Abstract
Objective
COVID-19-associated non-pharmaceutical interventions (NPI) have disrupted respiratory viral transmission. We quantified the changes in pediatric hospital admissions in 2020 from five different NPI phases in Western Australia for acute lower respiratory infections (ALRI) in children in the context of all-cause admissions.
Study Design and Setting
We assessed anonymised hospitalization data from Perth Children's Hospital (Jan 2015-Dec 2020) for all-cause admissions, ALRI, febrile illnesses and trauma (negative control) in those <17 years. We evaluated absolute changes in admissions and the weekly change estimated from interrupted time-series models.
Results
The absolute number of admissions was comparable in 2020 (15,678) vs. 2015 to 2019 average (15,310). Following the introduction of strict NPIs, all-cause admissions declined by 35%, recovered to pre-pandemic levels, then increased by 24% following NPI cessation. ALRI admissions in children <5 years initially declined by 89%, which was sustained throughout the gradual easing of NPI until an increase of 579% (997% in <3 months) following the final easing of NPI. Admissions for trauma showed minimal changes in 2020 compared to preceding years.
Conclusion
COVID-19-associated NPI had significant unintended consequences in health service utilization, especially for ALRI and infants <3 months, prompting the need to understand viral transmission dynamics in young children.
Keywords: Non-pharmaceutical interventions, hospitalization, acute lower respiratory infections, pediatric epidemiology, COVID-19
What is new?
-
•
COVID-19 non-pharmaceutical interventions (NPI) have had been associated with disrupted patterns of respiratory viruses, but the individual impacts of different NPI measures is unknown. In 2020, Western Australia experienced shorter and less stringent periods of NPI than the rest of Australia with no mandatory mask wearing.
-
•
In Western Australia's only tertiary pediatric hospital, we observed all-cause hospitalization admissions initially decline by 35%, recover to normal levels and then increase by 24% following the cessation of different NPI phases compared with a counterfactual scenario of no NPI measures.
-
•
With ALRI admissions, the introduction of NPIs saw a decline of 89% that was sustained until most NPI restrictions were lifted, then saw increases of 579% for children <5 years and up to 997% in infants <3 months coinciding with the return of interstate travel.
-
•
Respiratory syncytial virus (RSV) is the most common cause of ALRI hospitalisations and viral detections in 2020 followed the patterns we observed in ALRI. We need to continuously monitor ALRI trends following the continued use of NPI, to better understand RSV viral transmission dynamics, especially as licensure of new prevention products, including monoclonal antibodies, appears imminent.
1. Introduction
Non-pharmaceutical interventions (NPIs) were used in many jurisdictions to mitigate the effects of the COVID-19 pandemic. Such NPI measures including physical distancing, increased hand hygiene, travel restrictions and widespread border closures, implemented to reduce virus transmission, have resulted in multiple human behavioural changes and unforeseen health service utilisation impacts. Globally, acute lower respiratory infection (ALRI) is a leading cause of hospitalisation in children, with respiratory syncytial virus (RSV) the major pathogen, traditionally exhibiting clear winter peaks. [1,2] NPIs have disrupted viral transmission patterns of RSV and other respiratory pathogens, including influenza, [3], [4], [5], [6], [7], [8], [9] and reduced non-COVID-19 infection-related hospitalisations. [10,11] These early reports have been unable to distinguish different impacts of individual NPIs in the apparent suppression of respiratory illnesses. Additionally, most of these reports assessed the differences in viral detection rates or hospitalizations over an incomplete year in 2020 and compared patterns to only a single previous year. Infectious diseases are known to fluctuate annually. Hence, comparisons to understand the impact of NPIs should ideally include more than one pre-pandemic year and one complete season. This expanded comparison is particularly vital to overcome bias due to unseasonal epidemics, such as the high rate of influenza infections seen across Australia in 2019 which translated into higher than average hospitalisations. [12]
Western Australia (WA) has had relatively low case numbers of COVID-19 (1021 total cases to 28 June 2021 with 89.4% linked to international travel [13]) and has experienced a shorter and less stringent period of NPI than other parts of Australia. Nevertheless, we reported marked changes in respiratory viruses with initial reductions of 99.4% for influenza detections and 98.0% for RSV. [14] This was followed by a dramatic resurgence of RSV at the end of 2020 to higher than normal seasonal epidemic levels. [15] Here, we aim to quantify the impact of NPI measures covering both periods of suppression and resurgence of RSV on pediatric hospital admissions for ALRI in the context of all-cause hospital admissions from the previous five years. We employ interrupted time series (ITS) analyses by age and diagnosis to identify the most sensitive of the restriction measures to changes in hospitalization patterns.
2. Methods
2.1. Study Population and Data Source
WA encompasses the western third of Australia with a population of 2.67 million (31 December 2020), [16] approximately 75% of whom reside in the metropolitan area of the capital city, Perth. We obtained anonymized individual-level hospitalization data from Perth Children's Hospital, the only tertiary pediatric hospital in WA between January 1, 2015 and December 31, 2020 for all-cause admissions in children aged <17 years. Admissions of <24 hours duration were excluded. Each admission record included one or more diagnosis codes using the International Classification of Diseases diagnosis codes, version 10, Australian modification (ICD-10-AM). The resident population in the Perth metropolitan area was estimated from Australian Bureau of Statistics. [17]
2.2. Outcome measures
We categorized admissions into pre-specified diagnostic groups based on our previous work. [18] Our primary outcome of interest was ALRI as identified by a primary or secondary diagnosis of bronchiolitis (J21), pneumonia (J12-J18, B59, B05.2, B37.1, B01.2), influenza (J10-J11), whooping cough (A37), and unspecified acute lower respiratory infection (J22). As pathogen-specific codes are not reliable, [19] ALRI codes were grouped for our analysis. We also assessed trends for febrile and other viral illnesses (R50, R56, B34, P90), all-cause hospital admissions and admissions for trauma and external causes (S00-T00) as a negative control, chosen a priori as reasons for hospitalization that would not be affected by altered respiratory viral transmission dynamics due to COVID-19-associated NPIs. As younger children experience a higher health burden, we grouped ALRI admissions in those aged less than 3 months, 3-11 months and 1-4 years.
