Abstract
Background
The aim of this study was to assess the effectiveness of functional bracing in the treatment of humeral shaft fractures and identify factors that increased the risk of delayed or non-union.
Methods
All patients with humeral shaft fractures treated at Musgrove Park Hospital between 2010 and 2017 were identified. Patient electronic records were reviewed to identify demographic data, as well as outcomes and complications following treatment. Radiographs were reviewed to identify fracture pattern and location as well as fracture displacement and angulation.
Results
In total, 65 patients were treated with functional bracing of which 22 patients (34%) had a delayed or non-union. Fracture displacement and angulation were significantly associated with delayed or non-union. In particular, patients with fractures displaced more than 30 mm or angulated more than 30° had a significantly higher risk of delayed or non-union. Fracture location or pattern was not significantly associated with delayed or non-union.
Conclusion
Functional bracing is an effective treatment modality for the majority of patients with humeral shaft fractures, but patients with markedly displaced or angulated fractures are at a higher risk of failure of conservative treatment and therefore early operative intervention should be considered.
Keywords: humerus, fracture, shaft, union, delayed, non-union, functional bracing, Sarmiento
Introduction
Humeral shaft fractures account for approximately 3% of all fractures and are associated with a bimodal distribution; with high energy fractures in young patients, and low energy fractures in elderly patients.1–4 Traditionally humeral shaft fractures have been treated non-operatively with functional bracing, as originally described by Sarmiento.1–3 Functional bracing is associated with good outcomes, with union rates reported between 87% and 98%1–6 and good or very good functional outcome scores in 86% to 96% of cases. 7 Non-union rates with brace treatment have been noted to be higher in transverse fractures, proximal third fractures, in injuries with a persisting fracture gap following application of the brace and in obese patients.2,3,6–10
Operative treatment of humeral shaft fractures has gained popularity recently, with the development of new surgical techniques and implants.3,9,11 Surgical fixation is usually recommended in: open fractures, pathological fractures, high energy comminuted or segmental fractures, associated brachial plexus injury, ipsilateral forearm shaft fractures resulting in a floating elbow, fractures extending into the distal articular surface or proximal humeral head and fractures in which acceptable alignment cannot be achieved in a brace.2–4,6,11,12 Primary operative intervention for closed, isolated humeral shaft fractures is not recommended by most authors and instead surgery is usually reserved for patients who go on to non-union or in whom the brace fails to control fracture displacement.1,2,7,8 Outcomes are, however, known to be worse for patients treated operatively for non-union following failed conservative treatment.3,13
At Musgrove Park Hospital, a 700 bed district general hospital, the majority of patients with humeral shaft fractures are treated in a functional brace, in line with existing literature.1–6 The aim of this study was to determine the rate of non-union or delayed union in humeral shaft fractures treated with the brace and therefore to identify which patients may benefit from early operative fixation.
Methods
All patients with a humeral shaft fracture treated at Musgrove Park Hospital, between 2010 and 2017 were retrospectively identified using an electronic patient database. Inclusion criteria were patients with humeral shaft fractures who were 16 years or older. Exclusion criteria were open fractures, pathological fractures and fractures extending into the distal articular surface or proximal humeral head, which would not be amenable to bracing. The study was approved by the trust research and development department.
All conservatively treated patients had a humeral brace (Clasby Brace, Beagle Orthopaedics, United Kingdom) applied on presentation to the emergency department. The brace was adjusted at subsequent fracture clinic follow-up appointments, as soft tissue swelling decreased, and patients were reassessed clinically and radiographically at two and six weeks post-injury, by senior orthopaedic surgeons. Patients were weaned from the brace once pain had subsided and then commenced gentle range of movement exercises. Follow-up was continued until clinical or radiographic union was achieved. Radiological union was defined as bone bridging the fracture site across both cortices in orthogonal planes. Clinical union was defined as the absence of pain or mobility at the fracture site.
If there were no radiographic or clinical signs of union from six weeks post injury, this was treated as a delayed union, and surgical intervention was offered to patients. Patients who did not want or were not candidates for surgical fixation were continued with brace treatment and regular follow-up. When surgical fixation was performed, it was done so by consultant upper limb orthopaedic surgeons and performed through an anterolateral or posterior triceps splitting approach using a locking compression plate (4.5 mm, Synthes GmbH, Switzerland).
Patient clinical records and radiographs were reviewed using the electronic patient record (EPRO, United Kingdom) and picture archive clinical system (Intellipacs, Philips, the Netherlands) to identify demographic details, injury mechanism, treatments performed, complications and overall outcome.
