Abstract
Background
Total hip arthroplasty (THA) with ceramic-on-ceramic (CoC) was created to minimise wear debris and aseptic loosening. A decade ago, a meta-analysis showed a 10-year survival rate of just 89%. Based on the excellent tribology of the current CoC, significant improvement of implant survivorship is expected. In patients younger than 60, we conducted a meta-analysis to assess 10-year survival and complications after using current primary CoC THA.
Materials and methods
PubMed, Scopus, EMBASE, Virtual Health Library, and Cochrane Library were used to scan for published trials that met the inclusion criteria until January 2019. The qualified studies were subjected to a systematic review and proportional analysis, and the randomised controlled trials (RCTs) were included in a comparison meta-analysis.
Results
Thirteen studies were included 156 findings. The total number of hips was 2278. Nine studies were cohort, and four were RCTs between ceramic and polyethylene cups. The analysis revealed an average age of 44 years (range 24–54). The 10-year survival 96% (95% CI; 95.4–96.8%), aseptic loosening rate 0.516. (95% CI; 0.265–0.903), ceramic fracture rate 0.620 (95% CI; 0.34–1.034) and squeaking rate 2.687 (95% CI; 1.279–4.593). A comparison meta-analysis revealed the risk ratio (RR) for revision was 0.27 (95% CI; 0.15–0.47), and for aseptic loosening 0.15 (0.03–0.70) favouring CoC, while RR for component fracture was 1.62 (95% CI; 0.27–9.66) favouring the polyethylene.
Conclusion
In patients under sixty, current CoC THAs are correlated with better 10-year outcomes than before and have high survivorship rates.
Level of evidence: Level I.
Keywords: Ceramic, Arthroplasty, Hip, Non-elderly
Background
With longer life expectancy, total hip arthroplasties (THA) in young patients are likely to wear out faster with higher rates of aseptic loosening. While there is agreement on cementless fixation, there is no such agreement on articulating surfaces [1].
Ceramic-on-ceramic (CoC) THAs have low friction and wear due to their mechanical and chemical properties and surface lubrication by joint fluid, resulting in less osteolysis than other bearing surfaces currently available [2, 3].
Ceramics' brittleness, on the other hand, raises the possibility of component fracture. The replaced joint's squeaks are also a cause of concern. In the young and active patient, the best bearing surface for THA is still up for discussion [4–7]. So, continuous research to develop CoC bearings' properties could have more prolonged survival and fewer problems in the 3rd- and 4th-generation ceramic bearings [8].
Thus, we performed a systemic review and meta-analysis of studies that reported 10-year survival based on the CoC bearing of the 3rd-and 4th-generation CoC THAs in patients younger than 60 to address their complications and survival rate.
Materials and methods
Search strategy
In Jan 2019, the study was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA) rules [9]. Electronic searches were conducted in PubMed, Scopus, EMBASE, Virtual Health Library, and the Cochrane Library to identify relevant articles.
Medical Subject Headings (MeSH) terms and free words were used, including ceramic (CoC, alumina) and hip arthroplasty (THA, total hip replacement). Two investigators reviewed each article independently to identify the publication relevance to the eligibility criteria included primary THA for patients < 60 years with CoC bearing surfaces of the 3rd- (Forte) and 4th-(Delta) generations with reported 10-year survival. Studies included near 10-year results or more of Biolox forte or delta, full text in English, prospective or retrospective, cohort or RCTs were included.
Exclusion criteria were animal studies, case reports or studies with less than 15 patients, scientific correspondence, poster, conference, thesis, guidelines, and comments. Studies that included revision surgeries, insufficient data, or unclear identification of the patient population, or used implants were also excluded.
Data extraction
After eligibility of any study, two investigators independently extracted data from each report that included the first author's family name, year of publication, material design, patient demographic data, enrollment period, follow-up period, type of implant fixation, the bearing surfaces generation, and the outcomes.
Outcome measures
A proportional analysis for the eligible studies included the primary outcome, i.e. 10-year implant survival, was analysed for the systematic review. The secondary outcomes comprised the aseptic loosening rate, audible squeaks, ceramic component fractures, and the frequency of these complications for each bearing surface generation. A comparison meta-analysis of RCTs was calculated, including the revision rate, aseptic loosening, and component fracture.
Quality assessment
The quality of cohort studies was assessed by the Newcastle Ottawa Scale (NOS) [10, 11]. It has eight items, collected into three groups: population choice, the comparability of the groups, and the ascertainment of the exposure or outcome. A study can be considered as the highest quality if it is awarded nine stars.
Statistical analysis
The included studies were pooled using the Mantel–Haenszel fixed-effects method (FEM) and the DerSimonia Laird random-effects method (REM). In the absence of significant heterogeneity, the FEM was considered; otherwise, the REM was considered.
