Abstract
We aimed to compare the association of depression with aspects of quality of life (QoL) among older people users of primary health care (PHC) living in Brazil and Portugal.
We carried out an observational, cross-sectional and comparative study with a quantitative approach in the PHC scope in Brazil and Portugal, where we obtained a nonrandom sample of 150 participants aged 65 years or older (100 Brazilians and 50 Portuguese). We used the socioeconomic and health data questionnaire, the Medical Outcomes Short-Form Health Survey QoL (SF-36) questionnaire and the Beck Inventory.
Among the socioeconomic profiles, most were females aged between 65 and 80 years in both countries. There was a significant difference between groups in the income variable, with 100.0% of Portuguese people earning up to 1 minimum wage (P value <.001), and the presence of chronic diseases in 92.0% of respondents in Portugal (P value = .033). In the association analysis, most aspects of QoL had a higher median score (>50.0) within the categorical variables of “absent” and “mild” depression. The Emotional role functioning, Physical role functioning, Physical functioning, Mental health, Total score domains and the Mental health and Physical health summary measures stood out with this behavior in Brazil and in Portugal, where these latter 2 presented moderate to strong correlation values (ρ > 0.400) in Portugal. Greater associations of depression on QoL were revealed in Portugal than in Brazil. Among their most expressive associations, the Physical role functioning (odds ratio [OR] = 4.776; 95.0% confidence interval [CI]: 2.41–9.43), Physical functioning (OR = 3.037; 95.0% CI: 3.037), Vitality (OR = 6.000; 95.0% CI: 1.56–23.07) and Total score (OR = 3.727; 95.0% CI: 2.24–6.17) domains and the Mental health summary measure (OR = 3.870; 95.0% CI: 2.13–7.02) stood out.
Aspects related to the emotional, physical, functional and mental health components stood out. The association and correlation with depression were more expressive in Portugal compared to Brazil. However, similar results were obtained in Brazil but with less relevance.
Keywords: aged, depression, mental disorders, primary health care, quality of life
1. Introduction
Listed as one of the most frequent mental disorders in the world,[1,2] depression manifests itself as causing social isolation and physical and mental distress and can culminate in self-destructive behaviors, thus greatly impacting different aspects of people's lives.[3] Given its relevance as a public health problem,[1,4] the negative impact of depression on quality of life (QoL)[1,5,6] and its worsening with age are notable.[7] Depression is also more prevalent among older people individuals than younger individuals and has developed different clinical manifestations, making its diagnosis and treatment difficult.[4] Depression affects more than 121 million people worldwide; it was the fourth largest global cause of illness in 2000 and is projected to become the second most prevalent illness in the coming years.[8]
Although the relationship between depression and QoL has been proven,[1,2] there is much to be studied on the subject, given the complexity that permeates QoL. The World Health Organization conceptualizes QoL as the individual's understanding of his or her roles in life, in a cultural context, values and their relationship with goals, expectations, standards and concerns.[9]
Therefore, we should emphasize the relevance of screening and adequate follow-up of depression and QoL by structured health services, whose strategies should become effective, successful and efficient.[10] Brazil, whose primary health care (PHC) system has universal, equal and equitable access, is aiming to accomplish these goals, since its health service is designed to meet at least 80.0% of the population's health demands, with a mostly preventive approach.[11,12] Nevertheless, existing data have revealed a high prevalence of physical and mental health problems, mainly associated with failures in the screening, reception and treatment process at this health care level.[13] In 2015, it was estimated that 20.0% of the older people population in Brazil had mental or neurological disorders in addition to an increase in the coefficient of mortality from mental health problems between 2008 and 2014, even with decreasing hospitalization levels for the same reason.[14] According to the 2019 Brazilian National Health Survey, 10.2% of Brazilians were diagnosed with depression. Among them, older people citizens had the highest prevalence.[15]
Portugal, which is similar to the Brazilian scenario in the epidemiological aspects of chronic and mental illnesses, has a PHC that was better assessed in relation to Brazil, standing out for its accessibility, with a focus on preventive and follow-up action.[16,17] The National Health Survey in Portugal, carried out in 2019, showed that 24.3% of individuals over 65 years of age had some level of depression.[18] Of note, Portugal, as well as several countries in the European bloc, has a population age pyramid with a large presence of older people, as it follows the high life expectancy in the country.[19] Further, more than 70.0% of young Portuguese people have some healthy lifestyle activity, such as the practice of regular physical exercise, a habit strongly associated with the prevention of psychological disorders. However, there was a progressive percentage drop in these data as the age group increased.[20]
Even with the availability of these findings, new knowledge about the different environments in which older people with depressive disorders live raises questions about the possible impacts of depression on each aspect of QoL and whether there are different levels of this influence among different countries and cultures.[21] This scientific gap exerts the potential to offer subsidies in the field of PHC, in the prevention of mental disorders, as well as maintenance and improvement of QoL by diagnosing which of its aspects are most impacted by depression among older people citizens in the Brazilian and Portuguese contexts. It is also believed that PHC is the public health device with the greatest potential for preventing and following geriatric depression. Therefore, this study carried out an assessment of this population living in these 2 countries with different socioeconomic and cultural backgrounds.
We aimed to compare the association of depression with aspects of QoL among older people PHC users living in Brazil and Portugal. We hypothesized that the presence of depression is associated with worsening QoL at different levels.
2. Materials and methods
2.1. Design
This was an observational, cross-sectional and comparative study with a quantitative approach carried out in Brazil and Portugal as part of an international project. The study was assessed and approved in Brazil by the Research Ethics Committee of the Onofre Lopes University Hospital (registration n° 562.318), in Portugal by the Research Ethics Committee of the University of Évora (registration n° 14011) and by the Ethics Committee for Scientific Research in the Areas of Health and Human Well-Being of the University of Évora (registration n° 17.006/2018). Before each data collection, the participants were duly informed about the objectives, data collection instruments and the importance of the study, with caveats about the risks and benefits. Participants then signed the informed consent form as a way of accepting the precepts used in the study and authorizing the use of the information provided for scientific purposes. The research was conducted in accordance with the Declaration of Helsinki at all times and respecting the principles of good clinical practice.
2.2. Study place and population
In Brazil, the research was developed in the units of the Family Health Strategy in the cities of Natal and Santa Cruz, both in the state of Rio Grande do Norte. In Portugal, the study was conducted in older people health services in the coverage area of the family health units of continued primary care in Eborae, Plaicie and Salus, which are linked to the Regional Health Council of the Évora Council, as well as in the older people care services provided at the University of Évora.
