases, the rupture site is not taken down or attached to the FHL transfer. In cases of tendinopathy, the Achilles tendon is debrided and repaired or excised depending on the extent of degeneration. Similarly, the Achilles tendon in not secured onto the FHL transfer.
Postoperatively the patients are placed into a below knee equinus plaster slab. The vast majority of patients are discharged home the same day, and are prescribed a 6 week course of low molecular weight heparin for venous thromboembolism (VTE) prophylaxis. At 2 weeks, patients are converted into a full cast with the foot in mid-equinus position, or VACOped boot (OPED UK Ltd, Devizes, UK) locked in 20° plantar flexion, and patients are allowed to weightbear as tolerated. At 6–8 weeks, the cast or boot is removed and physiotherapy is commenced.
2.3. Outcome measures
-
•
EQ-5D, EQ-VAS and EQ-5D index values to assess current perceived state of health. The EQ-5D index value, which converts the responses of the 5 EQ-5D dimensions into a single value, are calculated using the Crosswalk value set for UK, where the minimum score is −0.594 and maximum score 1.000.25
-
•
Achilles Tendon Rupture Scores (ATRS) of the operated limb, and also the unaffected limb for comparison, where a total score of 0 indicates major limitations, and a score of 100 indicates no limitations.26
-
•
Satisfaction scores based on statements adapted from 10 items of the ATRS questionnaire, to assess improvement in symptoms and function following surgery (see Appendix). For example, Statement 1: ‘Surgery has increased strength in my calf/Achilles tendon/foot’. A 5-point Likert scale was used to assess each of the 10 items, giving a total score from 10 to 50, where 10 indicates complete disagreement/dissatisfaction, and 50 indicates complete agreement/satisfaction. This adapted score was designed and utilised to give a more specific satisfaction rating, and has not previously been used or validated.
-
•
Overall impressions regarding the surgery using 5-point Likert scales, assessing overall satisfaction with results, improvement in quality of life, if they would have the surgery again, and if they would recommend to a friend of family member.
-
•
Patient reported complications were collected using a yes/no format in the questionnaire, explicitly assessing for incidence of complications including ‘blood clots in legs or lungs’, infections or wound complications, nerve damage, ‘weakness of big toe’ and lesser toe deformities. Free text space was also available for the patient to elaborate or add additional complications or comments.
2.4. Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp. Released 2017. Armonk, NY). Mean, range and standard deviation (SD) are stated to describe continuous variables. Paired-samples t-tests were used to compare related samples, and independent-samples t-tests to compare unrelated samples. Multiple linear regression analyses were performed to assess the relationship between multiple continuous independent variables and a single dependent variable. P-values ≤0.05 were considered statistically significant.
3. Results
3.1. Patients
Over the 10-year period 65 patients were identified who underwent FHL transfer. Of the 65 patients, 49 (81.7%) were contactable by telephone and were invited to complete the patient reported outcomes questionnaire, of which 30 (61.2%) responded, whose data were included in the analysis.
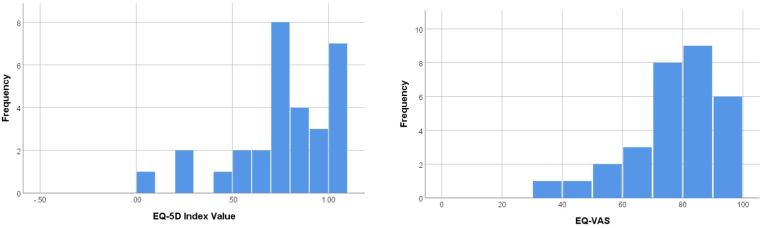
As summarized in Table 1, the overall mean patient age was 61 years (range 40–79, SD 11), with a mean follow-up of 57 months (4–118, SD 32) from date of surgery to time of completion of questionnaire; Follow-up was ≥24 months for the majority of patients (26/30). The indications for surgery were delayed presentation/neglected AT rupture (>6 weeks from injury) (n = 16), failure of tendon healing with non-operative treatment of AT rupture (n = 8), and recalcitrant non-insertional Achilles tendinopathy (n = 6). The ‘failure of tendon healing with non-operative treatment’ group included 2 cases of re-rupture occurring within 3 months of completing our non-operative treatment protocols used to treat approximately 150 patients each year following acute AT rupture. As shown in Fig. 1, overall patients reported good state of health, with mean EQ-5D index value of 0.750 (0.100–1.00, SD 0.238), and mean EQ-VAS score of 74 (36–99, SD 15).