Studies included were tested for heterogeneity using the following tests:
Cochran Q chi-square test: A statistically significant test (p value < 0.01) denoted heterogeneity among the studies.
I-squared (I2) index, which is calculated as follows: where Q is the chi-squared statistic and df is its degrees of freedom.
In the case of heterogeneity >50% at I2 test, a Mantel-Haenszel random-effect was planned. The continuous outcomes were expressed as mean and standard error (SE) and 95% confidence limits (95% CI). The odds ratio (OR) with 95% CI was calculated for binary outcomes. Data for survival percentage (frequency) were pooled using the inverse-variance method and the Freeman-Tukey double arcsine transformation to calculate proportion before returning to the original scale for plotting.
Statistical analyses of the meta-analysis were performed using RevMan V.5.3 (The Cochrane Collaboration, 2012). A two-sided p value < 0.05 denoted statistical significance.
Results
Search results
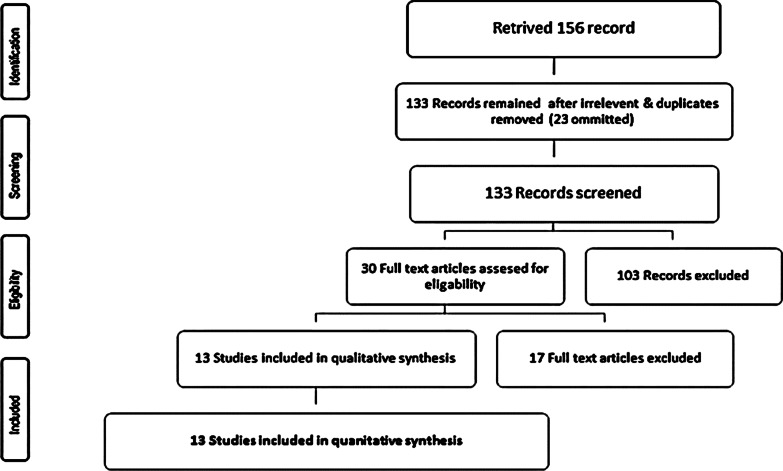
We identified a total of 156 studies, 23 duplicates were omitted. After application of our eligibility and exclusion criteria, we excluded 103 records. Due to the low quality of research according to NOS, we again excluded nine records. Again, eight records were excluded: due to the inaccessibility of English full texts. That leaves us with 13 records available for data extraction and quantitative synthesis. Figure 1
Fig. 1.
PRISMA flow diagram for selection of studies
These studies included four RCTs and nine cohort studies; five studies were prospective, four studies were retrospective, and all were published in peer-review journals between 2006 and 2018 [6, 12–23]. The total number of the included hips was 2278. The study sample sizes ranged from 29 to 930 patients per the study, with an average age of 44 (24–54 years). The average follow-up was around 10 years in each study (9.7–15 years). Biolox Forte ceramic articulations were used in 1339 hips, while Biolox Delta articulations were used in 939 hips in two studies [17, 22] Table 1.
Table 1.
Patients and implant characteristics based on the studies
| Study | Hips no | age (years) at surgery | Study type | Implant (Bioloox) | Fixation uncemented = both cup and stem | Outcome Score | Aseptic loosening | Prosthetic fracture | Bearing fracture | Squeaking | Follow-up (years) | K-M survival at 10 years (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Murphy 2006 [12] | 174 | 50 | Prospective | Forte | Uncemented | 98 | 1 | 1 | 1 | 0 | 10 | 99.3 |
| Boyer. 2010 [13] | 76 | 39 | prospective | Forte | Uncemented cup + cemented stem | 96 | 4 | 1 | 1 | 1 | 11 | 92 |
| Lee 2010 [14] | 88 | 41 | retrospective | Forte | Uncemented | 96 | 0 | 2 | 2 | 13 | 10 | 99 |
| Kim et al. 2010 [15] | 93 | 38 | prospective | Forte | Uncemented | 96 | 0 | 0 | 0 | 1 | 11.1 | 100 |
| Kress et al. 2011 [16] | 62 | 50 | prospective | Forte | Uncemented | 90 | 1 | 0 | 0 | 0 | 11 | 99 |
| Mesko et al. 2011 [17] | 930 | 51 | RCT | Forte/delta | Uncemented | 97 | 2 | 27 | 3 | 21 | 10 | 97 |
| D’Antonio et al. 2012 [18] | 189 | 54 | RCT | Forte | Uncemented | 96 | 0 | 6 | 1 | 3 | 10.3 | 99.3 |
| Yoon et al. 2012 [19] | 75 | 24 | retrospective | Forte | Uncemented | 97 | 0 | 1 | 1 | 12 | 10 | 98,9 |
| Beaupre et al. 2016 [20] | 48 | 53 | RCT | Forte | Uncemented | 98 | 0 | 2 | 0 | 2 | 11 | 94 |
| Wang et al. 2016 [21] | 90 | 40 | retrospective | Forte | Uncemented | 98 | 0 | 2 | 2 | 1 | 9.7 | 97.3 |
| Kim et al. 2016 [22] | 334 | 48 | prospective | Delta | Uncemented | 98 | 2 | 0 | 0 | 5 | 13.1 | 99.7 |
| Atrey et al. 2018 [6] | 29 | 41 | RCT | Forte | Uncemented | 96 | 0 | 1 | 1 | 0 | 15 | 89 |
| Lau et al. 2018 [23] | 90 | 40 | retrospective | Forte | Uncemented | 39.8/48 | 1 | 1 | 1 | 0 | 12.1 | 96.4 |
Quality assessment of bias risk
In general, the methodological quality of all the cohort trials was low in bias risk. In terms of NOS, the mean value was 6.7 stars. Three studies got a 6-star rating [12, 16, 19], five studies got a 7-star rating [13–15, 21, 23] and one study got an 8-star rating [22].
