Abstract
With the rapid aging of populations, neurologic disorders have become among the leading causes of disability and mortality worldwide. Most neurologic conditions have a prolonged prodromal phase—even if they tend to manifest with an acute syndrome such as stroke—and can lead to a relentless, often deleterious course creating a major burden on patients, caregivers, and society. This unique nature of neurologic diseases signifies the strong need for equally effective primary and secondary prevention strategies and focus on brain health before brain diseases ensue. The field of preventive neurology applies both universal and selective primary prevention strategies to promote brain health both at the public and personal levels. The preventive neurology approach aims to identify and target high-risk individuals and protect them from reaching a critical point where overt clinical symptoms are present and disease progression is irreversible. Universal and selective prevention training, along with dovetailed clinical and public health research, are 3 essential pillars of preventive neurology. The burgeoning field of preventive neurology aims to assess neurologic care needs in a society, promote the participation of neurologists in restructuring of the health care policies to promote brain health, and identify medium- and high-risk individuals to prevent or delay future neurologic events.
Preventive health care has deep roots in the history of medicine. Avicenna (Ibn Sina; 980–1037), founder of early modern medicine, in his influential book The Canon of Medicine puts a major emphasis on prevention of diseases by avoiding external factors leading to sickness.1 In the last century, with the use of vaccines and progress in our knowledge about infectious diseases, the so-called noncommunicable diseases such as stroke and dementia have replaced infectious diseases as the main causes of death and disability worldwide. Throughout the twentieth century, mounting scientific evidence coming from laboratories, clinical settings, and landmark population-based studies, such as the Framingham Heart Study, developed a basis for the identification of “risk factors” for noncommunicable diseases. Following the observational data, multiple clinical trials have shown that control and modification of those risk factors can reduce the burden of noncommunicable conditions.2 In recent decades, these scientific developments have been translated into transformations in clinical care, significantly influenced clinical practice guidelines in various disciplines, and led to major changes in educational activities to familiarize medical students, residents, and fellows with principles of preventive medicine. Such reforms have been more evident in certain fields of medicine such as cardiology where, for instance, a well-structured fellowship program is dedicated to offer training in preventive cardiology.
Burden of Neurologic Disorders and Role of Prevention
Recent data from the United States show that the absolute number of incident cases, prevalent cases, mortality, and disability-adjusted life-years of all neurologic disorders (except for meningitis and encephalitis) have increased. Standalone, the 3 major burdensome neurologic disorders (stroke, Alzheimer disease [AD] and other dementias, and migraine) result in more than 8.5 million disability-adjusted life-years in the United States.3 The economic burden of chronic neurologic diseases is enormous because of long-term and specialized care, and in resource-limited countries, it can endanger financial and political stability of societies. Although the rates of immediate mortality from detrimental neurologic conditions such as stroke have declined, a growing number of individuals live with the sequela of those conditions.4
From Brain Disease to Brain Health
Modern practice of neurology advocates for early and effective interventions after the occurrence and diagnosis of a neurologic condition. However, by the time most neurologic conditions manifest clinically, pathologic changes in the nervous system have already been established and often irreversible. Furthermore, most neurologic conditions are chronic—even if they tend to manifest with an acute syndrome such as stroke—and can lead to a relentless, often deleterious course creating a major burden on patients, caregivers, and society.5 This very specific nature of neurologic diseases highlights the strong need for equally effective primary and secondary prevention strategies. The concept of “brain health” has emerged in recent years with the emphasis on protecting the brain from reaching a critical point where overt clinical symptoms are present and disease progression is irreversible. There is a lack of a unified definition for brain health, and it is sometimes used interchangeably with cognitive health. Brain health is a more comprehensive concept that covers various domains of brain function and endorses the importance of protecting brain structural and functional integrity throughout early, middle, and late life. Maintenance of brain health leads to preservation of thought processing, planned actions, and sensory, motor, and emotional connections, which all positively influence the quality of lives and well-being of individuals, families, and communities.6 Preventive approaches in neurology have immense public health implications. As an example, strong evidence exists that about 40% of dementia cases, one of the most devastating and costly medical conditions globally, can be prevented or delayed by multimodal and feasible risk modification strategies.7 Implementation of such preventive measures requires involvement of highly trained physicians who understand brain function, structure, and vulnerabilities and focus on brain health, and not necessarily brain diseases.
