Abstract
Objective
To compare tenotomy versus tenodesis for the treatment of long head of the biceps tendon pathologies. The primary outcome was the shoulder functional outcome. The secondary outcomes consisted of postoperative pain, elbow flexion and forearm supination strengths and postoperative complications.
Methods
PubMed, MEDLINE, Google Scholar and Web of Science were searched until April 2020. Included studies were randomized controlled trials with a minimum 12 months’ follow-up.
Results
Both treatments had similar improvement on the Constant–Murley score at 6 months and 12 months. However, tenotomy had a significantly lower Constant–Murley score at two years with a mean difference of −1.13 (95% confidence interval −1.9, −0.35). Furthermore, tenotomy had a risk ratio of 2.46 (95% confidence interval 1.66, 3.64) for developing Popeye’s deformity. No significant difference was detected in other functional outcomes, pain, or elbow flexion and forearm strength indices.
Discussion
Tenodesis and tenotomy are both well-established techniques that similarly yield satisfactory outcomes. Despite that tenodesis had a statistically significant better Constant–Murley score at two years, this was clinically irrelevant. With the current evidence, we recommend either technique for the management of the long head of the biceps tendon pathologies.
Level of evidence
Therapeutic, Level II
Keywords: Long head, biceps, tenotomy, tenodesis, systematic review, meta-analysis
Introduction
Although the role of the long head of the biceps tendon (LHBT) is debated, any pathology that affects the LHBT can lead to anterior shoulder pain. 1 Several proposed mechanisms are implicated in the development of LHBT pathologies. 2 Degenerative changes due to the aging process are often associated with rotator cuff tears, which lead to LHBT tendinitis, partial and full thickness tears, and instability. Whereas, LHBT injuries in the younger population are associated with acute traumatic tears of the subscapularis tendon. Repetitive overhead activities, as in throwing athletes, lead to labral pathologies involving the LHBT anchor such as the superior labrum anterior-to-posterior (SLAP) lesions.
The management of isolated LHBT pathology is usually non-operative, with surgical treatment reserved for recalcitrant cases after the non-operative treatment. However, the surgical treatment for LHBT lesions is often carried out in the same setting of rotator cuff repairs, as 48–52% of cases with rotator cuff tears are associated with LHB tendinitis and subluxation/dislocation, respectively. 3
The two main surgical options are tenotomy and tenodesis. Tenotomy consists of releasing the LHBT tendon, whereas soft tissue tenodesis involves releasing and reattaching the tendon on the humerus. Tenotomy is a relatively safe, simple and quick procedure with shorter rehabilitation demands. On the other hand, tenodesis is less associated with cramping and cosmetic deformity despite being a more demanding procedure, higher rate of surgical complications and more rigorous postoperative rehabilitation protocols. 4 Latest meta-analyses on mixed randomized and non-randomized studies reported that tenodesis had superior functional outcomes with lower complications.5,6 However, since then several randomized trials were published on this topic that contradicted the findings of the aforementioned meta-analyses. Therefore, the aim of this study was to provide updated evidence consisting of randomized controlled trials (RCTs) comparing LHBT tenotomy versus tenodesis.
Materials and methods
This systematic review and meta-analysis was conducted with adherence to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). 7 The primary aim of this study was comparing the shoulder function between LHBT tenotomy and tenodesis. The secondary outcomes consisted of postoperative range of motion, strength, pain and complications.
Eligibility criteria
Studies comparing LHBT tenotomy versus tenodesis were sought. Included studies had to be RCTs (Level 1 and 2 studies) reporting functional outcome measures and having a minimum follow-up of 12 months. Non-randomized studies, abstracts and articles not published in English were excluded.
Information sources and search strategy
PubMed, MEDLINE, Google Scholar and Web of Science were searched until April 2020. The search strategy involved the use of the following keywords: ‘Biceps’ AND ‘Tenotomy’ AND ‘Tenodesis’. Studies were screened by titles and abstracts. A full-text review was performed if a study matched the eligibility criteria. Furthermore, the references of each eligible article were manually sought to ensure no eligible studies were missed. The search strategy was performed by two authors independently.
Data collection process and data items
Data collection forms were used independently by two authors. The data items that were collected included: the first authors’ surnames, study year and location, age, sex, number of patients, the treatments performed, follow-up time points, the Constant–Murley Score (CMS), the American Shoulder and Elbow Surgeons (ASES) scores, the visual analogue scale (VAS) for pain, biceps cramping pain, bicipital groove pain, forearm supination and elbow flexion strength indices, and complications developed after each treatment.