2.3. Stages of non-pharmaceutical interventions in WA
We categorized 2020 into five discrete periods based on the timing of NPI implementation and easing using calendar week as follows:
Pre-restriction (weeks 1-13 inclusive): This represents the pre-pandemic period with no formal NPIs. In Australia, the international border was closed to non-residents on 20 March 2020, with the WA state border closed to the other Australian states from 6 April.
Period 1 (weeks 14-17 inclusive): State-wide stay-at-home restrictions were in place from 29 March to 26 April including the closure of schools and regional borders within WA to further restrict population movement. This period had the most stringent NPI. Childcare centers remained open, but parents were encouraged to keep young children at home.
Period 2 (weeks 18-26 inclusive): From the end of April, restrictions were eased in a staged fashion, [20] commencing on 27 April with Phase 1 including gatherings of up to 10 people, with schools reopening on 29 April. School attendance reached >85% by mid-May. [21] Phase 2 commenced on 18 May with a social distancing rule of 4m [2] per person and gatherings of up to 20 people. Phase 3 began on 6 June with a social distancing rule of 2m [2] per person and gatherings of up to 100 people permitted.
Period 3 (weeks 27-46 inclusive): Phase 4 began on 27 June, which saw an approximate return to everyday practices with only major sporting and entertainment venues capped to 50% capacity. [20] This phase remained in place for the remainder of 2020. The majority of regional border restrictions within WA were lifted on 5 June. [22]
Period 4 (weeks 47-52 inclusive): This period saw the continuation of Phase 4 plus easing of interstate border restrictions for travellers from other states within Australia. This phase began on 14 November, with quarantine not required for travellers from states with no recorded community transmission of COVID-19. [23]
It should be noted that mask wearing was not mandated inWA in 2020. Throughout these staged relaxations (Periods 2-4), the importance of hand hygiene was maintained and communicated publicly through media campaigns and places of work and education. WA has also held a hard border to all international visitors with a strict requirement of 14 days in hotel quarantine for any returning overseas traveller. [24]
2.4. Statistical analysis
We compared the total number of admissions in 2020 to the average of the previous 5 years (2015-2019) in the five NPI periods and quantified the percentage change in absolute admission numbers. The average of the preceding five years was used to minimize bias of single year fluctuations. We conducted interrupted time series (ITS) analyses with negative binomial regression on the series of weekly admissions from 2015 to 2020. The ITS models included a binary variable to indicate the breakpoints in 2020 according to the NPI period (1 if the observed week was a breakpoint, 0 if otherwise), a covariate for time (week), harmonic terms to account for seasonality and the age-structured annual metropolitan population count as an offset. Further details on the model specifications are outlined in Supplementary material. The primary ITS model included two breakpoints indicating the start of Period 1 (start of NPI) and Period 4 (easing of NPI). We present results for all-cause admissions in children aged <17 years; ALRI in the pre-specified age groups (<3 months, 3-11 months, 1-4 years); febrile and other viral illnesses in children <5 years; and trauma admissions (negative control) in children <17 years (further groups presented in Supplementary material). We then performed secondary ITS models for each of the five breakpoints identified by NPI restriction periods for all-cause admissions in children <17 years, ALRI <5 years and trauma <17 years. These secondary ITS models assessed the changes between different periods to identify the NPI characteristic that resulted in the largest impact on health service utilisation. The estimated incidence rate ratio for the binary variable in each ITS provided the relative decline or increase with 95% confidence intervals (CI) in admissions with the differing NPI periods. We conducted a sensitivity analysis assessing admissions by primary diagnosis only.
2.5. Ethics
Ethical approval for this study was granted by the WA Child and Adolescent Health Services (RGS4320) with data provided under a waiver of consent. The research project was guided by two community research buddies identified through a community reference group.
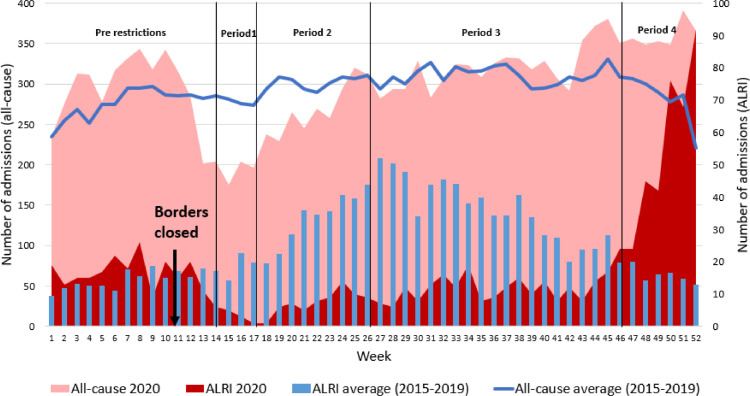
3. Results
There were 15,678 admissions overall in 2020 compared to an annual average of 15,310 from 2015 to 2019. Most admissions (93.3%) had up to 10 diagnosis codes recorded (range:1-70; median: 4). In Period 1, following the introduction of strict NPIs, all-cause admissions declined by 30% compared with the previous five years (Table 1 ). However, the number of admissions began to decline by week 11, two weeks before the formal start of the first NPI period (Fig. 1 ). As the restrictions eased across Periods 2 and 3, all-cause admissions in 2020 returned to pre-pandemic average levels by the end of Period 3. Hospital admissions then increased in Period 4, with numbers of all-cause admissions 29% higher than the same period from 2015 to 2019 (Table 1). ALRI admissions across all age groups also declined following Period 1 by 79% and remained at low levels before increasing in Period 4 by 269% compared with the previous five years (Fig. 1, Table 2 ).
