Abstract
Although several non-thermal plasmas (NTPs) technologies have been widely investigated in air treatment, very few studies have focused on the inactivation mechanism of viruses by NTPs. Due to its efficiency and environmental compatibility, non-thermal plasma could be considered a promising virus-inactivation technology. Plasma is a partly or fully ionized gas including some species (i.e., electrons, free radicals, ions, and neutral molecules) to oxidize pollutants or inactivate harmful organisms. Non-thermal plasmas are made using less energy and have an active electron at a much higher temperature than bulk gas molecules. This review describes NTPs for virus inactivation in indoor air. The different application processes of plasma for microorganism inactivation at both laboratory and pilot-scale was also reviewed This paper reports on recent advances in this exciting area of viral inactivation identifying applications and mechanisms of inactivation, and summarizing the results of the latest experiments in the literature. Moreover, special attention was paid to the mechanism of virus inactivation. Finally, the paper suggests research directions in the field of airborne virus inactivation using non-thermal plasma.
Keywords: Non-thermal plasma, Virus inactivation, Indoor air, Best-advanced oxidation
Introduction
Viruses are part of the life history on our planet and the most abundant and diverse microbes. These species dwelled in the World for billions of years and infected all cell-based life forms organisms, i.e., from bacteria to humans, animals, and plants (Couch, 1981). Consequently, they are responsible for numerous hospitalizations, animal diseases, deaths, and crop losses, leading to immense social, economic, and biological pressures (Filipić et al. 2020a). They have adapted to various climates and are now found in all environmental compartments, such as the air, where the risk of infectious respiratory diseases is higher than any other sources (Tregoning and Schwarze, 2010). A viral respiratory infection could be exposed to bacterial disease, thus duplicating the risk of death (Hament et al. 1999). Despite considerable public health efforts, epidemics of viral respiratory infections are still common (widespread) in healthy humans and can lead to the death of vulnerable people (Moriyama et al. 2020). In 2017 alone, the Global Burden of Disease study found that air pollution is a fatal source of nearly 5 million premature deaths (Xiao et al. 2020). Also, another study via the World Bank in 2007 found that air infection diseases kill 750,000 people annually in China (Chang, 2012).
Typically, viruses exist in the air at specific concentrations, which are not generally sufficient to cause disease in humans because the immune system of healthy humans prevents infections. However, the risk of human contamination rises significantly at higher infectious virus concentrations (Nikitin et al. 2014). Numerous epidemiological studies demonstrated that air transmissions via aerosols, large droplets, or direct contact with secretions lead to a substantial increase in human morbidity and mortality, making air the most significant vector of viral infection (Couch 1981; Martínez-Montelongo et al. 2020. Pollution of indoor and outdoor air has been identified as responsible for significant deleterious effects on human health and social and economic growth (Martínez-Montelongo et al. 2020). However, indoor air pollution is the primary concern as it is 2–5 times more polluted than outside air pollution; in extreme cases, it can be over 100 times higher (Fang et al. 2016). Also, indoor environments often harbor potentially unsafe microorganisms (La Giuseppina et al. 2013).
Pandemics such as the COVID-19 established the necessity for indoor air cleaning and air purification techniques (Kim and Jang 2018) and replacing, completing, or updating existing conventional viral inactivation methods (Li et al. 2020). Most decontamination processes commonly used for viral inactivation like photocatalysis (TiO2 + UVA) and filtration do not have an effective disinfection ability against viruses and have substantial inconveniences (Zhang and Gamage, 2010). Indeed, the most applied technologies to control and remove airborne pathogens are the collection of bioaerosols on filters, such as porcine reproductive and respiratory syndrome (PRRS), high-efficiency particulate arrestance (HEPA), minimum efficiency reporting value (MERV) 14 and MERV 16 filters, UV germicidal irradiation (UVGI), atmospheric pressure non-thermal plasmas (APNTP), and cold atmospheric pressure plasma (CAPP). HEPA filtration has been experienced to be very effective in removing bioaerosols from airstreams. In contrast, MERV filters were exhibited to be the safer choice for both roof bolter and face drill.
Indeed, Farnsworth et al. showed the highest efficiency (i.e., 96.5 ± 1.5%) of the bacterial collection of Baccilus subtilis by HEPA filtration. Alonso et al. reassessed the impact of air filtration from commercial sow farms on the incidence of PRRSV introductions. They found that air filtration resulted in a reduction of approximately 80% of the risk with introducing the new PRRSv, thus highlighting the role of PRRSv in aerosol filtration of the air. Otherwise, using HEPA filters denotes several disadvantages, such as high filter replacement costs, and high-pressure drops and increased energy consumption to maintain the desired ventilation rate (Amissah (2005), Tellier (2006), Tellier (2009)).
Likewise, HEPA filters do not deactivate pathogens, hence the possibility of re-emitting more resilient pathogens into the ambient air during the filter replacement and disposal processes. Effective UVGI disinfection requires enough high illumination intensity, achieved via an association of several bulbs with suitable exposure times in a well-designed airing system. However, the application of UVGI in the disinfection of indoor air is limited through the necessity to avoid the harmful effects of UV on human and animal health. One of those drawbacks is contamination with by-products of disinfection with carcinogenic effects and environmental pollution (Su et al. 2018). Unlike those chemical methods, NTPs, also named cold plasma (CP), entered the decontamination processes as a new, effective, clean solution for inactivating the virus (Lacombe et al. 2017). NTP is a complex mixture, consisting of a partially ionized gas containing high-energy photons (UV), free electrons, ions, radicals, and other reactive species (Assadi et al. 2015; Jia et al. 2015; Schmidt and Jo 2015; Jiang et al. 2017; Schiappacasse et al. 2020). It produces high-energy electrons which bump gas molecules, driving their dissociation, excitation, and ionization (Huang et al. 2018), thereby occurring many reactive oxidative species (ROS) including.OH, O2−, O3, and H2O2. This ROS may effectively inactivate viruses (Li et al. 2020), as well as nitrogen species (NS) which play vital roles in virus inactivation (Wang et al. 2016). It is one of the advanced oxidation technologies proven effective in biomedical fields, including decontamination and sterilization, due to its low cost, easy operation, and wide range of applications (Feng et al. 2020). It is also essentially clean and generates only small amounts of persistent chemical species (Moreau et al. 2008). Few papers report NTP as an antiviral treatment in the air, yet it shows great promise and has proven to inactivate many types of microorganisms such as airborne viruses (Gallagher et al. 2004; Scholtz et al. 2015). For instance, NTP inactivation of coronavirus (COVID-19) (Chen and Wirz, 2020), Newcastle disease virus (NDV) (Su et al. 2018), and avian influenza virus (AIV) (Wang et al. 2016) have been successful. Thus, strategies should continue to be developed to improve NTP-based technologies to battle viruses for humanity’s long-term benefit.
This review focuses on NTPs for the inactivation of viruses in indoor air. It is an attractive advanced oxidation technology since it is a new, effective, clean solution for inactivating the virus and presents recent advances in the exciting area of virus’s inactivation, identifying applications and inactivation mechanisms, and summarizing findings in the latest literature experiments. An enumeration of the worldwide problem related to airborne viruses is cited. The effect of key operating parameters on NTP plasma techniques used in the literature is developed.
Viruses in indoor air
The term “indoor” includes all enclosed spaces occupied by humans such as homes, offices, schools, workplaces, commercial units, airports, hospitals, other health facilities (Moreau et al. 2008). According to the Environmental Protection Agency (EPA), many people spend about 90% or more (i.e., most of their time indoors) (Chen et al. 2020). People spend more time at home than in any other indoor environment (Scholtz et al. 2015). Also, indoor air pollution is 2–5 times more polluted than outside air pollution. In extreme cases, it can be over 100 times higher (Chen et al. 2020) because of the various sources of indoor chemical pollution like formaldehyde from wood and biologic pollution (Anderson and Albert 1998). Besides, a study estimated the total concentrations of viruses in indoor air and found about 105 particles m−3, which is an extremely high concentration (Chen et al. 2020). Environmental Protection Agency (EPA) ranks indoor air pollution as one of the top 5 environmental hazards and health threats, improving indoor air quality (IAQ) to reduce sickness. IAQ is the field of applied science or analysis of indoor air conditions that includes the viral, microbiological, and chemical-physical composition in the air in and around buildings (Maisey 2012). The definition of acceptable IAQ is provided by standard ISO 16000 “air in confined environments” in particular ISO 16814: air in an internal building which does not displease the vast majority of people inside to ensure them healthy conditions and is unlikely to contain pollutants leading to a risk to exposure to health (Prussin et al. 2015). The World Health Organization (WHO) stated that IAQ is essential for preserving human health.