The proportional analysis was conducted for all 13 studies, and the comparison meta-analysis included four RCTs [6, 17, 18, 20] comparing COC-bearing surfaces to the polyethylene group in THA.
1-Proportional analysis
10-year survival The mean 10-year survivorship was 96% (95% CI; 95.4–96.8 p < 0.001). The random-effects model was used due to considerable heterogeneity (I2 = 99%). The proportion plot at the end of ten years is shown in Fig. 2.
Fig. 2.
Forest plot for ten-year survivorship
Aseptic loosening rate was 0.516 (95% CI; 0.265–0.903). Table 2 There was un-important heterogeneity (I2 = 22%); therefore, the fixed-effects model has used.
Table 2.
Aseptic loosening
| Study | Sample size | Proportion (%) | 95% CI | Weight (%) | |
|---|---|---|---|---|---|
| Fixed | Random | ||||
| Atrey 2018 | 29 | 0.000 | 0.000–11.944 | 1.31 | 2.04 |
| Beaupre 2015 | 48 | 0.000 | 0.000–7.397 | 2.14 | 3.23 |
| Boyer 2010 | 76 | 5.263 | 1.452–12.931 | 3.36 | 4.84 |
| D'Antonio 2012 | 189 | 0.000 | 0.000–1.933 | 8.29 | 10.07 |
| Kim 2010 | 93 | 0.000 | 0.000–3.889 | 4.10 | 5.75 |
| Kim 2016 | 334 | 0.599 | 0.0726–2.146 | 14.62 | 14.78 |
| Kress 2011 | 62 | 1.613 | 0.0408–8.662 | 2.75 | 4.05 |
| Lau 2018 | 90 | 1.111 | 0.0281–6.036 | 3.97 | 5.59 |
| Lee 2010 | 88 | 0.000 | 0.000–4.105 | 3.88 | 5.48 |
| Mesko 2011 | 930 | 0.215 | 0.0261–0.775 | 40.64 | 24.33 |
| Murphy 2006 | 174 | 0.575 | 0.0145–3.160 | 7.64 | 9.47 |
| Wang 2016 | 90 | 0.000 | 0.000–4.016 | 3.97 | 5.59 |
| Yoon 2012 | 75 | 0.000 | 0.000–4.800 | 3.32 | 4.78 |
| Total (fixed effects) | 2278 | 0.516 | 0.265–0.903 | 100.00 | 100.00 |
| Total (random effects) | 2278 | 0.614 | 0.271–1.092 | 100.00 | 100.00 |
The bold line indicates that a fixed-effects model was used rather than a random-effects model to account for modest outcome heterogeneity
The audible squeaking rate was 2.687% (95% CI; 1.279–4.593). There was considerable heterogeneity (I2 = 84.6%); therefore, the random-effects model was used.
Component fracture rate was 0.62% (95% CI; 0.341–1.034). There was moderate heterogeneity (I2 = 22%); therefore, the fixed-effects model was used.
Generation-specific complications; component fractures occurred in 11 cases out of 1339 hips in the 3rd-generation (0.8%) but decreased significantly to two cases out of 939 hips in the 4th-generation (0.2%) (p = 0.057). This was not the case when comparing the prevalence of squeaking, which was 2.9% in the 3rd-generation (40/1339 hips) and 2% in the 3rd-generation (19/939 hips), a statistically insignificant difference (p = 0.178).