Table 1.
Total number of all-cause admissions by age groups in the period 2015 to 2019 (average) and in 2020 during the different restriction periods
| Age Group | Number of admissions | By NPI Phase |
Overall | ||||
|---|---|---|---|---|---|---|---|
| Pre-restrictions | Period 1 | Period 2 | Period 3 | Period 4 | |||
| Overall | 2015-19 (Average) | 3586 | 1116 | 2718 | 6210 | 1681 | 15,310 |
| 2020 | 3868 | 779 | 2431 | 6436 | 2164 | 15,678 | |
| % changea | 8% | -30% | -11% | 4% | 29% | 2% | |
| <3 months | 2015-19 (Average) | 408 | 137 | 332 | 841 | 226 | 1945 |
| 2020 | 722 | 203 | 450 | 1084 | 396 | 2855 | |
| % changea | 77% | 48% | 35% | 29% | 75% | 47% | |
| 3-11 months | 2015-19 (Average) | 316 | 93 | 224 | 590 | 154 | 1377 |
| 2020 | 321 | 55 | 169 | 530 | 206 | 1281 | |
| % changea | 2% | -41% | -25% | -10% | 33% | -7% | |
| 1-4 years | 2015-19 (Average) | 835 | 274 | 656 | 1478 | 373 | 3616 |
| 2020 | 823 | 116 | 447 | 1315 | 571 | 3272 | |
| % changea | -1% | -58% | -32% | -11% | 53% | -10% | |
| 5-16 years | 2015-19 (Average) | 2027 | 613 | 1505 | 3301 | 927 | 8373 |
| 2020 | 2002 | 405 | 1365 | 3507 | 991 | 8270 | |
| % changea | -1% | -34% | -9% | 6% | 7% | -1% | |
% change in 2020 vs. average from 2015 to 2019
Figure 1.
Frequency of all-cause inpatient hospital admissions and ALRI admissions in children aged less than 17 years in 2020 compared to the average in 2015 to 2019
Table 2.
Total number of admissions for ALRI by age groups in the period 2015 to 2019 (average) and in 2020 during the different restriction periods
| Age Group | Number of admissions | By NPI Phase |
Overall | ||||
|---|---|---|---|---|---|---|---|
| Pre-restrictions | Period 1 | Period 2 | Period 3 | Period 4 | |||
| Overall | 2015-19 (Average) | 187 | 73 | 299 | 708 | 94 | 1,361 |
| 2020 | 220 | 15 | 69 | 244 | 347 | 895 | |
| % changea | 18% | -79% | -77% | -66% | 269% | -34% | |
| <3 months | 2015-19 (Average) | 19 | 10 | 51 | 125 | 12 | 216 |
| 2020 | 23 | 1 | 8 | 26 | 86 | 144 | |
| % changea | 21% | -90% | -84% | -79% | 617% | -33% | |
| 3-11 months | 2015-19 (Average) | 41 | 17 | 61 | 173 | 23 | 315 |
| 2020 | 62 | 2 | 12 | 66 | 78 | 220 | |