Table 1.
Summary of demographics of patients included in the study, including subgroup demographics according to indication for surgery.
| n = | Mean Age (range, SD) | Gender (M/F) | Mean Number of Months from Initial Injury to Surgery (range, SD) | Mean Number of Months Follow-up (range, SD) | |
|---|---|---|---|---|---|
| Delayed presentation/neglected AT rupture | 16 | 64 (40–79, SD 10) | 13 M/3F | 10 (5–24, SD 5) | 48 (4–90, SD 28) |
| Failure of tendon healing with non-operative treatment of AT rupture | 8 | 53 (40–62, SD 8) | 8 M/0F | 5 (1–11, SD 4) | 62 (9–118, SD 38) |
| Tendinopathy | 6 | 62 (49–73, SD 10) | 4 M/2F | – | 75 (21–106, SD 33) |
| Total | 30 | 61 (40 to 79, SD 11) | 25M/5F | 8 (0 to 24, SD 5) | 57 (4 to 118, SD 32) |
Fig. 1.
Simple histograms demonstrating distribution of EQ-5D Index Values and EQ-VAS scores.
3.2. ATRS outcome scores
Analysis of ATRS scores excluded results for 3 anomalous patients who had significantly impaired function of the ‘unaffected limb’, preventing use of comparison between limbs as an assessment of outcome. As summarized in Table 2, there was an overall significant difference in mean ATRS score of −20 points between the patients operated limbs (mean = 60; 28 to 98, SD 20) against their unaffected limbs (mean = 80; 39 to 100, SD 22); p = 0.001. This difference was not statistically significant in the tendinopathy group, perhaps due to low numbers.
Table 2.
Summary of mean ATRS scores, with subgroups according to indication for surgery.
| n = | Mean ATRS of Operated Limb (range, SD) | Mean ATRS of Unaffected Limb (range, SD) | Mean Difference in ATRS Between Limbs |
||
|---|---|---|---|---|---|
| (range, SD) | p-value | ||||
| Delayed presentation/neglected AT rupture | 15 | 62 (33–88, SD 18) | 79 (56–100, SD 15) | −17 (−29 to −6, SD 21) | 0.006∗ |
| Failure of tendon healing with non-operative treatment of AT rupture | 7 | 66 (28–93, SD 24) | 92 (72–100, SD 12) | −25 (−43 to −6, SD 22) | 0.016∗ |
| Tendinopathy | 5 | 47 (36–67, SD 13) | 65 (39–100, SD 25) | −17 (−50 to 16, SD 27) | 0.219 |
| Total | 27 | 60 (28 to 93, SD 20) | 80 (39 to 100, SD 18) | −20 (-28 to -11, SD 22) | 0.001∗ |
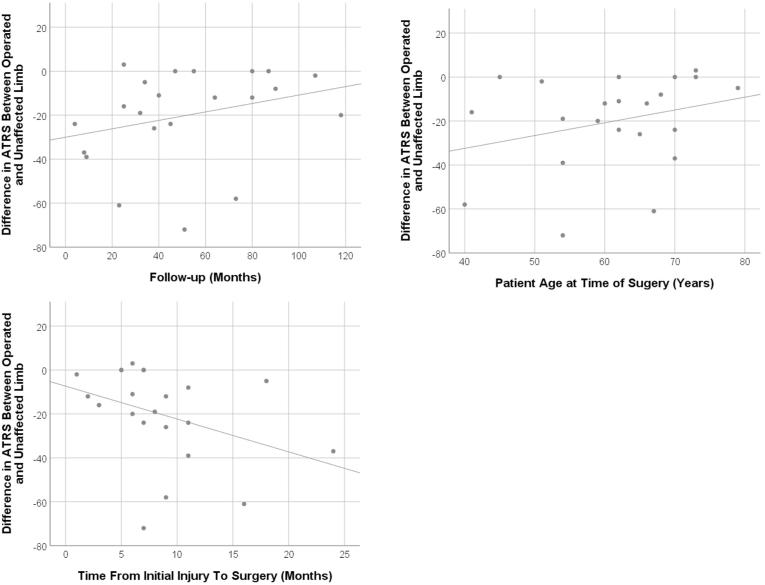