2-Comparison meta-analysis
Four RCTs compared the outcomes of THA between CoC and polyethylene bearings, including 1191 hips. The survival rate for CoC was 96% (95% CI; 92.8–98.7), and for the polyethylene was 92.4 (96% CI; 85.1–97.4). Risk Ratio (RR) of revision due to any cause was 0.27 (95% CI; 0.15–0.47), and for aseptic loosening was 0.15 (95% CI; 0.03–0.70); both were in favour of CoC. Contrary to the results mentioned above, RR for component fractures was 1.62 (95% CI; 0.27–9.66), favouring the polyethylene group as is shown in Table 3 and Fig. 3.
Table 3.
Comparison between CoC and polyethylene
| Hips no | Revision | Aseptic loosening | Component fracture | Survival analysis (%) |
|---|---|---|---|---|
| Atrey 2018 | ||||
| *CoC (29) | 1 | 0 | 1 | 89 |
| **CoP (28) | 5 | 4 | 0 | 85 |
| Beaupre | ||||
| CoC (48) | 0 | 0 | 0 | 94 |
| CoP (44) | 3 | 0 | 0 | 90 |
| D'Antonio | ||||
| CoC (184) | 6 | 0 | 1 | 99.3 |
| ***MoP (95) | 10 | 3 | 0 | 98.9 |
*CoC: Ceramic-on-ceramic
**CoP: Ceramic-on-polyethylene
***MoP: Metal-on-polyethylene
Fig. 3.
Forest plot of comparison meta-analysis including revision rates, aseptic loosening, and components fracture
Discussion
Hip replacement surgery is one of the most successful operations in all of medicine. Since the early 1960s, joint replacement surgical techniques and technology improvements have increased total hip replacement effectiveness [24, 25]. According to the Agency for Healthcare Research and Quality, more than 450,000 total hip replacements are performed each year in the United States [26].
Total hip arthroplasty is becoming more common in younger patients around the world. American Academy of Orthopaedic Surgeons (AAOS) reported a 123% increase in THA rates in the 45–64 age group from 2000 to 2009 [27]. Younger patients are more active and have a longer life span, so the option of THA bearing surface may be perplexing for a surgeon, leading to the recommendation of hard-on-hard bearings as CoC over hard-on-soft bearings (CoP or MoP) [1, 28], with suggested survival to be inferior compared to the elderly population [29]. THA implants are only approved for people if they have a 10-year revision rate of less than 5%, according to the UK National Institute of Health and Care Excellence benchmark in 2014 [30].
A decade ago, a meta-analysis tested three bearings CoC, MoP, and metal on metal (MoM), when used in young patients, and concluded that ceramic articulations had the lowest survival among the bearing surfaces (89% 10-year survival) with the highest survival rate for MoM articulations (95.4%) [31]. However, the ceramic tested in that study was the available second-generation before developing the 3rd and 4th ceramic generations. Besides, a substantial body of evidence has developed against MoM implants after the reported higher complication rates and premature failure [32–34].
Ceramic-specific complications include ceramic fracture, squeaking, and aseptic loosening, have been linked to a higher failure of CoC implants than hard-on-soft implants as MoP [35]. Early ceramic fractures rate was reported up to 5% in the 1st and 2nd generations [36], with overall survivorship between 75 and 84% after ten years [37], that improved with the introduction of hot iso-static pressing (HIP) techniques, which reduced the grain size during ceramic manufacturing. HIP improved the wear properties, resistance to fracture, and durability [38]. These techniques allowed the release of 3rd -generation ceramic (Biolox forte) in 1995 and after that the 4th -generation (Biolox delta) in 2000 [8], with a reduction in the bearing fracture rate to be as low as 0.126% for liners and 0.009% for femoral heads [39, 40].
Our meta-analysis found some expected findings consistent with previously published studies, and it also produced some new data by combining the included studies. In the proportional analysis, the 10-year survival rate of CoC THA was recorded as 96% (95% CI; 95.4–96.8, P < 0.001), tested in 13 studies that included 2278 patients with the 3rd- and 4th-generation CoC bearings. This survival rate is similar to the patients' of 60 years or more, recorded to be from 95.6 [24] to 96.7 [25]. Only one study had a survival rate of less than 90% [6]; however, this study has the most extended follow-up in the review (15 years) with the smallest number of cases. The ceramic fracture rate was recorded at a rate of 0.62 (95% CI; 0.341–1.034), with an audible squeak rate of 2.687% (95% CI; 1.279–4.593). The rate of aseptic loosening was found to be 0.516 (95% CI; 0.265–0.903).
Sandwich ceramic cup design with intervening polyethylene between the ceramic liner and metal shell had been attributed to a high fracture rate. Kawano et al. reported ceramic sandwich fractures in 50 hips out of 270 with a 13-year survival rate were only 68.0% [41]. One study reported two sandwich ceramic liners fractures out of 90 hips [21]. Another situation to be avoided was the cup edge loading by reducing the acetabular abduction angle and malalignment with subsequent stripe wear reduction. Reduction in the cup edge loading reduces the rate of ceramic fracture [42].