Indoor air quality has a significant impact on human health status. Therefore, WHO concluded that it is the human right to breathe healthy indoor air. It is, therefore, the responsibility of all those involved to ensure acceptable indoor air quality. It becomes just like an invisible killer (World Health Organization 2000). According to China Standardization Association, 68% of illnesses are caused by poor indoor air quality (Vohra et al. 2006). In addition, some authors reported that higher disease and mortality rates are linked to air pollution and poor indoor air quality [46]. Yet, exposure to air pollutants can increase the susceptibility and severity of respiratory viruses in indoor air. Most upper respiratory infections (URIs) like cold, pneumonia, pharyngitis, laryngitis, and epiglottitis are caused by over 200 different viruses, including influenza viruses, rhinoviruses, coronaviruses, adenoviruses, respiratory syncytial viruses, and enteroviruses (US EPA, 2006). Recently, other viruses emerged at the end of 2019, such as SARS-CoV-2, killing millions of people worldwide, thus demonstrating the dangerousness of infectious respiratory diseases. Due to their high airborne transmission ability, inhaling these viruses can cause or worsen disease in humans (Rahmani et al. 2020), especially in crowded and poorly ventilated environments. They are responsible for most upper respiratory infections (Cimbala 2003). Many of the illnesses associated with SARS-CoV-2 that increase the risk of death are those caused by long-term exposure to air pollution (Xiao et al. 2020). Indoor virus species is one of the most common environmental health problems reported today (Table1). Exposure to aerosols generated by coughing and sneezing from infected individuals or in contact with droplet-contaminated surfaces (plastic, metal, and clothing) has been widely viewed as the dominant mode of transmission of respiratory pathogens (virus and bacteria). In addition, it has been validated that airborne transmission is traditionally defined as involving the inhalation of infectious aerosols primarily at a distance of less than 1 to 2 m from the individual carrying the virus. Such transmission has been reported, and considered as the main route of virus transmission. However, recently airborne transmission of many respiratory viruses has been validated, such as coronavirus (SARS-CoV), Middle East respiratory syndrome (MERS)-CoV, and influenza virus (Wang et al. 2021).
Table 1.
Not exhaustive list on types of viruses and their effects on human health
| Type of virus | Effects on human health | Ref |
|---|---|---|
| SARS-CoV-2 | SARS-CoV-2 does not damage only the respiratory system and lungs; it can infect the urogenital system, nervous system, digestive system, and circulatory system. It can also cause an inflammatory cascade. Among its symptoms are mild disease, severe lung injury, and multi-organ failure leading to death, especially in older patients with other comorbidities. Other significant outcomes of coronavirus infection are acute respiratory distress syndrome and pulmonary fibrosis. The infection’s long-term implications on human health are unknown, like the virus’s possible impacts on cellular lifetime as well as organismal healthspan, which can cause diseases such as Parkinson’s and other neurodegenerative illnesses | (Day et al. 2020; Liang et al. 2020; Lippi et al. 2020; Monteil et al. 2020; Zhang et al. 2020) |
| Rhinoviruses | The main site of RV infection is the nasal mucosa. It is a common cause of colds (acute nasopharyngitis), which is a mild disease of the upper respiratory tract. It can also cause chronic obstructive pulmonary disease, asthma, or cystic fibrosis might become life-threatening | (Myatt et al. 2004; Turner 2007; Ashraf et al. 2013; Blaas and Fuchs 2016; Thibaut et al. 2016; To Kelvin et al. 2017) |
| MS2 Bacteriophage | MS2 is an enteric virus; it is non-hazardous to humans and animals and is widely utilized as a surrogate for pathogenic viruses in aerosol investigations. It is an example of noroviruses which are highly infectious and are associated with sporadic gastroenteritis | (Olson et al. 2004; Dawson et al. 2005; Tung-Thompson et al. 2015) |
| Influenza viruses (types A, B, C) | Influenza is a highly contagious viral respiratory disease. A dry cough, headaches, muscular and joint discomfort, and general weariness are among the symptoms. The flu can become dangerous, requiring hospitalization or even death | (Hayden et al. 1998; Brankston et al. 2007; Carrat et al. 2008; World Health Organization 2019) |
| Varicella viruses | Varicella virus, one of the five human herpes viruses, causes two distinct diseases, varicella (chickenpox) and shingles (herpes zoster). Its symptoms are fever concurrent with a self-limiting rash on the skin and sometimes mucosa. Headache, malaise, and loss of appetite | (Mueller et al. 2008; Andrei and Snoeck 2013; Sauerbrei 2016) |
| Measles virus | Measles is a disease that can infect only humans; it attacks immunological cells, leading to a rapid deterioration of the immune system. It can cause three different types of encephalitis or central nervous system (CNS) diseases which are acute postinfectious encephalitis, acute progressive infectious encephalitis, and the lethal neurodegenerative disease subacute sclerosing panencephalitis | (Bellini et al. 1994; Norrby and Kristensson 1997; Mrkic et al. 1998; Reuter and Schneider-Schaulies 2010; Mina et al. 2019) |
| Hantavirus | Hantavirus pulmonary syndrome is a zoonotic disease; its transmission to humans can lead to hemorrhagic fever with renal syndrome or nephropathy epidemic named hantavirus pulmonary syndrome, also leading to disease with severe cardiopulmonary | (Khaiboullina and St. Jeor 2002; Muranyi et al. 2005; Bartholomeusz and Locarnini 2006; Tersago et al. 2009, 2011; Muylaert et al. 2019) |
| Viral meningitis | Meningitis is considered a bacterial and viral disease. Viral meningitis can infect the human brain, and its infection can cause headaches, encephalitis, malaise, long-term sleep disorders, and depression. In most cases, there are no major side effects | (Peate 1999; Schmidt et al. 2006; Tuppeny 2013; McGill et al. 2017) |
| Mumps virus | Mumps is a mildly infectious disease that affects children. However, in some situations, its systemic infection can have serious clinical effects, particularly when the sickness is postponed into adulthood. It infects pancreatic Beta cells, which can lead to fever, swelling of the parotid glands, fatigue, low-grade fever, attacks of tachycardia, and night sweating | (Parkkonen et al. 1992; Gut et al. 1995; Nöjd et al. 2001; Mühlemann 2004) |
Viruses such as the coronavirus (i.e., SARS-CoV-2) are intracellular parasites that are very small in the range of 20 to 400 nm. These viruses are resistant to indoor air for a long time, especially in crowded or small environments. Inhaling these viruses causes illness or worsens infections of the upper respiratory tract (Prussin et al. 2015). In the event of a viral pandemic, many countries implement containment measures to prevent the spread of the virus. Still, this practice induces poor indoor air quality, which will lead to other health problems. Indoor air in enclosed public spaces is at increased risk of viruses because IAQ regulations are not adapted to current scientific research. So, viruses can spread through the air and even easily enter indoor air (World Health Organization 2000). Once locked in, even simple actions like talking, sneezing, and coughing that cause small virus-filled droplets of saliva to spread through the air and onto surfaces, especially on the hands (Alshraiedeh et al. 2013). Viral infection can spread from person to person, making humans a significant source of indoor viral infection. Pets are also a foremost source of indoor air contamination. Viruses can infect all living cell-based organisms, from bacteria to humans, animals, and plants (Filipić et al. 2020a, b).
Indoor air humidity is a major determinant of indoor air quality (Sakudo et al. 2014). It plays an important role in viral infections by promoting the survival rate of viruses and an increased risk of respiratory infections and allergic diseases (Aboubakr et al. 2018). Several studies demonstrated that indoor temperature and humidity (generally between 19 and 26 °C and 50–60% RH) positively affect the spread of infections and the vulnerability of individuals to viruses (Liang et al. 2020).
Pandemics such as COVID-19 require implementing new indoor air purification techniques (Kim and Jang, 2018), replacing, combining, or improving existing conventional viral inactivation methods. Conventional methods for viral inactivation, such as chlorine disinfection, do not have an effective disinfection ability against viruses (Ashraf et al. 2013). Unlike those methods, NTPs can deal with both transport and infectivity of airborne viruses by filtration and interact with interactive plasma species (Xia et al. 2019).
Parameters controlling viruses’ inactivation performance
Several parameters remain essential in the non-thermal discharge viruses’ inactivation, such as virus concentration, input power, air humidity, air composition, reactor design, and type of discharge. It is also worth noting the oxygen concentration.