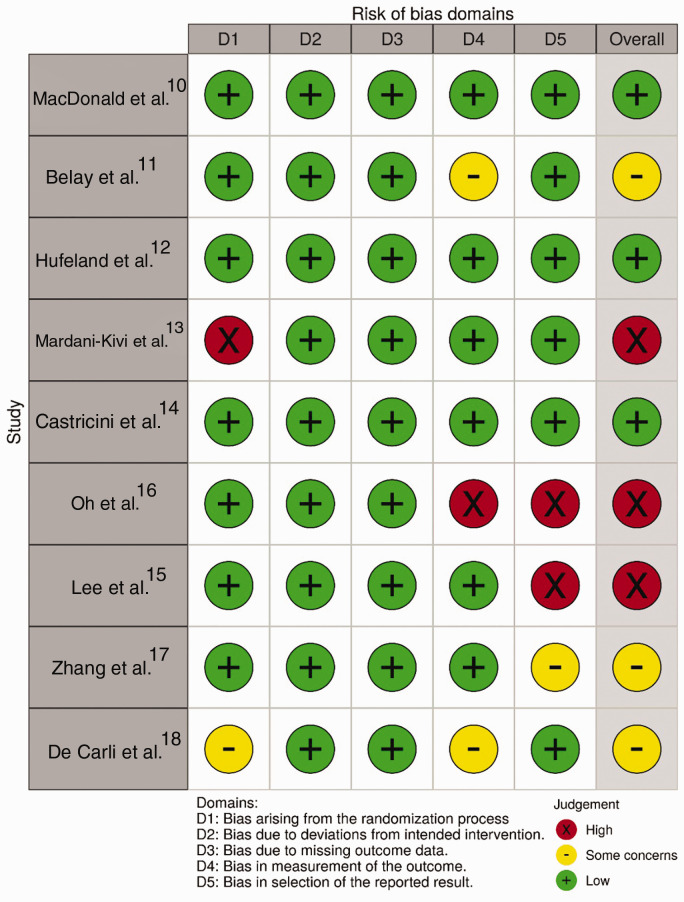
Risk of bias in individual studies
The qualitative analysis was performed with the revised Cochrane risk-of-bias tool for randomized trials (RoB 2). 8 The tool contains five domains which assess the randomization, adherence to intended treatments, missing outcomes, measurement bias and reporting bias. Each study was assessed by two authors independently.
Quantitative synthesis
The quantitative synthesis was performed with the use of Stata/IC (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC). The outcomes were estimated with the use of 95% confidence interval (CI), and a significant difference in outcomes was considered statistically significant if the P value was less than 0.05. The mean difference (MD) was used for estimating the treatment effect of continuous outcomes. The Hedges G standard mean difference (SMD) was used for estimating the effect on the postoperative strength indices due to potential variability in measurement among studies. The risk ratio (RR) was utilized for dichotomous outcomes. The meta-analytic models were based on random-effects with the use of the DerSimonian–Laird method as a heterogeneity variance estimator. If a study reported medians or ranges instead of means and standard deviations, the conversion formulas by Hozo et al. 9 were used.
Results
Study selection
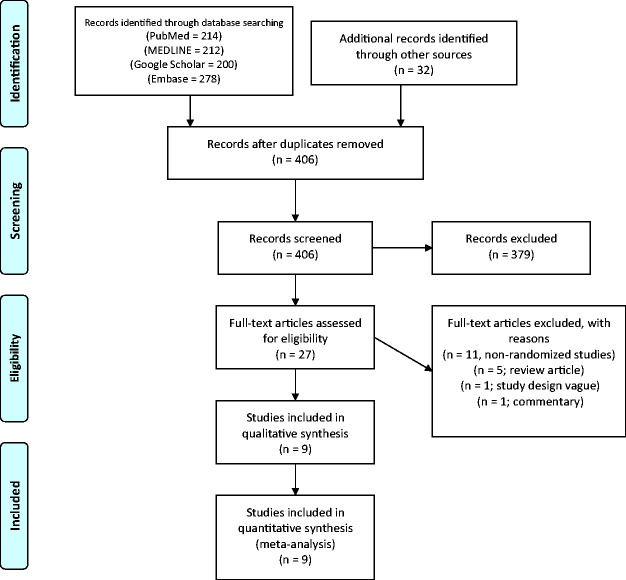
The search strategy resulted in 936 articles of which 530 articles were excluded, thus leaving 406 articles for searching by titles and abstracts. A total of 378 articles were excluded, resulting in 28 articles eligible for full-text reviews. Of the 28 articles, 18 articles were excluded which resulted in nine eligible articles. All nine eligible studies were included in the qualitative and quantitative analyses. The PRISMA flowchart is displayed in Figure 1.
Figure 1.
The search strategy flowchart.
Study characteristics
Table 1 presented the characteristics of the included studies. A total of 684 patients were included, of which 338 underwent LHBT tenotomy and 346 underwent tenodesis. The mean age among studies ranged between 51.5 and 62.9 years. The follow-up was at a mean of 24 months in all studies except in the study by Hufeland et al. 12 which had a follow-up of 12 months.