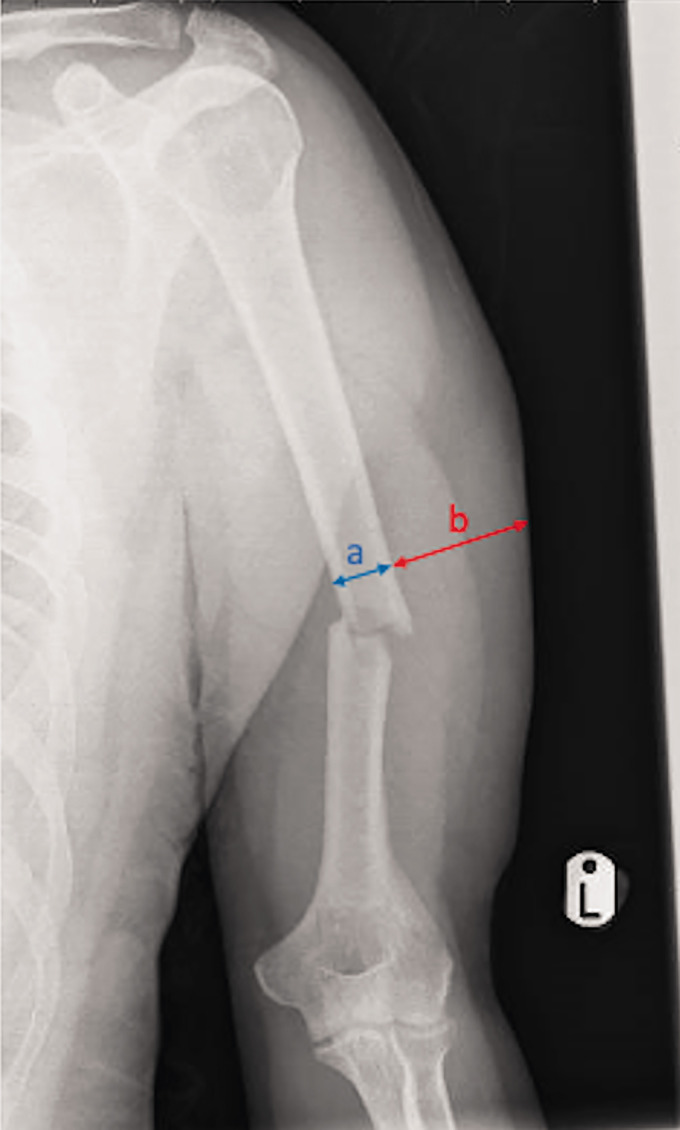
Fracture patterns were classified using the AO OTA fracture classification system. 14 Radiographic parameters included fracture alignment and displacement, before and after application of the brace. The soft tissue envelope at the lateral humeral mid-shaft was also measured and expressed as a ratio of bone to soft tissues. This ratio was used as a surrogate measurement for patient obesity (Figure 1).
Figure 1.
Measurement of bone to soft tissue ratio (a/b).
Statistical analysis was performed with SPSS (v20, IBM, USA) and Microsoft Excel (2017, USA) using an unpaired t-test for continuous variables and Chi-squared test for categorical variables. Level of significance was set to p < 0.05.
Results
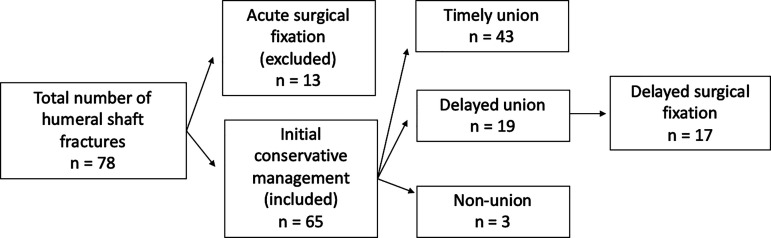
In total, 78 patients with humeral shaft fractures were identified over the study period. Of these, 13 patients had undergone acute surgical fixation of their fracture and were therefore excluded from the cohort. This left 65 patients for analysis.
The mean age was 64.3 years (range 17–94) and 40 patients (62%) were females. The mechanism of injury was defined as low energy in 55 cases (85%) and high energy in 10 cases (15%) (Table 1). The fracture pattern was spiral (A1) in 35 cases (54%), transverse (A3) in 25 cases (38%), wedge (B2) in 4 cases (6%) and segmental fragmentary (C3) in 1 case (2%). The fracture occurred at the midshaft in 47 cases (72%), at the proximal third in 13 cases (20%) and at the distal third in 5 cases (8%) (Table 2).