Biomechanically, ceramics offer the best wear resistance, owing to wettability and fluid film formation [43], and have a lower incidence of osteolysis than metal-on-metal, so considered the ideal bearing surface in the younger active patient with a low rate of aseptic loosening [44, 45].
Squeaking for CoC bearing had a reported rate from < 1 to 21%, with presumed multifactorial aetiology [46]. Elevated rim of the acetabular cup and excessive or insufficient cup anteversion cause the neck impingement with squeaks [47]. Patient factors such as younger age, increased height and weight, and rigorous physical activity were also accused, together with the stem design and the type of ceramic (less voice with Delta than Forte types) [48–51]
Due to the 4th-generation ceramics’ increased toughness and burst strength, it was expected that fractures would occur at a much lower rate than the 3rd -generation ceramics' reported fracture rate. The review reported this as having a fracture rate of 0.8%, compared to 0.2% for the 4th -generation. However, no significant difference in squeaking rates was observed. Recent articles directly comparing the 3rd- and 4th- generations reported similar findings in patients with an average age of greater than 50 years. [52, 53]. Similarly, in 2020, Luceri et al. reported excellent outcomes following THA with Biolox Detla implants in patients aged 14–20 years at the time of surgery and followed for an average of 3.3 years (range 0.7–10.1 years) [54].
Comparing CoC to polyethylene, this meta-analysis revealed better CoC bearings outcomes than the results obtained by Shetty et al. [31]. In their study, CoC-bearing surfaces (three studies, sample size of 254 patients) revealed a 10-year survival rate of 88.9% (95% CI; 79.4–95.7%), while MoP liners (20 studies, sample size of 3592 patients) achieved pooled 10-year survival rates of 92.0% (95% CI; 89.4–94.2%). In our review, the 10-year survival (four studies with 1191 hips) was 96% (95% CI; 92.8–98.7). We included only studies after 2006 to find a 10-year follow-up of Forte and so, Delta ceramics. Revision rates and aseptic loosening were in favour of CoC. Comparable results were obtained by Hu et al. [55], in a more recent meta-analysis which tested these rates among 3rd- and 4th -generation ceramic THA. However, this meta-analysis included studies with a follow-up of less than ten years. Bearing surfaces fracture rates fell in disfavour compared to the polyethylene group in all meta-analyses. In our meta-analysis, five ceramic fractures were among 1191 (0.4%), and in Hu et al. study, four fractures were recorded among 601 (0.66).
All studies in this systematic review have high methodological quality, and all RCTs included in the meta-analysis have follow-ups more than ten years with patients less than 60 years of age (average 44). The study strengths are the large patient sample size (2278 hips) and the ability to examine multiple risk factors. Besides, this study was able to combine multiple implants from various manufacturers. Finally, all the studies were published in the last fifteen years.
One weakness is that most of the included studies were level-of-evidence 2–4 studies. Only four of the included 13 studies were level-1-study. An effort was made to perform a "best evidence meta-analysis," including studies with appropriate methodology. Not every study examined the same variables. Thus, for each of the subgroup analyses, there were a different number of studies included.
Conclusion
Ceramic on ceramic-bearings in current THA has been associated with improved 10-year results and survival when used in patients less than 60 years than what was documented before. The improved manufacturing process of ceramic surfaces has a significant impact on these results.
Abbreviations
- THA
Total hip arthroplasty
- CoC
Ceramic-on-ceramic
- RCTS
Randomised controlled trials
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses statement
- MoP
Metal on polyethylene
- MoM
Metal on metal
- HIP
Hot iso-static pressing
Author’s contributions
IIE: Study design, data Collection and pooling, articles review, data extraction and testing of the articles, results analysis, statistical calculation and figures construction, and manuscript writing. AHH: Study design, data collection and pooling, articles review, data extraction and testing of the articles. ARM: Results analysis, revision of the statistical calculations, revision of the manuscript draft. All authors read and approved the final manuscript.
Funding
There is no funding source.
Availability of data and materials
Available on request.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Committee Board in August 2019.
Consent to publication
Not applicable.
Competing interests
The authors declare that there is no competing interests regarding this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ihab Ibraheam El-Desouky, Email: ehabede@hotmail.com.
Albaraa Hassan Helal, Email: dr.baraa.helal@gmail.com.
Ali Mohamed Reda Mansour, Email: alimreda@hotmail.com.
