Abstract
Background
Home Based Cardiac Rehabilitation (HBCR) has been considered a reasonable alternative to Center-based Cardiac Rehabilitation (CBCR) in patients with established cardiovascular disease, especially in the midst of COVID-19 pandemic. However, the long-term cardiovascular outcomes of patients referred to HBCR remains unknown.
Objectives
To compare outcomes of patients who were referred and attended HBCR vs patients referred but did not attend HBCR (Non-HBCR).
Methods
We performed a retrospective study of 269 patients referred to HBCR at Providence Veterans Affairs Medical Center (PVAMC). From November 2017 to March 2020, 427 patients were eligible and referred for Cardiac Rehabilitation (CR) at PVAMC. Of total patients, 158 patients were referred to CBCR and 269 patients to HBCR based on patient and/or clinician preference. The analysis of outcomes was focused on HBCR patients. We compared outcomes of patients who were referred and attended HBCR vs patients referred but did not attend HBCR (Non-HBCR) from 3 to 12 months of the referral date. HBCR consisted of face-to-face entry exam with exercise prescription, weekly phone calls for education and exercise monitoring, with adjustments where applicable, for 12-weeks and an exit exam. Primary outcome was composite of all-cause mortality and hospitalizations. Secondary outcomes were all-cause hospitalization, all-cause mortality and cardiovascular hospitalizations, separately. We used cox proportional methods to calculate hazard ratios (HR) and 95% CI. We adjusted for imbalanced characteristics at baseline: smoking, left ventricular ejection fraction and CABG status.
Results
A total of 269 patients (mean age: 72, 98% Male) were referred to HBCR, however, only 157 (58%) patients attended HBCR. The primary outcome occurred in 30 patients (19.1%) in the HBCR group and 30 patients (30%) in the Non-HBCR group (adjusted HR=0.56, CI 0.33-0.95, P=.03). All-cause mortality occurred in 6.4% of patients in the HBCR group and 13% patients in the Non-HBCR group 3 to 12 months after HBCR referral (adjusted HR=0.43, CI 0.18-1.0, P= .05). There was no difference in cardiovascular hospitalizations (HBCR: 5.7% vs Non-HBCR: 10%, adjusted HR 0.57, CI 0.22-1.4, P= .23) or all cause hospitalizations at 3 to 12 months between the groups (HBCR: 12.7% vs Non-HBCR: 21%, adjusted HR 0.53, CI 0.28-1.01, P= .05).
Conclusion
Completion of HBCR among referred patients was associated with a lower risk of the combined all-cause mortality and all-cause hospitalizations up to 12 months. Based on the outcomes, HBCR is a reasonable option that can improve access to CR for patients who are not candidates of or cannot attend CBCR. Randomized-controlled studies are needed to confirm these findings.
Keywords: Home based cardiac rehabilitation Cardiovascular hospitalizations, All cause hospitalizations, All cause deaths, Mortality, Cardiovascular diseases
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity worldwide. In the USA, CVD has an incidence of > 650000 every year and is the most common diagnosis for inpatient admission in patients aged > 65 years. CVD causes a huge burden on economy as it costs > $200 billions annually.1 Cardiac rehabilitation (CR) is standard of care for patients with cardiovascular disease and part of the standard treatment for CVD.2 CR has been shown to reduce all-cause and cardiovascular mortality, all-cause and HF hospitalizations, improved functional status and quality of life in patients with CVD.3., 4., 5. Despite its known benefits, CR is not available and accessible to all patients with CVD.
Home based cardiac rehabilitation (HBCR) has been offered as an alternative to center-based CR (CBCR) for patients who need CR but cannot attend for multiple reasons.6 HBCR consists of same core components of CBCR but with remote delivery. Previous literature has shown that compared to CBCR, HBCR was as effective in improving functional status and quality of life in eligible patients following a cardiac event.7., 8., 9., 10., 11., 12. In a recent multi-center retrospective study at Veterans Affairs (VA), patients were more likely to participate in CR when HBCR was available at the institution.13 Therefore, HBCR can be a resource for women and other patients with transport issues to provide a potentially effective therapy. Despite its increased use during the COVID-19 pandemic, the long-term cardiovascular outcomes including deaths and hospitalizations in patients who were referred for HBCR are unknown. Therefore, the aim for our study is to compare the outcomes of patients who were referred and attended HBCR vs patients referred but did not attend HBCR (Non-HBCR).
