Abstract
Objective:
To evaluate the overbite correction of fixed palatal crib (FPC) and bonded lingual spur (BLS) in the early treatment of anterior open bite (AOB) in mixed dentition (primary outcome) as well as its influence on dental and skeletal cephalometric measurements (secondary outcome).
Materials and Methods:
The selected patients had AOB and a mean age of 8.23 years. They were divided into the following three groups by casting lots: control (n = 13), palatal crib (n = 13), and spur (n = 13). Data from the lateral teleradiography was obtained at the beginning, at 6 months, and after 1 year. The cephalometric analysis was performed by Cef-X program, recording the values of SNA, SNB, ANB, SnG oGn, 1.PP, IMPA, nasolabial angle, overbite, and overjet. Intergroup and intragroup comparisons were obtained via one-way analysis of variance.
Results:
The degree of AOB was similar at baseline (P > .05). At 6 months and then after 1 year all groups showed improvement in the overbite. However, only the crib and spur groups showed positive overbite. No cephalometric measurements changed significantly over the period analyzed.
Conclusions:
We conclude that the FPC and BLS are simple and effective for the treatment of anterior open bite, with the advantage given to the FPC.
Keywords: Open bite, Orthodontic appliances
INTRODUCTION
An anterior open bite (AOB), one of the malocclusions with the greatest esthetic and functional impairment, is characterized by the presence of negative overbite between the incisal edges of the upper and lower front teeth when the posterior ones are in occlusion.1–3 Habits of sucking objects like a pacifier and a finger can cause or worsen AOB in predisposed patients. Most children grow out of the habit, but if they continue with it through mixed dentition they might need orthodontic intervention.4 Available data have shown that 12.1% of children past the age of 7 years maintain a digit- or pacifier-sucking habit, but general studies show that the prevalence of AOB decreases with age.5 It was reported that 17.7% of children from 6 to 8 years old, among those with malocclusion evaluated by the Index of Orthodontic Treatment Need, had anterior open bite.6
From the age of 5 years, if the habit is interrupted and the patient has a good facial growth pattern, correction of AOB may occur spontaneously.7 Self-correction of dental AOB may occur in up to 80% of patients when the negative habit is eliminated up until the phase of mixed dentition.2
In a systematic review, Borrie et al.4 showed that orthodontic appliances were beneficial in stopping the sucking habit compared with no treatment, and that the palatal crib was beneficial for occlusion compared with no treatment. The palatal crib works as an obstacle in nonnutritive sucking and maintains the tongue in a more retruded position, preventing its interposition between the incisors.
Nogueira et al.8 stated that a palatal crib and spurs are both effective methods for treating AOB in patients with atypical swallowing due to lingual pressing. However, the crib requires consultations to shape and install the device as well as incurring laboratory expenses. The spur, on the other hand, is inexpensive and promotes greater freedom to the tongue due to its small size.
Yang and Kiyak9 affirm that early treatment of AOB increases the stability of morphologic correction. Huang et al.10 showed that patients with AOB and who were treated with a palatal crib presented satisfactory stability in the correction of the bite 1 year after the end of treatment. Because the palatal crib acts passively and helps remove etiologic factors, there is evidence of stable correction of the AOB.1
No studies were found comparing the use of spurs to a control group11 or the use of spurs and palatal crib to verify the effectiveness of both treatments. Given this, the primary goal of this study was to evaluate the effects of the fixed palatal crib (FPC) and bonded lingual spur (BLS) for early treatment of AOB in the mixed dentition phase. This study also addressed the cephalometric effects of those appliances, as a secondary outcome.
MATERIALS AND METHODS
The project was approved by the Standing Committee on Ethics in Research Involving Humans of the Universidade Estadual de Maringa (CAAE, 0153.0.09.000-10, 441/2010 on August 12, 2010).
The sample was obtained from the clinical occlusal evaluations of patients at the Integrated Children's Clinic of the Department of Dentistry, State University of Maringá, in the city of Maringá in the state of Paraná. We selected patients with nonnutritive sucking habits and/or tongue thrusting from 5 years to 10 years old, with AOB, at the stage of mixed dentition. Patients who had already undergone prior orthodontic treatment, had deciduous/permanent dentition, were undergoing speech therapy, or had syndromes were all excluded from the study.