A nonrandom sample of participants was selected for convenience due to the difficult geographic access to reach the homes of some participants and the nonauthorization of data collection within the health units of the PHC in Évora. For this reason, the participants included those who received regular direct care (with at least 1 monthly service) and who met the study's inclusion criteria. Thus, for Brazil, we considered the population within the areas covered by the PHC services (n = 135) (Natal and Santa Cruz/Rio Grande do Norte); for Portugal (n = 60, 95% confidence level and 5% error margin), we considered those within the units of the services surveyed in the Évora Council. The sample calculation was performed with n = 100 and 60 participants, whose result was obtained with the help of an online calculator (https://calculareconverter.com.br/calculo-amostral).
The Brazilian participants were surveyed first, which enabled us to use their collected information as a baseline for the study and as a comparative structure with the participants from Portugal. To eliminate possible confounding factors generated by differences between these countries, we grouped the socioeconomic profiles of Brazilians using the following variables: gender (male or female), age group (65–80 or 81–100 years), marital status (married/cohabitating or single/widowed/divorced), chronic diseases (presence or absence) and family income in minimum wages (≤1 or >1). Each set of 5 variables constituted a representative code that, in turn, was assigned to each of the participants. In other words, each participant with the same combination of socioeconomic status was represented by a code. For each code, we established that there should be at least 1 individual from each country. Therefore, codes that were not represented by at least 2 participants (1 from Brazil and 1 from Portugal) were discarded.
The inclusion criteria adopted for the study were: being 65 years old or more, an age criterion established by the WHO to be considered older people;[22] being registered in the PHC in your research scenario (Brazil/Portugal) for at least 6 months before the study was completed; and presenting an uncompromised cognitive state that enabled participants to understand all instruments (this criterion was assessed using the Mini-Mental State Examination [MMSE]; participants had to score 17 points or more on the scale for inclusion in the study).[23] The following exclusion criteria were adopted: permanent or transitory physical disability at the time of data collection and personal or family trauma reported by the participant in a period less than or equal to 6 months prior to the time of the research.
2.3. Instruments and variables
We used the following instruments: questionnaire with socioeconomic and health data containing categorized responses (age, gender, schooling, family income and marital status, presence or absence of chronic diseases); the Medical Outcomes Short-Form Health Survey QoL (SF-36) questionnaire; The MMSE; and the Beck Inventory.
The SF-36, validated in Brazil and Portugal, has 36 questions on a Likert scale that measure the participant's feelings of health, physical and emotional limitations and expectations about their health. It is graded by intensity levels, with their metrics scores ranging from 0 to 100 (0.0–100.0) in each of its aspects divided into domains (Emotional role functioning, Physical role functioning, Physical functioning, Mental health, Vitality, Social role functioning, General health perceptions, Pain and Total score) and summary measures (Mental health and Physical health).[24] To enable categorical association analyses, the score for each aspect was classified as “best” when its score >50.0 and “worst” when ≤50.0.
We used the MMSE questionnaire[23] as a cognitive screening tool through tests of calculations, drawings and logical reasoning and counting the performance levels in the test through scores. The Beck Inventory[25] was validated and adapted for the Portuguese language[26] and used to measure the depression levels through a score obtained by considering 21 groups of statements, among which the participant selected the response that most identified his or her thoughts. The content of each set of testimonies/responses concerns various themes, such as sadness, personal interaction when living with people, interest in sex, sleep, appetite and suicidal ideation, measured through numerically categorized response levels and generating a score that classifies the depression levels among the categorical variables: “absent,” “mild,” “moderate,” and “severe”.[27] To compose the odds ratio (OR) analysis, the scale was recategorized between “absent” and “present” depression (mild + moderate + severe).
2.4. Data collection and availability
In Brazil, data collection was carried out by undergraduate nursing students and Master's and doctoral students in health sciences, including nurses, nutritionists and physiotherapists. In Portugal, data were collected by scholarship holders from the Master's programs from the University of Évora and researchers in a postdoctoral stage, in addition to some of the Brazilian participants who travelled to Portugal to help with data collection. There was prior training of the teams from both countries in the application of the questionnaires, and the training team performed this procedure without remuneration.
Data collection took place between December 2017 and July 2018, with a mean duration of 1 hour for each interview. Interviews were conducted in-person between researcher and participant, with questions guided by the selected instruments. The first collection stage was held in Brazil, where there was an active search for participants with the collaboration of community health workers and nurses from the areas covered by PHC. Participants were contacted by the address provided in the PHC services. With those who agreed to participate, days and times were scheduled for the interviews. In the second stage, held in Portugal, data collection took place at the Senior University of Évora and at the Elderly's Day Center in the parish of N. Sra. de Fátima, Eborae, Planicie and Salus, which are linked to the regional health council of Évora, members of the National Health System (NHS). The interviews took place individually in the participants’ homes and/or in the spaces of the university and listed health services. There was no blinding of any of the research participants.
The data sets generated during our study are available in the Mendeley Data repository and can be accessed via the link https://data.mendeley.com/datasets/nm8vr4rbp6/1.