| % changea | 51% | -88% | -80% | -62% | 239% | -30% | |
| 1-4 years | 2015-19 (Average) | 63 | 24 | 105 | 228 | 28 | 448 |
| 2020 | 61 | 3 | 19 | 96 | 152 | 331 | |
| % changea | -3% | -88% | -82% | -58% | 443% | -26% | |
| 5-16 years | 2015-19 (Average) | 64 | 22 | 82 | 182 | 31 | 382 |
| 2020 | 74 | 9 | 30 | 56 | 31 | 200 | |
| % changea | 16% | -59% | -63% | -69% | 0% | -48% | |
% change in 2020 vs. average from 2015 to 2019
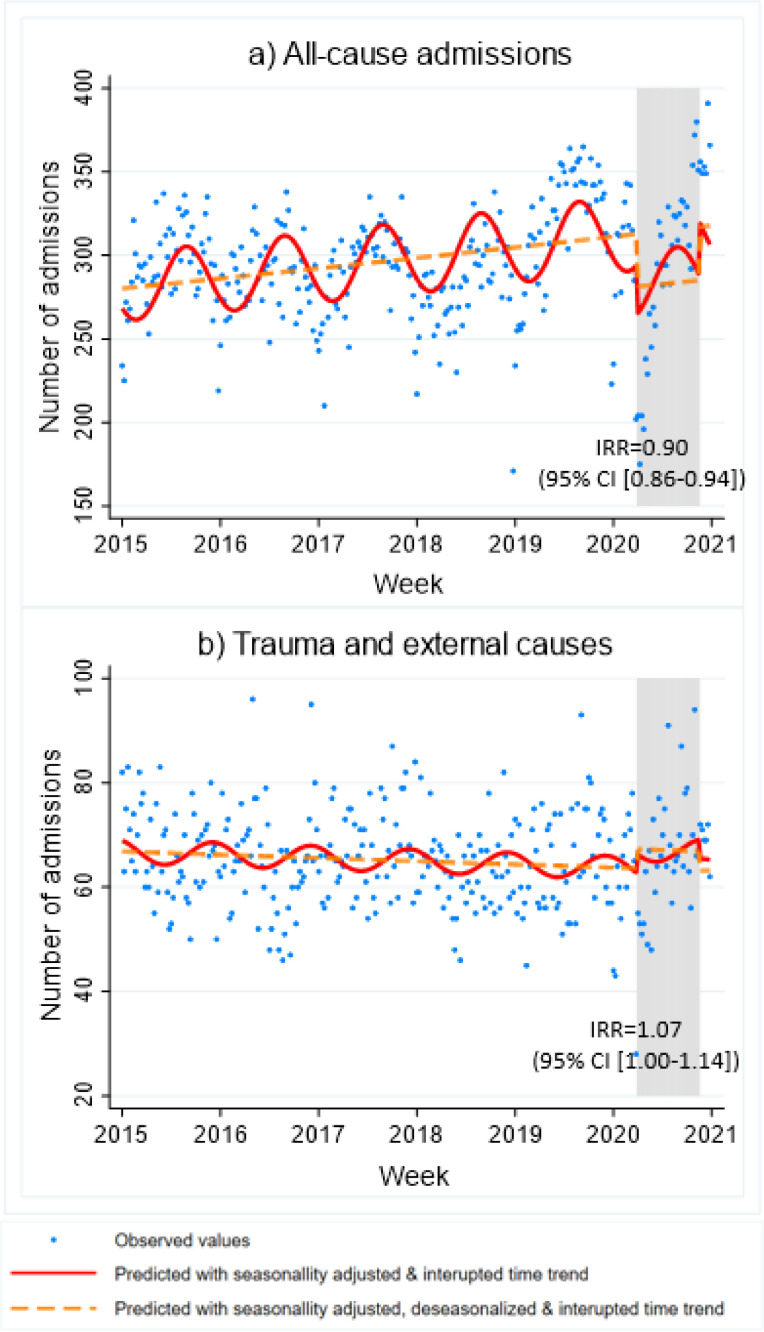
From our primary ITS model that accounted for annual seasonality and population offset, all-cause pediatric admissions were increasing at a rate of 0.01% per week (Fig. 2 A) but significantly declined by 10% following the introduction of NPIs across Periods 1, 2 and 3 (IRR=0.90 [95% CI: 0.86-0.94]). Conversely, admissions for trauma, as our negative control, showed an increase of 7% (IRR=1.07 [95%CI: 1.00-1.14]) following the introduction of the NPI period in 2020 compared with the longitudinal trend since 2015 (Fig. 2B).
Figure 2.
Interrupted-time series model of weekly hospital admissions in children aged <17 years for (A) all-cause admissions and (B) trauma and external causes (negative control) from 2015 to 2020
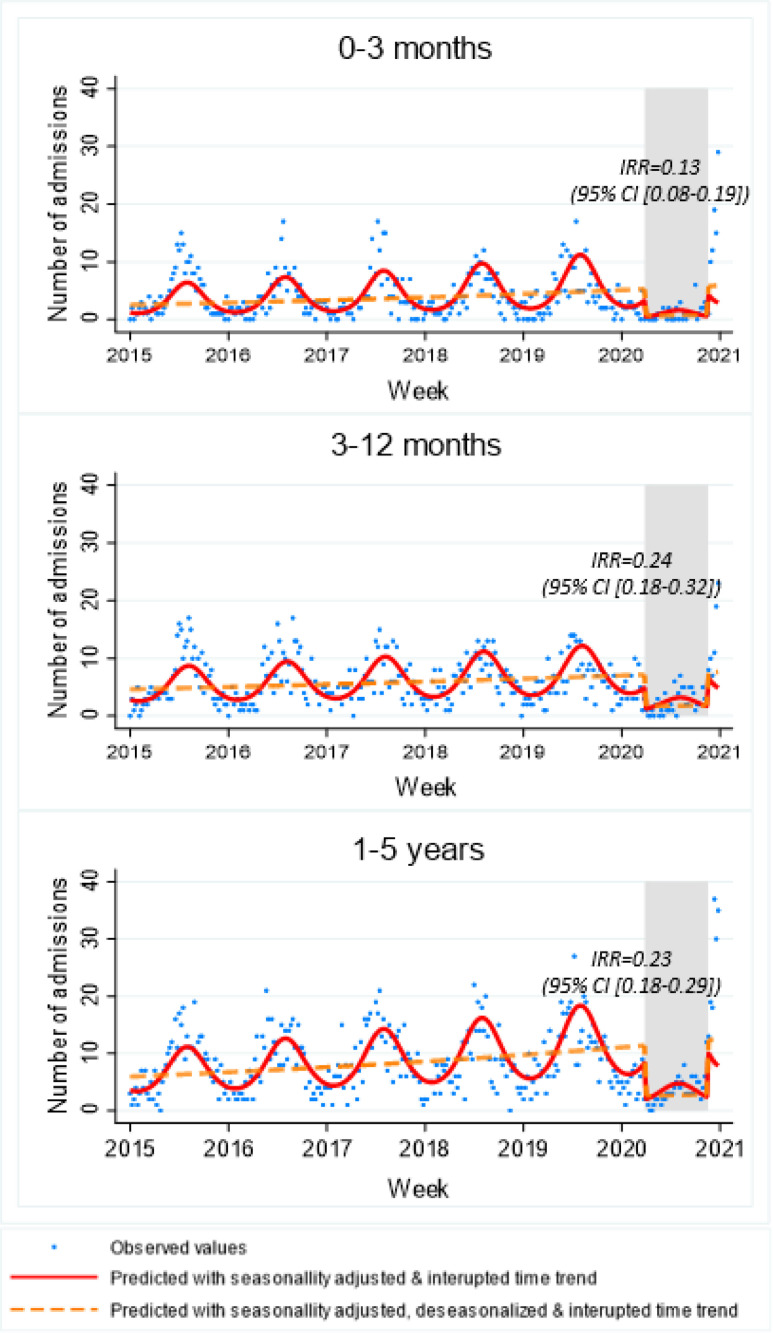
The magnitude of change in ALRI admissions differed across age groups with infants aged <3 months experiencing the greatest change. Period 1 saw a 90% absolute reduction in the number of admissions in this age group. This was opposite to all-cause admissions in those <3 months where absolute admissions were 48% higher (Table 1). The reduction in ALRI admissions was sustained through Period 2 and 3; and was then followed by a 617% absolute increase at the start of Period 4. Similar patterns for ALRI were seen in young children aged 3-11 months and 1-4 years (Table 2). For children aged 5-16 years, absolute reductions across Periods 1-3 of 59-69% were observed in 2020 compared with the 2015 to 2019 average. However, the absolute numbers of ALRI admissions in this age group were unchanged in Period 4 (Table 2). The primary ITS models accounting for annual seasonality and population offset for ALRI admissions in children <5 years are shown in Figure 3 . Declines were seen across all age groups following NPI introduction measures but were again greater in those aged <3 months than other age groups in young children, with a reduction of 87% (IRR=0.13 [95% CI: 0.08-0.19]; Fig. 3). Admissions for febrile and other viral illnesses in children <5 years showed similar declines to all-cause admissions following NPI introduction (IRR=0.82 [95% CI: 0.70-0.96]) despite the longitudinal trend showing a decline in these admissions from 2015 (Supplementary Table 2, Supplementary Figure 1).
Figure 3.
Interrupted-time series model of weekly hospital admissions by age group in children aged <5 years for ALRI from 2015 to 2020
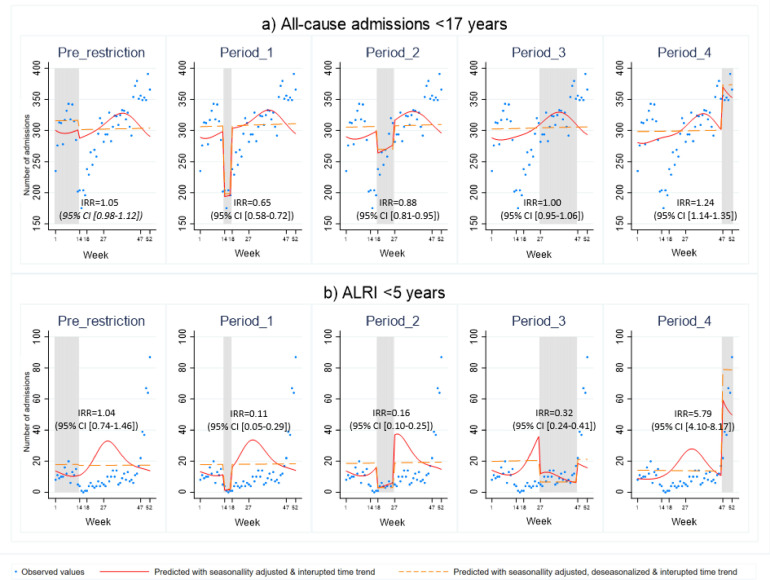
The secondary ITS models assessed the changes according to each NPI period. For all-cause pediatric admissions, the pre-restriction period saw a 5% increase (IRR=1.05 [95% CI: 0.98-1.12]) in weekly hospitalizations compared to the longitudinal trend from 2015. The commencement of restrictions in Period 1 saw the biggest change in magnitude with a 35% decline (IRR=0.65 [95% CI: 0.58-0.72]) compared to the counterfactual scenario with no NPIs. With the transition to Period 2, a smaller decline of 12% was seen (IRR=0.88 [95% CI: 0.81-0.94]) with no significant change detected with the move to Period 3, reflecting when absolute admission numbers had returned to pre-pandemic levels. Following the change to Period 4, admissions increased by 24% (IRR=1.24 [95% CI: 1.14-1.35]) compared to the 2015 to 2019 longitudinal trend (Fig. 4 A). These changes were more marked for ALRI in children aged <5 years, where reductions in Period 1 were 89% (IRR=0.11 [95% CI: 0.04-0.29]), a smaller decline of 84% (IRR=0.16 [95% CI: 0.10-0.25]) in Period 2, sustained decline of 68% (IRR=0.32 [95% CI: 0.24-0.41]) in Period 3 before a dramatic increase of 579% (IRR=5.79 [95% CI: 4.10-8.17]) in Period 4 (Fig. 4B). The increase in Period 4 was highest in infants aged <3 months with a 997% per week (IRR=9.97 [95% CI: 6.09-16.30]) increase (Supplementary Table 1). Similar patterns in the ITS models were seen when only the primary diagnosis code was used (Supplementary Table 1).
Figure 4.