The sample size of each group was calculated based on alpha significance level of 0.05 to achieve power of 80% with an error standard deviation of 0.5 for 0.8 mm of difference to be detected; this was drawn from a pilot study. The sample-size calculation showed that nine patients were needed in each group. The initial sample size of this study was 45 patients, and 39 patients completed all study periods. Patients were allocated into the following three groups by drawing lots (numbered envelopes): the control group (n = 13) consisted of 11 girls and 2 boys, the group treated with palatal crib (n = 13) consisted of 10 girls and 3 boys, and the group treated with bonded lingual spur (n = 13) consisted of 12 girls and 1 boy. All patients were instructed to give up the negative habit. At baseline the patients received and signed a consent form that contained explanations about the experiment and action taken for all groups. The initial mean age was 7.79 years for the control group, 8.46 years for the crib group, and 8.44 years for the spur group.
There was blinding during the allocation and during the cephalometric analysis; however, there was no blinding for the treatment process because it was apparent which patient had which treatment. Patients in all groups received instruction to stop the nonnutritive sucking habit and were followed monthly to monitor the progress of treatment and to reinforce the instruction to give up the sucking habit. They also received hygiene supervision and reinforcement every consultation. Lateral radiographs were performed at baseline, at 6 months, and after 1 year.
The control group had its 6-month values set at 1 year, given that, for ethical reasons, it was decided that the treatment would be introduced after 6 months of initial monitoring. For this, the difference between measurements of the overbite and overjet calculated per month from the beginning to the sixth month was projected for the next 6 months. The cephalometric measurements per se were annualized, using the same criteria, based on the Atlas of Craniofacial Growth by Riolo et al.12 considering that there is differential behavior (not progressive) for measurements. Previous studies have demonstrated the validity of this method when records are lacking for the required period.13 The control group had no interventions for 6 months (teleradiography at the beginning and at 6 months) and then were included as part of the spur group or the crib group.
The overbite measuring technique used in this evaluation measures the distance between the maxillary and mandibular incisor borders perpendicular to the occlusal plane. When AOB occurred this measurement was negative. The overjet measuring technique was obtained by a vertical perpendicular reference to the Frankfurt plane, it was positive when the superior incisive was in front of the inferior incisive. These references were executed by Cef-X software (CDT Software Version 1.04, Bauru, Brazil).
The FPC model included bands on the second deciduous molars or first permanent molars. Bands were transferred to the plaster models for welding a palatal stainless steel arch of 0.9 mm (Morelli, Sorocaba, Brazil). Then, palatal bars were added (three to five arches depending on the space) of 0.7 mm stainless steel, extended up to the height of the cervical lingual aspect of the lower incisors. Before cementing the FPC, prophylaxis was achieved with pumice and water; the region was then isolated. The appliances were cemented with glass ionomer (Vidrion C, SS White, Rio de Janeiro, Brazil). Figure 1 illustrates the FPC used.
Figure 1.

Model of palatal crib used in the study.
The lingual spur (Abzil, 3M, São José do Rio Preto, Brazil) was bonded with composite resin (Transbond-XT, 3M, St Paul, Minn) on the lingual of the upper central incisors after prophylaxis with pumice, relative isolation of the region, etching with 37% phosphoric acid and application of adhesive (Scotchbond, 3M). Figure 2 illustrates the BLSs.
Figure 2.

Lingual spurs used in the study.
Outcome Measures
The primary outcome measure to be assessed in this study was the overbite, and the secondary outcome measures were SNGoGn, ANB, SNA, SNB, 1.PP, IMPA, nasolabial angle, and overjet. After scanning, the Cef-X program was used to analyze these variables.
Statistical Analysis
All measurements were repeated after 15 days by the same operator to assess method error. For such, we applied the Dahlberg formula and the paired t-test. Comparisons were performed by one-way analysis of variance with Bonferroni post test using BioEstat 5.0 software (Mamiraua Institute, Amazonas, Brazil) with a confidence interval of 95%.
RESULTS
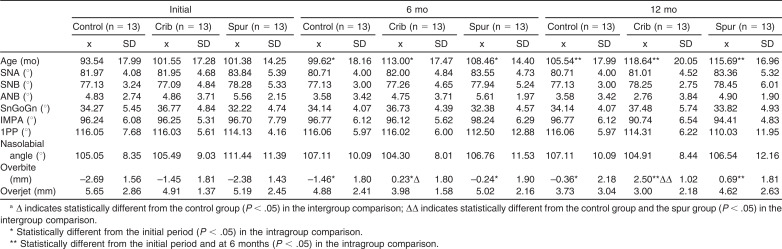
Both paired t-test and Dahlberg error revealed no significant difference for the method (P > .05). Table 1 presents the intergroup and intragroup comparisons, which demonstrated a significant evolution of the overbite as a primary outcome (P < .05) and no significant change in other measures evaluated as a secondary outcome (P > .05), except age, which varied according to the period of the study.