2.5. Data analysis and treatment
To accomplish the treatment and tabulation of data in tables, we used Microsoft Excel 2016 (Microsoft Corporation, Washington, WA, USA). Statistical Package for the Social Sciences, version 20.0 (International Business Machines Corporation, Armonk, NY, USA) was used for all statistical analyses. The Shapiro–Wilk test measured the non-normality of the sample. We used nonparametric descriptive tests (Pearson's Chi-Squared and Fisher exact test) for socioeconomic and health data to analyse the isonomy level between the 2 research groups. We used the Mann–Whitney U test and Pearson's Chi-Squared test, respectively, for the analyses of associations of the Medical Outcomes Short-Form Health Survey QoL (SF-36) scale (expressed in 25th, 50th, and 75th percentiles) and Beck depression levels with the study sites. To determine the association between the SF-36 median score and each depression level in the Beck Inventory, we used the Kruskal–Wallis test. The SF-36 domains and summary measures that obtained statistical significance, considering the absence of depression, were selected and submitted to Spearman's rho correlation test (ρ), adopting the following levels: weak (ρ < 0.400), moderate (ρ = 0.400–0.499) and strong (ρ > 0.499) to measure its correlation level with the Beck Inventory. For the bivariate analysis of the SF-36 Scale (Worst ≤50.0/Best >50.0) with the Beck Inventory in its dichotomous presentation (Absent/Present), to check if the odds ratio (OR) of depression is related to Worst QoL, we considered the parameter of OR ≥1.000. The dichotomous categorization of the SF-36 was adopted since the nonnormality of its variables was identified. The confidence interval (CI) 95.0% was adopted, and we considered results with a P value ≤.050 to be statistically significant.[28]
3. Results
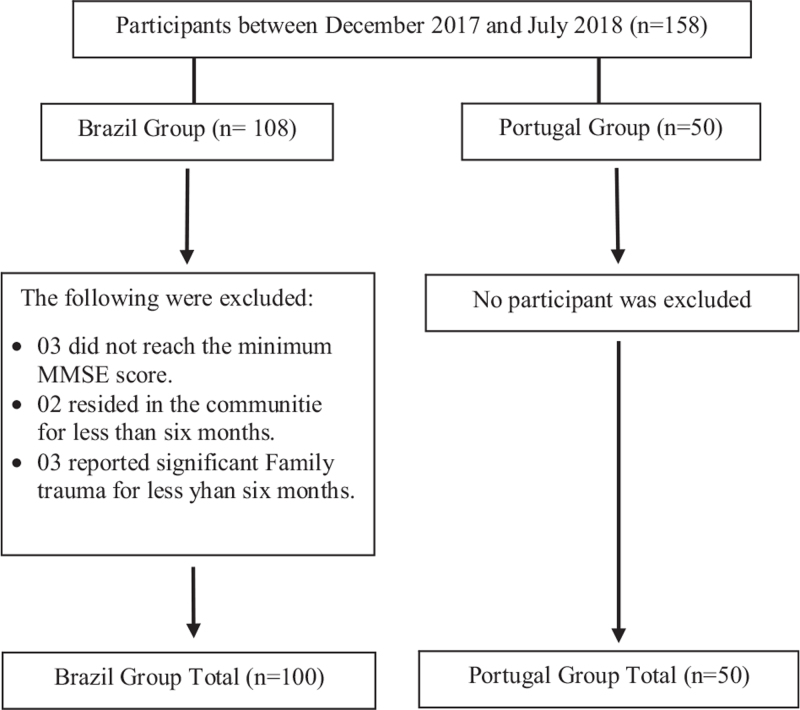
The sample consisted of 150 individuals, including 100 Brazilians and 50 Portuguese. In addition, individuals were approached and excluded in Brazil according to the exclusion criteria. In Portugal, no participants were excluded. The flowchart of the sample selection process is shown in Figure 1.
Figure 1.
Flowchart depicting consecutive participants and reasons for exclusion from the present study.
The socioeconomic profiles of both countries (Table 1) were proportionally different. Even with pairing through the combinations of the profile codes, there was a significant difference between the participants of both scenarios, as in the case of the income variable, with 100.0% of Portuguese people earning up to 1 minimum wage (P value <.001), and the presence of chronic diseases in 92.0% of respondents in Portugal (P value = .033). Despite the significant predominance (P value = .001) of Brazilians who did not live alone (86.0%) and schooling (predominance of 79.0% among Brazilians with up to 5 years of schooling, P value = .001), these variables did not constitute the criteria for pairing the study groups. However, they represent an important difference between the contexts of both scenarios.
Table 1.
Socioeconomic characterization and its association between Brazil and Portugal.
| Brazil (n = 100) | Portugal (n = 50) | ||||
| Variable | n | % | n | % | ∗P value |
| Sex | |||||
| Female | 73 | 73.0 | 41 | 82.0 | .311 |
| Male | 27 | 27.0 | 29 | 58.0 | |
| Age range, yr | |||||
| 65–80 | 89 | 89.0 | 43 | 86.0 | .602 |
| 81–100 | 11 | 11.0 | 7 | 14.0 | |
| Marital status | |||||
| Married/cohabitating | 49 | 49.0 | 28 | 56.0 | .489 |
| Single/ widowed/ divorced | 51 | 51.0 | 22 | 44.0 | |
| Educational attainment, years | |||||
| ≤5 | 79 | 79.0 | 26 | 52.0 | .001 |
| >5 | 21 | 21.0 | 24 | 48.0 | |
| Live alone | |||||
| Yes | 14 | 14.0 | 19 | 38.0 | .001 |
| No | 86 | 86.0 | 31 | 62.0 | |
| Household income, ∗∗∗minimum wage | |||||
| ≤1 | 42 | 42.0 | 50 | 100.0 | ∗∗ <.001 |
| > 1 | 58 | 58.0 | - | - | |
| Chronic Diseases | |||||
| Yes | 79 | 79.0 | 46 | 92.0 | ∗∗ .033 |
| No | 21 | 21.0 | 4 | 8.0 | |
Pearson's Chi-Squared test.
Fisher exact test.
Minimum wage, R$ 954.00 (BRL) in Brazil/ €618.00 (EUR) in Portugal (2018).
Table 2 presents the assessments of each aspect, distributed within the percentiles, and their association between the measured research sites. The Physical functioning (P value = <.001), Social role functioning (P value = .022), General health perceptions (P value = .043) and Total score (P value = .006) domains presented statistical significance, as well as the Physical health (P value <.001) summary measure. Similarly, Table 3 shows the comparison between both research sites, scaled across the 4 depression levels in the Beck Inventory. Attention was drawn to the absence of severe depression among Portuguese participants. Therefore, lower depression levels in Portugal stood out (P value = .042).
Table 2.
Association of quality of life between Brazil and Portugal.
| Brazil (n = 100) | Portugal (n = 50) | ||||||
| QoL (SF-36) | P∗ 25 | P 50 | P 75 | P 25 | P 50 | P 75 | ∗∗P value |
| Domains | |||||||
| Emotional role functioning | 33.3 | 100.0 | 100.0 | 66.7 | 100.0 | 100.0 | .359 |
| Physical role functioning | 35.0 | 67.5 | 90.0 | 50.0 | 75.0 | 90.0 | .174 |
| Physical functioning | 0.0 | 50.0 | 100.0 | 75.0 | 100.0 | 100.0 | <.001 |
| Mental Health | 52.0 | 56.0 | 60.0 | 48.0 | 56.0 | 64.0 | .332 |
| Vitality | 45.0 | 50.0 | 60.0 | 43.7 | 50.0 | 56.2 | .348 |
| Social role functioning | 50.0 | 50.0 | 50.0 | 37.5 | 50.0 | 50.0 | .022 |
| General health perceptions | 30.0 | 35.0 | 55.0 | 35.0 | 50.0 | 56.2 | .043 |
| Pain | 20.0 | 40.0 | 60.0 | 20.0 | 30.0 | 40.0 | .076 |
| Total score | 44.2 | 55.0 | 61.0 | 53.9 | 60.8 | 63.9 | .006 |
| Summary Measures | |||||||
| Mental health | 47.2 | 57.0 | 61.0 | 49.9 | 58.3 | 61.9 | .235 |
| Physical health | 40.0 | 50.0 | 57.0 | 49.7 | 57.0 | 63.0 | <.001 |
Percentile.
Mann–Whitney U test.
Table 3.
