Abstract
Objective:
To investigate risk factors specific to posterior crossbite and anterior open bite at the age of 3 years.
Materials and Methods:
The study included 422 children of the French EDEN mother-child cohort. The main outcomes were the presence of posterior crossbite and anterior open bite assessed by dentists at 3 years. Social characteristics (collected during pregnancy), neonatal characteristics (collected at birth), duration of breast-feeding (collected prospectively), sucking habits at 3 years, and open lips (as a proxy for mouth breathing) were studied and two logistic regressions conducted.
Results:
Preterm birth appears to be a risk factor specific for posterior crossbite (OR: 3.13; 95% CI: 1.13–8.68), whereas small for gestational age seems to be associated with a lower risk of posterior crossbite (OR: 0.32; 95% CI: 0.12–0.87). Ongoing pacifier or thumb sucking at 3 years is a risk factor for both posterior crossbite and anterior open bite.
Conclusions:
Children born preterm seem to be more at risk for posterior crossbite than those born at term. Different mechanisms may be involved in posterior crossbite and anterior open bite.
Keywords: Epidemiology, Crossbite, Orthodontics, Preterm birth, Child, Open bite
INTRODUCTION
A large part of the population is concerned about posterior crossbite in the primary dentition. Estimates of its prevalence range from 13% to 25%.1,2
Untreated persistent unilateral posterior crossbite may lead to mandibular rotation3 and to functional asymmetry of the temporomandibular joint.4,5 Bilateral posterior crossbite occurs more rarely and can result in mandibular or condylar asymmetry.6 French and American guidelines for orthodontics recommend orthodontic treatment for posterior crossbite to prevent these complications.7,8 It therefore seems relevant to look at early events and habits that might affect this malocclusion.
Posterior crossbite is often associated with anterior open bite,1,9 another malocclusion that develops early in childhood. Most anterior open bites correct spontaneously.9 These two malocclusions seem to share common risk factors.
The major common risk factor is nonnutritive sucking habits, such as pacifier or thumb sucking.1,10–13 The tongue, retained in a low position by pacifier or thumb, may be prevented from applying the pressure needed against the palate for transverse maxillary arch growth. It has been shown that tongue posture on the floor of the mouth is more frequent in children with posterior crossbite.14
A few studies have explored the relations between posterior crossbite11,15,16 or anterior open bite11,16,17 and breast-feeding habits, but these studies vary in the duration and type of breast- feeding considered (exclusive or mixed) and do not always control for nonnutritive sucking habits.
Mouth breathing is another commonly identified risk factor for both posterior crossbite and anterior open bite.18,19 Mouth breathers seem to have a narrower maxilla20,21 and a higher frequency of both posterior crossbite22–24 and anterior open bite25,26 than do nose breathers.
Because etiological mechanisms leading to posterior crossbite and anterior open bite may involve inadequate tongue capacity, factors that could affect lingual functions should be studied. Neurological immaturity in the case of preterm birth or neurological impairment occurring in some small-for-gestational-age (SGA) children may induce neuromotor dysfunction,27 which could affect lingual functions. Preterm birth and SGA might therefore be associated with both malocclusions.
As noted above, these malocclusions share some of the same risk factors. However, except for nonnutritive sucking factors, risk factors for posterior crossbite and those for anterior open bite are poorly known. Our aim was therefore to identify early risk factors for posterior crossbite and for anterior open bite in the primary dentition.