Methods
We performed a retrospective study of 269 patients referred to HBCR at Providence Veterans Affairs Medical Center (PVAMC). From November 2017 to March 2020, 427 patients were eligible and referred for Cardiac Rehabilitation (CR) at PVAMC. Although HBCR is available at PVAMC, the hospital does not have an on-site CR program, for which CBCR were referred out to the community CR programs paid for by the PVAMC. Of total patients referred to CR, 158 patients were referred to CBCR in the community and 269 patients to HBCR based on patient and clinician shared decision making. The analysis of outcomes was focused on HBCR patients. Patients who were referred for CBCR were excluded from this analysis because these patients received care from multiple CBCR facilities outside the VA hospital, and details of their outcomes with timelines were not available to the study team. This is a cohort study where patients who were referred and attended HBCR were compared against those patients who were referred but did not attend HBCR (Non-HBCR) to ensure that all patients in this study met initial eligibility criteria for HBCR. The study protocol was approved by the Internal Review Board at PVAMC. The HBCR program at PVAMC is supported by the VA Office of Rural Health HBCR Program,14 with the goal of expanding CR access to Veterans with eligible CR diagnoses. Medical records were reviewed from consecutive patients enrolled in the HBCR program at PVAMC, Rhode Island, from November 2017 to March 2020. Patients were referred to HBCR for eligible diagnoses such as recent myocardial infarction, percutaneous coronary intervention, Coronary Artery Bypass Graft (CABG), angina, Heart Failure (HF), heart transplantation or after heart valve procedure, as per American heart association/ American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) guidelines.15 , 16
Study Outcomes
Study outcomes were ascertained by chart review and data was complete on 100% of the Veterans using VA's cross-linked electronic medical records nation-wide for VA-hospitalizations and mortality. The data has a high reliability on death status given the burial claims submitted on behalf of the Veteran and the linkage of the records to the National death index. Weekly phone calls about weekly exercise and health status changes including hospitalizations were documented in the electronic medical records by the HBCR staff per HBCR protocol, which was captured through chart review. The primary outcome was a composite of all-cause mortality and hospitalizations from 3 months to 12 months after referral. The first 3-month blanking period after referral was established to minimize selection bias to ensure that patients from either group did not incur hospitalizations or death that would have precluded them from HBCR participation. The outcomes of first 3-months were reported separately in supplementary material. Secondary outcomes were all-cause hospitalization, all-cause mortality and cardiovascular hospitalizations, each separately, from 3 to 12 months of referral for HBCR.
Study Covariates
Hypertension, coronary artery disease, diabetes mellitus, hyperlipidemia, stroke and atrial fibrillation were recorded at the time of entry to CR. Smoking was self-reported and details were collected about current smoking habits as number of cigarettes per day and if patient has quit smoking or ever smoked in the past. Prescribed medications were reviewed and confirmed with the patient upon entry to CR. Patients were stratified into low, intermediate or high-risk categories based on AACVPR risk category.6 Left ventricular ejection fraction (LVEF) data was extracted from review of echocardiogram, left-ventricular angiogram, nuclear perfusion scan, cardiac CT scan or MRI, previous to CR enrollment.
Functional capacity was measured using the 6-minute walk test (6MWT) and the Duke Activity Status Index (DASI):
6. Minutes Walking Test (6MWT)
The 6MWT test is a commonly used test to estimate functional exercise capacity in patients, where a patient walked unassisted in a marked track for 6 minutes and the distance recorded.17
Duke Activity Status Index (DASI)
Duke Activity Status Index is a validated self-administered twelve item questionnaire that measures a patient's functional capacity. It is used to obtain an estimate of a patient's peak oxygen uptake.18
Depression symptoms were measured using the Patient Health Questionnaire (PHQ-9):
Patient Health Questionnaire (PHQ-9)
It is a well-validated nine-item questionnaire to assess depression symptoms. Score ranges from 0-27 where higher score is associated with more depression symptoms.19
Home-Based Cardiac Rehabilitation at Providence VAMC
Patients were required to attend an in-person examination session at entry and after completing 12 weeks of HBCR. After the entry visit where exercise prescription was provided, the expectation was that the patients perform daily exercises, whenever possible and as tolerated, for the 12 weeks of HBCR duration. Patients were provided with and educated about the use of, a portable peddler, a pedometer and elastic bands for resistance exercise. Achievable individualized goals on exercise and behavioral modification (diet, smoking and medication adherence) were set with the patient. Leg exercises (e.g., goal to start with 750 non-uphill walking steps per occasion for 5 minutes twice a day) were usually started prior to progression to arm exercises. Band exercises included arm curl/biceps curl, side raise, front raise (shoulder flexion), chest press and shoulder abduction (arms straight in front and pull apart without bending the elbows). For band exercises, a common prescription was 5 repetitions of each exercise 2 times per day, divided throughout the day. Patients were asked to check their weight in the morning, blood pressure and pulse two hours after taking their morning medications and to document them in a logbook. A weekly call from HBCR staff (e.g., nurse) were made at a mutually agreeable time to inquire about the progress. Patients also received education and counselling about nutrition, stress reduction, and other topics of secondary prevention of 20-minute duration during the phone calls. An exit exam was conducted at 12 weeks upon completion of the HBCR program with maintenance behavioral and exercise prescriptions to continue to perform at home or in the community. Patients were asked to complete a 6-minute walk test and three questionnaires at entry and exit of the HBCR program.