Assessment of depression levels in Brazil and Portugal.
| Brazil (n = 100) | Portugal (n = 50) | ||||
| Depressive Symptoms (Beck Inventory) | n | % | n | % | ∗P value |
| Absent | 54 | 54.0 | 30 | 60.0 | |
| Light | 33 | 33.0 | 12 | 24.0 | |
| Moderate | 6 | 6.0 | 8 | 16.0 | .042 |
| Severe | 7 | 7.0 | - | - | |
Pearson's Chi-Squared test.
Table 4 highlights the association between depression levels and the median QoL score within each of the scenarios. In both, it is possible to note that most aspects of QoL had a higher median score (>50.0) within the categories of absent and Mild Depression compared to the medians of scores at the Moderate and Severe levels.
Table 4.
Association between quality of life medians and depression levels.
| ∗Depressive symptoms (Beck inventory) | ||||||||
| Brazil (n = 100) | Portugal (n = 50) | |||||||
| QoL (SF-36) | A | L | M | S | A | L | M | P value∗∗ |
| Domains | ||||||||
| Emotional role functioning | 100.0 | 100.0 | 16.7 | 0.0 | 100.0 | 100.0 | 33.4 | <.001 |
| P value∗∗ | .001 | .005 | ||||||
| Physical role functioning | 80.0 | 35.0 | 62.5 | 20.0 | 85.0 | 52.5 | 30.0 | <.001 |
| Pvalue | <.001 | <.001 | ||||||
| Physical functioning | 87.5 | 25.0 | 75.0 | 0.0 | 100.0 | 100.0 | 87.5 | <.001 |
| p-value | .005 | .059 | ||||||
| Mental Health | 60.0 | 56.0 | 54.0 | 48.0 | 60.0 | 48.0 | 48.0 | <.001 |
| P value | .001 | .046 | ||||||
| Vitality | 50.0 | 50.0 | 57.5 | 50.0 | 55.0 | 45.0 | 45.0 | .003 |
| P value | .062 | .002 | ||||||
| Social role functioning | 50.0 | 50.0 | 50.0 | 50.0 | 50.0 | 43.8 | 37.5 | .031 |
| P value | .917 | .02 | ||||||
| General health perceptions | 35.0 | 45.0 | 55.0 | 65.0 | 47.5 | 45.0 | 60.0 | <.001 |
| P value | .001 | .024 | ||||||
| Pain | 30.0 | 40.0 | 50.0 | 70.0 | 20.0 | 45.0 | 45.0 | <.001 |
| P value | <.001 | <.001 | ||||||
| Total Score | 58.5 | 49.0 | 50.0 | 40.0 | 61.9 | 55.4 | 47.1 | <.001 |
| P value | .001 | .069 | ||||||
| Summary Measures | ||||||||
| Mental health | 58.0 | 50.0 | 45.0 | 45.0 | 60.9 | 48.2 | 49.7 | <.001 |
| P value | .109 | .005 | ||||||
| Physical health | 54.0 | 41.0 | 59.0 | 42.0 | 59.0 | 52.0 | 50.5 | <.001 |
| P value | .007 | .025 | ||||||
Depression levels (A: Absent; L: Light; M: Moderate e S: Severe).
Kruskal–Wallis Association Test.
Among these aspects of QoL, the Emotional role functioning (P value = 001), Physical role functioning (P value < .001) and Physical functioning (P value = .005); Mental health (P value = .001); and Total score (P value = .001) domains stood out in Brazil with this behaviour, as well as the Physical health (P value = .007) summary measure. In Portugal, the Emotional role functioning (P value = .005), Physical role functioning (P value < .001), Mental health (P value = .046), and Vitality (P value = .002) domains, as well as the Mental health (P value = .005) and Physical health (P value = .025) summary measures stood out.
To refine the analyses for testing the study hypothesis, we selected the domains and summary measures that stood out in this context (excluding the others) for correlation analysis (Table 5).
Table 5.
Correlation of quality of life and depression.
| Depressive symptoms (Beck inventory) | ||||
| Brazil (n = 100) | Portugal (n = 50) | |||
| QoL (SF-36) | ρ∗ | ∗∗p-value | ρ | P value |
| Domains | ||||
| Emotional role functioning | −0.356 | <.001 | −0.510 | <.001 |
| Physical role functioning | −0.455 | <.001 | −0.673 | <.001 |
| Physical functioning | −0.284 | .004 | −0.468 | .001 |
| Mental health | −0.330 | .001 | −0.362 | .01 |
| Vitality | 0.052 | .604 | −0.500 | <.001 |
| Total score | −0.374 | <.001 | −0.574 | <.001 |
| Summary Measures | ||||
| Mental health | −0,374 | <.001 | −0.593 | <.001 |
| Physical health | −0,244 | .014 | −0.447 | .001 |
Rô Test Parameters (ρ) (Weak: ρ < 0.400; Moderate: ρ = 0.400-0.490; Strong: ρ > 0.490).
Spearman's correlation.
In all selected aspects of QoL (SF-36), the correlation with the Beck Inventory score was negative, with the exception of the Vitality domain in Brazil (ρ = 0.052/P value = .604).
Additionally, in Brazil, the physical role functioning domain was the only domain with moderate correlation (ρ = −0.455/P value < .001), while all other aspects of QoL showed a weak correlation. In the Portuguese sample, only the Mental health domain showed a weak correlation (ρ = −0.362/P value = .01). All aspects showed statistical significance in their correlation with depression.
The same aspects of QoL selected to measure the correlation with depression were categorized and crossed with the depression variables (Absent/Present), as shown in Table 6. The OR was measured to check the association of the presence of depression in individuals with worse QoL (SF-36 ≤50.0).
Table 6.
Odds ratio for quality of life and depression.