Table 1.
Characteristics of included studies.
| Author | Country | Mean age (range or ± SD) | Sex (Male/ Female) | Number | Tenodesis technique | Follow-up intervals | Outcome measures |
|||
|---|---|---|---|---|---|---|---|---|---|---|
| Function | Pain | Strength | Complications | |||||||
| MacDonald et al. 10 | Canada | TT: 56.3 (8.1) TD: 58.7 (10.9) | TT: 45/12 TD: 47/10 | TT: 57 TD: 57 | Suprapectoral and subpectoral | 3, 6, 12 and 24 mo | ASES | VAS Cramping | Elbow flexion Forearm supination | Popeye’s deformity Reoperations Tenodesis failure |
| Belay et al. 11 | UK/USA | TT: 57.7 ± 8.7 TD: 52.9 ± 10.8 | TT: 19/1 TD: 12/2 | TT: 20 TD: 14 | Suprapectoral | 3 and 24 mo | ASES | VAS Cramping Bicipital groove | NR | Popeye’s deformity Adhesive capsulitis Tenodesis failure |
| Hufeland et al. 12 | Germany | TT: 52.8 (26–62) TD: 51.5 (37–63) | TT: 4/7 TD: 7/2 | TT: 11 TD: 9 | Suprapectoral | 6 and 12 mo | CMS ASES | Cramping | Elbow flexion Forearm supination | Popeye’s deformity |
| Mardani-Kivi et al. 13 | Iran | TT: 54.5 ± 5.3 TD: 55.5 ± 5.2 | TT: 20/9 TD: 22/11 | TT: 29 TD: 33 | Subpectoral | 6, 12, 24 mo | CMS | VAS Cramping | NR | Popeye’s deformity |
| Castricini et al. 14 | Italy | TT: 59.9 (40–71) TD: 57.1 (40–70) | TT: 14/17 TD: 7/17 | TT: 31 TD: 24 | Suprapectoral | 6 and 24 mo | CMS | VAS Cramping | Elbow flexion | Popeye’s deformity Rotator cuff retear |
| Lee et al. 15 | South Korea | TT: 62.8 (55–77) TD: 62.9 (50–75) | TT: 11/45 TD: 18/54 | TT: 56 TD: 72 | Suprapectoral | Mean follow-up: Tenotomy: 25.1 mo Tenodesis: 19.7 mo | CMS ASES | VAS | Elbow flexion Forearm supination | Popeye’s deformity Rotator cuff retear Tenodesis failure |
| Oh et al. 16 | South Korea | TT: 61 (53–69) TD: 56.6 (42–76) | TT: 9/18 TD: 21/10 | TT: 27 TD: 31 | Suprapectoral | Mean follow-up: Tenotomy: 22 mo Tenodesis: 21.5 mo | ASES | VAS Cramping Bicipital groove | Elbow flexion Forearm supination | Popeye’s deformity Rotator cuff retear |
| Zhang et al. 17 | China | TT: 61 (55–67) TD: 61 (55–71) | TT: 36/41 TD: 35/39 | TT: 77 TD: 74 | Suprapectoral | 24 mo | CMS | VAS Cramping | Elbow flexion Forearm supination | Popeye’s deformity |
| De Carli et al. 18 | Italy | TT: 59.6 ± 8.7 TD: 56.3 ± 3.9 | Overall: 48/17 | TT: 30 TD: 35 | Intracuff | Mean follow-up Tenotomy: 23 mo Tenodesis: 25 mo | CMS | Biceps cramping | Elbow flexion | Popeye’s deformity |
ASES: American Shoulder and Elbow Surgeons score; CMS: Constant–Murley Score; mo: months; NR: not reported; SD: standard deviation; SST: simple shoulder test; TD: tenodesis; TT: tenotomy; VAS: visual analogue scale.
The LHBT pathologies were degenerative tears, tenosynovitis, subluxation and SLAP lesions. Eight10,11,13–18 out of total nine studies included concomitant rotator cuff tears which were reparable, with only the study by Hufeland et al. 12 including SLAP lesions without rotator cuff tears. The status of the rotator cuff tear was variable among these studied ranging from high-grade partial-thickness tears to varying sizes of full-thickness tears (small to large).
The rehabilitation protocol in the included studies was variable. Eight of the included studies had rotator cuff repair which had a brief period of immobilization with an abduction brace for 3–6 weeks depending on the degree of rotator cuff tear. Gradual passive and active range of motion training were instituted after brace removal and strengthening began at 4–12 weeks following surgery. Return to sports and manual labour was permitted at six months. No immobilization was performed in the study by Hufeland et al. 12 as patients had isolated LHBT injuries.