Multiple linear regression analysis was performed, excluding patients from the tendinopathy group, to assess if the continuous variables of age, number of months from initial injury to surgery and number of months follow-up could predict outcome in patients operated on following AT rupture. The results indicated that the model was statistically significant (F(3,18) = 4.452, p = 0.017), with adjusted R2 0.330. Age (standardized beta coefficient 0.583, p = 0.010) and number of months from injury to surgery (standardized beta coefficient −0.563, p = 0.019) were found to be significant predictors, meaning increasing age or earlier surgery would result in less functional deficit in terms of ATRS score (i.e. better outcome). Scatter plots demonstrating the raw correlations are shown in Fig. 2. Whilst a general trend towards improved function with increasing number of months follow-up can be visualised, this was not statistically significant.
Fig. 2.
Scatter plots demonstrating raw correlations between age, length of follow-up and time from injury to surgery, and difference in ATRS between limbs (excluding.
When all patients with <24 months follow-up (n = 4) are compared to patients with ≥24 months follow-up (n = 23), a statistically significant mean difference in ATRS between limbs is seen; −40 points (SD 15) vs −16 points (SD 21), p = 0.039. No significant difference is seen between patients with 24–72 months follow-up (n = 13) and patients with ≥72 months follow-up (n = 10); −16 points (SD 20) vs −16 points (SD 24), p = 0.987.
3.3. Patient satisfaction
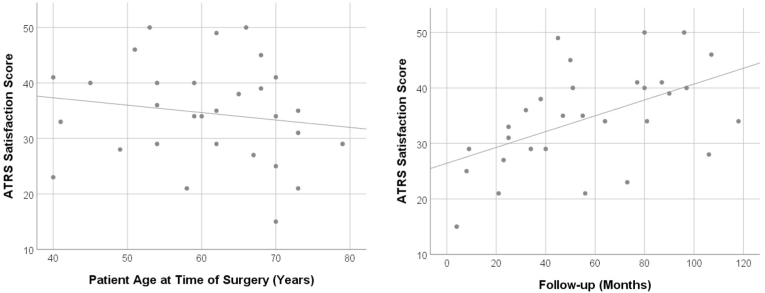
Mean satisfaction score using the adapted ATRS instrument, where a total score of 50 would indicate complete satisfaction, was 35 (15–50, SD 9). Multiple linear regression analysis was performed, including all patients, to assess if the continuous variables of age and length of follow-up could predict satisfaction. The results indicated that the model was statistically significant (F(2,27) = 4.894, p = 0.015), with adjusted R2 0.266. Only number of months follow-up (standardized beta coefficient 0.519, p = 0.006) was found to be a significant predictor, meaning that increasing number of months follow-up could predict greater patient satisfaction. Scatter plots demonstrating the raw correlations are shown in Fig. 3.
Fig. 3.
Scatter plots demonstrating raw correlations between age and length of follow-up, and ATRS satisfaction score.