| Depressive symptoms (Beck inventory) | ||||||||
| Brazil (n = 100) | Portugal (n = 50) | |||||||
| Absent | Present | Absent | Present | |||||
| QoL (SF-36) | n (%) | n (%) | ∗OR | ∗CI (95%) | n (%) | n (%) | OR | CI (95%) |
| Domains | ||||||||
| Emotional role functioning | ||||||||
| Better | 45 (45.0) | 23 (23.0) | 2.125 | 1.42–3.16 | 29 (58.0) | 11 (22.0) | 3.273 | 1.90–5.63 |
| Worse | 9 (9.0) | 23 (23.0) | 1 (2.0) | 9 (18.0) | ||||
| Physical role functioning | ||||||||
| Better | 44 (44.0) | 17 (17.0) | 2.668 | 1.71–4.15 | 29 (58.0) | 7 (14,0) | 4.776 | 2.41–9.43 |
| Worse | 10 (10.0) | 29 (29.0) | 1 (2.0) | 13 (26.0) | ||||
| Physical functioning | ||||||||
| Better | 33 (33.0) | 15 (15.0) | 1.908 | 1.18–3.06 | 29 (58.0) | 12 (24.0) | 3.037 | 1.79–5.15 |
| Worse | 21 (21.0) | 31 (31.0) | 1 (2.0) | 8 (16.0) | ||||
| Mental Health | ||||||||
| Better | 51 (51.0) | 32 (32.0) | 2.136 | 1.50–3.03 | 24 (48.0) | 9 (18.0) | 2.373 | 1.22–4.58 |
| Worse | 3 (3.0) | 14 (14.0) | 6 (12.0) | 11 (22.0) | ||||
| Vitality | ||||||||
| Better | 23 (23.0) | 22 (22.0) | 0.893 | 0.58–1.36 | 18 (36.0) | 2 (4.0) | 6.000 | 1.56–23.07 |
| Worse | 31 (31.0) | 24 (24.0) | 12 (24.0) | 18 (36.0) | ||||
| Total Score | ||||||||
| Better | 44 (44.0) | 21 (21.0) | 2.211 | 1.46–3.33 | 30 (60.0) | 11 (22.0) | 3.727 | 2.24–6.17 |
| Worse | 10 (10.0) | 25 (25.0) | - | 9 (18.0) | ||||
| Summary Measures | ||||||||
| Mental Health | ||||||||
| Better | 44 (44.0) | 21 (21.0) | 2.211 | 1.46–3.33 | 29 (58.0) | 9 (18.0) | 3.870 | 2.13–7.02 |
| Worse | 10 (10.0) | 25 (25.0) | 1 (2.0) | 11 (22.0) | ||||
| Physical health | ||||||||
| Better | 32 (32.0) | 16 (16.0) | 1.731 | 1.08–2.75 | 27 (54.0) | 10 (20.0) | 2.846 | 1.55–5.22 |
| Worse | 22 (22.0) | 30 (30.0) | 3 (6.0) | 10 (20.0) | ||||
Odds Ratio (Confidence Interval 95.0%) for cohort of Present Depression in Worst QoL (SF-36 ≤ 50.0).
This analysis revealed higher associations of depression with QoL in Portugal than in Brazil. Among its most expressive associations, the worst assessment of QoL was in the Physical role functioning (OR = 4.776; 95.0% CI: 2.41–9.43), Physical functioning (OR = 3.037; 95.0% CI: 3.037), Vitality (OR = 6.000; 95.0% CI: 1.56–23.07), and Total score (OR = 3.727; 95.0% CI: 2.24–6.17) domains, as well as in the Mental health (OR = 3.870; 95.0% CI: 2.13–7.02) summary measure. Brazil also presented high associations with the Emotional role functioning (OR = 2125; 95.0% CI: 1.42–3.16), Physical role functioning (OR = 2.668; 95.0% CI: 1.71–4.15), Mental health (OR = 2.136; 95.0% CI: 1.50–3.03) and Total score (OR = 2.211; 95.0% CI: 1.46–3.33) domains, as well as in the Mental health (OR = 2.211; 95.0% CI: 1.46–3.33) summary measure.
4. Discussion and conclusions
4.1. Evidence found
This study showed the presence of moderate to strong associations and correlations between domains and summary measures related to emotional, physical and emotional components with depression. There was also a higher association with depression when scores were poor. Comparatively, Portugal stood out with more expressive association and correlation values in relation to Brazil. The findings as a situational diagnosis can serve as a basis for the formulation of new health policies and tools within the PHC scope of different countries, even though they do not have external validity power. They also help fill the gaps regarding studies that approach the association of depression with QoL. Understanding its degree of interference is extremely relevant to provide support and consistency in strategies to prevent mental disorders and maintain the autonomy of the older people, especially when considering the cultural and socioeconomic factors with which PHC teams deal.[16,17]
When comparing the socioeconomic profiles of the 2 countries, even with pairing variables, we found significant differences in schooling, whether they lived alone at home, family income and presence/absence of chronic diseases. The relationship between depression and QoL can be explained by these differences, as other studies have shown that better socioeconomic and health conditions are strongly associated with better QoL[29] and lower depression levels.[30] Among the variables that showed significant differences, the longest schooling period was proportional to Portuguese. In Brazil, there was higher income, more people sharing their homes with others and a lower presence of chronic diseases. Although numerically these data suggest a better condition among Brazilians, it is pertinent to question whether the greater economic power in relation to the currency, greater autonomy of life and better screening of diseases by PHC among the Portuguese constitute a counterpoint to these findings.[16,17] Alternatively, the fact that most Portuguese live alone does not imply a risk for worsening depressive disorders, as already noted in the literature.[31]
The descriptive analysis of QoL revealed that the aspects related to physical, functional, mental and emotional health stood out the most in relation to their performance. We found higher scores in the Portuguese scenario, where lower depression levels were noted and presented as the only group without severe depression. A possible explanation for these findings lies in the benefits already evidenced of the maintenance and preservation of physical capacity in emotional aspects,[32] in addition to being mitigating factors for depressive symptoms when the individual has healthy lifestyle habits.[33]
Among the results of the association, Portugal stood out. The Emotional role functioning, Physical role functioning and Physical functioning domains stood out, as well as the Mental health and Physical health summary measures. We should emphasize that these domains are assessed according to the individual's autonomy and physical capacity,[24] which are important predictors of better QoL scores in several studies and regardless of the cultural scenario.[34–36] In Taiwan, the emotional support received and the social interaction/conviviality of the older people within his or her community also stood out as important protective factors for depressive crises.[37] Regarding physical health and functionality, other findings highlight that the focus on physical activities potentially contributes to the autonomy and resilience of older people in their basic activities of life, which are consistently associated with their mental health.[5,34] The fact that an older people can independently carry out activities, such as bank payments, moving around the city or preparing his or her own meals, directly impacts his or her self-perception of mental health.[38]
The association with depression was also more expressive in the Portuguese group in all assessed aspects of QoL (excluding those without association in the descriptive analysis), although in Brazil, the association was also present in almost all aspects. The only domain where a difference in the association with depression was noted was vitality. Interestingly, Brazilians did not present association, while in Portugal, it was the domain where its most relevant value was noted. Regarding vitality, it is noteworthy that its measurement in the SF-36 refers to the individual's energy and fatigue levels.[24] With advancing age, feeling fatigued and lacking energy much of the time is increasingly common and is related to sleep fragmentation, commonly seen in long-lived older people individuals.[39] Despite this, in our results, the older people over 80 years old citizens formed a minority within both groups and had very similar representations. There was no stratification of the age group with the greatest number of categories, which could allow more consistent conclusions to be drawn.