The effect of the viruses’ concentration
The virus concentration effect in the non-thermal discharge viruses’ inactivation was reported in several studies (Chen et al. 2010). Indeed, Puligundla and Mok (Puligundla and Mok, 2016) revealed a reduction of at least 4 to 6 log10 of two bacteriophages at concentrations of 106 PFU/mL−1 after 10 min of exposure to NTP.
After a couple of seconds of discharge treatment, the number of infectious phages decreased quickly, and 6 orders of magnitude inactivation were achieved. On the other hand, the virus concentrations used in NTPs ranked from 1 × 106 PFU mL−1 to 300 PFU mL−1 within several studies (Chen et al. 2010; Puligundla and Mok 2016; Jiang et al. 2017; Filipić et al. 2020a). We noted 105 TCID50/mL of bacteriophage MS2, matching 69 × 106 PFU/mL according to Xia et al. (Xia et al. 2019) study, while that of Venezia et al. (Alshraiedeh et al. 2013) denoted 109 PFU/mL.
Thus, some works reported a proportional relationship between virus concentration and the inactivation performance with non-thermal plasma: the inactivation yield of virus decrease with very polluted indoor air. This finding might be due to the higher virus concentration, and the step limitation is the reaction between reactive species and viruses (Lee et al. 2021).
Input power
Input power is an important factor in influencing virus removal in NTP reactors. In fact, virus elimination measurements are a function of input power (Mustafa et al. 2018). Several previous studies demonstrated that the removal efficiencies of harmful airborne components increase with the NTP input power (Shimizu and Oda 1999; An et al. 2011; Pinard et al, 2019; Xia et al. 2019). It is well known that the power of the plasma is proportional to the voltage applied in the discharge zone. Indeed, the increase in electric power pleads in favor of having an increase in electric current in the vicinity of the virus. Since the virus is in direct contact with the plasma, the exposure of the virus to species produced by short-lived plasma, including electrons, ions, radicals, and UV rays, is significantly higher compared to other treatment modalities. Likewise, the virus will also be subjected to high electric fields at the plasma-surface interface. All of these active species (OH°, O°, O3, e−) ensure the inactivation of the virus (Mohamed et al. 2021).
Indeed, Xia et al. (Xia et al. 2019) examined viruses’ inactivation through NTP coupled with a packed-bed dielectric barrier discharge plasma. After NTP treatment, the results revealed a higher inactivation of phage MS2 with a rise in the applied voltage up to 30 kV (Alshraiedeh et al. 2013).
Air humidity
The non-thermal discharge viruses’ inactivation can be affected by many environmental factors such as air humidity versus the different reactors. For instance, Cutler et al. (Cutler et al. 2012) demonstrated that for any temperature, the rate of the inactivation of the airborne porcine reproductive and respiratory syndrome (PRRS) was highest at a relative humidity between 25 and 79% and lowest at relative humidity > 80%. Likewise, Xia et al. (Xia et al. 2020) found 98.6% as the PRRSv inactivation efficiency with 38% of relative humidity under 20-kV voltage supplied to the packed-bed NTP reactor. However, some authors investigated the spread of relative humidity (RH) within the NTP reactor, and they found that the RH evolved to reach 60% at a steady state in 30 min (Xia et al. 2019). This result obtained with the NTP reactor corroborates that of Cutler et al. (Cutler et al. 2012) in the case of the PRRS virus, regarding the RH effect on the reactor efficiency. On the other hand, other studies have reported that the relative humidity of the PRRS virus depends on the viral envelopes (Elazhary and Derbyshire, 1979). Viruses with lipoprotein envelopes tend to be more stable at lower relative humidity and non-enveloped viruses more stable at higher relative humidity. Overall, relative humidity plays an important role in the different reactors’ yields. The divergence in the resulting level is due to the difference in generating the plasma process, the residence time, reactor configuration, etc.
Reactor for the inactivation of viral aerosols
Over the past 20 years, several technologies have been devised for the inactivation of non-thermal discharge viruses (Jacobs et al. 2010; Alshraiedeh et al. 2013; Sakudo et al. 2014).
Recently, some studies examined microbial inactivation, sterilization, and disinfection using APNTP within a field of biomedical application (Fridman et al. 2008). APNTP applying possesses potential favor over standard chemical sterilants and disinfectants (Fig. 1). These include the design’s simplicity and operation. It uses non-toxic gases with the absence of toxic residues and the production of a large amount of various microbicidal active species, including chemically reactive species (Yardimci and Setlow, 2010; Nayak et al. 2018) (Table 2).
Fig. 1.
Schematic of the DBD packed-bed reactor for the inactivation of viral aerosols (Michielsen et al. 2017; Uytdenhouwen et al. 2018)
Table 2.
plasma reactor configuration for viruses and bacterial inactivation treatment for some types of the virus with reactive species.
| Virus | Reactive species responsible for the inactivation | NTP reactor configuration | Mode of inactivation | References |
|---|---|---|---|---|
| SARS-CoV-2 | RONS | Cylindrical cold atmospheric plasma reactor (CCAPR) | DNA/RNA degradation | (Chen et al. 2020) |
| MS2 bacteriophage | O | Tubular atmospheric pressure cold plasma (TAPCP) | Both protein and DNA/RNA degradation | (Wu et al. 2015) |
| O3 | NA | (Xia et al. 2019) | ||
| Adenovirus | H2O2 | surface micro-discharge (SMD) plasma electrode using an insulator plate made of Al2O3 | DNA/RNA degradation | (Sakudo et al. 2016) |
| O3 | NA | (Zimmermann et al. 2011) | ||
| T4, Φ174, and MS2 | O2, NO2, and ONOO− | Mesh electrode with a planar configuration | Both protein and DNA/RNA degradation | (Guo et al. 2018) |
| Feline calicivirus (FCV) | O and ONOOH | Tubular reactor plasma | Protein degradation | (Aboubakr et al. 2016) |
| O2 and ONOO− | DNA/RNA degradation | (Yamashiro et al. 2018) | ||
| O2 and O3 | Both protein and RNA degradation | (Aboubakr et al. 2018) | ||
| NOx and O3 | NA | (Nayak et al. 2018) | ||
| Respiratory syncytial virus (RSV) | H2O2 | Tubular NTP reactor | DNA/RNA degradation | (Sakudo et al. 2017) |
| HIV-1 | O2+, O, NO, and N2 | Cylindrical cold atmospheric plasma reactor (CCAPR) | DNA/RNA degradation | (Volotskova et al. 2016) |
| Newcastle disease virus (NDV) | H2O2, OH•, and NOx | Magnetically rotated gliding arc & DBD plasma planar reactor | Both protein and DNA/RNA degradation | (Su et al. 2018) |
| RONS | RNA degradation | (Schiappacasse et al. 2020) | ||
| Influenza viruses | H2O2 | Both protein and RNA degradation | (Sakudo et al. 2014) | |
| Influenza A | OH and O3 | NA | (Gallagher et al. 2004) |
Combined system for virus disinfection
Several works have been reported on conventional techniques for viruses and bacterial inactivation treatment, whether physical or chemical (Table 3). Some technologies have been combined with different forms of electric discharge plasma or other decontamination processes to deal with various pathogenic microorganisms’ high levels of contamination to improve inactivation efficiency (Bourke et al. 2018; Kordová et al. 2018; Rtimi and Kiwi, 2021).
Table 3.