Secondary interrupted-time series models by each NPI restriction period of weekly hospital admissions in 2020 for (A) all-cause admissions <17 years, and (B) ALRI <5 years
4. Conclusion
Public health measures used to mitigate the impact of COVID-19 have had significant unintended consequences in pediatric health service utilization, with marked changes for ALRI and especially for ALRI in infants aged less than three months. In WA's only tertiary pediatric hospital, we observed all-cause hospitalization initially decline by 35%, recover to normal levels and then increase by 24% following the cessation of NPI compared with a counterfactual scenario of no NPI measures. For ALRI, the introduction of NPIs saw a decline of 89% that was sustained until Period 4, when admissions increased by 579% for children aged less than five years and up to 997% in young infants. This period saw the final easing of NPI with the careful reintroduction of interstate travel to WA.
Differentiating the impact of individual NPI measures on health service utilization is difficult as NPI measures can cause changes in health-seeking behavior as well as actual changes in disease incidence through altered pathogen transmission dynamics. We conducted multiple ITS models to tease out the impacts on health service utilization according to the staged implementation of NPI in our jurisdiction. Not surprisingly, the most effective measure to minimize hospitalization was widespread restrictions, experienced early in the pandemic with school closures and strict stay-at-home orders. These measures suppressed ALRI admissions that was then sustained for most of 2020, while all-cause admissions recovered to pre-pandemic levels; especially in the period that saw a return to everyday activities with the exception of international and interstate travel. There are now multiple reports of the remarkable and immediate impact of NPIs on pediatric hospitalizations globally, often with a greater reduction in respiratory infection-related admissions than other infections such as urinary tract infections and skin and soft tissue infections and non-infectious admissions such as cancer.[11, [25], [26], [27]] It is important to note that schools were only closed for four weeks in WA (which included the normal two-week April school holiday period), childcare centers remained open and there was no mandate of mask wearing. Our school closure was a much shorter duration than other countries and yet we still noted a dramatic immediate and sustained decline in ALRI and febrile admissions.
Infectious diseases are the primary reasons for hospitalization in WA [28], with ALRI accounting for the largest burden. [29] While all-cause admissions saw an increase following the last period of restrictions being eased, the changes with ALRI were the driving force behind that increase, with a 579% increase in children aged less than 5 years. RSV, the major contributor of ALRI burden in WA [2], surged unexpectedly in late 2020 in our population [15] although with minimal difference in disease severity. [30] This summer resurgence and concomitant increase in ALRI hospitalizations as reported here, coincided with the relaxation of the interstate border, months after other NPI measures across WA were relaxed. Our data suggest that the extended closure of our state border, preventing the introduction of viruses from international and national sources, decreased population movement, and subsequent community transmission, may play a role in the sustained reduction in respiratory viral transmission. This is more so than strict social distancing and school closure NPI measures which were short-lived in our population. This provides important insights into respiratory viral transmission, especially as school children are known to be the main transmitters of infection and social distancing of this group will likely impact transmission. [31] Recent genomic analysis of RSV strains from WA, Victoria and New South Wales indicates that WA RSV activity was due to a separate lineage than other Australian RSV outbreaks, [32] suggesting that relaxation of interstate borders was not likely the pivotal event to reintroduce RSV circulation in WA. Another possible explanation is the unusual weather conditions experienced in Perth in November 2020, with the recorded highest rainfall in the past 140 years, and the coolest temperate in the past 12 years. [33] However, there is no clear explanation why these meteorological conditions would only affect RSV circulation and not other respiratory viruses commonly affecting children. Further study into the role of meteorological and environmental factors on viral infections is needed. It is also possible that the increased size of the RSV-naïve population due to the attenuated 2020 winter season overcame the usual climactic factors associated with RSV transmission, leading to the observed inter-seasonal surge, at levels well above the usual seasonal peak.
Several reports have emerged on the RSV resurgence following extended periods of suppression due to NPIs, including New Zealand [34] and France [35], with no clear explanation as to the driving force. Our data coupled with international reports of unusual RS seasonality raise questions as to the most optimal seasonal-based prevention strategy and warrants further investigation into RSV transmission dynamics. No licensed RSV vaccine exists, yet a range of vaccines and longer-lasting monoclonal antibodies are in late-stage clinical trials. It is important to note that while RSV no doubt has driven the increase in ALRI in young children and there also has been no return of influenza virus activity, other aetiologies could be playing a role. Indeed, not all respiratory viruses associated with ALRI, including rhinovirus and adenovirus, experienced similar dramatic changes following NPI. [36]
Our study does have some notable limitations. We only included admissions from Perth Children's Hospital, and therefore, our study is not representative of all WA pediatric hospitals. However, we have no reason to believe that the patterns due to NPI would be different in this hospital compared to others admitting pediatric patients. We are in the process of obtaining total population-based data through record linkage mechanisms, to provide >10 years of population-based data to validate and strengthen our findings. We used dates of the NPI restriction phases according to state Government advice. [20] However, in the early phases of the pandemic, when community knowledge of COVID-19 was low, and there was worldwide media attention, parents may have already altered their health-seeking behavior and hygiene practices before the introduction of NPI restrictions. Indeed, our descriptive analysis showed a marked decline in admissions in the 2 weeks prior to the NPI commencement. While ALRI admissions contributed to the decrease in overall hospital use, there are likely other conditions that increased over this time during the NPI periods. The negative effect of NPI on mental health in children is expected to be one of these other conditions, which warrants further investigation. Our ITS approach measured the effect of NPI's compared to a counterfactual scenario of no NPI. While this method is theoretically robust, there may be other external factors contributing to the change in trends in 2020. For example, we assumed the same annual seasonal dynamics, however the seasonal forces due to changes in climate and social drivers of infection may vary with year.