References
- 1.Kurtz S, Lau E, Ong K, Zhao K, Kelly M, Bozic K. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Esposito C, Maclean F, Campbell P, Walter WL, Walter WK, Bonar SF. Periprosthetic tissues from third-generation alumina-on-alumina total hip arthroplasties. J Arthroplasty. 2013;28(5):860–866. doi: 10.1016/j.arth.2012.10.021. [DOI] [PubMed] [Google Scholar]
- 3.Zagra L, Gallazzi E. Bearing surfaces in primary total hip arthroplasty. EFORT Open Rev. 2018;3:217–224. doi: 10.1302/2058-5241.3.180300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bedard N, Burnett R, DeMik D, Gao Y, Liu S, Callaghan J. Are trends in total hip arthroplasty bearing surface continuing to change? 2007–2015 usage in a large database cohort. J Arthroplasty. 2017;32:3777–3781. doi: 10.1016/j.arth.2017.07.044. [DOI] [PubMed] [Google Scholar]
- 5.Wyles CC, Jimenez-Almonte JH, Murad MH, Norambuena-Morales GA, Cabanela ME, Sierra RJ, et al. There are no differences in short- to mid-term survivorship among total hip-bearing surface options: a network meta-analysis. Clin Orthop Relat Res. 2015;473(6):2031–2041. doi: 10.1007/s11999-014-4065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atrey A, Wolfstadt JI, Hussain N, Khoshbin A, Ward S, Shahid M, et al. The ideal total hip replacement bearing surface in the young patient: a prospective randomized trial comparing alumina ceramic-on-ceramic with ceramic-on-conventional polyethylene: 15-year follow-up. J Arthroplasty. 2018;33(6):1752–1756. doi: 10.1016/j.arth.2017.11.066. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Rey E, Bizot P, Garcia-Cimbrelo E. Ceramic-on-ceramic cementless total hip arthroplasty in patients aged 40 years or under: Do pre-operative conditions affect long-term results? Orthop Traumatol Surg Res 2021;107(1). [DOI] [PubMed]
- 8.Jenabzadeh A, Pearce S, Walter W. Total hip replacement: ceramic-on-ceramic. Semin Arthroplasty. 2012;23:232–240. [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 10.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of non randomised studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 11.Deeks J, Dinnes J, D’Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess (Rockv) 2003;7(27). [DOI] [PubMed]
- 12.Murphy SB, Ecker TM, Tannast M. Two- to 9-year clinical results of alumina ceramic-on-ceramic THA. Clin Orthop Relat Res. 2006;453:97–102. doi: 10.1097/01.blo.0000246532.59876.73. [DOI] [PubMed] [Google Scholar]
- 13.Boyer P, Huten D, Loriaut P, Lestrat V, Jeanrot C, Massin P. Is alumina-on-alumina ceramic bearings total hip replacement the right choice in patients younger than 50 years of age? A 7- to 15-year follow-up study. Orthop Traumatol Surg Res. 2010;96:616–622. doi: 10.1016/j.otsr.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 14.Lee Y, Ha Y, Yoo J, Koo K, Yoon K, Kim H. Alumina-on-alumina total hip arthroplasty: a concise follow-up, at a minimum of ten years, of a previous report. J Bone Jt Surg Ser A. 2010;92:1715–1719. doi: 10.2106/JBJS.I.01019. [DOI] [PubMed] [Google Scholar]
- 15.Kim Y, Choi Y, Kim J. Cementless total hip arthroplasty with ceramic-on-ceramic bearing in patients younger than 45 years with femoral-head osteonecrosis. Int Orthop. 2010;34:1123–1127. doi: 10.1007/s00264-009-0878-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kress A, Schmidt R, Holzwarth U, Forst R, Mueller L. Excellent results with cementless total hip arthroplasty and alumina-on-alumina pairing: minimum ten-year follow-up. Int Orthop. 2011;35:195–200. doi: 10.1007/s00264-010-1150-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mesko J, D'Antonio J, Capello W, Bierbaum B, Naughton M. Ceramic-on-ceramic hip outcome at a 5- to 10-year interval. Has it lived up to its expectations? J Arthroplasty. 2011;26:172–7. doi: 10.1016/j.arth.2010.04.029. [DOI] [PubMed] [Google Scholar]
- 18.D'Antonio J, Capello W, Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012;470:373–381. doi: 10.1007/s11999-011-2076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoon H, Yoo J, Yoon K, Koo K, Kim H. Alumina-on-alumina THA performed in patients younger than 30 years: a 10-year minimum follow-up study. Clin Orthop Relat Res. 2012;470:3530–3536. doi: 10.1007/s11999-012-2493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beaupre L, Al-Houkail A, Johnston D. A randomised trial comparing ceramic-on-ceramic bearing vs ceramic-on-crossfire-polyethylene bearing surfaces in total hip arthroplasty. J Arthroplasty. 2016;31:1240–1245. doi: 10.1016/j.arth.2015.11.043. [DOI] [PubMed] [Google Scholar]