MATERIALS AND METHODS
Population
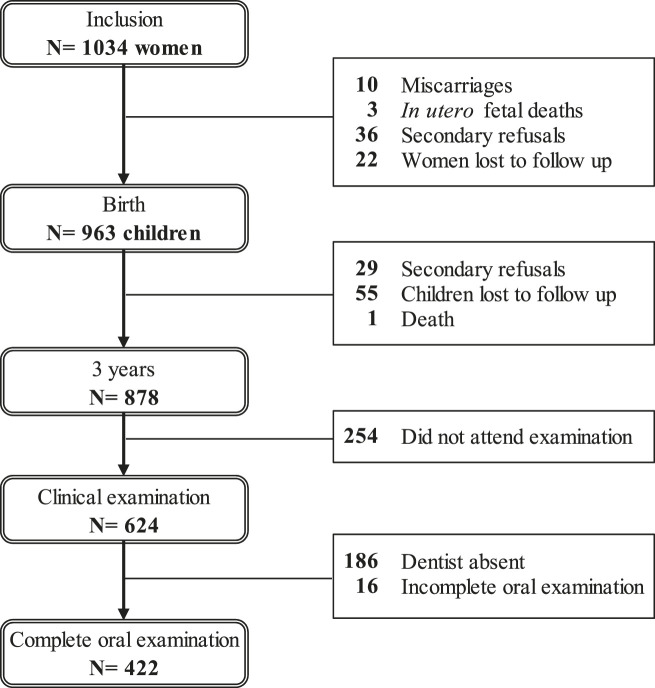
The EDEN mother-child cohort, which aimed to investigate the pre- and early postnatal determinants of child health and development, included pregnant women in the university maternity hospitals of two French cities, Nancy and Poitiers.28 Since oral examination of children was conducted in Nancy only, this study examines only the subjects in Nancy; 1034 women were recruited before the 24th week of gestation between September 2003 and January 2006 (Figure 1). Cohort noninclusion criteria were pregestational diabetes, multiple pregnancy, inability to read French, and plans to move away from the region in the following 3 years. Data at birth were available for 963 children, who were invited to a medical and oral examination at age 3. Oral examinations were performed by three dentists specially trained to follow the specific study protocol. Due to the unexpected unavailability of one of the three dentists, 186 children had no oral examination.
Figure 1.
Participation chart.
The study was approved by the ethics committee of the Kremlin-Bicêtre Hospital and by the Data Protection Authority. Written consent was obtained from the mother for herself at inclusion and for her newborn child after delivery.
Data
Social and demographic characteristics were obtained by interview during pregnancy, with parents’ occupational group defined as the higher occupation in the couple and maternal age determined at birth.
Neonatal characteristics were obtained from the hospital record. Preterm birth was defined as birth before 37 completed weeks of gestation and SGA by a birth weight less than the 10th percentile according to a customized growth model based on the method proposed by Gardosi et al.29
Duration of exclusive or mixed breast-feeding was obtained by self-administered questionnaires sent to the mothers at 4, 8, and 12 months. We considered exclusive breast-feeding and mixed breast-feeding (breast-feeding and formula) together.
Outcomes: For the oral examination, children lay on their mother’s lap and the dentist performed the examination with a mirror and a light. Posterior crossbite was defined by at least one mandibular canine or molar cusp positioned buccal to the maxillary cusp. Anterior open bite was defined by a vertical space (>0 mm) between maxillary and mandibular incisors. Sucking habits at 3 years were collected by interview of the mother during the oral examination. Open lips were observed at rest during the oral examination as a proxy for mouth breathing.
Statistical Analysis
Characteristics of the study sample were compared with those of the other children of the cohort (refusals, children lost to follow-up, those who did not attend the examination, and those with an incomplete oral examination). We next studied the association of posterior crossbite with anterior open bite and then the associations between posterior crossbite and social and neonatal characteristics, duration of breast-feeding, and presence of sucking habits and open lips. To select the subset of risk factors, the P-value threshold of 20 was chosen, following the recommendations when risk factors of disease in question are mostly unknown.30 Two multiple logistic regressions were run: posterior crossbite according to the selected characteristics and anterior open bite according to the same characteristics. The significance level was set at .05. SAS software, version 9.3 (SAS Institute Inc, Cary, NC) was used for multivariate analyses.