Summary of studies on plasma combination technologies for virus inactivation
| Combination systems | Virus types | Experimental conditions | Results | Ref |
|---|---|---|---|---|
| Non-thermal plasma-activated by NaCl or H2O2 solutions | Newcastle disease virus (NDV) | 10 mL sterile distilled water, 0.9% NaCl, and 0.3% H2O2 solutions | Complete inactivation of NDV after only 30 min of treatment | (Su et al. 2018) |
| Atmospheric pressure non-thermal plasma (NTP) jet with Ar/O2/N2 | Newcastle disease virus (NDV) strain and H9N2 avian influenza virus (AIV) | A mixture containing 88% Ar, 2% O2, and 10% N2 at a flow rate of 5 L/min was used as working gas | Complete inactivation in 2 min of treatment for both NDV and AIV | (Wang et al. 2016) |
| Cold oxygen plasma + an internal classic UV-C lamp | Respiratory syncytial virus (RSV) and human parainfluenza virus type 3 (hPIV-3), and influenza virus A (H5N2) | 50 mL of viral pellets were suspended in PBS | More than 99.98 of reduction regardless of the virus type | (Assadi et al. 2015) |
| Non-thermal plasma coupled to a packed-bed dielectric barrier discharge reactor | Aerosols of phage MS2 | At 30 kV and an airflow rate of 170 standard liters per minute | A reduction of ~ 2 log of the MS2 inactivated and ~ 0.35 log physically removed in the packed bed was observed | (Xia et al. 2020) |
| Packed-bed dielectric barrier discharge non-thermal plasma combined with filtration | Porcine reproductive and respiratory syndrome virus (PRRSv | From 12 to 30 kV with RH = 38–49% at 5–12 cfm | More than 40% at 12 cfm and more than 80% at 5 cfm of reduction regardless of the virus SARS (MS2) | (Xia et al. 2019) |
In recent years, current trends have been moving towards the coupling of plasma and nanomaterials with dimensions in the order of a nanometer (i.e., 1 to 100 nm). This process has been well confirmed with the inactivation effects of nanomaterials on various viruses due to a large specific surface area, including the generation of ROS (Abidi et al. 2019, 2020). The effects resulting from the combination between the plasma in the catalytic oxidation, the photothermal influences, and the release of metal ions allow having a synergistic impact on the antiviral performances (Li et al. 2021). Therefore, there is a comprehensive promise in developing antiviral nanomaterials and using them to air purifier filters, building ventilation systems, antiviral fabrics, and antiviral spray agents, which assists in controlling the spread of viruses through aerosols.
Mechanism of viral inactivation by the non-thermal discharge
Non-thermal plasma constitutes one of the recent processes of advanced oxidation processes (AOPs). This technology allows the formation of heavy mixtures and lighting from the excitation of gases by electric discharge. Probably, the effectiveness of NTPs is because they combine both physical and chemical mechanisms (Ateia et al. 2020). However, these coupled techniques generate highly reactive oxidizing components, free radicals, and ions (e.g., ozone, hydrogen peroxide, hydroxyl, and superoxide radicals) in aqueous solutions under UV irradiation (Wang et al. 2018). Figure 1 shows a schematic of the action of NTP of viral inactivation by the non-thermal discharge. The generation of reactive oxygen species (ROS) and/or reactive nitrogen species (RNS) is the main feature of NTP that contributes to virus inactivation. The main target of ROS/RNS is virus capsid, genome, protein, and glycoprotein. The short lifespan of ROS or RNS makes the identification and assessment of ROS/RNS a challenging task. Furthermore, the experimental conditions (the gas used for the NTP generation, the matrix, the virus treated…etc.) play a crucial role in the generation of particular ROS/RNS.
The most crucial component for evaluating virus inactivation is the degradation of the capsid. The viral envelope or capsid is the first contact point with the host cell. For an efficient recognition of a virus by the cell receptors, their outer structure must be intact.
The increased oxidative force of NTP can denature the virus and genome structure by affecting both proteins and nucleic acids. Conformational disruption of the capsid proteins caused by ROS/RNS can result in loss of viral infectivity due to the virus’s disruption binding to receptors on the host cell membrane (Filipić et al. 2020b).
In addition to capsid and nucleic acid, further damage could be seen in lipid components from the envelope the virus influenza A (Sakudo et al. 2014). Particularly in the case of bacteriophage λ (Yasuda et al. 2010) and FCV (Aboubakr et al. 2018), it has been proved that the main mode of NCP inactivation is the degradation of the capsid proteins proceeding with the degradation of nucleic acids (Fig. 2). However, in several studies, it was impossible to determine which degradation path contributed more to the decay in viral infectivity (Filipić et al. 2020b).
Fig. 2.
A schematic of the action of NTP of viral inactivation by the non-thermal discharge
Chemical processes’ reactions
It is worthy to note that in humid air, electrons with very high kinetic energy and could react with water vapor to occur reactive species. Then, some reactive chemical species (i.e., H2O2, O3, O2−·,·OH) also react by attacking the high-energy electron (Wang et al. 2018). In fact, electrons energy generated through the electrical discharge plasma process can outdo the decay or ionization energy of water molecules (Joshi et al. 1995; Wang et al. 2008). Through electron collisions, the dissociation of water molecules in the air could form H, OH, and other hydrated cations as follows (Hong and Zeng, 2002; Wang et al. 2008):
| 1 |
| 2 |
| 3 |
where * denoted high-energy electron state. These formed radicals could react together or recombine with other reactive species, as presented in the following reactions (Zhou et al. 2016):
| 4 |
| 5 |
| 6 |
| 7 |
| 8 |
Despite the free radicals’ generation for virus degradation in NTPs, ozone (O3) reactions also occur. Once ·O is formed (i.e., Eq. 8) via high-energy electronic attack, it could react with O2 and organic matter (M) to generate O3, as shown in the reaction (9) (Wang et al. 2018).
| 9 |
where M is organic matter, O3 could react with various compounds through direct O3 and indirect O3 oxidation reactions. In previous studies, also it was found that the ozone produced by plasma was not the main contributor to the inactivation effect; nevertheless, it is involved in the inactivation (Morrison et al. 2021). In fact, Morisson and her co-workers (Morisson et al. 2021) showed that ozone disinfection had demonstrated high efficacy against enveloped and non-enveloped viruses, including viruses similar in morphology to SARS-CoV-2.
Physical processes’ reactions
The physical processes of the inactivation effect in non-thermal plasma can occur via UV irradiation (Sun et al. 2005; Wang et al. 2006; Tang et al. 2018), shock waves (Šunka 2001; Ghernaout and Elboughdiri, 2020), and electric field effects (Schoenbach et al. 1997, 2000). Indeed, the UV irradiation from gas-phase discharges is weaker than that from the liquid phase. The types of UV irradiation from gas-phase discharges at atmospheric pressure are generally within the UVA and UVB regions, with wavelengths ranging of 320–400 nm and 280–320 nm, respectively. Matsumoto et al. (Matsumoto et al. 1992) reported that UV irradiation performed an essential part in bacteria inactivation. Moreover, UV irradiation has also been used in the gas-phase discharge plasma process (Xue et al. 2008).
In the absence of electric discharge, the electric field is an alternative method for inactivating cells and processing food products. Previous research reported that a potent electric field could inactivate the microorganisms and biofilm bacteria on the walls of cooling and drinking water pipes (Schoenbach et al. 2000).
Conclusions and outlook
Over the past decades, interest in applying non-thermal plasma technology for virus inactivation within indoor air has considerably increased. In this review paper, commonly used non-thermal plasma reactors and their effectiveness in virus inactivation have been extensively exhibited. Moreover, the inactivation mechanisms and the factors controlling these reactors, such as virus concentration, input power, air humidity, air composition, and reactor design, have also earned attention.
Notwithstanding the determining factors in non-thermal plasma processes, the production and evolution of active species and the physical effects of viral inactivation must be further investigated to explain the mechanisms of plasma oxidation and optimize the oxidation non-thermal plasmas process. Furthermore, investigations should be performed on the impact of target properties, including volatility, hydrophobic/hydrophilic nature, stability, and diffusivity. However, non-thermal plasma can be combined with other technologies involving catalysts like carbonaceous materials, metal oxides, and metal ions. The mechanism of interaction between viral inactivation and catalysts needs to be well studied. Well-mastered non-thermal plasma could be a promising alternative to face these waves of COVID-19 infections.
Author contribution
Imen ASSADI: validation, investigation, visualization, resources, writing–original draft, writing–review & editing.
Oussama BAALOUDJ and Hichem ZEGHIOUD: methodology, validation, writing–original draft, writing–review & editing.
Walid ELFALLEH and Naoufel BENHAMMADI: conceptualization, validation, writing–original draft, writing–review & editing, visualization, supervision.
Ahlem GUESMI: methodology, resources, supervision.
Lotfi KHEZAMI: methodology, validation, investigation, review & editing.
Aymen ASSADI: conceptualization, methodology, supervision.