Table 1.
Intergroup and Intragroup Mean (x) and Standard Deviation (SD) Comparisons Using One-Way Analysis of Variance With Bonferroni Post Testa
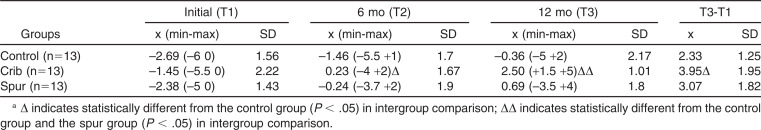
Table 2 presents comparisons between the mean values; the minimum and maximum of initial overbite at study onset (T1), at 6 months, and at 12 months (T2); and the differences between T3 and T1 from the studied groups. The overbite development in the crib group was the largest in the study period (3.95 mm) compared with the spur group (3.07 mm) and the control group (2.33 mm), but there was no statistically significant difference (P > .05). Only in the crib group after 12 months was the overlap positive in all patients (minimum value for overbite = 1.5 mm).
Table 2.
Intergroup Mean (x) and Standard Deviation (SD) Comparisons of Initial Overbite (mm), at 6 Months and at 12 Months and Differences Between T3 and T1 for the Control, Crib and Spur Groupsa
DISCUSSION
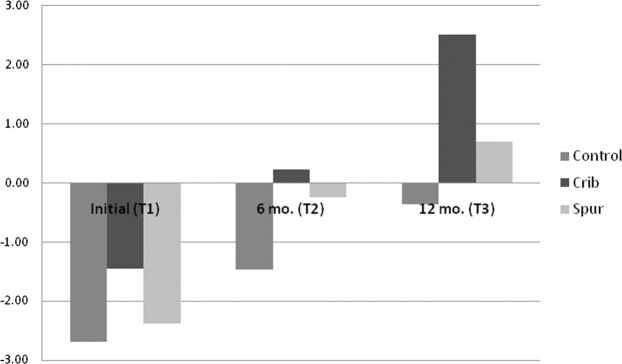
Correcting AOB remains a challenge for orthodontists when the patient does not receive intervention at an early age, and relapse occurs in up to 38% of patients14 during treatment at the phase of permanent dentition. Early treatment, up to the mixed dentition phase, executed by a general dentist practitioner or an orthodontist can provide occlusal stability and, consequently, decrease the perpetuation of functional alteration of AOB, favoring occlusal stability in the long term.1,9,10 The present study shows the effectiveness of two methods of correcting early AOB as well as the influence of simple instruction and motivation for removing the deleterious habit of finger sucking or pacifier use. All groups studied had, on average, improvement of the overbite after 1 year, although only those groups with the intervention of the crib or spur achieved positive values (Tables 1 and 2, Figure 3).
Figure 3.
Graph showing overbite comparison between the groups.
The sample groups had similar degrees of AOB (P > .05), and patients had an average age of 8.2 years (98.8 months) which was also similar among the groups (P > .05) (Table 1). It has been reported that at this stage intervention for the AOB is necessary, since interrupting the bad habit alone is no longer guaranteed for self-correction, although it may still occur.7 Spontaneous correction would be more likely if there was interruption of the deleterious habits at the stage of deciduous dentition,2 which is a chance that patients in this study did not have, considering the age at which treatment was sought. However, even at the stage of mixed dentition three patients showed improvement in the control group, representing 23% of the sample.
Most cephalometric variables analyzed (SNA, SNB, ANB, SnGoGn, IMPA, 1PP, and nasolabial angle) showed no statistical difference in the period studied, corroborating the results of various authors.1,14–16 Only minor changes were noted in 1PP and IMPA, though there was no statistical significance, as in some patients the overbite correction occurred by extrusion without inclination. Nasolabial angle, ANB, and SNB also presented minor changes without significance, reflecting individual variability in such ages.12 Pedrin et al.17 examined patients who underwent treatment with removable palatal crib associated with high pull chin cup and a control group involving untreated patients for a period of 12 months. They noted a reduction of AOB of 1.38 mm in the control group and 5.01 mm in the treated group. They concluded that palatal crib associated with high pull chin cup did not promote significant changes in maxillary and mandibular skeletal components and that treatment effects were dentoalveolar, corroborating the findings of the present study. In the present study the overbite was reduced on average 2.33 mm in the control group and 3.95 mm in the crib group.