The strengths of our analysis are using more than one pre-pandemic year to assess longitudinal changes, especially important as 2019 saw unseasonal high influenza activity [12] which translated in higher ALRI admissions in 2019 compared to 2015 to 2018 (data not shown). To further tease out the impact of NPIs on respiratory viral transmission and resulting ALRI trends, we chose trauma admissions as a negative control which would not be impacted by altered viral respiratory transmission dynamics. These results showed little change in the admission trend, suggesting this was an adequate choice of a negative control. Rather than previous reports assessing admissions in the months immediately following NPI, we separately evaluated age groups for ALRI and captured the initial decline and resurgence in health service utilization, a further strength of our study.
In conclusion, our findings have highlighted the impact of NPI's on reducing the transmission of respiratory viruses in children, with the short-lived mandate of physical distancing, social distancing and school closures being enough to disrupt annual respiratory viral transmission dynamics with long-lasting effects. This sustained reduction was followed by a marked, resurgence in ALRI. As NPI measures continue to be used in Australia in 2021, the impact on future RSV and other respiratory infection-related morbidity and international trends in ALRI should be closely monitored.
Acknowledgments
The authors would like to thank the Business Intelligence Unit at Perth Children's Hospital for data extraction for this study. This study was supported by a Wesfarmers Centre for Vaccines and Infectious Diseases (WCVID) Clinician-Scientist Partnership Grant 2020. AOM is supported by a National Health and Medical Research Council (NHMRC) Postgraduate Scholarship (1191465), a WCVID Ad Hoc Postgraduate Top Up Scholarship and an Australian Government Research Training Program Fees Offset. CCB is supported by a NHMRC Investigator award (1173163).
Footnotes
Conflict of interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jclinepi.2021.11.021.
Appendix. Supplementary materials
References
- 1.Hogan AB, Anderssen RS, Davis S, Moore HC, Lim FJ, Fathima P, et al. Time series analysis of RSV and bronchiolitis seasonality in temperate and tropical Western Australia. Epidemics. 2016;16:49–55. doi: 10.1016/j.epidem.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Moore HC, Lim FJ, Fathima P, Barnes R, Smith DW, de Klerk N, et al. Assessing the burden of laboratory-confirmed respiratory syncytial virus infection in a population cohort of Australian children through record linkage. J Infect Dis. 2020;222:92–101. doi: 10.1093/infdis/jiaa058. [DOI] [PubMed] [Google Scholar]
- 3.Cowling BJ, Ali ST, Ng TW, Tsang TK, Li JC, Fong MW, et al. Impact assessment of non-pharmaceutical interventions against COVID-19 and influenza in Hong Kong: an observational study. The Lan. Pub. Health 5.5. 2020:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun J, Shi Z, Xu H. Non-pharmaceutical interventions used for COVID-19 had a major impact on reducing influenza in China in 2020. J Travel Med. 2020 doi: 10.1093/jtm/taaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr Infect Dis J. 2020;39:e423–e427. doi: 10.1097/INF.0000000000002845. [DOI] [PubMed] [Google Scholar]
- 6.Trenholme A, Webb R, Lawrence S, Arrol S, Taylor S, Ameratunga S, et al. COVID-19 and infant hospitalizations for seasonal respiratory virus infections, New Zealand, 2020. Emerg Infect Dis. 2021;27:641. doi: 10.3201/eid2702.204041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in Pediatric Emergency Department Utilization after Institution of COVID-19 Mandatory Social Distancing. J Pediatr. 2020:274–277. doi: 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Britton PN, Hu N, Saravanos G, Shrapnel J, Davis J, Snelling T, et al. COVID-19 public health measures and respiratory syncytial virus. The Lancet Child & Adolescent Health. 2020;4:e42–e43. doi: 10.1016/S2352-4642(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marriott D, Beresford R, Mirdad F, Stark D, Glanville A, Chapman S, et al. Concomitant marked decline in prevalence of SARS-CoV-2 and other respiratory viruses among symptomatic patients following public health interventions in Australia: data from St Vincent's Hospital and associated screening clinics, Sydney, NSW. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kadambari S, Abo Y-N, Phuong LK, Osowicki J, Bryant PA. Decrease in Infection-Related Hospital Admissions During COVID-19: Why Are Parents Avoiding the Doctor? Pediatr Infect Dis J. 2020;39:e385–e386. doi: 10.1097/INF.0000000000002870. [DOI] [PubMed] [Google Scholar]
- 11.Todd IM, Miller JE, Rowe SL, Burgner DP, Sullivan SG. Changes in infection-related hospitalizations in children following pandemic restrictions: an interrupted time-series analysis of total population data. Int J Epidemiol. 2021 doi: 10.1093/ije/dyab101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barr IG, Deng YM, Grau ML, Han AX, Gilmour R, Irwin M, et al. Intense interseasonal influenza outbreaks, Australia, 2018/19. Eurosurveillance. 2019;24 doi: 10.2807/1560-7917.ES.2019.24.33.1900421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Health Western Australia. Coronavirus COVID-19 in Western Australia 2021. 2021; Available at: https://experience.arcgis.com/experience/359bca83a1264e3fb8d3b6f0a028d768, Accessed 5 Sept 2020
- 14.Yeoh DK, Foley DA, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. Impact of Coronavirus Disease 2019 Public Health Measures on Detections of Influenza and Respiratory Syncytial Virus in Children During the 2020 Australian Winter. Clin Infect Dis. 2020;72:2199–2202. doi: 10.1093/cid/ciaa1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foley DA, Yeoh DK, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019–related public health measures. Clin Infect Di. 2021;73:e2829–e2830. doi: 10.1093/cid/ciaa1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Australian Bureau of Statistics. National, state and territory population 2021. 2021; Available at: https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release#data-download, Accessed 5 Sept 2020
- 17.Australian Bureau of Statistics. Estimated Residence Population by SA2, Age and Sex. 2021 [25 June 2021]; Available at: https://stat.data.abs.gov.au/, pp 1-8
- 18.Moore HC, De Klerk N, Richmond P, Lehmann D. A retrospective population-based cohort study identifying target areas for prevention of acute lower respiratory infections in children. BMC public health. 2010;10:1–9. doi: 10.1186/1471-2458-10-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim FJ, Blyth CC, Fathima P, de Klerk N, Moore HC. Record linkage study of the pathogen-specific burden of respiratory viruses in children. Influenza and other respiratory viruses. 2017;11:502–510. doi: 10.1111/irv.12508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Department of Premier and Cabinet Western Australia. COVID-19 coronavirus: WA roadmap. 2020 [2 September 2020]; Available at: https://www.wa.gov.au/organisation/department-of-the-premier-and-cabinet/covid-19-coronavirus-wa-roadmap.