Funding
This research was supported by the Deanship of Scientific Research, Imam Mohammad Ibn Saud Islamic University (IMSIU), Saudi Arabia, Grant No. (21–13-18–035).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication:
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abidi M, Assadi AA, Bouzaza A, et al. Photocatalytic indoor / outdoor air treatment and bacterial inactivation on CuxO / TiO2 prepared by HiPIMS on polyester cloth under low intensity visible light Applied Catalysis B : Environmental photocatalytic indoor / outdoor air treatment and bacterial. Appl Catal B Environ. 2019;259:118074. doi: 10.1016/j.apcatb.2019.118074. [DOI] [Google Scholar]
- Abidi M, Hajjaji A, Bouzaza A, et al. Simultaneous removal of bacteria and volatile organic compounds on Cu2O- NPs decorated TiO2 nanotubes competition effect and kinetic studies Journal of Photochemistry & Photobiology A : Chemistry Simultaneous removal of bacteria and volatile organic compo. J Photochem Photobiol A Chem. 2020;400:112722. doi: 10.1016/j.jphotochem.2020.112722. [DOI] [Google Scholar]
- Aboubakr HA, Gangal U, Youssef MM, et al. Inactivation of virus in solution by cold atmospheric pressure plasma: identification of chemical inactivation pathways. J Phys D Appl Phys. 2016;49:45. doi: 10.1088/0022-3727/49/20/204001. [DOI] [Google Scholar]
- Aboubakr HA, Mor SK, Higgins LA, et al. Cold argon-oxygen plasma species oxidize and disintegrate capsid protein of feline calicivirus. PLoS ONE. 2018;13:1–24. doi: 10.1371/journal.pone.0194618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshraiedeh NH, Alkawareek MY, Gorman SP, et al. Atmospheric pressure, nonthermal plasma inactivation of MS2 bacteriophage: effect of oxygen concentration on virucidal activity. J Appl Microbiol. 2013;115:1420–1426. doi: 10.1111/jam.12331. [DOI] [PubMed] [Google Scholar]
- Amissah P. Indoor air quality: combining air humidity with construction moisture. Environ Pollut. 2005;449:461–469. doi: 10.1016/j.scitotenv.2012.12.043. [DOI] [Google Scholar]
- An G, Sun Y, Zhu T, Yan X. Degradation of phenol in mists by a non-thermal plasma reactor. Chemosphere. 2011;84:1296–1300. doi: 10.1016/j.chemosphere.2011.05.007. [DOI] [PubMed] [Google Scholar]
- Anderson EL, Albert RE (1998) Risk assessment and indoor air quality
- Andrei G, Snoeck R (2013) Advances in the treatment of varicella-zoster virus infections, 1st edn. Copyright © 2013 Elsevier Inc. All rights reserved. [DOI] [PubMed]
- Ashraf S, Brockman-Schneider R, Bochkov YA, et al. Biological characteristics and propagation of human rhinovirus-C in differentiated sinus epithelial cells. Virology. 2013;436:143–149. doi: 10.1016/j.virol.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assadi AA, Bouzaza A, Wolbert D, et al (2015) Study of synergetic effect by surface discharge plasma / TiO2 combination for indoor air treatment : sequential and continuous configurations at pilot scale to cite this version : HAL Id : hal-01158449
- Ateia M, Alalm MG, Awfa D, et al. Modeling the degradation and disinfection of water pollutants by photocatalysts and composites: a critical review. Sci Total Environ. 2020;698:134197. doi: 10.1016/j.scitotenv.2019.134197. [DOI] [PubMed] [Google Scholar]
- Australia Building Codes Board (2018) Handbook: indoor air quality
- Bartholomeusz A, Locarnini S. Associated with antiviral therapy. Antivir Ther. 2006;55:52–55. doi: 10.1002/jmv. [DOI] [Google Scholar]
- Bellini WJ, Rota JS, Rota PA. Virology of measles virus. J Infect Dis. 1994;170:S15–S23. doi: 10.1093/infdis/170.Supplement_1.S15. [DOI] [PubMed] [Google Scholar]
- Blaas D, Fuchs R. Mechanism of human rhinovirus infections. Mol Cell Pediatr. 2016;3:16–19. doi: 10.1186/s40348-016-0049-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourke P, Ziuzina D, Boehm D, et al. The potential of cold plasma for safe and sustainable food production. Trends Biotechnol. 2018;36:615–626. doi: 10.1016/j.tibtech.2017.11.001. [DOI] [PubMed] [Google Scholar]
- Brankston G, Gitterman L, Hirji Z, et al. Transmission of influenza A in human beings. Lancet Infect Dis. 2007;7:257–265. doi: 10.1016/S1473-3099(07)70029-4. [DOI] [PubMed] [Google Scholar]
- Carrat F, Vergu E, Ferguson NM, et al. Time lines of infection and disease in human influenza: a review of volunteer challenge studies. Am J Epidemiol. 2008;167:775–785. doi: 10.1093/aje/kwm375. [DOI] [PubMed] [Google Scholar]
- Chang Y. China needs a tighter PM2.5 limit and a change in priorities. Environ Sci Technol. 2012;46:7069–7070. doi: 10.1021/es3022705. [DOI] [PubMed] [Google Scholar]
- Chen CY, Wu LC, Chen HY, Chung YC. Inactivation of staphylococcus aureus and escherichia coli in water using photocatalysis with fixed TiO2. Water Air Soil Pollut. 2010;212:231–238. doi: 10.1007/s11270-010-0335-y. [DOI] [Google Scholar]
- Chen Z, Garcia G, Arumugaswami V, Wirz RE (2020) Cold atmospheric plasma for SARS-CoV-2 inactivation. Phys Fluids 3210.1063/5.0031332 [DOI] [PMC free article] [PubMed]
- Chen Z, Wirz RE (2020) Cold atmospheric plasma for COVID-19. Preprints 1–7. 10.20944/preprints202004.0126.v1
- Cimbala JM (2003) Indoor air quality engineering_ environmental health and control of indoor pollutants (Drugs & the Pharmaceutical Sciences)
- Couch RB. Viruses and indoor air pollution. Bull New York Acad Med J Urban Heal. 1981;57:907–921. [PMC free article] [PubMed] [Google Scholar]
- Cutler TD, Wang C, Hoff SJ, Zimmerman JJ. Effect of temperature and relative humidity on ultraviolet (UV 254) inactivation of airborne porcine respiratory and reproductive syndrome virus. Vet Microbiol. 2012;159:47–52. doi: 10.1016/j.vetmic.2012.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DJ, Paish A, Staffell LM, et al. Survival of viruses on fresh produce, using MS2 as a surrogate for norovirus. J Appl Microbiol. 2005;98:203–209. doi: 10.1111/j.1365-2672.2004.02439.x. [DOI] [PubMed] [Google Scholar]
- Day T, Gandon S, Lion S, Otto SP. On the evolutionary epidemiology of SARS-CoV-2. Curr Biol. 2020;30:R849–R857. doi: 10.1016/j.cub.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elazhary MA, Derbyshire JB. Effect of temperature, relative humidity and medium on the aerosol stability of infectious bovine rhinotracheitis virus. Can J Comp Med. 1979;43:158–167. [PMC free article] [PubMed] [Google Scholar]
- Fang B, Xu Q, Park T, Zhang M (2016) AirSense: an intelligent home-based sensing system for indoor air quality analytics. UbiComp 2016 - Proc 2016 ACM Int Jt Conf Pervasive Ubiquitous Comput 109–119. 10.1145/2971648.2971720
- Feng X, Chen C, He C, et al. Non-thermal plasma coupled with MOF-74 derived Mn-Co-Ni-O porous composite oxide for toluene efficient degradation. J Hazard Mater. 2020;383:121143. doi: 10.1016/j.jhazmat.2019.121143. [DOI] [PubMed] [Google Scholar]
- Filipić A, Gutierrez-Aguirre I, Primc G, et al. Cold plasma, a new hope in the field of virus inactivation. Trends Biotechnol. 2020 doi: 10.1016/j.tibtech.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipić A, Gutierrez-Aguirre I, Primc G, et al (2020b) Cold plasma, a new hope in the field of virus inactivation. Trends Biotechnol xx:1–14. 10.1016/j.tibtech.2020.04.003 [DOI] [PMC free article] [PubMed]