RESULTS
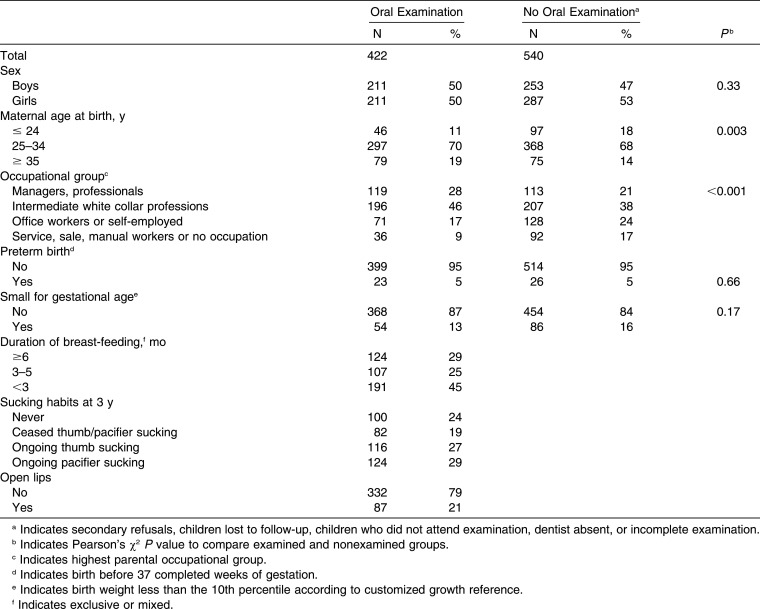
Mothers of the children who were examined were older and had a higher social status than those of the children not examined (Table 1). Frequencies of preterm birth and SGA were similar in both groups.
Table 1.
Description of the Population
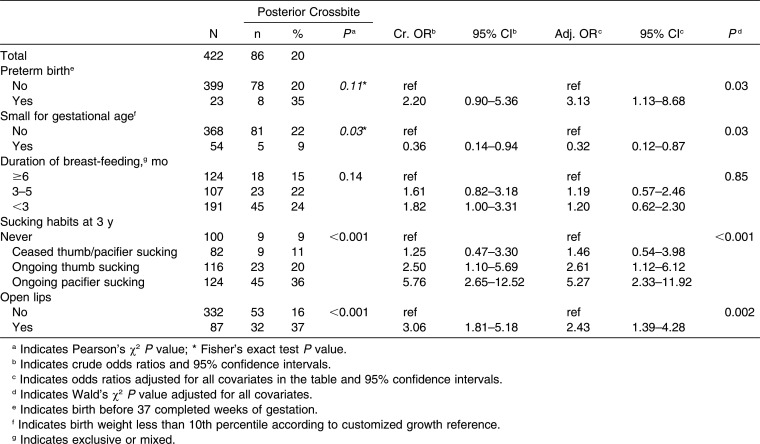
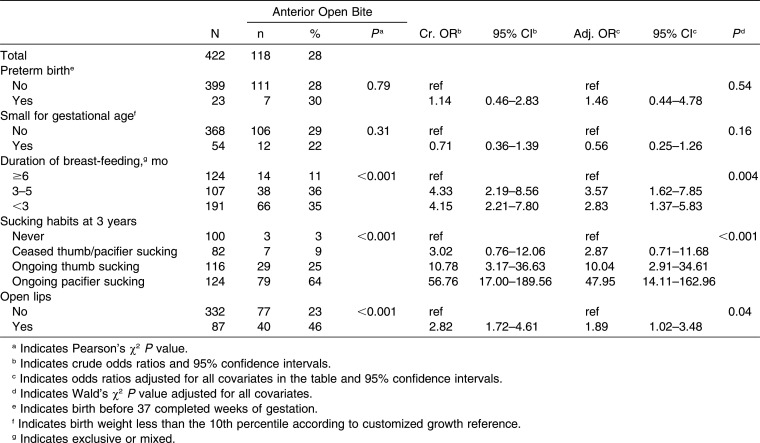
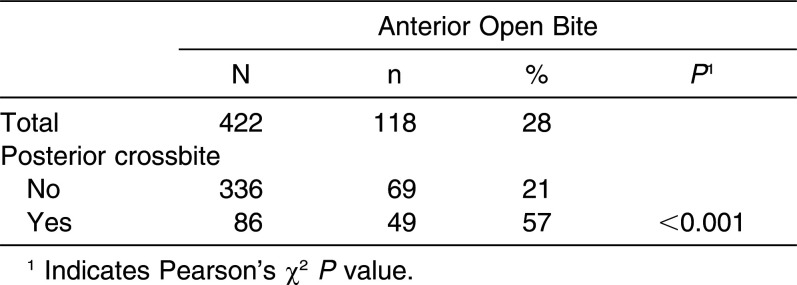
Posterior crossbite was found in 20% of the children (Table 2) and anterior open bite in 28% (Table 3). Posterior crossbite was closely associated with anterior open bite (P < .001); 57% of children with posterior crossbite also had an anterior open bite.