Eight out of nine studies had no difference in rehabilitation between tenotomy and tenodesis. However, in the study by Zhang et al., 17 the tenodesis group was restricted with a return to elbow active range of motion allowed at six weeks postoperatively and unrestricted use of the biceps muscle at 16–20 weeks postoperatively. The tenotomy group had only elbow immobilization for one week in that study. The postoperative rehabilitation in the study by De Carli et al. 18 was not detailed.
Risk of bias within studies
With the use of the Cochrane RoB 2 tool, three studies were well designed with low risk of bias,10,12,14 three studies had some concerns,11,17,18 and three studies had a high risk for bias.13,15,16 **Figure 2 summarizes the risk of bias assessment across the five domains of bias.
Figure 2.
The Cochrane risk of bias assessment.
Results of individual studies
Shoulder function scores
The functional outcomes reported were the CMS in six studies12–15,17,18 and ASES in five studies.10–12,15,16 The functional outcomes were not statistically different between LHBT tenotomy and tenodesis at 6, 12 or 24 months in all randomized trials reporting shoulder function.
Pain outcomes
The VAS score for pain was reported in seven studies out of nine. Zhang et al. 17 found a significant reduction in pain in the tenotomy group at two weeks (P < 0.001) postoperatively with no difference at four weeks. At longer follow-up points, only the study by Mardani-Kivi et al. 13 showed significantly improved pain at 12 and 24 months in favour of tenotomy. However, other studies did not report any significant difference at 6, 12 and 24 months.10,11,14–16
Subjective biceps cramping pain was reported in seven studies out of nine.10–14,16,17 No significant differences were found in all included studies in terms of the subjective cramping pain except in the study by Mardani-Kivi et al., 13 which reported cramping in 31% of patients who had tenotomy versus 0% in tenodesis (P < 0.001).
Bicipital groove tenderness was reported in two studies, and no significant difference was reported between LHBT tenotomy or tenodesis.11,16
Elbow flexion and forearm supination strengths
The elbow flexion strength was reported in seven studies.10,12,14–18 No differences were found in elbow flexion strength indices at 6, 12 and 24 months. However, Hufeland et al. 12 found that tenodesis achieved significant improvement in elbow flexion at six months, despite no significant difference detected at 12 months.
The postoperative forearm supination strength was reported in five studies.10,12,15–17 Only the study by Oh et al. 16 reported superior supination strength for LHBT tenodesis at 24 months, whereas the other four studies found no significant difference between tenotomy and tenodesis.
Complications
The postoperative complications in all included studies are summarized in Table 2. The incidence of Popeye deformity was found to be significantly higher in LHBT tenotomy in five studies,10,13–15,18 whereas the other four studies reported no significant difference.
Table 2.
Summary of postoperative complications.
| Author | Tenotomy | Tenodesis |
|---|---|---|
| MacDonald et al. 10 | Popeye’s sign = 17 Reoperation = 5 | Popeye’s sign = 5 Reoperation = 4 Tenodesis failure = 0 |
| Belay et al. 11 | Popeye’s sign = 5 Adhesive capsulitis = 1 | Popeye’s sign = 1 Adhesive capsulitis = 1 Tenodesis failure = 1 |
| Hufeland et al. 12 | Popeye’s sign = 3 | Popeye’s sign = 3 |
| Mardani-Kivi et al. 13 | Popeye’s sign = 7 | Popeye’s sign = 1 |
| Castricini et al. 14 | Popeye’s sign = 18 Cuff retear = 1 | Popeye’s sign = 5 Cuff retear = 1 |
| Lee et al. 15 | Popeye’s sign = 11 Rotator cuff retear = 9 | Popeye’s sign = 4 Rotator Cuff retear = 11 Tenodesis failure = 7 |
| Oh et al. 16 | Popeye’s sign = 10 Cuff retear = 5 | Popeye’s sign = 8 Cuff retear = 2 |
| Zhang et al. 17 | Popeye’s sign = 7 | Popeye’s sign = 2 |
| De Carli et al. 18 | Popeye’s sign = 5 | None |
Three studies reported tenodesis failure rate at 24 months’ follow-up. Lee et al. 15 reported that 7 out 72 (10%) patients had failure of the LHBT tenodesis, Belay et al. 11 reported one case of tenodesis failure in 14 patients and MacDonald et al. 10 reported no tenodesis failures in 54 patients.
Revision surgeries were only reported by MacDonald et al. with no difference between tenotomy (five cases) and tenodesis (four cases). In all studies, no differences were detected retears for concomitantly repaired rotator cuffs.
Synthesis of results
Constant-Murley Scores
The comparison was performed on three studies12–14 at six months, two studies at 12 months,12,13 and four studies13,14,17,18 at two years postoperatively (Supplementary File 1). The meta-analytic comparison between tenotomy and tenodesis resulted in an MD of −0.67 points (95% CI −3.75, 2.4; P = 0.67; I2 = 22%) at six months; −5.08 (95% CI −14.02, 3.87; P = 0.27; I2 = 73.05%) at 12 months and −1.13 (95% CI −1.9, −0.36; P = <0.001; I2 = 0.00%) at two years.