- Fridman G, Friedman G, Gutsol A, et al. Applied plasma medicine. Plasma Process Polym. 2008;5:503–533. doi: 10.1002/ppap.200700154. [DOI] [Google Scholar]
- Gallagher MJ, Gutsol A, Fridman A, et al (2004) Non-thermal plasma applications in air sterilization. IEEE Int Conf Plasma Sci 19810.1109/plasma.2004.1339779
- Ghernaout D, Elboughdiri N. Disinfecting water: plasma discharge for removing coronaviruses. Oalib. 2020;07:1–29. doi: 10.4236/oalib.1106314. [DOI] [Google Scholar]
- Giuseppina La Rosa, Marta Fratini SDL, Muscill MI and M (2013) Viral infections acquired indoors through airborne, droplet or contact transmission. Ann Ist Super Sanità 124–13210.4415/ANN_13_02_03 [DOI] [PubMed]
- Guo L, Xu R, Gou L, et al. Mechanism of virus inactivation by cold atmospheric-pressure plasma and plasma-activated water. Appl Env Microbiol. 2018;84:1–10. doi: 10.1128/AEM.00726-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gut J-P, Lablache C, Behr S, Kirn A. Symptomatic mumps virus reinfections. J Med Virol. 1995;45:17–23. doi: 10.1002/jmv.1890450104. [DOI] [PubMed] [Google Scholar]
- Hament JM, Kimpen JLL, Fleer A, Wolfs TFW. Respiratory viral infection predisposing for bacterial disease: a concise review. FEMS Immunol Med Microbiol. 1999;26:189–195. doi: 10.1016/S0928-8244(99)00159-5. [DOI] [PubMed] [Google Scholar]
- Hayden FG, Fritz RS, Lobo MC, et al. Local and systemic cytokine responses during experimental human influenza A virus infection. Relation to symptom formation and host defense. J Clin Invest. 1998;101:643–649. doi: 10.1172/JCI1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong PKA, Zeng Y. Degradation of pentachlorophenol by ozonation and biodegradability of intermediates. Water Res. 2002;36:4243–4254. doi: 10.1016/S0043-1354(02)00144-6. [DOI] [PubMed] [Google Scholar]
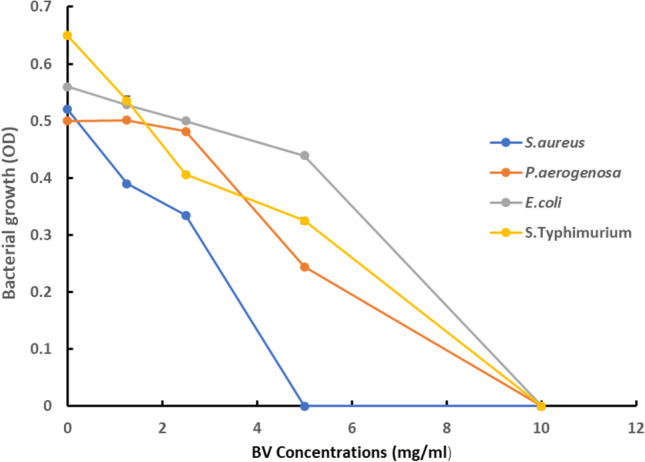
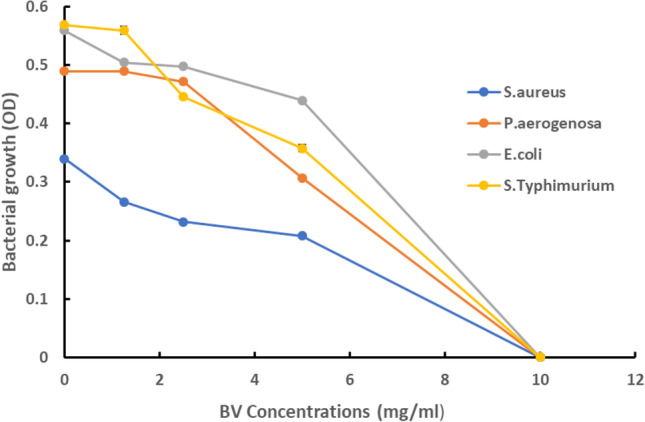
- Huang M, Zhuang H, Wang J, et al. Inactivation kinetics of Salmonella typhimurium and Staphylococcus aureus in different media by dielectric barrier discharge non-thermal plasma. Appl Sci. 2018;8:1–15. doi: 10.3390/app8112087. [DOI] [Google Scholar]
- Jacobs AC, Hermann JR, Muñoz-Zanzi C, et al. Stability of porcine reproductive and respiratory syndrome virus at ambient temperatures. J Vet Diagnostic Investig. 2010;22:257–260. doi: 10.1177/104063871002200216. [DOI] [PubMed] [Google Scholar]
- Jia Z, Barakat C, Dong B, Rousseau A (2015) VOCs Destruction by plasma catalyst coupling using AL-KO PURE Air purifier on industrial scale. 19–26
- Jiang N, Qiu C, Guo L, Shang K (2017) Post plasma-catalysis of low concentration VOC Over alumina-supported silver catalysts in a surface / packed-bed hybrid discharge reactor10.1007/s11270-017-3296-6
- Joshi AA, Locke BR, Arce P, Finney WC. Formation of hydroxyl radicals, hydrogen peroxide and aqueous electrons by pulsed streamer corona discharge in aqueous solution. J Hazard Mater. 1995;41:3–30. doi: 10.1016/0304-3894(94)00099-3. [DOI] [Google Scholar]
- Khaiboullina SF, St Jeor SC. Hantavirus immunology. Viral Immunol. 2002;15:609–625. doi: 10.1089/088282402320914548. [DOI] [PubMed] [Google Scholar]
- Kim J, Jang J. Inactivation of airborne viruses using vacuum ultraviolet photocatalysis for a flow-through indoor air purifier with short irradiation time. Aerosol Sci Technol. 2018;52:557–566. doi: 10.1080/02786826.2018.1431386. [DOI] [Google Scholar]
- Kordová T, Scholtz V, Khun J, et al (2018) Inactivation of microbial food contamination of plastic cups using nonthermal plasma and hydrogen peroxide. J Food Qual 201810.1155/2018/5616437
- Lacombe A, Niemira BA, Gurtler JB, et al. Nonthermal inactivation of norovirus surrogates on blueberries using atmospheric cold plasma. Food Microbiol. 2017;63:1–5. doi: 10.1016/j.fm.2016.10.030. [DOI] [PubMed] [Google Scholar]
- Lee J, Bong C, Lim W, et al. Fast and easy disinfection of coronavirus-contaminated face masks using ozone gas produced by a dielectric barrier discharge plasma generator. Environ Sci Technol Lett. 2021;8:339–344. doi: 10.1021/acs.estlett.1c00089. [DOI] [PubMed] [Google Scholar]
- Li H, Li T, He S, et al (2020) Efficient degradation of antibiotics by non-thermal discharge plasma: Highlight the impacts of molecular structures and degradation pathways. Chem Eng J 39510.1016/j.cej.2020.125091
- Li R, Cui L, Chen M, Huang Y. Nanomaterials for airborne virus inactivation: a short review. Aerosol Sci Eng. 2021;5:1–11. doi: 10.1007/s41810-020-00080-4. [DOI] [Google Scholar]
- Liang Y, Wang ML, Chien CS, et al (2020) Highlight of immune pathogenic response and hematopathologic effect in SARS-CoV, MERS-CoV, and SARS-Cov-2 infection. Front Immunol 1110.3389/fimmu.2020.01022 [DOI] [PMC free article] [PubMed]
- Lippi A, Domingues R, Setz C, et al. SARS-CoV-2: at the crossroad between aging and neurodegeneration. Mov Disord. 2020;35:716–720. doi: 10.1002/mds.28084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisey SJ (2012) Air quality in homes: investigating the chemistry of indoor air pollutants through the development of a model tailored with field measurements
- Martínez-Montelongo JH, Medina-Ramírez IE, Romo-Lozano Y, Zapien JA. Development of a sustainable photocatalytic process for air purification. Chemosphere. 2020;257:127236. doi: 10.1016/j.chemosphere.2020.127236. [DOI] [PubMed] [Google Scholar]
- Matsumoto Y, Shioji N, Satake T, Sakuma A (1992) Inactivation of microorganisms by pulsed high voltage application. 652–659. 10.1109/ias.1991.178248
- McGill F, Griffiths MJ, Solomon T. Viral meningitis: current issues in diagnosis and treatment. Curr Opin Infect Dis. 2017;30:248–256. doi: 10.1097/QCO.0000000000000355. [DOI] [PubMed] [Google Scholar]
- Michielsen I, Uytdenhouwen Y, Pype J, et al. CO2 dissociation in a packed bed DBD reactor: first steps towards a better understanding of plasma catalysis. Chem Eng J. 2017;326:477–488. doi: 10.1016/j.cej.2017.05.177. [DOI] [Google Scholar]
- Mina MJ, Kula T, Leng Y, et al. Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Viral Immunol. 2019;606:599–606. doi: 10.1126/science.aay6485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed H, Nayak G, Rendine N, et al. Non-thermal plasma as a novel strategy for treating or preventing viral infection and associated disease. Front Phys. 2021;9:1–25. doi: 10.3389/fphy.2021.683118. [DOI] [Google Scholar]
- Monteil V, Kwon H, Prado P, et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020;181:905–913.e7. doi: 10.1016/j.cell.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreau M, Orange N, Feuilloley MGJ. Non-thermal plasma technologies: new tools for bio-decontamination. Biotechnol Adv. 2008;26:610–617. doi: 10.1016/j.biotechadv.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Moriyama M, Hugentobler WJ, Iwasaki A. Annual review of virology seasonality of respiratory viral infections. Annu Rev Virol. 2020;7:1–19. doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- Morrison C, Atkinson A, Zamyadi A, et al. Critical review and research needs of ozone applications related to virus inactivation: potential implications for SARS-CoV-2. Ozone Sci Eng. 2021;43:2–20. doi: 10.1080/01919512.2020.1839739. [DOI] [Google Scholar]