- 21.Wang T, Sun J, Zhao X, Liu Y, Yin H. Ceramic-on-ceramic bearings total hip arthroplasty in young patients. Arthroplast Today. 2016;2:205–209. doi: 10.1016/j.artd.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim Y, Park J, Kim J. Alumina delta-on-alumina delta bearing in cementless total hip arthroplasty in patients aged <50 years. J Arthroplasty. 2016;31:2209–2214. doi: 10.1016/j.arth.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 23.Lau Y, Sarmah S, Witt J. 3rd generation ceramic-on-ceramic cementless total hip arthroplasty: a minimum 10-year follow-up study. HIP Int. 2018;28:133–138. doi: 10.1177/1120700018768617. [DOI] [PubMed] [Google Scholar]
- 24.Milošev I, Kovač S, Trebše R, Levašič V, Pišot V. Comparison of ten-year survivorship of hip prostheses with use of conventional polyethylene, metal-on-metal, or ceramic-on-ceramic bearings. J Bone Jt Surg Ser A. 2012;94:1756–1763. doi: 10.2106/JBJS.J.01858. [DOI] [PubMed] [Google Scholar]
- 25.Yin S, Zhang D, Du H, Du H, Yin Z, Qiu Y. Is there any difference in survivorship of total hip arthroplasty with different bearing surfaces? A systematic review and network meta-analysis. Int J Clin Exp Med. 2015;8:21871–21885. [PMC free article] [PubMed] [Google Scholar]
- 26.Total Hip Replacement - OrthoInfo - AAOS in https://orthoinfo.aaos.org/en/treatment/total-hip-replacement/. Accessed 1 June 2021
- 27.OASIS in https://www.abstractsonline.com/Plan/ViewAbstract.aspx?sKey=8aee1902-36d1-4626-9e3b-3fb48ce6bb61&cKey=cbe5d81e-5b06-4de5-9dda-7d7b4c599010&mKey=4393d428-d755-4a34-8a63-26b1b7a349a1 Accessed 1 June 2021
- 28.Bizot P, Banallec L, Sedel L, Nizard R. Alumina-on-Alumina Total Hip Prostheses in Patients 40 Years of Age or Younger. Clin Orthop Relat Res. 2000;379:68–76. doi: 10.1097/00003086-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Bayliss LE, Culliford D, Monk AP, Glyn-Jones S, Prieto-Alhambra D, Judge A, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017;389:1424–1430. doi: 10.1016/S0140-6736(17)30059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393:647–654. doi: 10.1016/S0140-6736(18)31665-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shetty V, Shitole B, Shetty G, Thakur H, Bhandari M. Optimal bearing surfaces for total hip replacement in the young patient: a meta-analysis. Int Orthop. 2011;35:1281–1287. doi: 10.1007/s00264-010-1104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bozic K, Lau E, Ong K, Vail T, Rubash H, Berry D. Comparative effectiveness of metal-on-metal and metal-on-polyethylene bearings in medicare total hip arthroplasty patients. J Arthroplasty. 2012;27(8 SUPPL.):37–40. doi: 10.1016/j.arth.2012.03.031. [DOI] [PubMed] [Google Scholar]
- 33.Hasegawa M, Yoshida K, Wakabayashi H, Sudo A. Prevalence of adverse reactions to metal debris following metal-on-metal THA. Orthopedics. 2013; 36(5). [DOI] [PubMed]
- 34.Wyles CC, Van Demark RE, Sierra RJ, Trousdale RT. High rate of infection after aseptic revision of failed metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472:509–16. doi: 10.1007/s11999-013-3157-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gallo J, Goodman SB, Lostak J, Janout M. Advantages and disadvantages of ceramic on ceramic total hip arthroplasty: a review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2012;156:204–212. doi: 10.5507/bp.2012.063. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Cimbrelo E, Martinez-Sayanes JM, Minuesa A, Munuera L. Mittelmeier ceramic-ceramic prosthesis after 10 years. J Arthroplasty. 1996;11:773–781. doi: 10.1016/s0883-5403(96)80176-8. [DOI] [PubMed] [Google Scholar]
- 37.Nizard RS, Sedel L, Christel P, Meunier A, Soudry M, Witvoet J. Ten-year survivorship of cemented ceramic-ceramic total hip prosthesis. Clin Orthop Relat Res. 1992;282:53–63. [PubMed] [Google Scholar]
- 38.Willmann G. Ceramic femoral head retrieval data. Clin Orthop Relat Res. 2000;379:22–28. doi: 10.1097/00003086-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Howard DP, Wall PDH, Fernandez MA, Parsons H, Howard PW. Ceramic-on-ceramic bearing fractures in total hip arthroplasty. Bone Jt J. 2017;99B:1012–1019. doi: 10.1302/0301-620X.99B8.BJJ-2017-0019.R1. [DOI] [PubMed] [Google Scholar]