Moore18 conducted a critical analysis on the use of fixed appliances such as palatal crib for the treatment of nonnutritive sucking habits and concluded that it can cause unnecessary pain and suffering to treat this habit. McRae11 evaluated the use of bonded lingual spur to see if it would correct lingual malposition or eliminate the habit of nonnutritive sucking and close the AOB. He evaluated 12 patients with nonnutritive sucking habits and/or atypical lingual projection who were treated for 6 months with BLS. Overbite improvement was observed in 11 of 12 patients in the sample, and the average AOB was reduced 1.38 mm in a period of 6 months. In this study the use of the spur reduced the overbite in 12 of the 13 patients studied, altering the average 2.14 mm in the first 6 months.
Cassis et al.19 conducted a 12-month evaluation of the spur associated with chin cup for treating AOB in patients with mixed dentition. They observed that in the control group there was a spontaneous closure of 1.98 mm of the AOB, which was enough to correct the overbite in 13.3% of patients. The group treated with spur and chin cup had an increase in overbite of 5.23 mm, promoting correction of AOB in 86.7% of patients. In the present study autocorrection occurred in 23% for the control group, with a mean change of 2.33 mm. However, for the spur group, even after 12 months, the vertical correction of 3.07 mm led to a positive overlap in only 53.8% of patients. The final average overbite was +0.69, indicating correction. It is interesting to observe that after a 6-month period, therapy with spurs appears to indicate which patients will succeed, given that the average increase for initial correction was not maintained until the 12th month. In other words, in the first semester of evaluation there was a mean reduction of 2.14 mm, and almost half of those with AOB already had positive overbite, while in the second half there was an additional increase of only 0.93 mm, and 7 of the 13 patients had positive overlap.
Figure 3 illustrates the behavior of the overbite. The crib group showed a significant difference after 6 and 12 months compared with the control group as well as a significant difference at 12 months compared with the spur group. Although clinical improvement was seen, the spur group was not statistically different from the control group at any of the times evaluated. However, only the control group had a negative overbite after 12 months.
In light of our findings, there was still no prospective study in the literature that had compared the effects of crib with those of spur as well as a control group, with no additional appliance. It was clear that, although the lingual spurs can act positively on AOB at this stage of development, it does not have a comparable effect to the classic palatal crib, at least in the period evaluated. Among the advantages of bonded spurs are the simplicity, cost, and easy patient compliance. But besides a lower performance in achieving correction compared with the palatal crib, disadvantages include the possibility that it will come off and be swallowed as well as irritation of the tip of the tongue. As to the palate crib, its efficiency can be considered an advantage (perhaps due to the large blocked area for tongue projection and/or preventing introduction of a finger or pacifier) and the system of fastening bands, which prevents swallowing accidents. The disadvantages include the need for laboratory time and expenses as well as lower initial patient acceptance due to the immediate alteration of speech. A subsequent study can evaluate the long-term stability of the changes observed in this sample.
CONCLUSIONS
The FPC was effective in the early treatment of AOB in 100% of patients, while the BLS, although it reduced the overbite in all subjects, resulted in positive trespass in only 53.8% of patients after 12 months.
Instruction and motivation for removing the negative habit during the mixed dentition phase can result in spontaneous correction of the AOB, and this occurred in 23% of the control subjects.
Treatment of AOB with FPC or BLS did not significantly alter the cephalometric variables within 12 months.
ACKNOWLEDGMENTS
We acknowledge Araucária and Capes Foundation’s support of this research.