- 21.Laschon E, Kaur H, O’Flaherty A. All WA school students ordered to redturn to school, marking end of coronavirus absences . Australian Broadcasting Corporation (ABC) News. 2020 https://www.abc.net.au/news/2020-05-14/all-wa-students-to-return-to-school-as-coronavirus-absences-end/12245712 [Google Scholar]
- 22.Department of Premier and Cabinet Western Australia. COVID-19 coronavirus: Travel advice. 2020 [5 September 2020]; Available at: https://www.wa.gov.au/organisation/department-of-the-premier-and-cabinet/covid-19-coronavirus-travel-advice.
- 23.Government of Western Australia. COVID-19 coronavirus: Controlled border WA roadmap 2020. 2020; Available at: https://www.wa.gov.au/government/publications/covid-19-coronavirus-controlled-border-wa-roadmap, Accessed 5 Sept 2020
- 24.Department of Premier and Cabinet Western Australia. COVID-19 coronavirus: Travel to WA 2020. 2020; Available at: https://www.wa.gov.au/organisation/department-of-the-premier-and-cabinet/covid-19-coronavirus-travel-advice, Accessed 5 Sept 2020
- 25.Angoulvant F, Ouldali N, Yang DD, Filser M, Gajdos V, Rybak A, et al. Coronavirus disease 2019 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections—a time series analysis. Clin Infect Dis. 2021;72:319–322. doi: 10.1093/cid/ciaa710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huh K, Kim Y-E, Ji W, Kim DW, Lee E-J, Kim J-H, et al. Decrease in hospital admissions for respiratory diseases during the COVID-19 pandemic: a nationwide claims study. Thorax. 2021;76:939–941. doi: 10.1136/thoraxjnl-2020-216526. [DOI] [PubMed] [Google Scholar]
- 27.Kishimoto K, Bun S, Shin J-h, Takada D, Morishita T, Kunisawa S, et al. Early impact of school closure and social distancing for COVID-19 on the number of inpatients with childhood non-COVID-19 acute infections in Japan. Eur J Pediatr. 2021:1–8. doi: 10.1007/s00431-021-04043-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carville KS, Lehmann D, Hall G, Moore H, Richmond P, De Klerk N, et al. Infection is the major component of the disease burden in aboriginal and non-aboriginal Australian children: a population-based study. Pediatr Infect Dis J. 2007;26:210–216. doi: 10.1097/01.inf.0000254148.09831.7f. [DOI] [PubMed] [Google Scholar]
- 29.Moore HC, de Klerk N, Richmond P, Lehmann D. A retrospective population-based cohort study identifying target areas for prevention of acute lower respiratory infections in children. BMC public health. 2010;10:757. doi: 10.1186/1471-2458-10-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foley DA, Phuong LK, Peplinski J, Lim SM, Lee WH, Farhat A, et al. Examining the interseasonal resurgence of respiratory syncytial virus in Western Australia. Arch Dis Child. 2021 doi: 10.1136/archdischild-2021-322507. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 31.Heymann A, Hoch I, Valinsky L, Kokia E, Steinberg D. School closure may be effective in reducing transmission of respiratory viruses in the community. Epidemiology & Infection. 2009;137:1369–1376. doi: 10.1017/S0950268809002556. [DOI] [PubMed] [Google Scholar]
- 32.Eden J-S, Sikazwe C, Xie R, Deng Y-M, Sullivan SG, Michie A, et al. Off-season RSV epidemics in Australia after easing of COVID-19 restrictions. medRxiv. 2021 doi: 10.1038/s41467-022-30485-3. 2021.2007.2021.21260810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ceranic I. Perth weather delivers city’s wettest November on record and its coolest in 12 years. ABC News. 2020 https://www.abc.net.au/news/2020-11-30/perth-endures-wettest-november-on-record-and-coolest-in-12-years/12935668 [Google Scholar]
- 34.Huang QS, Wood T, Jelley L, Jennings T, Jefferies S, Daniells K, et al. Impact of the COVID-19 nonpharmaceutical interventions on influenza and other respiratory viral infections in New Zealand. Nat Commun. 2021;12:1–7. doi: 10.1038/s41467-021-21157-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Casalegno J-S, Ploin D, Cantais A, Masson E, Bard E, Valette M, et al. Characteristics of the delayed respiratory syncytial virus epidemic, 2020/2021, Rhône Loire, France. Eurosurveillance. 2021;26 doi: 10.2807/1560-7917.ES.2021.26.29.2100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sullivan SG, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Eurosurveillance. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.47.2001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.