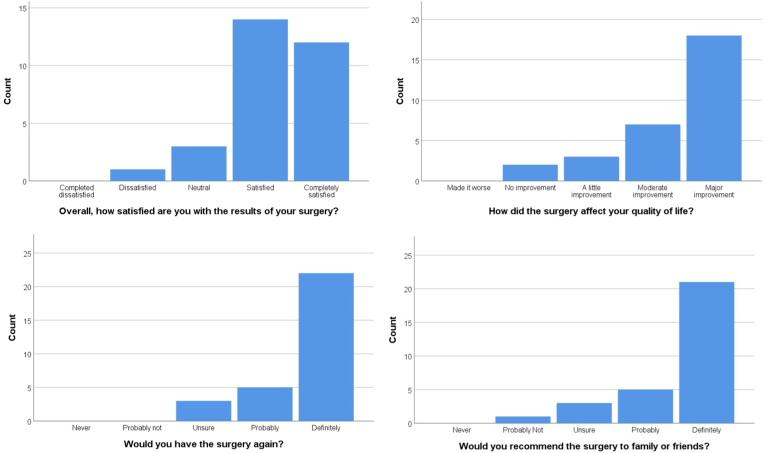
As demonstrated in Fig. 4, the responses to the summary statements show high levels of overall satisfaction. Over 86% of patients were either satisfied or completely satisfied with the results of their surgery and would undergo the surgery again if required. 83% of patients reported that the surgery gave them a moderate or major improvement in quality of life.
Fig. 4.
Histograms summarizing distribution of responses to the overall satisfaction statements.
3.4. Complications
There were no major patient reported complications, in particular no cases of postoperative DVT/PE, wound problems, infection, nerve injury, or re-operation. The most common complications reported were weakness of big toe (n = 6), and calf muscle wasting (n = 5). One patient commented that the weakness of the big toe affected their balance and ability to perform sports. Other reported complications were leg swelling (n = 2), deformity to the lesser toes (n = 1), heel pain (n = 1), calf pain (n = 1) and scar sensitivity (n = 1).
4. Discussion
The aim of this study was to assess patient reported outcomes and satisfaction following single incision FHL augmentation for chronic AT pathologies. Our results show that despite a reported residual functional deficit when compared to the unaffected limb, there is an overall high level of satisfaction with the outcome of surgery. Whist functional improvements, in terms of ATRS, may plateau after 24 months, satisfaction continues to improve linearly with time. No serious complications or failures were reported in our cohort of patients, demonstrating the benefit of a ‘less is more’ approach, over more extensive reconstructive or augmentation techniques.
The high levels of satisfaction following surgery seen in our cohort is similar to findings of other studies of patients treated with FHL transfer.21,22 Our results suggest that both functional deficit and patient satisfaction appear to improve with time; Reasons for this are likely multifactorial. In a previous study using MRI evaluation, Hahn et al. noted hypertrophy of the FHL muscle of more than 15% in 80% of the study population at a mean follow-up of 46.5 months, with similar findings also reported by other studies.19,27, 28, 29 Another factor may be the benefits of the well vascularized FHL muscle bulk coming into proximity of the relatively avascular portion of the AT, resulting in integration to, and repair of the AT over time.27,30 By advancing the FHL tendon until the muscle contacts the mouth of the bone tunnel, as described in our methods, this beneficial effect would be maximised. These processes could therefore be considered to result in biological AT reconstruction, and support use of a technique where no surgical AT reconstruction in performed in addition to the FHL augmentation. Furthermore, these findings may be helpful when setting expectations and counselling future patients regarding rehabilitation time.