Statistical Analysis
Values were presented as mean ± standard deviation, frequencies and percentage. T-test was used to compare continuous variables between groups. For the main analysis, subjects were grouped into HBCR and Non-HBCR and their baseline characteristics compared. Cox proportional hazards modeling was used to compare the primary and secondary outcomes of patients who attended HBCR versus those who did not, adjusting for imbalanced baseline characteristics (smoking, LVEF and CABG). Time zero was set at 3 months from the referral date and outcomes compared up to 12 months from the referral date. A separate sensitivity analysis was conducted to compare the outcomes of the patients with time zero set at the date of referral (no three-month blanking period), up to 12 months after referral.
In a subgroup analysis for patients who attended HBCR, the CR outcomes of 6MWT, DASI and PHQ-9; as well as weight, blood pressure, lipid panel and hemoglobin A1c (for patients with diabetes) were compared, before and after HBCR. There were very few data points missing (less than 5% of patients had incomplete data) mostly affecting laboratory values (hemoglobin A1c), for which the missing observations were not counted for the estimate of the index laboratory variable. A retrospective power size calculation to detect statistical difference among the two groups were undertaken and 68 patients in each group (with 80% power and 5% alpha) were needed. A 2-sided level of significance of P < 0.05 was used for statistical significance. Statistical analyses were carried out using Stata statistical package (Stata 15.1).
Results
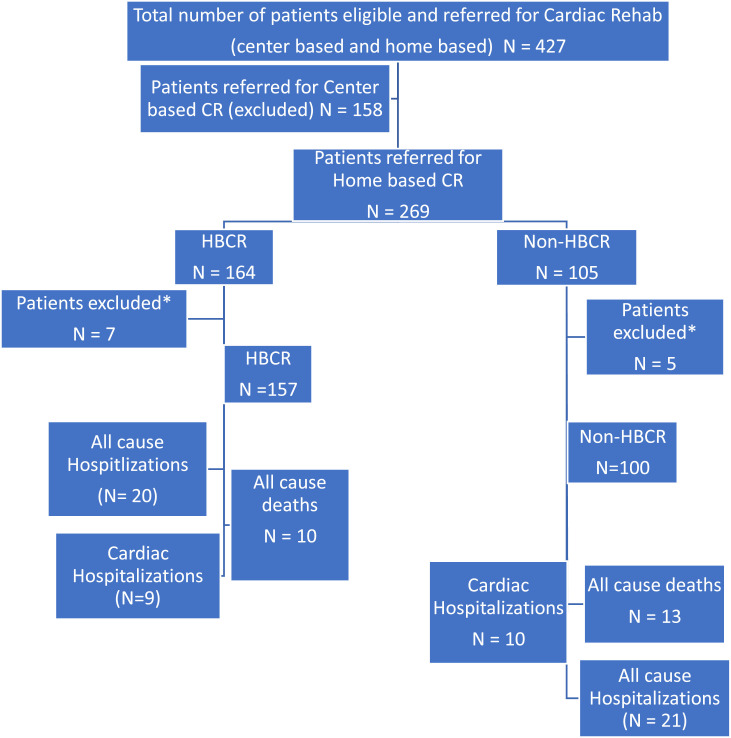
A total of 269 patients were referred to HBCR. Twelve patients were excluded from the main analysis as they experienced a primary or secondary outcome in less than 90 days since referral (figure 1 ). The mean age of the patients was 72 years, 98% were male and 93% were white. Out of total patients referred for HBCR, 157 (58%) patients attended HBCR. Patients in HBCR group were less likely to be smokers (HBCR: 13% vs Non-HBCR: 28%, P< .01) and less likely to have undergone CABG (HBCR: 17% vs Non-HBCR: 27%, P= .04) than patients in the Non-HBCR group. Baseline comorbidities and AACVPR risk were similar between both groups with the exception of LVEF. Patients who attended HBCR group had a higher LVEF than patients in the Non-HBCR group (51 ± 15% vs 47 ± 14%, P= .02), Table 1 .