To work precisely on the aspects highlighted among our findings, multidimensional interventions have already shown improvement in depression and QoL in older people individuals when tested within the Brazilian PHC scope, as they focused on activities to encourage physical autonomy, social interaction and emotional support.[40] However, for strategies to be effective, the target aspects must be well delineated, measured and worked on by professionals truly committed to establishing strong ties with the community.[41,42]
4.2. Cultural and public health implications
Identifying solutions for complex health demands is a constant challenge in any scenario, and this identification becomes even more difficult in mental health. This is because PHC environments aim to approach the user in a holistic perspective in a social, economic, family and cultural context where he or she is inserted.[10]
It is also important to highlight that the Brazilian PHC has been historically insufficient in a large part of the country with regard to a specialized mental health network,[11] something that may be related to the poor assessments noted in the group in Brazil. Additionally, there is an eminent stigma in the Brazilian population associated with the diagnosis of mental disorders, which makes it extremely difficult to receive and follow-up with users as well as stimulate adherence to treatment.[43] Regarding this problem, another Brazilian study found that older people with depression and other mental disorders did not perceive the presence of an established bond with their PHC unit, unlike others who were not depressed. Rather, they perceived support for being linked to hypertension and diabetes programs, diseases for which there are advanced and well-established policies in Brazil.[44]
On the other hand, family health units in Portugal have a history of good service assessments, especially in terms of accessibility and user satisfaction.[16,17] Even so, there is an important gap in terms of meeting their mental health demands.[45] When present, interventions to address depression and other mental disorders are carried out by psychologists integrated into the primary care service, members of the Portuguese Psychologists Association, who are referred by the general practitioner of the PHC health centers, a process that is required by the Portuguese health system and has been effective after several treatment sessions.[46] Despite the success of this strategy, it is noteworthy that this care model differs from that adopted by the Brazilian PHC, which, in turn, has as a basis for its actions in the formation and strengthening of the bond between the team members and the population of their area of coverage. In this case, the objective is to solve at least 80.0% of its demands within the PHC itself.[11]
Another important factor that can be related to the findings is the cultural component of both countries, in relation to the way users use health services, their habits of life in general, and their language and interpretation of the items placed in the research instruments. Regarding this last aspect, even with the validation of the instruments in both countries and the great grammatical similarity between the languages of Brazil and Portugal,[24–27] the understanding of what is being asked can be influenced by the individual's schooling level, which can modify his or her own understanding of the concepts of QoL and depressive symptoms. Among the findings, the differences between groups regarding the length of schooling were significant and proportionally higher in Portugal.
Regarding the way Brazilian older people use PHC services, their demand is mainly focused on the prevention and treatment of noncommunicable chronic diseases, such as hypertension and diabetes, with little direct approach to mental health and without a well-defined referral system for specialized services.[47] We should also highlight community health workers, who play an important role in strengthening the link between the user and the service; among their duties is to visit users in their homes to check their specific needs and enable their access to PHC. Their access strategies include scheduling outpatient appointments, exams, vaccines, and even consultations at home, which, for older people users, is an important tool to meet their demands, even if they are unable to travel to the units.[48] Actions focused on the QoL of older people are also a focus of Brazilian PHC and need to be worked on with a focus on emotional, functional and physical aspects,[47] as evidenced in our own data.
In a study conducted in northern Portugal, more than 35.0% of PHC users were older people, but the greatest demand was for the treatment of chronic diseases.[49] These data imply great demands for screening and follow-up of the older population, including its mental components, since it has already been proven to be directly associated with physical health.[33]
Brazil and Portugal have a historical relationship regarding their public health policy frameworks. On the 30th anniversary of the Declaration of Alma-Ata,[50] the World Health Organization called on all governments to reflect on major reforms of PHC. The cities of Lisbon and Rio de Janeiro stood out, presenting proposals, for example, referring to teamwork aspects with professional motivation, investment in the information system and its computerization, quality, and accreditation of units by public agencies.[51] Within the context of mental health, the integration between PHC and the specialized network is also important, since the management of disorders by specialized professionals has proven to be efficient.[11]
4.3. Study limitations
The main limitation of our study was the limited sample, especially in the group from Portugal, which occurred due to the difficulty of accessing data collection sites and non-authorization by their PHC services within the health units. The cross-sectional cutting applied to our findings implies a break in the generalization potential of the results, without power of inferences or causal relationships. To mitigate these biases and limitations, we paired the groups from the 2 countries, which allowed us to perform interesting and decisive analyses to meet the research objective. Another possible bias was that the previous psychological follow-up of some participants could have influenced the results. However, the interviews did not ask if they had already received any treatment or follow-up in their own health network or in the private system.
4.4. Conclusions and final considerations
The results revealed a strong association and moderate to strong correlation between the absence of depression and better QoL in the Emotional aspects, Functional aspects, Physical aspect, Mental health and Total score domains, as well as in the Mental health and Physical health summary measures. This, in turn, showed a greater association with depression in the face of poorer performance. Although this study explored different countries regarding geographical space and culture, that is, health conditions in Portugal and Brazil, the association with depression were higher in the worst QoL. In this context, Portugal presented more expressive results than Brazil, which also presented association with the same aspects highlighted among the Portuguese. Given the evidence of the findings, the hypothesis of the study should be accepted.
Given the cross-sectional cut-off of both scenarios, a longitudinal approach is needed to explore outcomes and study the cause-and-effect relationship between depression and aspects of QoL, including the use of effective interventions.
Acknowledgments
We would especially like to thank the following people: Thazia Costa and colleagues, who made it possible to include this research in the Natal area; the team from the Santa Cruz Family Health Strategy, since they allowed us to carry out the research in their environment; and Professor Dr. João Manuel Galhanas Mendes, who welcomed the team of Brazilian researchers and students in Évora, Portugal, which made it possible to have contact with his community and carry out the study in that environment.
Author contributions
Conceptualization: Bruno Araújo da Silva Dantas, Anna Carolyna Vieira Cavalcante, Jéssica Maria Arouca de Miranda, Gislani Acásia da Silva Toscano.
Data curation: Felismina Rosa Parreira Mendes, Gilson de Vasconcelos Torres.
Formal analysis: Gilson de Vasconcelos Torres.
Funding acquisition: Gilson de Vasconcelos Torres.
Investigation: Bruno Araújo da Silva Dantas, Anna Carolyna Vieira Cavalcante, Jéssica Maria Arouca de Miranda, Gislani Acásia da Silva Toscano, Felismina Rosa Parreira Mendes.
Methodology: Bruno Araújo da Silva Dantas, Anna Carolyna Vieira Cavalcante, Jéssica Maria Arouca de Miranda, Gislani Acásia da Silva Toscano, Felismina Rosa Parreira Mendes, Francisco Arnoldo Nunes de Miranda, Eulália Maria Chaves Maia, Gilson de Vasconcelos Torres.
Project administration: Thaiza Teixeira Xavier Nobre, Felismina Rosa Parreira Mendes, Francisco Arnoldo Nunes de Miranda, Gilson de Vasconcelos Torres.