In cases of neglected rupture or failure of tendon healing with non-operative treatment of acute AT rupture, our results suggest that younger age and longer time from initial injury to surgery may be predictors of greater residual functional deficit. Given that the youngest patient in our study was 40 years old, further studies would be required to assess if this is an appropriate treatment option for restoring function in a younger active patient. The latter finding is similar to Yeoman et al. who reported that patients with the longest injury to operation interval also had the slowest recovery and poorer post-operative outcome.24 It may be that the biological benefits of FHL transfer described above are most beneficial when performed during the earlier stages of remodelling following AT rupture.30,31
The FHL tendon can be harvested using either single or double incisions. The single incision technique negates the risks associated with the double incision, such as plantar nerve damage, morbidity of multiple incisions and additional infection risk. Conversely, the dual incision approach has the advantage of allowing a long tendon harvest, giving the options of weaving through the Achilles tendon stumps or looping through the calcaneus, thereby reconstructing and augmenting simultaneously. Risks of a short harvest technique include reliance on the tenodesis screw for fixation, and inability to salvage the short tendon in the unlikely event of failure during tenodesis screw insertion.6,20,32,33 In our cohort, no serious complications or failures occurred, demonstrating that fixation of a short tendon harvest using an interference screw is safe and secure. Passing the tendon through the tunnel until the muscle belly reaches the mouth of the tunnel, rather than passing a measured length to achieve a specific foot position, can help ensure adequate fixation when using this technique.
Weakness of the hallux plantarflexion strength is a well-known morbidity of FHL transfer as also highlighted in our findings, with six patients reporting weakness. Only one of these patients reported a functional impairment as a result, stating that it resulted in less balance when playing sports, but remained overall satisfied. Previous studies have noted FHL transfer morbidity to be clinically insignificant and to not translate to functional disability, and our findings would support this.6,34
There are some limitations to our study. Due to limitations caused by the COVID-19 pandemic, collection of only patient reported outcome measures was possible during the study period. Additionally, no preoperative scores were collected, hence the focus of outcome was on deficit between the operated and unaffected limb. Unique methods using adapted instruments were required to provide the best reflection of treatment outcome, also making comparison with other studies challenging. However, the methods are sufficient for producing a useful insight into trends, predictors, and overall patient satisfaction. Several interesting conclusions can be made based on these methods and results, which may be helpful when making treatment decisions and counselling patients. Finally, there is likely to be some degree of recall bias with regards to complications, and incidence of minor complications that have no significant or lasting impact on health or function may be underreported.
In conclusion, our study demonstrates that single incision FHL augmentation using short tendon harvest with interference screw fixation is safe and secure technique. Functional recovery takes at least 24 months following this procedure, and despite a residual functional deficit, there is high level of patient satisfaction. Younger age and increasing interval from injury to surgery may be predictors of lesser outcomes. Further studies are recommended to determine optimal patient selection and timing of surgery for this treatment option.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2021.101650.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