Figure 1.
Flow diagram of patient enrollment
* Patients excluded with outcomes less then 90 days of enrollment, Abbreviations: CR, cardiac rehabilitation; HBCR, Patients completed home based cardiac rehabilitation; Non-HBCR, Patients who were referred but not completed home based cardiac rehabilitation
Table 1.
Clinical and demographic characteristics (N=257)
| Patients Enrolled in Home Based Cardiac Rehab (N=157) | Patients Not Enrolled in Home Based Cardiac Rehab (N=100) | P Value* | |
|---|---|---|---|
| Age, years | 73 ± 9 | 70 ± 11 | 0.06 |
| Male | 153 (98) | 99 (99) | 0.38 |
| Ethnicity, White | 144 (92) | 94 (94) | 0.50 |
| BMI, kg/m2 | 33 ± 8 | 32 ± 8 | 0.46 |
| SBP, mmHg | 126 ± 17 | 128 ± 18 | 0.33 |
| AACVPR Risk Category High Intermediate Low |
29 (19) 112 (71) 16 (10) |
23 (23) 62 (62) 13 (13) |
0.40 |
| Risk Factors Hypertension Diabetes Mellitus Current smoker Hyperlipidemia Stroke Atrial Fibrillation |
141 (90) 75 (48) 20 (13) 134 (85) 12 (8) 66 (42) |
87 (87) 47 (47) 28 (28) 86 (86) 10 (10) 45 (45) |
0.49 0.90 <0.01 0.88 0.51 0.64 |
| Enrollment Diagnosis STEMI/NSTEMI PCI CABG CHF Valve disease CAD PAD |
36 (23) 27 (17) 26 (17) 105 (67) 16 (10) 85 (54) 11 (7) |
27 (27) 26 (26) 27 (27) 72 (72) 8 (8) 59 (59) 7 (7) |
0.46 0.09 0.04 0.39 0.56 0.44 1.0 |
| LVEF | 51 ± 15 | 47 ± 14 | 0.02 |
| Glycated Hemoglobin A1C | 6.5 ± 1.9 | 7 ± 2 | 0.06 |
| Total Cholesterol, mg/dl | 147 ± 43 | 152 ± 49 | 0.34 |
| Triglycerides, mg/dl | 141 ± 105 | 140 ± 82 | 0.92 |
| Statin use | 86 (55) | 66 (66) | 0.07 |
Abbreviations: BMI; body mass index; SBP, systolic blood pressure; AACVPR, Association of Cardiovascular and Pulmonary Rehabilitation risk category; STEMI, ST elevation myocardial infraction; NSTEMI, Non-ST elevation myocardial infarction; PCI, Percutaneous Coronary Intervention; CABG, Coronary Artery Bypass Graft; CHF, Congestive Heart Failure; CAD, Coronary Artery Disease; PAD, Peripheral Arterial Disease; LVEF, left ventricular ejection fraction
*P value comparing two groups
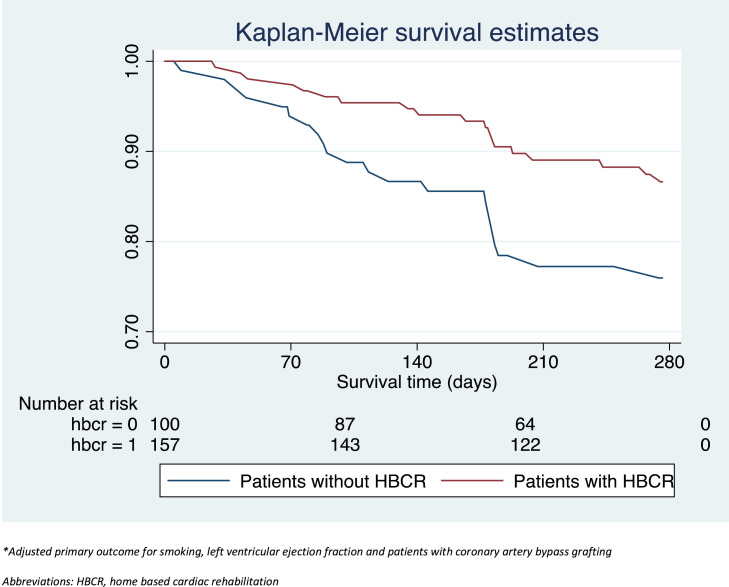
Primary outcome occurred in 30 patients (19.1%) in the HBCR group and 30 patients (30%) in the Non-HBCR group from 3 to 12 months after HBCR referral (adjusted HR=0.56, CI 0.33-0.95, P= .03), Figure 2 . All-cause mortality occurred in 6.4% of patients in the HBCR group and 13% patients in the Non-HBCR group, 3 to 12 months after HBCR referral (adjusted HR=0.43, CI 0.18-1.0, P= .05). There was no significant difference in cardiovascular hospitalizations (HBCR: 5.7% vs Non-HBCR: 10%, adjusted HR 0.57, CI 0.22-1.4, P= .23) or all cause hospitalizations at 3 to 12 months between the groups (HBCR: 12.7% vs Non-HBCR: 21%, adjusted HR 0.53, CI 0.28-1.01, P= .05), Table 2 . Sensitivity analyses that included outcomes from date of referral to 12 months showed a similar trend of results, Supplemental Table and Figure.