Table 1.
Clinical parameters of humeral shaft fractures in relation to union or delayed/non-union.
| Union | Delayed/ non-union | |
|---|---|---|
| Number of patients | 43 (66%) | 22 (34%) |
| Mean age | 68.4 (range 17–91) | 63.8 (range 25–94) |
| Female-to-male ratio | 0.67 | 0.59 |
| High energy injury | 7 (16%) | 3 (14%) |
Table 2.
Radiographic parameters of humeral shaft fractures in relation to union or delayed/non-union.
| Union | Delayed/ non-union | |
|---|---|---|
| Mid-shaft fractures | 31 (72%) | 15 (68%) |
| Proximal third fractures | 10 | 4 |
| Distal third fractures | 2 | 3 |
| Spiral fractures (A1) | 26 (60%) | 10 (45%) (p = 0.29) |
| Transverse fractures (A3) | 15 (35%) | 11 (50%) (p = 0.29) |
| Wedge fractures (B2) | 3 | 1 |
| Multi-fragmentary fractures (C3) | 3 | 0 |
| Mean fracture displacement (mm) | 20.9 | 32.3 (p < 0.001) |
| Mean fracture angulation (degrees) | 20.2 | 29.2 (p = 0.01) |
| Bone to soft tissue ratio | 0.52 (range 0.33–0.83) | 0.48 (range 0.34–0.71) (p = 0.16) |
Nine patients had associated injuries (14%) which included two contralateral proximal humeral fractures, two radial head fractures, two distal radial fractures, two patients with rib fractures and one patient with an ankle fracture. There were two cases of radial nerve injury and one case of musculocutaneous nerve injury, which occurred at the time of the injury. All patients with nerve injuries had delayed unions and subsequently underwent surgical fixation, with full neurological recovery post-operatively.
The mean fracture displacement was 23 mm (range 0–60) prior to brace application and 18 mm (range 0–43) after application of the brace. The mean fracture angulation was 25° (range 0–60), prior to application of the brace and 15° (range 0–40) after application of the brace. The mean ratio of bone to soft tissues at the mid-humeral shaft was 0.50 (range 0.33–0.83) (Table 2).
The mean period of immobilisation in the brace was 11.9 weeks (range 6–16), and the mean time to fracture union was 12.9 weeks (range 8–40). The most common malunion after brace treatment was a varus deformity, with mean angulation of 7° (range 0–25) and a posterior angulation deformity, with mean angulation of 6.9° (range 0–20).
There were three cases of established non-union (5%) and 19 cases of delayed union (29%) of which 17 patients underwent surgical fixation (26% of total cohort). The three patients with established non-union were treated non-operatively as they were elderly and frail patients. Two of the patients with delayed union eventually healed with conservative treatment after 40 weeks (Figure 2).
Figure 2.
Flowchart demonstrating study inclusion and the union and management outcome of study patients.
Patients who underwent surgical fixation did so at a mean 12.6 weeks following injury (range 6–20). All patients who had surgery underwent open reduction and internal fixation using a plate. The mean time to union following surgical fixation was 16 weeks (range 6–24).
The mean displacement prior to brace application of patients who united was 21 mm and 32 mm in patients who went on to non-union or delayed union (p < 0.001). The mean displacement after brace application was 15 mm in patients who united and 24 mm in patients who sustained non-union or delayed union (p < 0.001) (Table 2).
The mean fracture angulation of patients prior to brace application was 20° in patients who united and 29° in patients who sustained delayed or non-union (p = 0.01). The mean fracture angulation of patients after brace application was 12° in patients who united and 18° in patients who sustained non or delayed union (p = 0.03) (Table 2).
Patients with fracture displacement of greater than 30 mm or angulation greater than 30°, prior to application of the brace, were particularly at risk of developing a delayed or non-union (odds ratio 7.6, p = 0.002, 95% confidence interval 2.0–28.9; and odds ratio 5.6, p = 0.005, 95% confidence interval 1.7–19.0).
There was no significant difference in patient age, gender, high or low energy injury, fracture location or bone to soft tissue ratio, when comparing patients who united and those who developed a delayed or non-union. There was an increased trend of delayed or non-union in patients with transverse fractures (50% versus 35%), but this was not statistically significant (Table 1). A post-hoc power calculation demonstrated that a sample size of 338 transverse fractures would be required to demonstrate a significant difference in this subgroup, and a total study sample of 438 humeral shaft fractures would be required to demonstrate a difference in union rates of different fracture locations.
Complications of brace treatment included six cases of shoulder or elbow stiffness and two cases of skin rash (complication rate 11%). There were two cases of non-union in the surgical cohort, both of whom underwent revision surgery (non-union rate 12%).