REFERENCES
- 1.Almeida RR, Henriques JFC, Almeida MR, Vasconcelos MHF. Early treatment of anterior open bite—prevention of orthognathic surgery. In: Davidovitch Z, Mah J, editors. Biological Mechanisms of Tooth Eruption Resorption and Replacement by Implants. Boston, Mass: Harvard Society for the Advancement of Orthodontics; 1998. pp. 585–588. [Google Scholar]
- 2.Worms FW, Meskin LH, Isaacson RJ. Open bite. Am J Orthod Dentofacial Orthop. 1971;59:589–595. doi: 10.1016/0002-9416(71)90005-4. [DOI] [PubMed] [Google Scholar]
- 3.Subtelny JD, Sakuda M. Open bite: diagnosis and treatment. Am J Orthod Dentofacial Orthop. 1964;50:337–358. [Google Scholar]
- 4.Borrie FRP, Bearn DR, Innes NPT, Ilheozor-Ejiofor Z. Interventions for the cessation of non-nutritive sucking habits in children. Cochrane Database Syst Rev. 2015;3:CD008694. doi: 10.1002/14651858.CD008694.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel A. Digit sucking habits in children resident in Kettering (UK) J Orthod. 2008;35:255–261. doi: 10.1179/14653120722761. [DOI] [PubMed] [Google Scholar]
- 6.Tausche E, Luck O, Harzer W. Prevalence of malocclusion in the early mixed dentition and orthodontic treatment need. Eur J Orthod. 2004;26:237–244. doi: 10.1093/ejo/26.3.237. [DOI] [PubMed] [Google Scholar]
- 7.Graber TM, Rakosi T, Petrovic AG. Dentofacial Orthopedics With Functional Appliances. St Louis, Mo: CV Mosby Co: 1985. pp. 139–160. [Google Scholar]
- 8.Nogueira FF, Mota LM, Nouer PR, Nouer DF. Esporão lingual colado Nogueira®: tratamento coadjuvante da deglutição atípica por pressionamento lingual. Rev Dent Press Ortod Ortop Facial. 2005;10(2):129–156. [Google Scholar]
- 9.Yang EY, Kiyak A. Orthodontic treatment timing: a survey of orthodontists. Am J Orthod Dentofacial Orthop. 1998;113:96–103. doi: 10.1016/S0889-5406(98)70281-1. [DOI] [PubMed] [Google Scholar]
- 10.Huang GJ, Justus R, Kennedy DB, Kokich VG. Stability of anterior openbite treated with crib therapy. Angle Orthod. 1990;60:17–24. doi: 10.1043/0003-3219(1990)060<0017:SOAOTW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.McRae EJ. Bondable Lingual Spur Therapy to Treat Anterior Open Bite. Milwaukee, Wis: Marquette University; 2010: [master’s thesis] Available at: http://epublications.marquette.edu/theses_open/25 Accessed December 6, 2014. [Google Scholar]
- 12.Riolo ML, Moyers RE, McNamara JA, Hunter WS. An Atlas of Craniofacial Growth. Ann Arbor, Mich: Center for Human Growth and Development, University of Michigan; 1974. [Google Scholar]
- 13.Baccetti T, McGill JS, Franchi L, McNamara JA, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343. doi: 10.1016/s0889-5406(98)70306-3. [DOI] [PubMed] [Google Scholar]
- 14.Silva Filho OG, Chaves ASM, Almeida RR. Efeitos terapêuticos suscitados pelo uso da grade palatina: um estudo cefalométrico. Rev Soc Par Ortod. 1995/1996;1:9–15. [Google Scholar]
- 15.Almeida RR, Almeida-Pedrin RR, Almeida MR, Ferreira FPC, Pinzan A, Insabralde CMB. displasias verticais: mordida aberta anterior—tratamento e estabilidade. Rev Dent Press Ortod Ortop Facial. 2003;8(4):91–119. [Google Scholar]
- 16.Almeida RR, Santos SCBN, Santos ECA, Insabralde CMB, Almeida MR. Mordida aberta anterior—considerações e apresentação de um caso clínico. Rev Dent Press Ortod Ortop Facial. 1998;3(2):17–29. [Google Scholar]
- 17.Pedrin F, Almeida MR, Almeida RR, Almeida-Pedrin RR, Torres F. A prospective study of the treatment effects of a removable appliance with palatal crib combined with high-pull chincup therapy in anterior open-bite patients. Am J Orthod Dentofacial Orthop. 2006;129:418–423. doi: 10.1016/j.ajodo.2005.04.035. [DOI] [PubMed] [Google Scholar]
- 18.Moore NL. Suffer the little children: fixed intraoral habit appliances for treating childhood thumbsucking habits: a critical review of the literature. Int J Orofacial Myology. 2002;28:6–38. [PubMed] [Google Scholar]
- 19.Cassis MA, Almeida RR, Janson G, Almeida-Pedrin RR, Almeida MR. Treatment effects of bonded spurs associated with high-pull chincup therapy in the treatment of patients with anterior open bite. Am J Orthod Dentofacial Orthop. 2012;142:487–493. doi: 10.1016/j.ajodo.2012.04.022. [DOI] [PubMed] [Google Scholar]