Figure 2.
Survival curve for patients who have completed HBCR vs patients not completed HBCR*
*Adjusted primary outcome for smoking, left ventricular ejection fraction and patients with coronary artery bypass grafting, Abbreviations: HBCR, home based cardiac rehabilitation
Table 2.
Morbidity and Mortality of patients in Home Based Cardiac Rehabilitationa (N=257)
| Patients Enrolled in Home Based Cardiac Rehab (N=157) | Patients Not Enrolled in Home Based Cardiac Rehab (N=100) | Unadjusted Hazard Ratio(95% CI) | P Value* | Adjusted Hazard Ratio (95% CI) | P Value* | |
|---|---|---|---|---|---|---|
| Primary outcome⁎⁎ | 30 (19.1) | 30 (30) | 0.57 (0.35-0.95) | 0.03 | 0.56 (0.33-0.95) | 0.03 |
| All cause deaths | 10 (6.4) | 13 (13) | 0.50 (0.20-1.03) | 0.06 | 0.43 (0.18-1.00) | 0.05 |
| All cause hospitalizations | 20 (12.7) | 21 (21) | 0.54 (0.29-1.00) | 0.05 | 0.53 (0.28-1.01) | 0.05 |
| CV hospitalizations | 9 (5.7) | 10 (10) | 0.51 (0.21-1.26) | 0.15 | 0.57 (0.22-1.40) | 0.23 |
*P value comparing two groups
** Combined outcome (all cause death and hospitalizations)
All outcomes from 3-12 months of referral
In the subgroup analyses of patients who participated in HBCR (N=157), 138 (87.9%) patients completed HBCR and the average duration of enrollment was 11.1 weeks. Improvements in blood pressure, total cholesterol and PHQ-9 scores were observed after HCBR when compared to baseline, Table 3 .
Table 3.
Pre HBCR and Post HBCR values in patients completed Rehab (N=157)
| Pre-HBCR (95% CI) | Post HBCR (95% CI) | Difference (95% CI) | P Value* | |
|---|---|---|---|---|
| Weight, Ibs | 220 (211, 229) | 219 (210, 227) | -1 (-5, 3) | 0.53 |
| SBP, mmHg | 126 (123, 129) | 117 (112, 122) | -8 (-14, -3) | <0.01 |
| DBP, mmHg | 71 (69, 73) | 67 (64, 70) | -4 (-8, -1) | <0.01 |
| Cholesterol, mg/dl | 145 (139, 151) | 132 (124, 140) | -13 (-20, -6) | <0.01 |
| LDL, mg/dl | 79 (73, 84) | 76 (62, 89) | -3 (-15, 9) | 0.61 |
| HDL, mg/dl | 42 (39, 44) | 39 (36, 41) | -3 (-5, -1) | 0.02 |
| Triglycerides, mg/dl | 134 (120, 148) | 123 (110, 136) | -11 (-23, 2) | 0.10 |
| HbA1C | 6.5 (6.2-6.8) | 6.2 (5.8, 6.5) | 0 (-1, 0) | 0.05 |
| Duke score | 20 (18, 23) | 21 (19, 24) | 1 (-1, 3) | 0.38 |
| 6MWT, ft | 249 (226, 271) | 258 (230, 286) | 9 (-14, 32) | 0.44 |
| PHQ-9 | 6 (5, 7) | 5 (4, 6) | -2 (-3, -1) | <0.01 |
Abbreviations: HBCR, Home base cardiac rehabilitation; SBP, Systolic blood pressure; DBP, Diastolic blood pressure; LDL, Low density lipoprotein; HDL, High density lipoprotein; HBA1C, Hemoglobin A1C; 6MWT, 6 Minutes walking test; PHQ-9, Patient health questionnaire
*P value comparing groups Pre and Post HBCR
Discussion
The study findings showed that amongst patients who were referred to HBCR at PVAMC, attendance of HBCR was associated with a lower composite risk of all-cause mortality and hospitalizations at 12 months when compared to patients who did not attend HBCR. Amongst HBCR participants, improvements were seen in blood pressure, lipids and depression scores compared to baseline, and can be potential mechanisms that explained the observed favorable outcomes in regard to combined all-cause mortality and hospitalizations.