figs1
References
- 1.Ochen Y., Beks R.B., Van Heijl M., et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2018;364 doi: 10.1136/bmj.k5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leslie H.D.H., Edwards W.H.B. Neglected ruptures of the achilles tendon. Foot Ankle Clin. 2005;10(2):357–370. doi: 10.1016/j.fcl.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Inglis A., Scott W., Sculco T., Patterson A. Ruptures of the tendo achillis. An objective assessment of surgical and non-surgical treatment. J Bone Joint Surg. 1976;58(7):990–993. doi: 10.2106/00004623-197658070-00015. [DOI] [PubMed] [Google Scholar]
- 4.Jozsa L., Kvist M., Balint B.J., et al. The role of recreational sport activity in Achilles tendon rupture. Am J Sports Med. 1989;17(3):338–343. doi: 10.1177/036354658901700305. [DOI] [PubMed] [Google Scholar]
- 5.Jarin I., Bäcker H.C., Vosseller J.T. Meta-analysis of noninsertional achilles tendinopathy. Foot Ankle Int. 2020;41(6):744–754. doi: 10.1177/1071100720914605. [DOI] [PubMed] [Google Scholar]
- 6.Wapner K.L., Hecht P.J. Repair of chronic achilles tendon rupture with flexor hallucis longus tendon transfer. Operat Tech Orthop. 1994;4(3):132–137. doi: 10.1016/S1048-6666(06)80123-0. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs D., Martens M., Van Audekercke R., Mulier J.C., Mulier F.R. Comparison of conservative and operative treatment of Achilles tendon rupture. Am J Sports Med. 1978;6(3):107–111. doi: 10.1177/036354657800600302. [DOI] [PubMed] [Google Scholar]
- 8.Maffulli N., Ajis A. Management of chronic ruptures of the Achilles tendon. J Bone Jt Surg Am Vol. 2008;90(6):1348–1360. doi: 10.2106/JBJS.G.01241. [DOI] [PubMed] [Google Scholar]
- 9.Arshad Z., Lau E.J.S., Leow S.H., Bhatia M. Management of chronic Achilles ruptures: a scoping review. Int Orthop. 2021;1:1–17. doi: 10.1007/S00264-021-05102-5. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maffulli N., Oliva F., Maffulli G.D., Buono A Del, Gougoulias N. Surgical management of chronic Achilles tendon ruptures using less invasive techniques. Foot Ankle Surg. 2018;24(2):164–170. doi: 10.1016/J.FAS.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Mulier T., Pienaar H., Dereymaeker G., Reynders, Broos P. The management of chronic achilles tendon ruptures: gastrocnemius turn down flap with or without flexor hallucis longus transfer. Foot Ankle Surg. 2003 doi: 10.1016/S1268-7731(03)00048-1. [DOI] [Google Scholar]
- 12.Maffulli N., Spiezia F., Testa V., Capasso G., Longo U.G., Denaro V. Free gracilis tendon graft for reconstruction of chronic tears of the achilles tendon. J Bone Joint Surg. 2012;94(10):906–910. doi: 10.2106/JBJS.K.00869. [DOI] [PubMed] [Google Scholar]
- 13.Padanilam T.G. Chronic achilles tendon ruptures. Foot Ankle Clin. 2009;14(4):711–728. doi: 10.1016/j.fcl.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Pérez Teuffer A. Traumatic rupture of the Achilles Tendon. Reconstruction by transplant and graft using the lateral peroneus brevis. Orthop Clin N Am. 1974;5(1):89–93. doi: 10.1016/S0030-5898(20)31242-6. [DOI] [PubMed] [Google Scholar]
- 15.Mann R.A., Holmes G.B., Seale K.S., Collins D.N. Chronic rupture of the Achilles tendon. J Bone Joint Surg. 1991;73(2):214–219. doi: 10.2106/00004623-199173020-00009. [DOI] [PubMed] [Google Scholar]
- 16.Abraham E., Pankovich A. Neglected rupture of the Achilles tendon. Treatment by V-Y tendinous flap. J Bone Joint Surg. 1975;57(2):253–255. doi: 10.2106/00004623-197557020-00019. [DOI] [PubMed] [Google Scholar]
- 17.Stenroos A., Brinck T. Achilles tendon reconstruction with semitendinous tendon grafts is associated with a high complication rate. J Am Podiatr Med Assoc. 2020;110(2):1–7. doi: 10.7547/18-014. [DOI] [PubMed] [Google Scholar]
- 18.Hansen S.T. In: Disorders of the Foot and Ankle. Jahhs M., editor. WB Saunders; Philadelphia: 1991. Trauma to the heel cord; p. 2357. [Google Scholar]