Risk Assessment and Stratification Tools in Neurology
Neurologists may use several validated tools to risk-stratify patients both with and without an established neurologic disorder. Such tools predict risks of developing a disease and/or recurrent events, clinical deterioration, decline in functional status, and mortality, which can assist clinicians in developing individualized approaches for primary, secondary, or tertiary prevention. The Framingham Stroke Risk Score and Functional Outcome in Patients with Primary Intracerebral Hemorrhage Score are 2 clear examples of tools that are applied to predict future risks of primary or secondary neurologic outcomes.8 Early recognition of patients with high-risk sociodemographic, clinical, and biological markers can be obtained through preventive neurology clinics where a dedicated neurologist can evaluate such patients and flag them for long-term risk modification and monitoring. However, at the population level, public education about signs and symptoms and promotion of healthy behaviors can target a broad range of individuals. Educating and caring for patients at risk should be grounded in evidence-based and safe recommendations focused on brain health such as lifestyle modification with diet, exercise, environmental exposures, and control of vascular risk factors (e.g., high blood pressure, high cholesterol, and diabetes). The American Heart Association (AHA) Life's Simple 7 is an example of a well-established measure for brain health assessment and promotion.9
Advantages and Benefits of the Primary Prevention Approach in Neurology
Primary prevention is the science and art of preventing a disease or stopping individuals from being classified at high risk. Universal and selective preventive interventions are 2 key elements of primary prevention. Universal primary prevention targets the general public, whereas selective primary prevention focuses on individuals or subgroups whose risk of developing a disease is significantly higher than average, as evidenced by biological, psychological, or social risk factors. At the population level, neurologists with a preventive approach and requisite knowledge can contribute to public health education and design of health policies and procedures, which will promote brain health. This contribution may safeguard a large number of people at risk from reaching a critical threshold of becoming sick and suffering an irreversible course of neurologic deterioration. Population-level approaches have significant implications not only in reducing the overall burden of neurologic disorders but also in closing gaps in terms of inequalities in awareness, access, and social engagement of different layers of the population. In addition, it needs to be emphasized that public and the patient's education are inseparable parts of a successful approach in primary prevention. At an individual level, preventive neurology clinics and research programs are best poised to identify, assess, and monitor individuals at high risk and apply interventions to promote brain health. In addition, neurologists in their clinical practice can further engage in promoting brain healthy behaviors such as traumatic brain injury prevention and early recognition, sleep hygiene, as well as social and educational engagement. As neurologists, we frequently face family and friends of patients with AD, stroke, Parkinson disease, multiple sclerosis, epilepsy, and several other neurologic conditions who express concerns about their own risks given shared genetic and environmental exposures. One approach to address their concerns can be deferring those questions to primary care physicians. But, a more proactive approach can include a formal evaluation of those individuals while exploring the reason behind their concerns, obtaining a detailed clinical, medical, and family history, neurologic examination, screening tests (guided by history and examination), and, importantly, monitoring for prodromal symptoms before the symptomatic phase begins. Current evidence indicates that life course exposures such as cardiovascular risk factors in young adulthood and middle age, head injury, educational activities, and social engagements are closely linked with later life cerebrovascular and neurodegenerative disorders. Hence, a preventive approach targeting middle age and young adults can have significant implications for brain health in older age. It is worth mentioning that, in addition to the chronologic (calendar) age, the preventive care needs to be customized to the biological age (based on the degree of medical comorbidities, frailty, and genetic predispositions) of individuals, which might better reflect brain vulnerability and the need for earlier interventions. Although a few clinical programs focus on AD risk reduction and brain health, current promising real-world comparative effectiveness data suggest that individualized multidomain care can improve cognitive outcomes and reduce both calculated AD and cardiovascular risk.10
Academic Needs and Proposed Training Structures
In recent years, multiple academic foundations including the American Academy of Neurology (AAN) and AHA/American Stroke Association have endorsed and emphasized the need for focusing on brain health and taking preventive approaches in neurology. This highlights the increasing recognition of the issue by neurologists and a great interest for developing brain health–specific preventive programs. We propose launching preventive neurology fellowship programs, following the successful example of preventive cardiology fellowship, where both newly trained and established neurologists can receive a comprehensive training in primary and secondary prevention of neurologic disorders with the emphasis on the promotion of brain health over the life course. To this end, an outline of the key elements of an educational model for training physicians who are specialized in preventive neurology and can therefore serve as brain health experts is presented (Figure). The burgeoning field of preventive neurology aims to close the gap between the growing burden of neurologic disorders and the overall population brain health.
Figure. Key Elements of an Educational Model for Preventive Neurology Training Program.