HBCR has been shown to be as effective as center-based CR by previous meta-analysis results in terms of mortality, exercise capacity and health related quality of life7. The same meta-analysis did not show differences in mortality or morbidity in HBCR vs. center-based CR.7 The findings of the current study showed that patients who attended HBCR have a better composite outcome of combined all-cause mortality and hospitalizations than patients who did not attend HBCR. Although findings of the current study did not directly compare CBCR and HBCR, similar improvements in clinical outcomes were previously shown after CBCR and HBCR by Anderson et al7. Indeed, there is paucity of randomized-controlled studies that compared long-term outcomes of HBCR versus usual care. A recent study of home-based mobile guided CR compared to non-participation in CR among elderly patients in Europe, showed improvement in fitness, but no difference in 1-year cardiac events.20 The HBCR program at VA hospitals improved access to and participation in CR for Veterans,13 since CBCR is not available in many VA hospitals. Yet, evidence of long-term adverse outcome reductions associated with the program was still lacking. Our study built upon previous studies to show that HBCR, provided as part of the VA nationwide HBCR program, was associated with improved cardiac outcomes compared to usual care. Potential mechanisms include the effectiveness of the program in improving functional capacity, quality of life, and psychological symptoms, shown in patients who attended the HBCR program, similar to short-term results from previous studies.8 , 21., 22., 23. Recently, Aronov et al. (2019) showed that CR (both HBCR and CBCR) can help in reducing total cholesterol values in patients with CVD which can further improve quality of life and reduce cardiovascular complications.23
Given the location and schedule flexibility offered by the delivery of HBCR, HBCR has the potential to increase the overall access to CR for all eligible patients who are facing these obstacles of participation. As such, it should be considered as means to achieve the goals of the Million Hearts® 2022 program, which is a national initiative led by the Centers for Disease Control and Prevention (CDC) to increase CR participation to prevent 1 million heart attacks and strokes within 5 years24. As CR is an underutilized component,25 due to multiple obstacles such as transportation, schedule26 and other factors, HBCR can be a viable alternative. As shown by Schopfer et al,13 the presence of HBCR in an institution increased patient participation in CR. In addition, HBCR can be an ideal tool in the era of COVID19 pandemic where in-person CR programs had to be limited due to social distancing.
Limitations
This is a single center study. The majority of patients in our study were male and white, making it less applicable to women and those of other ethnicities. Although women participation has been consistently low27 in CR programs across the country, it is especially so in the current study of Veterans, where women represent less than 10% of the current Veteran population, for which the generalizability to women with CR needs is limited. The current study results should be interpreted with caution and only applicable to the subset of patients who attended HBCR and who were not referred to CBCR based on the decision of the patient in conjunction to the referring physician. The study design was observational and non-randomized for which the possibility of residual confounding cannot be excluded despite our efforts using strict inclusion criteria, multi-variate adjustment and sensitivity analyses. It is possible that the observed difference was a result of healthier patients more willing to attend HBCR compared to those who did not.28 , 29 However, the adjusted results as well as the 3-month post-referral blanking period including the sensitivity analyses (without 3-month blanking period) showed consistent results. It is also possible that the non-VA hospitalizations were incompletely captured but this problem would affect both groups and underestimate the true difference in study outcomes. In addition, the improvements seen in blood pressure, cholesterol and depression scores in HBCR patients could also have been achieved by patients who did not attend HBCR; however, this information was incomplete or not available for non-HBCR patients and should be better addressed in future randomized-controlled trials. The current study participants did not show improvements in exercise capacity after completion of HBCR and the reason that their functional capacity did not significantly increase could be due to more adherence to some elements and less to others such as the exercise, given the lack of on-site supervision. Given that significant findings for the primary outcome, the remaining non-exercise components such as lifestyle counselling and support, and health monitoring provided as part of the HBCR, were likely meaningful. Despite the above weaknesses, this study is helpful in providing the first effect size estimates for the design of future randomized-controlled trials.