The American Shoulder and Elbow Surgeons scores
The comparison was performed on two studies at 6 and 12 months,10,12 and on three studies at two years11,16 (Supplementary File 2). The meta-analytic comparison between tenotomy and tenodesis resulted in an MD of −5.36 (95% CI −26, 15.34; P = 0.61; I2 = 78.5%) at six months; −7.59 (95% CI −26.39, 11.21; P = 0.43; I2 = 80.5%) at 12 months and 0.26 (95% CI −3.7, 4.22; P = 0.9; I2 = 6.48%) at two years.
Postoperative pain
The VAS for pain comparison was performed on three studies13,14 at six months, two studies10,13 at 12 months and four studies11,13,14,16 at two years (Supplementary File 3). The comparison between tenotomy and tenodesis resulted in an MD of 0.17 (95% CI −0.16, 0.51; P = 0.3; I2 = 1.02%) at six months; an MD of −0.25 (95% CI −1.10, 0.61; P = 0.57; I2 = 56.21) at 12 months and an MD of −0.16 (95% CI −0.57, 0.25; P = 0.44; I2 = 43.79%) at two years.
In addition, the incidence subjective cramping pain was pooled in six studies. The RR for tenotomy when compared with tenodesis was 1.43 for subjective cramping pain at the latest follow-up point (95% CI 0.57, 3.58; P = 0.44; I2 = 38.48%) (Supplementary File 4).
Postoperative strength
Elbow strength and forearm supination indices were pooled at 6, 12 months and at two years. When comparing tenotomy to tenodesis, the SMD for elbow strength was 0.28 (95% CI −0.12, 0.69; P = 0.17; I2 = 11.13%) at six months; 0.14 (95% CI −0.08, 0.37; P = 0.22; I2 = 0%) at 12 months and 0 (95% CI −0.26, 0.26; P = 1; I2 = 0%) at final follow-up. The SMD for forearm supination when comparing tenotomy to tenodesis was 0.297 (95% CI −0.06, 0.65; P = 0.11; I2 = 0%) at six months; −0.84 (95% CI −2.5, 0.8; P = 0.31; I2 = 96.7%) at 12 months and −0.24 (95% CI −0.77, 0.3; P = 0.38; I2 = 68.6%) at two years. Table 3 presents the comparison of the pooled strength indices.
Table 3.
Comparison of elbow flexion strength and forearm supination strength between long head of biceps tendon tenodesis versus tenotomy.
| Outcome measure | Study ID | Follow-up | SMD | 95% CI | P value | % Weight | Heterogeneity (I2) |
|---|---|---|---|---|---|---|---|
| Elbow flexion strength | MacDonald et al. 10 Hufeland et al. 12 Random-effects model | 6 mo | 0.39 −0.11 0.28 | −0.001, 0.78 −0.96, 0.73 −0.12, 0.69 | 0.17 | 78.6 21.4 | 11.13% |
| MacDonald et al. 10 Hufeland et al. 12 Oh et al. 16 Lee et al. 15 Random-effects model | 12 mo | 0.31 −0.08 −0.14 0.17 0.14 | −0.08, 0.7 −0.93, 0.76 −0.65, 0.37 −0.17, 0.52 −0.08, 0.37 | 0.22 | 32.5 7 19.2 41.25 | 0.00% | |
| Zhang et al. 17 De Carli et al. 18 Random-effects model | 2 years | 0.00 0.00 0.00 | −0.32, 0.32 −0.48, 0.48 −0.26, 0.26 | 1.00 | 69.7 30.3 | 0.00% | |
| Forearm supination strength | MacDonald et al. 10 Hufeland et al. 12 Random-effects model | 6 mo | 0.351 0.018 0.297 | −0.04, 0.75 −0.83, 0.86 −0.06, 0.65 | 0.11 | 83.82 16.18 | 0.00% |
| MacDonald et al. 10 Hufeland et al. 12 Lee et al. 15 Random-effects model | 12 mo | −0.08 0.085 −2.5 −0.84 | −0.45, 0.29 −0.76, 0.93 −2.94, −2 −2.5, 0.8 | 0.31 | 34.23 31.87 33.90 | 96.7% | |
| Oh et al. 16 Zhang et al. 17 Random-effects model | 2 years | −0.55 0.00 −0.24 | −1.07, −0.04 −0.32, 0.32 −0.77, 0.3 | 0.38 | 42.85 57.15 | 68.6% |
mo: months; SMD: standardized mean difference. Bold text reflects the pooled estimates with their P values and heterogeneity.