Discussion
Humeral shaft fractures are often regarded as a relatively benign injury. 6 This is largely due to the success of conservative treatment with functional bracing which was popularised by Sarmiento.1,5 In his original cohort, Sarmiento demonstrated a 98% union rate following functional bracing, which was then supported by a longer-term follow-up study demonstrating a 97% union rate.1,5
These results have been supported by other studies, albeit with slightly lower union rates. Koch et al. treated 67 patients with nine non-unions (13%). 6 Ekholm et al. treated 78 patients with a 90% union rate, with surgery performed for non-union at a mean 8.7 months following the time of injury. 3 Ali et al. assessed 138 humeral shaft fractures and demonstrated a union rate of 83%, with patients undergoing surgery for non-union at a mean 8.3 months. 8
This study has confirmed that functional bracing is a successful treatment method for the majority of patients with humeral shaft fractures, and 66% of patients had timely fracture union following functional bracing. It is important to note, however, that one third of patients sustained a delayed or non-union of which the majority went on to have surgical fixation. The results of this study are comparable to that of Harkin and Large who demonstrated a failure of conservative treatment in 33% of patients treated with functional bracing and therefore recommended acute surgical intervention. 13
The reason for the lower union rate in this study is uncertain but may relate to the more aggressive treatment of delayed union than in other studies. Patients who underwent surgical fixation in this study, did so at a mean of 12.6 weeks, which is much shorter than in other studies. Whilst it is possible that some of these fractures would have gone to unite, it is important not to underestimate the significant disability of prolonged brace therapy and delayed bony union. 12
This study has demonstrated that patients with markedly displaced and angulated fractures (greater than 30 mm displacement or 30° angulation) are at a higher risk of delayed or non-union, which has been supported by previous literature (Figures 3 and 4).6,7,11 The option of early surgical intervention should therefore be discussed with these patients. Unlike in some studies, the level of the fracture did not appear to affect the rate of union, and transverse fractures demonstrated only a non-significant trend to higher rates of delayed or non-union.6,15,16 Some authors have suggested that displacement, specifically fracture gap, is more important a risk factor for non-union than angulation. 10 In this study, however; both appeared to be significant predictors of delayed or non-union.
Figure 3.
Minimally displaced and angulated fracture demonstrating timely union with functional bracing.
Figure 4.
Markedly displaced and angulated fracture resulting in delayed union and requiring open reduction and internal fixation.
Patients who were treated by bracing did often have a varus and posterior angulation malunion; however, this was within the limits of previously published literature and has been demonstrated not to negatively impact on functional outcome.1,2,4,7
There were two cases of radial nerve injury in this study, both of whom developed delayed unions and subsequently underwent surgical fixation. Previous studies have, however, demonstrated that the majority of patients with radial nerve injuries can still expect to make a full recovery with conservative treatment and this in itself should not be considered an indication for surgical treatment.2,6 Obesity has also been suggested as a risk factor for failure of functional brace treatment.3,17 This was not supported by the bone to soft tissue ratio measurements we performed and suggests that functional bracing is still valid in patients with an extensive soft tissue envelope.
Some authors have recommended acute surgical intervention for all humeral shaft fractures. 13 Whilst the majority of patients make a good recovery following surgical fixation of humeral shaft fractures, it is also important to recognise that surgery is associated with potential risks and a complicate rate of up to 26% is quoted in the literature.2,7,9 In this study, two of the patients (11%) who underwent surgical fixation developed a non-union and required revision surgery, which is consistent with other studies and confirms that surgery is not universally successful.7,9
Limitations of this study include the fact that it was a retrospective review and relied upon the quality of information in the electronic patient database. Body mass index information was not routinely available for all patients and therefore the bone to soft tissue ratio was used as a surrogate measure. This has, however; not previously been validated and may have been influenced by other factors such as fracture haematoma. The number of patients with proximal or distal third fractures was also relatively low, which limited meaningful comparison of these fracture subtypes. In addition, the definition of delayed union used was not based on definitive radiographic and clinical findings but rather the combination of such findings together with the expertise of the assessing physician. Indeed, this probably more accurately represents the everyday practice of most orthopaedic surgeons and is therefore generalisable across United Kingdom practice.
This study has again demonstrated that functional bracing is successful in the vast majority of patients with humeral shaft fractures and should remain the first of line treatment in fractures without significant displacement or angulation. In patients, however, with significantly displaced or angulated fractures, early surgical fixation should be considered and should be part of the informed consent process for patients.