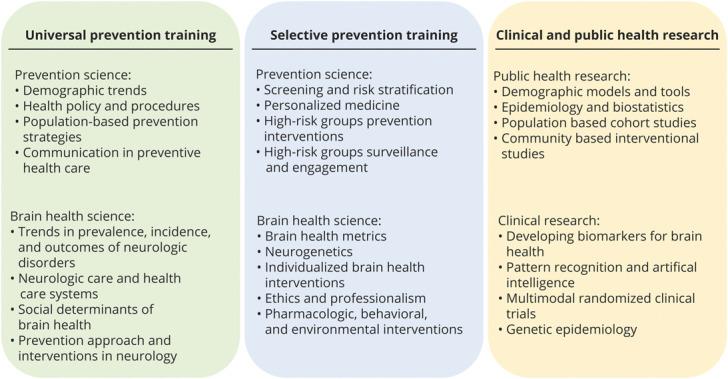
The 3 key elements of a preventive neurology program include training in universal and selective preventive health care and proficiency in public and clinical research. The universal preventive training familiarizes the trainees with national and global demographic and epidemiologic trends and procedures and subsequently focuses on brain health–specific issues with the goal to prepare the trainee as an independent expert in situation analysis and health policy making. The selective program familiarizes the trainees with principles and concepts of high-risk group recognition and will enable the trainees to establish brain health clinics for evaluation, monitoring, and management of high-risk individuals. The research program will equip the trainees with research tools to conduct brain health–oriented studies with the goal to advance the field and develop novel diagnostic, prognostic, and therapeutic interventions. The length of such training program can be 1–2 years depending on the duration of the research training section.
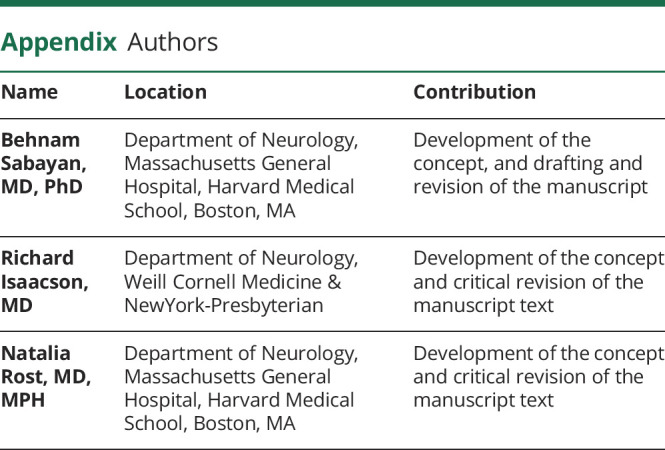
Appendix. Authors
Study Funding
The authors report no targeted funding.
Disclosure
B.S., R.I., and N.R. report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Zargaran A, Mehdizadeh A, Zarshenas MM, Mohagheghzadeh A. Avicenna (980–1037 AD). J Neurol. 2012;259(2):389-390. [DOI] [PubMed] [Google Scholar]
- 2.Ezzati M, Riboli E. Can noncommunicable diseases be prevented? Lessons from studies of populations and individuals. Science. 2012;337(6101):1482-1487. [DOI] [PubMed] [Google Scholar]
- 3.Collaborators GUND; Feigin VL, Vos T, Alahdab F, et al. Burden of neurological disorders across the US from 1990–2017: a global burden of disease Study. JAMA Neurol. 2020;78(2):165-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hewer RL. The economic impact of neurological illness on the health and wealth of the nation and of individuals. J Neurol Neurosurg Psychiatry. 1997;63(suppl 1):S19-S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collaborators GBDN. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorelick PB, Furie KL, Iadecola C, et al. Defining optimal brain health in adults: a presidential advisory from the American Heart Association/American Stroke Association. Stroke. 2017;48(10):e284-e303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rost NS, Smith EE, Chang Y, et al. Prediction of functional outcome in patients with primary intracerebral hemorrhage: the FUNC score. Stroke. 2008;39(8):2304-2309. [DOI] [PubMed] [Google Scholar]
- 9.Sacco RL. Achieving ideal cardiovascular and brain health: opportunity amid crisis: presidential address at the American Heart Association 2010 scientific sessions. Circulation. 2011;123(22):2653-2657. [DOI] [PubMed] [Google Scholar]
- 10.Isaacson RS, Hristov H, Saif N, et al. Individualized clinical management of patients at risk for Alzheimer's dementia. Alzheimers Dement. 2019;15(12):1588-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]