Postoperative complications
The incidence of Popeye’s deformity was reported in all studies, and the RR was 2.46 when comparing tenotomy to tenodesis at the latest follow-up point (95% CI 1.66, 3.64; P < 0.001; I2 = 1.77%) (Supplementary File 5). The overall tenodesis failure occurred in 2.3% (8 out of 346 tenodesis cases). The overall complication rate was not pooled due to the heterogeneity of the complications reported across studies.
Discussion
This systematic review was conducted to compare LHBT tenotomy versus tenodesis due to the controversial results in the recent literature. Our findings have shown that both treatments achieved satisfactory patient-reported outcomes on the CMS. No significant difference was detected at 12 months; however, there was a statistically significant difference in favour of tenodesis at two years postoperatively (MD = −1.13; 95% CI −1.9, −0.36). It is important to acknowledge that this difference is not clinically relevant since the minimally important clinical difference for the CMS has been reported to be between 10 and 15 points. 19 All of the RCTs12–15,17 comparing both treatments and most comparative cohort studies20–22 have found no difference in CMS up to two years of follow-up.
Furthermore, in this systematic review there were no significant differences detected in the ASES scores at 6 months, 12 months and two years of follow-up. Despite that each pooled follow-up point had only 2–3 studies, our findings were similar to the findings of each trial individually.10–12,15,16
The LHBT has been notable as a source for anterior shoulder pain. 1 Both tenotomy and tenodesis have been effective in achieving improvement in pain relief. However, tenotomy has been associated with subjective cramping pain in up to 20% in a case series on 104 patients. 23 Authors favouring tenodesis have argued that the prevalent pain following tenotomy can lead to delay in returning to work and less than optimal outcomes with individuals with high functional demands. 24 We found no significant difference between both treatment regarding pain on the VAS at a follow-up of two years. Moreover, the presence of subjective cramping pain was statistically insignificant between both treatments with most of the cramping resolving or improving within a period of 2–24 months postoperatively.14,16,17 However, MacDonald et al. 10 found that the cramping pain was relatively unchanged over time with a follow-up period of 24 months.
Several studies have found that tenodesis achieves superior forearm supination and elbow flexion strength. In the trial by Lee et al., tenodesis had significantly stronger supination (P = 0.02). Moreover, another study on 35 patients demonstrated that tenotomy had significantly larger decrements in supination peak torque. 25 In the case series by Kelly et al., 26 38% of patients who underwent tenotomy had biceps fatigue discomfort after resisted elbow flexion. Hence, tenodesis has been recommended for younger individuals with high occupational or recreational demands. On the contrary, most RCTs on this matter refuted such findings. This meta-analysis did not demonstrate any superiority of one treatment over the other in forearm supination or elbow flexion strength at 6, 12 and 24 months postoperatively.
Regarding cosmetic outcomes in the management of the LHBT, tenotomy has been associated with significantly higher risk of Popeye’s deformity reaching up to 43%. 27 Therefore, biceps tenodesis has been recommended for reducing the cosmetic deformity. However, several surgeons have suggested techniques to circumvent the high rate Popeye’s deformity in tenotomy by minimizing the LHBT distal retraction. Such techniques described include releasing part of the superior labrum along with the LHBT 28 or by using a compressive wrap around the arm. 29 It is noteworthy that tenodesis does not eliminate the risk of Popeye’s deformity. In the trial by Oh et al., both treatments had no significant difference in the development of Popeye’s deformity with a rate of 37% for tenotomy and 26% for tenodesis. This can be attributed to tenodesis failure or inappropriate tension at the site of tenodesis. We found that tenotomy had 2.5 times the risk for developing a Popeye’s deformity compared to tenodesis which was statistically significantly.
Several limitations exist for this meta-analysis. First, the intrinsic risk of bias within the included studies cannot be adjusted. For example, two included randomized trials had a level of evidence of 2 which reduces the overall strength of this study. Second, included studies did not utilize similar outcome measures which prevented pooling more data for the CMS score and have prevented meta-analytic comparisons of other validated outcome measures. For example, our analysis at two years for the CMS score was statistically significant but not clinically relevant. This could have resulted in a clinically meaningful difference had we been able to pool more data. Third, due to limited number of studies we could not conduct meta-regression analyses based on the technique of biceps tenodesis such as suprapectoral or the subpectoral techniques, which could influence the functional outcomes or complication rates. 30 In a recent retrospective review of 1526 LHBT tenodesis cases, subpectoral tenodesis had high risk of revision when compared to tenodesis in the suprapectoral position. Moreover, soft tissue tenodesis had higher anterior shoulder pain and subjective weakness when compared with implant-based tenodesis. 31 Fourth, the length of follow-up of two years might not be sufficient to detect a difference in outcomes between both treatments.