Conclusions
Completion of HBCR among referred patients was associated with a lower risk of combined all-cause mortality and all-cause hospitalizations up to 12 months. Based on the outcomes, HBCR is a reasonable option that can improve access to CR for patients who are not candidates of or cannot attend CBCR. Randomized-controlled studies are needed to confirm these findings.
Acknowledging ORH HBCR Program
This material is based upon the work of the Department of Veteran Affairs, Veterans Health Administration Office of Rural Health, Veterans Rural Health Resource Center-Iowa City Home-based Pulmonary Rehabilitation Program.
Standard federal government disclaimers and copyright procedures
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Declaration of Competing Interest
None.
Acknowledgements
This material is based upon work supported by the Department of Veteran Affairs, Veterans Health Administration Office of Rural Health, Veterans Rural Health Resource Center- Iowa City.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.hrtlng.2021.11.005.
Appendix. Supplementary materials
References
- 1.Donna K Arnett R.S.B., Albert Michelle A., et al. 19 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:563–595. doi: 10.1161/CIR.0000000000000677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MA W. AACVPR Guidelines for cardiac rehabilitation programs & secondary prevention programs. 2004 [Google Scholar]
- 3.Long L, Bridges C MI, et al. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst Rev. Cochrane Database Syst Rev. 2019. Jan 29;1(1) doi: 10.1002/14651858.CD003331.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson L, ON Thompson DR, et al. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. JACC. 2016;67(1):1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 5.Taylor RS, WS Smart NA, et al. Impact of Exercise Rehabilitation on Exercise Capacity and Quality-of-Life in Heart Failure: Individual Participant Meta-Analysis. JACC. 2019. April,;73:1430–1443. doi: 10.1016/j.jacc.2018.12.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balady GJ, WM Ades PA, Bittner V, Comoss P, Foody JM, Franklin B, Sanderson B, Southard D. American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Nursing; American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Nutrition, Physical Activity, and Metabolism; American Association of Cardiovascular and Pulmonary Rehabilitation. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007. May;22(115 (20)):2675–2682. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 7.Anderson L, SG Norton RJ. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017. Jun(6) doi: 10.1002/14651858.CD007130.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen YW, WC Lai YH, et al. Home-based cardiac rehabilitation improves quality of life, aerobic capacity, and readmission rates in patients with chronic heart failure. Medicine (Baltimore) 2018. Jan(4):e9629. doi: 10.1097/MD.0000000000009629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kraal JJ, Abu-Hanna A VdA-VMM, Stut W, Peek N, Kemps HM. Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: Results of the FIT@Home study. Eur J Prev Cardiol. 2017. Aug(12):1260–1273. doi: 10.1177/2047487317710803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang R, Morris NR BJ, Mandrusiak A, Russell T. Home-based telerehabilitation is not inferior to a centre-based program in patients with chronic heart failure: a randomised trial. J Physiother. 2017. April(63):101–107. doi: 10.1016/j.jphys.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 11.Avila A, Goetschalckx K CJ, et al. Home-Based Rehabilitation With Telemonitoring Guidance for Patients With Coronary Artery Disease (Short-Term Results of the TRiCH Study): Randomized Controlled Trial. J Med Internet Res. 2018. June(22):e225. doi: 10.2196/jmir.9943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas RJ, Beckie TM BA, et al. Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Am Coll Cardiol. 2019;74(1):133–153. doi: 10.1016/j.jacc.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schopfer DW, KN Shen H, Duvernoy CS, Forman DE, Whooley MA. Association of Veterans Health Administration Home-Based Programs With Access to and Participation in Cardiac Rehabilitation. JAMA Intern Med. 2018;178(5):715–717. doi: 10.1001/jamainternmed.2017.8039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wakefield BJ, DK Paez M, Grover S, Franciscus C, Reisinger HS, Kaboli PJ, El Accaoui R. Creating and disseminating a home-based cardiac rehabilitation program: experience from the Veterans Health Administration. BMC Cardiovasc Disord. 