Table 2.
Posterior Crossbite According to Neonatal Characteristics, Duration of Breast-feeding, Sucking Habits, and Open Lips
Table 3.
Anterior Open Bite According to Neonatal Characteristics, Duration of Breast-feeding, Sucking Habits, and Open Lips
Posterior crossbite was not associated with sex (P = 0.63) or parents’ occupational group (P = .64), but was associated with maternal age (P = .05). Because we had no hypothesis underlying this association, maternal age was not included in the multivariate models. Preterm birth, SGA, duration of breast-feeding, sucking habits at 3 years, and open lips were included in the multivariate models. Because lip posture was not recorded for three children, the multivariate models included 419 children.
The frequency of posterior crossbite was higher in children born preterm and lower in SGA children (Table 2). Posterior crossbite was also more frequent in children who sucked their thumbs or pacifiers at 3 years and in children with open lips. Duration of breast-feeding was not associated with posterior crossbite. Anterior open bite was more frequent in children breast-fed less than 6 months, in thumb suckers and especially in pacifier suckers at 3 years, and in children with open lips than in the other children. Anterior open bite was not associated with preterm birth or with SGA (Table 3).
Table 4.
Links Between Posterior Crossbite and Anterior Open Bite
DISCUSSION
This study suggests that preterm birth is a risk factor specific to posterior crossbite and SGA a possible protective factor for posterior crossbite. Our study confirmed that open lips increased the risk for posterior crossbite, with or without anterior open bite.
One strength of our study is that neonatal characteristics and duration of breast-feeding were collected prospectively, which reduced possible errors. The fact that the oral examinations were carried out by only three dentists, specially trained for the study, reduced possible misclassification. Furthermore, the criteria set to identify posterior crossbite were objective and accurate enough for us to believe that the collected information was reliable. Moreover, if misclassification had occurred, it would have been independent of the risk factors and thus have led to an underestimation of the relations.
Only one study has explored the relations between preterm birth and posterior crossbite,31 and the small size of its sample prevented it from reaching a conclusion. An association between gestational age and alteration of palatal morphology has been found in very preterm children.32 In case of preterm birth, even moderately as in the present study, immaturity of lingual functions might have an impact on palatal growth. Preterm babies are more often SGA than others and SGA babies are less often found to have a posterior crossbite. That explains why the association of preterm birth with posterior crossbite became significant when SGA was taken into account. Unexpectedly, SGA appeared as a protective factor for posterior crossbite. A previous study reported a nonsignificant similar trend.17 Tongue overuse could explain this inverse relation between SGA and posterior crossbite. The fast weight catch-up in most SGA babies suggests that they eat more in their first months of life33 and thus probably suck and swallow more often than others. These links between neonatal characteristics and early posterior crossbite need to be confirmed, and these possible explanations should be considered with caution. No association was observed between preterm birth or SGA and anterior open bite. These results suggest that the mechanisms leading to posterior crossbite are different from those leading to anterior open bite.
A nonnutritive sucking habit is the best-known risk factor for posterior crossbite and for anterior open bite.1,10 The association found here seems to concern only children with an ongoing habit, for both malocclusions. Dimberg explored the evolutions of posterior crossbites and anterior open bites from 3 to 11.5 years of age,34 but more longitudinal studies are needed to explore the links between age at which the nonnutritive sucking habit ceased and posterior crossbite and anterior open bite, and their spontaneous correction.
To identify mouth breathers, various authors have used different proxies. We used open lips as a proxy for mouth breathing, but some normal breathers might have been misclassified as mouth breathers, for example, because of open lips due to a cold on the day they were examined. Open lips might therefore slightly overestimate mouth breathing. Nonetheless, the frequency of 21% of open lips in our population is close to that of 19% of mouth breathers in Swedish children of the same age.35 Besides, this potential misclassification should be independent of the studied risk factors and the link between mouth breathing and posterior crossbite using open lips as a proxy is therefore probably only slightly underestimated.