- Mrkic B, Pavlovic J, Rülicke T, et al. Measles virus spread and pathogenesis in genetically modified mice. J Virol. 1998;72:7420–7427. doi: 10.1128/jvi.72.9.7420-7427.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller NH, Gilden DH, Cohrs RJ, et al. Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency. Neurol Clin. 2008;26:675–697. doi: 10.1016/j.ncl.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mühlemann K. The molecular epidemiology of mumps virus. Infect Genet Evol. 2004;4:215–219. doi: 10.1016/j.meegid.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Muranyi W, Bahr U, Zeier M, Van Der Woude FJ. Hantavirus infection. J Am Soc Nephrol. 2005;16:3669–3679. doi: 10.1681/ASN.2005050561. [DOI] [PubMed] [Google Scholar]
- Mustafa MF, Fu X, Liu Y, et al. Volatile organic compounds (VOCs) removal in non-thermal plasma double dielectric barrier discharge reactor. J Hazard Mater. 2018;347:317–324. doi: 10.1016/j.jhazmat.2018.01.021. [DOI] [PubMed] [Google Scholar]
- Muylaert RL, Bovendorp RS, Sabino-Santos G, et al. Hantavirus host assemblages and human disease in the Atlantic Forest. PLoS Negl Trop Dis. 2019;13:1–19. doi: 10.1371/journal.pntd.0007655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myatt TA, Johnston SL, Zuo Z, et al. Detection of airborne rhinovirus and its relation to outdoor air supply in office environments. Am J Respir Crit Care Med. 2004;169:1187–1190. doi: 10.1164/rccm.200306-760oc. [DOI] [PubMed] [Google Scholar]
- Nayak G, Aboubakr HA, Goyal SM, Bruggeman PJ. Reactive species responsible for the inactivation of feline calicivirus by a two-dimensional array of integrated coaxial microhollow dielectric barrier discharges in air. Plasma Process Polym. 2018;15:1–32. doi: 10.1002/ppap.201700119. [DOI] [Google Scholar]
- Nikitin N, Petrova E, Trifonova E, Karpova O (2014) Influenza virus aerosols in the air and their infectiousness. Adv Virol 201410.1155/2014/859090 [DOI] [PMC free article] [PubMed]
- Nöjd J, Tecle T, Samuelsson A, Örvell C. Mumps virus neutralizing antibodies do not protect against reinfection with a heterologous mumps virus genotype. Vaccine. 2001;19:1727–1731. doi: 10.1016/S0264-410X(00)00392-3. [DOI] [PubMed] [Google Scholar]
- Norrby E, Kristensson K. Measles virus in the brain. Brain Res Bull. 1997;44:213–220. doi: 10.1016/S0361-9230(97)00139-1. [DOI] [PubMed] [Google Scholar]
- Olson MR, Axler RP, Hicks RE. Effects of freezing and storage temperature on MS2 viability. J Virol Methods. 2004;122:147–152. doi: 10.1016/j.jviromet.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Parkkonen P, Hyöty H, Koskinen L, Leinikki P. Mumps virus infects Beta cells in human fetal islet cell cultures upregulating the expression of HLA class I molecules. Diabetologia. 1992;35:63–69. doi: 10.1007/BF00400853. [DOI] [PubMed] [Google Scholar]
- Peate I (1999) Meningitis: causes, symptoms and signs and nursing management. Br J Nurs 8:1290–1296. 10.12968/bjon.1999.8.19.1290 [DOI] [PubMed]
- Pinard L, Ayoub N, Batiot-Dupeyrat C. Regeneration of a coked zeolite via nonthermal plasma process: a parametric study. Plasma Chem Plasma Process. 2019 doi: 10.1007/s11090-019-09972-x. [DOI] [Google Scholar]
- Prussin AJ, Garcia EB, Marr LC. Total concentrations of virus and bacteria in indoor and outdoor air. Environ Sci Technol Lett. 2015;2:84–88. doi: 10.1021/acs.estlett.5b00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puligundla P, Mok C. Non-thermal plasmas (NTPs) for inactivation of viruses in abiotic environment. Res J Biotechnol. 2016;11:91–96. [Google Scholar]
- Reuter D, Schneider-Schaulies J. Measles virus infection of the CNS: human disease, animal models, and approaches to therapy. Med Microbiol Immunol. 2010;199:261–271. doi: 10.1007/s00430-010-0153-2. [DOI] [PubMed] [Google Scholar]
- Rtimi S, Kiwi J. Update on interfacial charge transfer (IFTC) processes on films inactivating viruses/bacteria under visible light: mechanistic considerations and critical issues. Catalysts. 2021;11:1–22. doi: 10.3390/catal11020201. [DOI] [Google Scholar]
- Sakudo A, Misawa T, Shimizu N, Imanishi Y (2014) N2 gas plasma inactivates influenza virus mediated by oxidative stress. Front Biosci - Elit 6 E:69–79. 10.2741/e692 [DOI] [PubMed]
- Sakudo A, Toyokawa Y, Imanishi Y. Nitrogen gas plasma generated by a static induction thyristor as a pulsed power supply inactivates adenovirus. PLoS ONE. 2016;11:1–17. doi: 10.1371/journal.pone.0157922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakudo A, Toyokawa Y, Imanishi Y, Murakami T. Crucial roles of reactive chemical species in modification of respiratory syncytial virus by nitrogen gas plasma. Mater Sci Eng C. 2017;74:131–136. doi: 10.1016/j.msec.2017.02.007. [DOI] [PubMed] [Google Scholar]
- Sauerbrei A. Diagnosis, antiviral therapy, and prophylaxis of varicella-zoster virus infections. Eur J Clin Microbiol Infect Dis. 2016;35:723–734. doi: 10.1007/s10096-016-2605-0. [DOI] [PubMed] [Google Scholar]
- Schiappacasse C, Peng P, Zhou N, et al. inactivation of aerosolized newcastle disease virus with non-thermal. Plasma. 2020;36:55–60. [Google Scholar]
- Schmidt H, Cohrs S, Heinemann T, et al. Sleep disorders are long-term sequelae of both bacterial and viral meningitis. J Neurol Neurosurg Psychiatry. 2006;77:554–558. doi: 10.1136/jnnp.2005.071142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt M, Jo I (2015) Non-thermal plasma based decomposition of volatile organic compounds in industrial exhaust gases. 3745–3754. 10.1007/s13762-015-0814-1
- Schoenbach KH, Joshi RP, Stark RH, et al. Bacterial decontamination of liquids with pulsed electric fields. IEEE Trans Dielectr Electr Insul. 2000;7:637–645. doi: 10.1109/94.879359. [DOI] [Google Scholar]
- Schoenbach KH, Peterkin FE, Alden RW, Beebe SJ. The effect of pulsed electric fields on biological cells: experiments and applications. IEEE Trans Plasma Sci. 1997;25:284–292. doi: 10.1109/27.602501. [DOI] [Google Scholar]
- Scholtz V, Pazlarova J, Souskova H, et al. Nonthermal plasma - a tool for decontamination and disinfection. Biotechnol Adv. 2015;33:1108–1119. doi: 10.1016/j.biotechadv.2015.01.002. [DOI] [PubMed] [Google Scholar]
- Shimizu K, Oda T. Denox process in flue gas combined with nonthermal plasma and catalyst. IEEE Trans Ind Appl. 1999;35:13111317. doi: 10.1109/ias.1997.626324. [DOI] [Google Scholar]
- Su X, Tian Y, Zhou H, et al. Inactivation efficacy of nonthermal plasmaactivated solutions against Newcastle disease virus. Appl Environ Microbiol. 2018;84:1–12. doi: 10.1128/AEM.02836-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun YH, Zhou YX, Jin MJ, et al. New prototype of underwater sound source based on the pulsed corona discharge. J Electrostat. 2005;63:969–975. doi: 10.1016/j.elstat.2005.03.070. [DOI] [Google Scholar]
- Šunka P. Pulse electrical discharges in water and their applications. Phys Plasmas. 2001;8:2587–2594. doi: 10.1063/1.1356742. [DOI] [Google Scholar]