- 19.Oksanen M.M., Haapasalo H.H., Elo P.P., Laine H.-J. Hypertrophy of the flexor hallucis longus muscle after tendon transfer in patients with chronic Achilles tendon rupture. Foot Ankle Surg. 2014;20(4):253–257. doi: 10.1016/j.fas.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Malagelada F., Clark C., Dega R. Management of chronic Achilles tendon ruptures—a review. Foot. 2016 doi: 10.1016/j.foot.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Suttinark P., Suebpongsiri P. Clinical outcomes of flexor hallucis longus transfer for the treatment of Achilles tendinosis rupture. J Med Assoc Thail. 2009 [PubMed] [Google Scholar]
- 22.Mahajan R.H., Dalal R.B. Flexor hallucis longus tendon transfer for reconstruction of chronically ruptured Achilles tendons. J Orthop Surg. 2009 doi: 10.1177/230949900901700215. [DOI] [PubMed] [Google Scholar]
- 23.Wegrzyn J., J Luciani J.F., Philippot R., Brunet-Guedj E., Moyen B., Besse J. Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int Orthop. 2010 doi: 10.1007/s00264-009-0859-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeoman T.F.M., Brown M.J.C., Pillai A. Early post-operative results of neglected tendo-Achilles rupture reconstruction using short flexor hallucis longus tendon transfer: a prospective review. Foot. 2012 doi: 10.1016/j.foot.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Van Hout B., Janssen M.F., Feng Y.S., et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–715. doi: 10.1016/j.jval.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 26.Nilsson-Helander K., Thomeé R., Grävare-Silbernagel K., et al. The achilles tendon total rupture score (ATRS): development and validation. Am J Sports Med. 2007;35(3):421–426. doi: 10.1177/0363546506294856. [DOI] [PubMed] [Google Scholar]
- 27.Hahn F., Meyer P., Maiwald C., Zanetti M., Vienne P. Treatment of chronic achilles tendinopathy and ruptures with flexor hallucis tendon transfer: clinical outcome and MRI findings. Foot Ankle Int. 2008 doi: 10.3113/FAI.2008.0794. [DOI] [PubMed] [Google Scholar]
- 28.Richardson D.R., Willers J., Cohen B.E., Davis W.H., Jones C.P., Anderson R.B. Evaluation of the hallux morbidity of single-incision flexor hallucis longus tendon transfer. Foot Ankle Int. 2009 doi: 10.3113/FAI.2009.0627. [DOI] [PubMed] [Google Scholar]
- 29.Wegrzyn J., Luciani J.-F., Philippot R., Brunet-Guedj E., Moyen B., Besse J.-L. Chronic Achilles tendon rupture reconstruction using a modified flexor hallucis longus transfer. Int Orthop. 2010;34(8):1187–1192. doi: 10.1007/s00264-009-0859-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Batista J.P., Abdelatif N.M.N., Del Vecchio J.J., Diniz P., Pereira H. Endoscopic flexor hallucis longus transfer for the management of acute achilles tendon ruptures: a prospective case series report with a minimum of 18 Months' follow-up. J Foot Ankle Surg. 2020;59(5):927–937. doi: 10.1053/J.JFAS.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 31.Pendse A., Kankate R. Reconstruction of chronic achilles tendon ruptures in elderly patients, with vascularized flexor hallucis longus tendon transfer using single incision technique. Acta Orthop Belg. 2019;85:137–143. [PubMed] [Google Scholar]
- 32.Benca E., Willegger M., Windhager R., et al. Biomechanical evaluation of two methods of fixation of a flexor hallucis longus tendon graft. Bone and Joint Journal. 2018;100B(9):1175–1181. doi: 10.1302/0301-620X.100B9.BJJ-2018-0100.R2. [DOI] [PubMed] [Google Scholar]
- 33.DeCarbo W.T., Hyer C.F. Interference screw fixation for flexor hallucis longus tendon transfer for chronic Achilles tendonopathy. J Foot Ankle Surg. 2008;47(1):69–72. doi: 10.1053/j.jfas.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 34.Coull R., Flavin R., Stephens M.M. Flexor hallucis longus tendon transfer: evaluation of postoperative morbidity. Foot Ankle Int. 2003;24(12):931–934. doi: 10.1177/107110070302401211. [DOI] [PubMed] [Google Scholar]