Resources: Gilson de Vasconcelos Torres.
Supervision: Thaiza Teixeira Xavier Nobre, Felismina Rosa Parreira Mendes, Francisco Arnoldo Nunes de Miranda, Eulália Maria Chaves Maia, Gilson de Vasconcelos Torres.
Validation: Thaiza Teixeira Xavier Nobre, Felismina Rosa Parreira Mendes, Francisco Arnoldo Nunes de Miranda, Eulália Maria Chaves Maia, Gilson de Vasconcelos Torres.
Visualization: Thaiza Teixeira Xavier Nobre, Francisco Arnoldo Nunes de Miranda, Eulália Maria Chaves Maia, Gilson de Vasconcelos Torres.
Writing – original draft: Bruno Araújo da Silva Dantas, Gislani Acásia da Silva Toscano, Thaiza Teixeira Xavier Nobre, Felismina Rosa Parreira Mendes, Francisco Arnoldo Nunes de Miranda, Gilson de Vasconcelos Torres.
Writing – review & editing: Bruno Araújo da Silva Dantas, Jéssica Maria Arouca de Miranda, Gislani Acásia da Silva Toscano, Thaiza Teixeira Xavier Nobre, Felismina Rosa Parreira Mendes, Francisco Arnoldo Nunes de Miranda, Eulália Maria Chaves Maia, Gilson de Vasconcelos Torres.
Footnotes
Abbreviations: CI = confidence interval, MMSE = mini-mental state examination, OR = odds ratio, PHC = primary health care, QoL = quality of life, SF-36 = medical outcomes short-form health survey QoL.
How to cite this article: Dantas BA, Cavalcante AC, Miranda JM, Toscano GA, Nobre TT, Mendes FR, Miranda FA, Maia EM, Torres Gd. Depression and quality of life in Brazilian and Portuguese older people communities: analysis of association. Medicine. 2021;100:46(e27830).
This research was funded by the Brazilian National Council for Scientific and Technological Development through process number 454771/2014-2, Call: MCTI/CNPQ/Universal 14/2014 - Range B.
The authors have no conflicts of interests to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].Cerin E, Sit CH, Zhang CJ, et al. Neighbourhood environment, physical activity, quality of life and depressive symptoms in Hong Kong older adults: a protocol for an observational study. BMJ Open 2016;6:01–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Polat U, Bayrak Kahraman B, Kaynak I, Gorgulu U. Relationship among health-related quality of life, depression and awareness of home care services in older patients. Geriatr Gerontol Int 2016;16:1211–9. [DOI] [PubMed] [Google Scholar]
- [3].Jeong SH, Chun BC. Individual and regional factors associated with suicidal ideation among Korean elderly: a multilevel analysis of the Korea Community Health Survey. Epidemiol Health 2019;41:01–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Pilania M, Yadav V, Bairwa M, et al. Prevalence of depression among the elderly (60 years and above) population in India, 1997-2016: a systematic review and meta-analysis. BMC Public Health 2019;19:01–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].de Oliveira L, Souza EC, Rodrigues RAS, Fett CA, Piva AB. The effects of physical activity on anxiety, depression, and quality of life in elderly people living in the community. Trends Psychiatry Psychother 2019;41:36–42. [DOI] [PubMed] [Google Scholar]
- [6].Chang YC, Yao G, Hu SC, Wang JD. Depression affects the scores of all facets of the WHOQOL-BREF and May mediate the effects of physical disability among community-dwelling older adults. PLoS One 2015;10:01–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hajek A, Brettschneider C, Mallon T, et al. The impact of social engagement on health-related quality of life and depressive symptoms in old age - evidence from a multicenter prospective cohort study in Germany. Health Qual Life Outcomes 2017;15:01–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. World Health Organization. The World Health Report 2001. Mental Health: New Understanding, New Hope. 1 ed: April, 2002; 2002. [Google Scholar]
- [9].WHOQOL Group. The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med 1995;41:1403–9. [DOI] [PubMed] [Google Scholar]
- [10].Jauregui A, Ponte J, Salgueiro M, et al. Efficacy of a cognitive and behavioural psychotherapy applied by primary care psychologists in patients with mixed anxiety-depressive disorder: a research protocol. BMC Fam Pract 2015;16:01–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Andrade MV, Noronha K, Cardoso CS, Oliveira CDL, Calazans JA, Souza MN. Challenges and lessons from a primary care intervention in a Brazilian municipality. Rev Saude Publica 2019;53:01–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Augusto DK, Lima-Costa MF, Macinko J, Peixoto SV. Factors associated with the evaluation of quality of primary health care by older adults living in the Metropolitan Region of Belo Horizonte, Minas Gerais, Brazil, 2010. Epidemiol Serv Saude 2019;28:01–11. [DOI] [PubMed] [Google Scholar]
- [13].Rodrigues MM, Alvarez AM, Rauch KC. Trends in hospitalization and mortality for ambulatory care sensitive conditions among older adults. Rev Bras Epidemiol 2019;22:01–11. [DOI] [PubMed] [Google Scholar]
- [14].Santos VC, Anjos KF, Boery RN, Moreira RM, Cruz DP, Boery EN. Hospitalization and hospital mortality of elderly people with mental and behavioral disorders in Brazil, 2008-2014. Epidemiol Serv Saude 2017;26:39–49. [DOI] [PubMed] [Google Scholar]
- [15]. Brasil. Percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal: Brasil e grandes regiões. In: Pesquisa Nacional de Saúde 2019, ed. 2020, ed. Intituto Brasileiro de Geografia e Estatística, Coordenação de Trabalho e Rendimento. - Rio de Janeiro, 2020: 113p. [Google Scholar]
- [16].Pinto LF, Rocha CM, Lapao LV, Pisco LA. Comparative health systems: primary health care in the cities of Lisbon and Rio de Janeiro. Cien Saude Colet 2017;22:676–7. [DOI] [PubMed] [Google Scholar]
- [17].Lapao LV, Pisco L. Primary health care reform in Portugal, 2005-2018: the future and challenges of coming of age. Cad Saude Publica 2019;35: (Suppl 2): 01–12. [DOI] [PubMed] [Google Scholar]
- [18]. Instituto Nacional de Estatística. Inquérito Nacional de Saúde 2019. 2019 ed. Portugal, 2020. [Google Scholar]
- [19]. Eurostat. Alterações demográficas na Europa — Fichas informativas por país: Portugal, 2019. Disponível em: https://ec.europa.eu/eurostat/documents/10186/10990320/PT-PT.pdf. [Google Scholar]
- [20].Pereira HV, Palmeira AL, Carraca EV, Santos I, Marques MM, Teixeira PJ. Running prevalence in Portugal: Socio-demographic, behavioral and psychosocial characteristics. PLoS One 2021;16:01–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Brandao MP, Martins L, Szewczyczak M, Talarska D, Philp I, Cardoso MF. Threats to health and well-being perceived by older people in Poland and Portugal. Acta Med Port 2018;31:409–15. [DOI] [PubMed] [Google Scholar]