Removal of premature contacts in the primary dentition can prevent a posterior crossbite from persisting into the permanent dentition.36 Later, a quad-helix appliance or an expansion plate can treat posterior crossbite in the mixed dentition.37 It follows that, in some cases of posterior crossbite, early orthodontic treatment is less complex than later comprehensive treatment.38,39 Early diagnosis, therefore, seems to be of meaningful help. However, 3 years is a very early age, and longitudinal studies are needed to understand the evolution of these malocclusions and their relationships with risk factors.
CONCLUSIONS
Preterm birth seems to be a risk factor for early posterior crossbite.
Ongoing sucking habits seem to be risk factors for early posterior crossbite.
SGA appears to be associated with a lower risk of early posterior crossbite.
This study helps to identify new risk factors for posterior crossbite.
Posterior crossbite and anterior open bite may result from different mechanisms.
ACKNOWLEDGMENTS
We are indebted to the participating families and to the midwife research assistants for data collection. We thank Dr C. Jantzen-Olsen for her participation in the oral examinations. We acknowledge all the funding sources for the EDEN study: Fondation pour la Recherche Médicale, French Ministry of Research, IFR and Cohort program, INSERM Nutrition Research Program, French Ministry of Health Perinatality Program, French Agency for Environment Security, French National Institute for Population Surveillance, Paris-Sud University, French National Institute for Health Education, Nestlé, Mutuelle Générale de l’Education Nationale, French-speaking Association for the Study of Diabetes and Metabolism, National Agency for Research (ANR nonthematic program), National Institute for Research in Public Health (TGIR cohort santé 2008 program).
Members of the EDEN Mother-child cohort study group: I. Annesi-Maesano, J. Y. Bernard, J. Botton, M. A. Charles, P. Dargent-Molina, B. de Lauzon-Guillain, P. Ducimetière, M. de Agostini, B. Foliguet, A. Forhan, X. Fritel, A. Germa, V. Goua, R. Hankard, B. Heude, M. Kaminski, B. Larroque, N. Lelong, J. Lepeule, G. Magnin, L. Marchand, C. Nabet, F. Pierre, R. Slama, M. J. Saurel-Cubizolles, M. Schweitzer, and O. Thiebaugeorges.
REFERENCES
- 1.Duncan K, McNamara C, Ireland AJ, Sandy JR. Sucking habits in childhood and the effects on the primary dentition: findings of the Avon Longitudinal Study of Pregnancy and Childhood. Int J Paediatr Dent. 2008;18:178–188. doi: 10.1111/j.1365-263X.2007.00905.x. [DOI] [PubMed] [Google Scholar]
- 2.Dimberg L, Bondemark L, Soderfeldt B, Lennartsson B. Prevalence of malocclusion traits and sucking habits among 3-year-old children. Swed Dent J. 2010;34:35–42. [PubMed] [Google Scholar]
- 3.O’Byrn BL, Sadowsky C, Schneider B, BeGole EA. An evaluation of mandibular asymmetry in adults with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1995;107:394–400. doi: 10.1016/s0889-5406(95)70092-7. [DOI] [PubMed] [Google Scholar]
- 4.Andrade AS, Gaviao MB, Derossi M, Gameiro GH. Electromyographic activity and thickness of masticatory muscles in children with unilateral posterior crossbite. Clin Anat. 2009;22:200–206. doi: 10.1002/ca.20726. [DOI] [PubMed] [Google Scholar]
- 5.Lam PH, Sadowsky C, Omerza F. Mandibular asymmetry and condylar position in children with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1999;115:569–575. doi: 10.1016/s0889-5406(99)70282-9. [DOI] [PubMed] [Google Scholar]
- 6.Veli I, Uysal T, Ozer T, Ucar FI, Eruz M. Mandibular asymmetry in unilateral and bilateral posterior crossbite patients using cone-beam computed tomography. Angle Orthod. 2011;81:966–974. doi: 10.2319/022011-122.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ANAES . Paris: ANAES; 2002. Indications de l’Orthopédie Dento-Faciale et Dento-Maxillo-Faciale; p. 10. [Google Scholar]