- 40.Beckmann NA, Gotterbarm T, Innmann MM, Merle C, Bruckner T, Kretzer JP, Streit MR. Long-term durability of alumina ceramic heads in THA. BMC Musculoskelet Disord. 2015;16:249. doi: 10.1186/s12891-015-0703-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kawano S, Sonohata M, Shimazaki T, Kitajima M, Mawatari M, Hotokebuchi T. Failure analysis of alumina on alumina total hip arthroplasty with a layered acetabular component Minimum ten-year follow-up study. J Arthroplasty. 2013;28:1822–1827. doi: 10.1016/j.arth.2013.04.027. [DOI] [PubMed] [Google Scholar]
- 42.Poggie R, Turgeon T, Coutts R. Failure analysis of a ceramic bearing acetabular component. J Bone Jt Surg. 2007;89:367. doi: 10.2106/JBJS.F.00148. [DOI] [PubMed] [Google Scholar]
- 43.Hannouche D, Hamadouche M, Nizard R, Bizot P, Meunier A, Sedel L. Ceramics in total hip replacement. Clin Orthop Relat Res. 2005;430:62–71. doi: 10.1097/01.blo.0000149996.91974.83. [DOI] [PubMed] [Google Scholar]
- 44.Kumar A, Bloch BV, Esler C. Trends in total hip arthroplasty in young patients—results from a regional register. HIP Int. 2017;27:443–448. doi: 10.5301/hipint.5000485. [DOI] [PubMed] [Google Scholar]
- 45.Higuchi Y, Seki T, Takegami Y, Komatsu D, Morita D, Ishiguro N. Same survival but higher rate of osteolysis for metal-on-metal Ultamet versus ceramic-on-ceramic in patients undergoing primary total hip arthroplasty after 8 years of follow-up. Orthop Traumatol Surg Res. 2018;104:1155–1161. doi: 10.1016/j.otsr.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 46.Imbuldeniya AM, Pearce SJ, Walter WL, Zicat BA, Walter WK. Squeaking: current knowledge and how to avoid it. Curr Rev Musculoskelet Med. 2013;6:342–349. doi: 10.1007/s12178-013-9181-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Parvizi J, Adeli B, Wong JC, Restrepo C, Rothman RH. A squeaky reputation: the problem may be design-dependent. Clin Orthop Relat Res. 2011;469:1598–1605. doi: 10.1007/s11999-011-1777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Walter WL, O’toole GC, Walter WK, Ellis A, Zicat B. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007;22:496–503. doi: 10.1016/j.arth.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 49.Walter WL, Waters TS, Gillies M, Donohoo S, Kurtz SM, Ranawat AS, et al. Squeaking hips. J Bone Joint Surg Am. 2008;90(Suppl 4):102–11. doi: 10.2106/JBJS.H.00867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Glaser D, Komistek RD, Cates HE, Mahfouz MR. Clicking and squeaking: in vivo correlation of sound and separation for different bearing surfaces. J Bone Jt Surg. 2008;90(Suppl 4):112–120. doi: 10.2106/JBJS.H.00627. [DOI] [PubMed] [Google Scholar]
- 51.Restrepo C, Post ZD, Kai B, Hozack WJ. The effect of stem design on the prevalence of squeaking following ceramic-on-ceramic bearing total hip arthroplasty. J Bone Jt Surg. 2010;92(3):550–557. doi: 10.2106/JBJS.H.01326. [DOI] [PubMed] [Google Scholar]
- 52.Kim SM, Rhyu KH, Yoo JJ, Lim SJ, Yoo JH, Kweon SH, et al. The reasons for ceramic-on-ceramic revisions between the third- and fourth-generation bearings in total hip arthroplasty from multicentric registry data. Sci Rep. 2021;11:5539. doi: 10.1038/s41598-021-85193-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim SC, Lim YW, Jo WL, Park HW, Han SB, Kwon SY, et al. Fourth-generation ceramic-on-ceramic THA results in improvements in midterm outcomes compared to third-generation THA but does not resolve noise problems: a cohort study of a single-hip system. BMC Musculoskelet Disord. 2019;20:263. doi: 10.1186/s12891-019-2641-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Luceri F, Morelli I, Sinicato CM, Della-Grazia A, Verdoni F, Maffulli N, et al. Medium-term outcomes of total hip arthroplasty in juvenile patients. J Orthop Surg Res. 2020;15(1):476. doi: 10.1186/s13018-020-01990-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hu D, Tie K, Yang X, Tan Y, Alaidaros M, Chen L. Comparison of ceramic-on-ceramic to metal-on-polyethylene bearing surfaces in total hip arthroplasty: a meta-analysis of randomised controlled trials. J Orthop Surg Res. 2015;10:22. doi: 10.1186/s13018-015-0163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available on request.