- [22].Kalache A, Gatti A. Active ageing: a policy framework. Advances in gerontology = Uspekhi gerontologii 2003;11:07–18. [PubMed] [Google Scholar]
- [23].Murden RA, McRae TD, Kaner S, Bucknam ME. Mini-mental state exam scores vary with education in blacks and whites. J Am Geriatr Soc 1991;39:149–55. [DOI] [PubMed] [Google Scholar]
- [24].Ciconelli RM, Ferraz MB, Santos W, Meinão I, Quaresma MR. Tradução para a língua portuguesa e validação do questionário genérico de avaliação de qualidade de vida SF-36 (Brasil SF-36). Rev bras reumatol 1999;39:143–50. [Google Scholar]
- [25].Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561–71. [DOI] [PubMed] [Google Scholar]
- [26].Gomes-Oliveira MH, Gorenstein C, Lotufo Neto F, Andrade LH, Wang YP. Validation of the Brazilian Portuguese version of the Beck Depression Inventory-II in a community sample. Braz J Psychiatry 2012;34:389–94. [DOI] [PubMed] [Google Scholar]
- [27].Morin CM, Landreville P, Colecchi C, McDonald K, Stone J, Ling W. The beck anxiety inventory: psychometric properties with older adults. J Clin Geropsychol 1999;5:19–29. [Google Scholar]
- [28]. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2ª ed, Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers, 1988. [Google Scholar]
- [29].Rong J, Ding H, Chen G, Ge Y, Xie T, Meng N. Quality of life of rural poor elderly in Anhui, China. Medicine (Baltimore) 2020;99:01–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Scott KM, Lim C, Al-Hamzawi A, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry 2016;73:150–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Hu C, Zhao D, Gong F, Zhao Y, Li J, Sun Y. Risk factors for suicidal ideation among the older people living alone in rural region of China: A path analysis. Medicine (Baltimore) 2020;99:01–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Lopez-Torres Hidalgo J, Grou D-E. Effectiveness of physical exercise in the treatment of depression in older adults as an alternative to antidepressant drugs in primary care. BMC Psychiatry 2019;19:01–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Branco JC, Jansen K, Sobrinho JT, et al. Physical benefits and reduction of depressive symptoms among the elderly: results from the Portuguese “National Walking Program”. Cien Saude Colet 2015;20:789–95. [DOI] [PubMed] [Google Scholar]
- [34].Lin PS, Hsieh CC, Cheng HS, Tseng TJ, Su SC. Association between physical fitness and successful aging in Taiwanese older adults. PLoS One 2016;11:01–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Arija V, Villalobos F, Pedret R, et al. Physical activity, cardiovascular health, quality of life and blood pressure control in hypertensive subjects: randomized clinical trial. Health Qual Life Outcomes 2018;16:01–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Rodjer L, H Jonsdottir I, Borjesson M. Physical activity on prescription (PAP): self-reported physical activity and quality of life in a Swedish primary care population, 2-year follow-up. Scand J Prim Health Care 2016;34:443–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Li YT, Tung TH. Effects of protective factors on the depressive status of elderly people in Taiwan. Medicine (Baltimore) 2020;99:01–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Pinto JM, Fontaine AM, Neri AL. The influence of physical and mental health on life satisfaction is mediated by self-rated health: A study with Brazilian elderly. Arch Gerontol Geriatr 2016;65:104–10. [DOI] [PubMed] [Google Scholar]
- [39].Toprak M. The relationship between psychological factors and quality of life in elderly population of Van, eastern Turkey. J Pak Med Assoc 2019;69:1803–7. [DOI] [PubMed] [Google Scholar]
- [40].Dantas BAS, Miranda JMA, Cavalcante ACV, et al. Impact of multidimensional interventions on quality of life and depression among older adults in a primary care setting in Brazil: a quasi-experimental study. Braz J Psychiatr 2020;42:201–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Mountain G, Windle G, Hind D, et al. A preventative lifestyle intervention for older adults (lifestyle matters): a randomised controlled trial. Age Ageing 2017;46:627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Pols AD, Adriaanse MC, van Tulder MW, et al. Two-year effectiveness of a stepped-care depression prevention intervention and predictors of incident depression in primary care patients with diabetes type 2 and/or coronary heart disease and subthreshold depression: data from the Step-Dep cluster randomised controlled trial. BMJ Open 2018;8:01–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Onocko-Campos RT, Amaral CEM, Saraceno B, de Oliveira BDC, Treichel C, Delgado PGG. Functioning of psychosocial care centers in four cities in BrazilActuacion de los Centros de Atencion Psicosocial en cuatro centros urbanos en Brasil. Rev Panam Salud Publica 2018;42:01–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Aragao EIS, Portugal FB, Campos MR, Lopes CS, Fortes S. Different patterns of social support perceived and their association with physical (hypertension, diabetes) or mental diseases in the context of primary health care. Cien Saude Colet 2017;22:2367–74. [DOI] [PubMed] [Google Scholar]
- [45].Alves S, Teixeira L, Azevedo MJ, Duarte M, Ribeiro O, Paul C. Unmet needs in Primary Care of older clients with mental health concerns. Int J Qual Health Care 2019;31:312–8. [DOI] [PubMed] [Google Scholar]
- [46].Ricou M, Marina S, Vieira PM, et al. Psychological intervention at a primary health care center: predictors of success. BMC Fam Pract 2019;20:01–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Schenker M, Costa DHD. Advances and challenges of health care of the elderly population with chronic diseases in Primary Health Care. Cien Saude Colet 2019;24:1369–80. [DOI] [PubMed] [Google Scholar]
- [48].Simas PRP, Pinto ICM. Health work: portrait of community workers in the Northeast region of Brazil. Cien Saude Colet 2017;22:1865–76. [DOI] [PubMed] [Google Scholar]
- [49].Prazeres F, Santiago L. Prevalence of multimorbidity in the adult population attending primary care in Portugal: a cross-sectional study. BMJ Open 2015;5:01–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].World Health Organization. International conference on primary health c. Declaration of Alma-Ata. WHO Chron 1978;32:428–30. [PubMed] [Google Scholar]
- [51].Soranz D, Pisco LA. Primary health care reform in the cities of Lisbon and Rio de Janeiro: context, strategies, results, learning and challenges. Cien Saude Colet 2017;22:679–86. [DOI] [PubMed] [Google Scholar]