The strength of this systematic review is that it is the first of its kind on RCTs only, thereby offering a higher level of evidence on this matter. Our results have found no significant difference on functional outcomes between both treatments which is different than previous meta-analyses. All previously published meta-analyses reported superior results in favour of LHBT tenodesis, and all were based on mixed cohort and randomized studies.5,6 Another strength to this study is that we were able to analyse functional outcomes at different time intervals from six months and up to two years of follow-up.
In conclusion, LHBT tenodesis and tenotomy are both well-established techniques that similarly yield satisfactory outcome in the treatment of LHBT pathologies. There was no difference between both techniques in terms of shoulder functional outcomes. Moreover, no difference between both techniques was found in terms of pain, elbow flexion or forearm supination strength indices. Biceps tenotomy had 2.5 times the risk for developing Popeye’s deformities when compared to tenodesis. With the current evidence, we recommend either technique for the management of the LHBT tenotomy. Given that tenodesis has shown a statistically significant but clinically irrelevant improvement in CMS at two years, further large prospective comparative studies are warranted to determine whether tenodesis truly leads to superior functional outcomes as demonstrated.
Supplemental Material
Supplemental material, sj-pdf-1-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Supplemental material, sj-pdf-2-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Supplemental material, sj-pdf-3-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Supplemental material, sj-pdf-4-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Supplemental material, sj-pdf-5-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Footnotes
Contributorship: AFA and AT researched the literature. AFA performed the statistical analysis and wrote both the method and result sections. AT wrote the introduction section and submitted the manuscript through the journal portal. SM and GOA assisted in editing the discussion section. MAA and BAZ conceived the study and provided overall supervision of conducting this review. All authors reviewed and edited the manuscript and approved the final version.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent: Not applicable.
Guarantor: AFA.
ORCID iDs: Abdulaziz F Ahmed https://orcid.org/0000-0002-1902-3291
Ammar Toubasi https://orcid.org/0000-0003-2899-883X
Shady Mahmoud https://orcid.org/0000-0002-3077-3317
Supplemental material: Supplemental material for this article is available online.
References
- 1.Chalmers PN, Cip J, Trombley R, et al. Glenohumeral Function of the Long Head of the Biceps Muscle: An Electromyographic Analysis. Orthop J Sports Med 2014; 2(2): 2325967114523902. [DOI] [PMC free article] [PubMed]
- 2.Krupp RJ, Kevern MA, Gaines MD, et al. Long head of the biceps tendon pain: differential diagnosis and treatment. J Orthop Sports Phys Ther 2009; 39: 55–70. [DOI] [PubMed] [Google Scholar]
- 3.Walch G, Edwards T, Boulahia A, et al. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg 2005; 14: P238–P246. [DOI] [PubMed] [Google Scholar]
- 4.Virk MS, Cole BJ. Proximal biceps tendon and rotator cuff tears. Clin Sports Med 2016; 35: 153–161. [DOI] [PubMed] [Google Scholar]
- 5.Ge H, Zhang Q, Sun Y, et al. Tenotomy or tenodesis for the long head of biceps lesions in shoulders: a systematic review and meta-analysis. PLoS One 2015; 10: e0121286–e0121286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Na Y, Zhu Y, Shi Y, et al. A meta-analysis comparing tenotomy or tenodesis for lesions of the long head of the biceps tendon with concomitant reparable rotator cuff tears. J Orthop Surg Res 2019; 14: 370–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Int J Surg 2010; 8: 336–341. [DOI] [PubMed] [Google Scholar]
- 8.Page MJ, McKenzie JE, Higgins JPT. Tools for assessing risk of reporting biases in studies and syntheses of studies: a systematic review. BMJ Open 2018; 8: e019703–e019703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005; 5: 13–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacDonald P, Verhulst F, McRae S, et al. Biceps tenodesis versus tenotomy in the treatment of lesions of the long head of the biceps tendon in patients undergoing arthroscopic shoulder surgery: a prospective double-blinded randomized controlled trial. Am J Sports Med 2020, pp. 48(6): 1439–1449–48(6): 1439–1449. [DOI] [PubMed] [Google Scholar]
- 11.Belay ES, Wittstein JR, Garrigues GE, et al. Biceps tenotomy has earlier pain relief compared to biceps tenodesis: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc 2019; 27: 4032–4037. [DOI] [PubMed] [Google Scholar]