Although delayed surgical intervention can be performed for failed conservative treatment, it is important to acknowledge that functional outcomes for delayed surgery are generally worse, and early surgical intervention may offer patients the possibility to avoid morbidity associated with prolonged brace therapy, whilst maximising ultimate functional outcome.3,12
Conclusion
This study has demonstrated that the majority of patients with humeral shaft fractures can be treated successfully with functional bracing. There is, however, a 34% rate of delayed or non-union, which is significantly higher in patients with markedly displaced or angulated fractures (greater than 30 mm displacement or 30° angulation). Early surgical intervention should therefore be considered in this patient cohort.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent: The study was approved by the Research and Development Department at Musgrove Park Hospital, Taunton.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: BS.
Contributorship: CK and BS researched the literature and conceived the study. CK collected data for the study. CK and BS analysed the results. CK drafted the paper. BS reviewed the paper. CK and BS re-wrote the paper following reviewer comments.
ORCID iD: Cezary Kocialkowski https://orcid.org/0000-0001-7069-3859
Previous Communication: This study was present at the British Trauma Society meeting 7 November 2019.
References
- 1.Sarmiento A, Kinman PB, Galvin EG, et al. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am 1977; 59: 596–601. [PubMed] [Google Scholar]
- 2.Walker M, Palumbo B, Badman B, et al. Humeral shaft fractures: a review. J Shoulder Elbow Surg 2011; 20: 833–844. [DOI] [PubMed] [Google Scholar]
- 3.Ekholm R, Tidermark J, Törnkvist H, et al. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma 2006; 20: 591–596. [DOI] [PubMed] [Google Scholar]
- 4.Shields E, Sundem L, Childs S, et al. The impact of residual angulation on patient reported functional outcome scores after non-operative treatment for humeral shaft fractures. Injury 2016; 47: 914–918. [DOI] [PubMed] [Google Scholar]
- 5.Sarmiento A, Zagorski J, Zych G, et al. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am 2000; 82: 478–486. [DOI] [PubMed] [Google Scholar]
- 6.Koch P, Gross D, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg 2002; 11: 143–150. [DOI] [PubMed] [Google Scholar]
- 7.Pidhorz L. Acute and chronic humeral shaft fractures in adults. J Orthop Trauma 2015; 101: S41–S49. [DOI] [PubMed] [Google Scholar]
- 8.Ali E, Griffiths D, Obi N, et al. Nonoperative treatment of humeral shaft fractures revisited. J Shoulder Elbow Surg 2015; 24: 210–214. [DOI] [PubMed] [Google Scholar]
- 9.Mahabier K, Vogels M, Punt B, et al. Humeral shaft fractures: retrospective results of non-operative and operative treatment of 186 patients. Injury 2013; 44: 427–430. [DOI] [PubMed] [Google Scholar]
- 10.Neuhaus V, Menendez M, Kurylo JC, et al. Risk factors for fracture mobility six weeks after initiation of brace treatment of mid-diaphyseal humeral fractures. J Bone Joint Surg Am 2014; 96: 403–407. [DOI] [PubMed] [Google Scholar]
- 11.Bhandari M, Devereaux P, McKee M, et al. Compression plating versus intramedullary nailing of humeral shaft fractures – a meta-analysis. Acta Orthop 2006; 77: 279–284. [DOI] [PubMed] [Google Scholar]
- 12.Updegrove G, Mourad W, Abboud J. Humeral shaft fractures. J Shoulder Elbow Surg 2018; 27: e87–e97. [DOI] [PubMed] [Google Scholar]
- 13.Harkin F, Large R. Humeral shaft fractures: union outcomes in a large cohort. J Shoulder Elbow Surg 2017; 26: 1881–1888. [DOI] [PubMed] [Google Scholar]
- 14.AO Foundation and Orthopaedic Trauma Association. Fracture and dislocation classification compendium. J Orthop Trauma 2018; 32: S1–S170. [DOI] [PubMed] [Google Scholar]
- 15.Rutgers M, Ring D. Treatment of diaphyseal fractures of the humerus using a functional brace. J Orthop Trauma 2007; 20: 597–601. [DOI] [PubMed] [Google Scholar]
- 16.Ring D, Chin K, Taghinia AH, et al. Nonunion after functional brace treatment of diaphyseal. J Trauma 2007; 62: 1157–1158. [DOI] [PubMed] [Google Scholar]
- 17.Decomas A, Kaye K. Risk factors associated with failure of treatment of humeral diaphyseal fractures after functional bracing. J La State Med Soc 2010; 162: 33–35. [PubMed] [Google Scholar]