- 8.AAO . St Louis: American Association of Orthodontists; 2008. Clinical Practice Guidelines for Orthodontics and Dentofacial Orthopedics; p. 6. [Google Scholar]
- 9.Dimberg L, Lennartsson B, Soderfeldt B, Bondemark L. Malocclusions in children at 3 and 7 years of age: a longitudinal study. Eur J Orthod. 2013;35:131–137. doi: 10.1093/ejo/cjr110. [DOI] [PubMed] [Google Scholar]
- 10.Warren JJ, Slayton RL, Bishara SE, et al. Effects of nonnutritive sucking habits on occlusal characteristics in the mixed dentition. Pediatr Dent. 2005;27:445–50. [PubMed] [Google Scholar]
- 11.Viggiano D, Fasano D, Monaco G, Strohmenger L. Breast feeding, bottle feeding, and non-nutritive sucking: effects on occlusion in deciduous dentition. Arch Dis Child. 2004;89:1121–1123. doi: 10.1136/adc.2003.029728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heimer MV, Tornisiello Katz CR, Rosenblatt A. Non-nutritive sucking habits, dental malocclusions, and facial morphology in Brazilian children: a longitudinal study. Eur J Orthod. 2008;30:580–585. doi: 10.1093/ejo/cjn035. [DOI] [PubMed] [Google Scholar]
- 13.Petren S, Bondemark L, Soderfeldt B. A systematic review concerning early orthodontic treatment of unilateral posterior crossbite. Angle Orthod. 2003;73(5):588–596. doi: 10.1043/0003-3219(2003)073<0588:ASRCEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Volk J, Kadivec M, Music MM, Ovsenik M. Three-dimensional ultrasound diagnostics of tongue posture in children with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 2010;138:608–612. doi: 10.1016/j.ajodo.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 15.Karjalainen S, Ronning O, Lapinleimu H, Simell O. Association between early weaning, non-nutritive sucking habits and occlusal anomalies in 3-year-old Finnish children. Int J Paediatr Dent. 1999;9:169–173. doi: 10.1046/j.1365-263x.1999.00133.x. [DOI] [PubMed] [Google Scholar]
- 16.Chen X, Xia B, Ge L. Effects of breast-feeding duration, bottle-feeding duration and non-nutritive sucking habits on the occlusal characteristics of primary dentition. BMC Pediatr. 2015;15:46. doi: 10.1186/s12887-015-0364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peres KG, Barros AJ, Peres MA, Victora CG. Effects of breastfeeding and sucking habits on malocclusion in a birth cohort study. Rev Saude Publica. 2007;41:343–350. doi: 10.1590/s0034-89102007000300004. [DOI] [PubMed] [Google Scholar]
- 18.Gois EG, Ribeiro-Junior HC, Vale MP, et al. Influence of nonnutritive sucking habits, breathing pattern and adenoid size on the development of malocclusion. Angle Orthod. 2008;78:647–654. doi: 10.2319/0003-3219(2008)078[0647:IONSHB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Malandris M, Mahoney EK. Aetiology, diagnosis and treatment of posterior cross-bites in the primary dentition. Int J Paediatr Dent. 2004;14:155–166. doi: 10.1111/j.1365-263X.2004.00546.x. [DOI] [PubMed] [Google Scholar]
- 20.Cheng MC, Enlow DH, Papsidero M, et al. Developmental effects of impaired breathing in the face of the growing child. Angle Orthod. 1988;58:309–320. doi: 10.1043/0003-3219(1988)058<0309:DEOIBI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Bresolin D, Shapiro GG, Shapiro PA, et al. Facial characteristics of children who breathe through the mouth. Pediatrics. 1984;73:622–625. [PubMed] [Google Scholar]
- 22.Souki BQ, Pimenta GB, Souki MQ, et al. Prevalence of malocclusion among mouth breathing children: do expectations meet reality. Int J Pediatr Otorhinolaryngol. 2009;73:767–773. doi: 10.1016/j.ijporl.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Harari D, Redlich M, Miri S, Hamud T, Gross M. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. Laryngoscope. 2010;120:2089–2093. doi: 10.1002/lary.20991. [DOI] [PubMed] [Google Scholar]