- Tang S, Yuan D, Rao Y, et al. Persulfate activation in gas phase surface discharge plasma for synergetic removal of antibiotic in water. Chem Eng J. 2018;337:446–454. doi: 10.1016/j.cej.2017.12.117. [DOI] [Google Scholar]
- Tellier R. Review of aerosol transmission of influenza A virus. Emerg Infect Dis. 2006;12:1657–1662. doi: 10.3201/eid1211.060426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellier R (2009) Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface 610.1098/rsif.2009.0302.focus [DOI] [PMC free article] [PubMed]
- Tersago K, Verhagen R, Servais A, et al. Hantavirus disease (nephropathia epidemica) in Belgium: effects of tree seed production and climate. Epidemiol Infect. 2009;137:250–256. doi: 10.1017/S0950268808000940. [DOI] [PubMed] [Google Scholar]
- Tersago K, Verhagen R, Vapalahti O, et al. Hantavirus outbreak in Western Europe: reservoir host infection dynamics related to human disease patterns. Epidemiol Infect. 2011;139:381–390. doi: 10.1017/S0950268810000956. [DOI] [PubMed] [Google Scholar]
- Thibaut HJ, Lacroix C, De Palma AM, et al. Toward antiviral therapy/prophylaxis for rhinovirus-induced exacerbations of chronic obstructive pulmonary disease: challenges, opportunities, and strategies. Rev Med Virol. 2016;26:21–33. doi: 10.1002/rmv.1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- To Kelvin KW, Yip CCY, Yuen KY. Rhinovirus – from bench to bedside. J Formos Med Assoc. 2017;116:496–504. doi: 10.1016/j.jfma.2017.04.009. [DOI] [PubMed] [Google Scholar]
- Tregoning JS, Schwarze J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev. 2010;23:74–98. doi: 10.1128/CMR.00032-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung-Thompson G, Libera DA, Koch KL, et al. Aerosolization of a human norovirus surrogate, bacteriophage MS2, during simulated vomiting. PLoS ONE. 2015;10:1–13. doi: 10.1371/journal.pone.0134277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuppeny M. Viral meningitis and encephalitis. Crit Care Nurs Clin North Am. 2013;25:363–380. doi: 10.1016/j.ccell.2013.04.003. [DOI] [PubMed] [Google Scholar]
- Turner RB. Rhinovirus: More than just a common cold virus. J Infect Dis. 2007;195:765–766. doi: 10.1086/511829. [DOI] [PubMed] [Google Scholar]
- U.S. Environmental Protection Agency Green Building Workgroup (2009) Buildings and their Impact on the Environment: A Statistical Summary
- Uytdenhouwen Y, Van Alphen S, Michielsen I, et al. A packed-bed DBD micro plasma reactor for CO2 dissociation: Does size matter? Chem Eng J. 2018;348:557–568. doi: 10.1016/j.cej.2018.04.210. [DOI] [Google Scholar]
- Vohra A, Goswami DY, Deshpande DA, Block SS. Enhanced photocatalytic disinfection of indoor air. Appl Catal B Environ. 2006;64:57–65. doi: 10.1016/j.apcatb.2005.10.025. [DOI] [Google Scholar]
- Volotskova O, Dubrovsky L, Keidar M, Bukrinsky M. Cold atmospheric plasma inhibits HIV-1 replication in macrophages by targeting both the virus and the cells. PLoS ONE. 2016;11:1–9. doi: 10.1371/journal.pone.0165322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang CC, Prather KA, Sznitman J, et al (2021) Airborne transmission of respiratory viruses. Science (80-) 373:. 10.1126/science.abd9149 [DOI] [PMC free article] [PubMed]
- Wang G, Zhu R, Yang L, et al. Non-thermal plasma for inactivated-vaccine preparation. Vaccine. 2016;34:1126–1132. doi: 10.1016/j.vaccine.2015.10.099. [DOI] [PubMed] [Google Scholar]
- Wang H, Li J, Quan X. Decoloration of azo dye by a multi-needle-to-plate high-voltage pulsed corona discharge system in water. J Electrostat. 2006;64:416–421. doi: 10.1016/j.elstat.2005.11.004. [DOI] [Google Scholar]
- Wang H, Li J, Quan X, Wu Y. Enhanced generation of oxidative species and phenol degradation in a discharge plasma system coupled with TiO2 photocatalysis. Appl Catal B Environ. 2008;83:72–77. doi: 10.1016/j.apcatb.2008.02.004. [DOI] [Google Scholar]
- Wang T, Jia H, Guo X, et al. Evaluation of the potential of dimethyl phthalate degradation in aqueous using sodium percarbonate activated by discharge plasma. Chem Eng J. 2018;346:65–76. doi: 10.1016/j.cej.2018.04.024. [DOI] [Google Scholar]
- World Health Organization (2000) The right to healthy indoor air : report on a WHO meeting, Bilthoven, The Netherlands. 15. https://apps.who.int/iris/handle/10665/108327
- World Health Organization (2019) Global influenza strategy 2019–2030. Geneva: 2019. Licence: CC BY-NC-SA 3.0 IGO.Cataloguing-in-Publication (CIP) data.
- Wu Y, Liang Y, Wei K, et al. MS2 virus inactivation by atmospheric-pressure cold plasma using different gas carriers and power levels. Appl Environ Microbiol. 2015;81:996–1002. doi: 10.1128/AEM.03322-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia T, Kleinheksel A, Lee EM, et al (2019) Inactivation of airborne viruses using a packed bed non-thermal plasma reactor. J Phys D Appl Phys 5210.1088/1361-6463/ab1466 [DOI] [PMC free article] [PubMed]
- Xia T, Yang M, Marabella I, et al. Inactivation of airborne porcine reproductive and respiratory syndrome virus (PRRSv) by a packed bed dielectric barrier discharge non-thermal plasma. J Hazard Mater. 2020;393:1–30. doi: 10.1016/j.jhazmat.2020.122266. [DOI] [PubMed] [Google Scholar]
- Xiao Wu, Nethery RC, Benjamin Sabath M, Danielle Braun FD. Exposure to air pollution and COVID-19 mortality in the United States: a nationwide cross-sectional study. Harvard Univ. 2020 doi: 10.1101/2020.04.05.20054502. [DOI] [Google Scholar]
- Xue J, Chen L, Wang H. Degradation mechanism of Alizarin Red in hybrid gas-liquid phase dielectric barrier discharge plasmas: experimental and theoretical examination. Chem Eng J. 2008;138:120–127. doi: 10.1016/j.cej.2007.05.055. [DOI] [Google Scholar]
- Yamashiro R, Misawa T, Sakudo A. Key role of singlet oxygen and peroxynitrite in viral RNA damage during virucidal effect of plasma torch on feline calicivirus. Sci Rep. 2018;8:1–13. doi: 10.1038/s41598-018-36779-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yardimci O, Setlow P. Plasma sterilization: opportunities and microbial assessment strategies in medical device manufacturing. IEEE Trans Plasma Sci. 2010;38:973–981. doi: 10.1109/TPS.2010.2041674. [DOI] [Google Scholar]
- Yasuda H, Miura T, Kurita H, et al. Biological evaluation of DNA damage in bacteriophages inactivated by atmospheric pressure cold plasma. Plasma Process Polym. 2010;7:301–308. doi: 10.1002/ppap.200900088. [DOI] [Google Scholar]
- Zhang Y, Geng X, Tan Y, et al. New understanding of the damage of SARS-CoV-2 infection outside the respiratory system. Biomed Pharmacother. 2020;127:110195. doi: 10.1016/j.biopha.2020.110195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Gamage J (2010) Applications of photocatalytic disinfection. Int J Photoenergy 201010.1155/2010/764870
- Zhou R, Zhou R, Zhang X, et al. Synergistic effect of atmospheric-pressure plasma and TiO2 Photocatalysis on inactivation of escherichia coli cells in aqueous media. Sci Rep. 2016;6:1–10. doi: 10.1038/srep39552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann JL, Dumler K, Shimizu T, et al (2011) Effects of cold atmospheric plasmas on adenoviruses in solution. J Phys D Appl Phys 4410.1088/0022-3727/44/50/505201
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