2019. november(6):242. doi: 10.1186/s12872-019-1224-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balady GJ, AP Bittner VA, et al. American Heart Association Science Advisory and Coordinating Committee. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011. Dec;124(25):2560–2591. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 16.Thomas RJ, Lui K KM, Oldridge N, Piña IL, J Spertus. ACCFAHA Task Force on Performance Measures. AACVPR/ACCF/AHA 2010 Update: Performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: A report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation) J Cardiopulm Rehabil Prev. 2010. Sep-Oct;30(5):279–288. doi: 10.1097/HCR.0b013e3181f5e36f. [DOI] [PubMed] [Google Scholar]
- 17.Troosters T, GR Decramer M. Six minute walking distance in healthy elderly subjects. Eur Respir J. 1999. Aug;14(2):270–274. doi: 10.1034/j.1399-3003.1999.14b06.x. [DOI] [PubMed] [Google Scholar]
- 18.Hlatky MA, Higginbotham MB BR, Lee KL, Mark DB, Califf RM, Cobb FR, Pryor DB. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989. Sep;15(64 (10)):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 19.Milette K, HM Baron M, BD Thombs. Canadian Scleroderma Research Group. Comparison of the PHQ-9 and CES-D depression scales in systemic sclerosis: internal consistency reliability, convergent validity and clinical correlates. Rheumatology (Oxford) 2010. April;49(4):789–796. doi: 10.1093/rheumatology/kep443. [DOI] [PubMed] [Google Scholar]
- 20.Snoek JA, PE van der Velde AE, et al. Effectiveness of Home-Based Mobile Guided Cardiac Rehabilitation as Alternative Strategy for Nonparticipation in Clinic-Based Cardiac Rehabilitation Among Elderly Patients in Europe: A Randomized Clinical Trial. JAMA Cardiol. 2021. Apr;6(4):463–468. doi: 10.1001/jamacardio.2020.5218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aamot IL, FS Gustad K, et al. Home-based versus hospital-based high-intensity interval training in cardiac rehabilitation: a randomized study. Eur J Prev Cardiol. 2014. Sep;21(9):1070–1078. doi: 10.1177/2047487313488299. [DOI] [PubMed] [Google Scholar]
- 22.Drwal KR, WB Forman DE, Wu WC, Haraldsson B, El Accaoui RN. Home-Based Cardiac Rehabilitation: EXPERIENCE FROM THE VETERANS AFFAIRS. Cardiopulm Rehabil Prev. 2021;41(2):93–99. doi: 10.1097/HCR.0000000000000594. [DOI] [PubMed] [Google Scholar]
- 23.Aronov D, BM Iosseliani D, Orekhov A. Clinical Efficacy of а Medical Centre- and Home-based Cardiac Rehabilitation Program for Patients with Coronary Heart Disease After Coronary Bypass Graft Surgery. Arch Med Res. 2019. April;50(3):122–132. doi: 10.1016/j.arcmed.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Wright JS, WH Ritchey MD. Million Hearts 2022: Small Steps Are Needed for Cardiovascular Disease Prevention. JAMA. 2018;320(18):1857–1858. doi: 10.1001/jama.2018.13326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.JS A. Cardiac Rehabilitation: An Underutilized Class I Treatment for Cardiovascular Disease. Am J Med. 2020;133(9):1005–1006. doi: 10.1016/j.amjmed.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 26.Thomas RJ, BA Beckie TM, et al. Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation. 2019. July;140(1):69–89. doi: 10.1161/CIR.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 27.Galati A, PM Tourkmani N, et al. Working Group on Cardiac Rehabilitation of the Italian Society of Cardiology. Cardiac rehabilitation in women: state of the art and strategies to overcome the current barriers. J Cardiovasc Med (Hagerstown) 2018. Dec;19(12):689–697. doi: 10.2459/JCM.0000000000000730. [DOI] [PubMed] [Google Scholar]
- 28.Carlsson AC, WP Gigante B, Leander K, Hellenius ML, de Faire U. Seven modifiable lifestyle factors predict reduced risk for ischemic cardiovascular disease and all-cause mortality regardless of body mass index: a cohort study. Int J Cardiol. 2013. Sep;30(168 (2)):946–952. doi: 10.1016/j.ijcard.2012.10.045. [DOI] [PubMed] [Google Scholar]
- 29.Tsai MC, LC Liu SC, Tseng PJ, Chien KL. Combined healthy lifestyle factors are more beneficial in reducing cardiovascular disease in younger adults: a meta-analysis of prospective cohort studies. Sci Rep. 2020. Oct;10(1) doi: 10.1038/s41598-020-75314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.