- 12.Hufeland M, Wicke S, Verde PE, et al. Biceps tenodesis versus tenotomy in isolated LHB lesions: a prospective randomized clinical trial. Arch Orthop Trauma Surg 2019; 139: 961–970. [DOI] [PubMed] [Google Scholar]
- 13.Mardani-Kivi M, Karimi Mobarakeh M, Keyhani S, et al. Treatment of long head of biceps tendon lesions together with rotator cuff tears: which method is preferred? Tenotomy or tenodesis. Techniq Shoulder Elbow Surg 2018; 19: 101–105. [Google Scholar]
- 14.Castricini R, Familiari F, De Gori M, et al. Tenodesis is not superior to tenotomy in the treatment of the long head of biceps tendon lesions. Knee Surg Sports Traumatol Arthrosc 2018; 26: 169–175. [DOI] [PubMed] [Google Scholar]
- 15.Lee HJ, Jeong JY, Kim CK, et al. Surgical treatment of lesions of the long head of the biceps brachii tendon with rotator cuff tear: a prospective randomized clinical trial comparing the clinical results of tenotomy and tenodesis. J Shoulder Elbow Surg 2016; 25: 1107–1114. [DOI] [PubMed] [Google Scholar]
- 16.Oh JH, Lee YH, Kim SH, et al. Comparison of treatments for superior labrum-biceps complex lesions with concomitant rotator cuff repair: a prospective, randomized, comparative analysis of debridement, biceps tenotomy, and biceps tenodesis. Arthroscopy 2016; 32: 958–967. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Q, Zhou J, Ge H, et al. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc 2015; 23: 464–469. [DOI] [PubMed] [Google Scholar]
- 18.De Carli A, Vadala A, Zanzotto E, et al. Reparable rotator cuff tears with concomitant long-head biceps lesions: tenotomy or tenotomy/tenodesis? Knee Surg Sports Traumatol Arthrosc 2012; 20: 2553–2558. [DOI] [PubMed] [Google Scholar]
- 19.McKee RC, Whelan DB, Schemitsch EH, et al. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am 2012; 94: 675–684. [DOI] [PubMed] [Google Scholar]
- 20.Boileau P, Baque F, Valerio L, et al. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am 2007; 89: 747–757. [DOI] [PubMed] [Google Scholar]
- 21.Cho NS, Cha SW, Rhee YG. Funnel tenotomy versus intracuff tenodesis for lesions of the long head of the biceps tendon associated with rotator cuff tears. Am J Sports Med 2014; 42: 1161–1168. [DOI] [PubMed] [Google Scholar]
- 22.Koh KH, Ahn JH, Kim SM, et al. Treatment of biceps tendon lesions in the setting of rotator cuff tears: prospective cohort study of tenotomy versus tenodesis. Am J Sports Med 2010; 38: 1584–1590. [DOI] [PubMed] [Google Scholar]
- 23.Meeks BD, Meeks NM, Froehle AW, et al. Patient satisfaction after biceps tenotomy. Orthop J Sports Med 2017, pp. 5(5): 2325967117707737–5(5): 2325967117707737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Romeo AA. The proximal biceps tendon. Clin Sports Med 2016; 35: xv–xvi. [DOI] [PubMed] [Google Scholar]
- 25.Wittstein JR, Queen R, Abbey A, et al. Isokinetic strength, endurance, and subjective outcomes after biceps tenotomy versus tenodesis: a postoperative study. Am J Sports Med 2011; 39: 857–865. [DOI] [PubMed] [Google Scholar]
- 26.Kelly AM, Drakos MC, Fealy S, et al. Arthroscopic release of the long head of the biceps tendon: functional outcome and clinical results. Am J Sports Med 2005; 33: 208–213. [DOI] [PubMed] [Google Scholar]
- 27.Slenker NR, Lawson K, Ciccotti MG, et al. Biceps tenotomy versus tenodesis: clinical outcomes. Arthroscopy 2012; 28: 576–582. [DOI] [PubMed] [Google Scholar]
- 28.Bradbury T, Dunn WR, Kuhn JE. Preventing the popeye deformity after release of the long head of the biceps tendon: an alternative technique and biomechanical evaluation. Arthroscopy 2008; 24: 1099–1102. [DOI] [PubMed] [Google Scholar]
- 29.Rudzki JR and Shaffer BS. Arthroscopic treatment of biceps tendonopathy. In: Miller M, editor. Operative Techniques in Sports Medicine Surgery. 2nd ed. Philadelphia: Wolters Kluwer, 2012, pp.51–60.
- 30.Gombera MM, Kahlenberg CA, Nair R, et al. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med 2015; 43: 1077–1083. [DOI] [PubMed] [Google Scholar]
- 31.McCrum CL, Alluri RK, Batech M, et al. Complications of biceps tenodesis based on location, fixation, and indication: a review of 1526 shoulders. J Shoulder Elbow Surg 2019; 28: 461–469. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Supplemental material, sj-pdf-2-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Supplemental material, sj-pdf-3-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Supplemental material, sj-pdf-4-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow
Supplemental material, sj-pdf-5-sel-10.1177_1758573220942923 for Long head of biceps tenotomy versus tenodesis: a systematic review and meta-analysis of randomized controlled trials by Abdulaziz F Ahmed, Ammar Toubasi, Shady Mahmoud, Ghalib O Ahmed, Mohammed Al Ateeq Al Dosari and Bashir A Zikria in Shoulder & Elbow