- 24.Lofstrand-Tidestrom B, Thilander B, Ahlqvist-Rastad J, Jakobsson O, Hultcrantz E. Breathing obstruction in relation to craniofacial and dental arch morphology in 4-year–old children. Eur J Orthod. 1999;21:323–332. doi: 10.1093/ejo/21.4.323. [DOI] [PubMed] [Google Scholar]
- 25.Lopatiene K, Babarskas A. [Malocclusion and upper airway obstruction] Medicina. 2002;38(3):277–283. Kaunas. [PubMed] [Google Scholar]
- 26.Vazquez-Nava F, Quezada-Castillo JA, Oviedo-Trevino S, et al. Association between allergic rhinitis, bottle feeding, non-nutritive sucking habits, and malocclusion in the primary dentition. Arch Dis Child. 2006;91:836–840. doi: 10.1136/adc.2005.088484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Larroque B, Ancel PY, Marret S, et al. Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): a longitudinal cohort study. Lancet. 2008;371:813–820. doi: 10.1016/S0140-6736(08)60380-3. [DOI] [PubMed] [Google Scholar]
- 28.EDEN http://eden.vjf.inserm.fr/index.php/en .
- 29.Gardosi J, Chang A, Kalyan B, Sahota D, Symonds EM. Customised antenatal growth charts. Lancet. 1992;339:283–287. doi: 10.1016/0140-6736(92)91342-6. [DOI] [PubMed] [Google Scholar]
- 30.Greenland S, Rothman K. Introduction to stratified analysis. Modern Epidemiology. Philadelphia. In: Rothman K, Greenland S, editors. Lippincott Williams & Wilkins; 1998. pp. 256–257. [Google Scholar]
- 31.Paulsson L, Soderfeldt B, Bondemark L. Malocclusion traits and orthodontic treatment needs in prematurely born children. Angle Orthod. 2008;78:786–792. doi: 10.2319/083007-402.1. [DOI] [PubMed] [Google Scholar]
- 32.Germa A, Marret S, Thiriez G, et al. Neonatal factors associated with alteration of palatal morphology in very preterm children: the EPIPAGE cohort study. Early Hum Dev. 2011 doi: 10.1016/j.earlhumdev.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 33.Larsen T, Greisen G, Petersen S. Intrauterine growth correlation to postnatal growth—influence of risk factors and complications in pregnancy. Early Hum Dev. 1997;47:157–165. doi: 10.1016/s0378-3782(96)01780-x. [DOI] [PubMed] [Google Scholar]
- 34.Dimberg L, Lennartsson B, Arnrup K, Bondemark L. Prevalence and change of malocclusions from primary to early permanent dentition: a longitudinal study. Angle Orthod. 2015;85:728–734. doi: 10.2319/080414-542.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dimberg L, Lennartsson B, Soderfeldt B, Bondemark L. Malocclusions in children at 3 and 7 years of age: a longitudinal study. Eur J Orthod. 2011;35:131–137. doi: 10.1093/ejo/cjr110. [DOI] [PubMed] [Google Scholar]
- 36.Harrison JE, Ashby D. Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev. 2008:CD000979. doi: 10.1002/14651858.CD000979. [DOI] [PubMed] [Google Scholar]
- 37.Petren S, Bjerklin K, Bondemark L. Stability of unilateral posterior crossbite correction in the mixed dentition: a randomized clinical trial with a 3-year follow-up. Am J Orthod Dentofacial Orthop. 2011;139:e73–e81. doi: 10.1016/j.ajodo.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 38.King GJ, Spiekerman CF, Greenlee GM, Huang GJ. Randomized clinical trial of interceptive and comprehensive orthodontics. J Dent Res. 2012;91(suppl 1):59S–64S. doi: 10.1177/0022034512448663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Muchitsch AP, Winsauer H, Wendl B, et al. Remodelling of the palatal dome following rapid maxillary expansion (RME): laser scan-quantifications during a low growth period. Orthod Craniofac Res. 15:30–38. doi: 10.1111/j.1601-6343.2011.01534.x. [DOI] [PubMed] [Google Scholar]