Abstract
Background
Tibial Pilon fractures are severe fractures accompanied by soft tissue injury. Although open reduction and internal fixation (ORIF) are effective in treating Pilon fractures, there is a controversy over time to surgery due to reported postoperative complications. However, there is no systematic review evaluating the difference of postoperative complications between early and delayed ORIF for treating pilon fractures.
Methods
Relevant literature written in English will be searched through PubMed, Cochrane Library, Embase, MEDLINE, and Web of Science. The study aims to compare the effects and complications of early and delayed ORIF for treating fresh pilon fractures in adult patients. The primary outcome will be infection rate, fracture union time, nonunion and malunion rate. And the secondary outcome will be metalwork removal, amputation, and ankle function grade. Two reviewers will independently assess the eligibility of the studies according to the pre-defined inclusion and exclusion criteria. A meta-analysis for the available data will be conducted using Revman 5.3. To measure effect size, odds ratios (ORs) and mean difference will be used for dichotomous and continuous data, respectively. Statistical heterogeneity will be explored. And a random-effects model or a fixed-effects will be used in pooled data on the basis of the existence or absence of heterogeneity. Subgroup analysis will be conducted to identify sources of heterogeneity and sensitivity analysis to test the results’ robustness. We will assess the risk of bias by four different quality assessment tools according to the study design. Publication bias will be evaluated by funnel plot. The study data will be stored in the Open Science Framework website.
PROSPERO registration number
1. Introduction
Tibial Pilon fractures, defined as fractures of distal tibial extending to the joint surface, account for 1% of all lower limb fractures [1]. They are commonly caused by high-energy axial forces and rotational forces. The combinations of articular comminution and metadiaphyseal osseous deficits result in difficulty of fracture reduction, which is a challenge for surgeons [2–4]. Additionally, because of extensive soft tissue damage in high-energy trauma, there are high risks of wound infection, nonunion, and delayed union. Posttraumatic arthritis is also a common complication of pilon fractures [5, 6].
Management of pilon fracture aims not only to achieve anatomical reduction with the restoration of mechanical axis and length of the lower limbs and joint congruity, fixation stable enough for exercises, and early functional mobility but also to prevent complications [7]. The complication rate, however, is relevant to soft tissue conditions, comorbidities, time to operation, and surgical intervention approach [8–10]. Early ORIF, known as a one-stage procedure with definitive internal fixation, which was reported by Ruedi and Allgower in 1969 with good outcomes in pilon fracture [11]. Although the anatomical reduction is achieved, other orthopedic surgeons are faced with a higher complication rate. Literature reported that infection rate ranges from 0% to 55% [12]. However, recently a cohort study documented that the infection rate of early ORIF is only 2.7% and a good reduction rate is 90% [13]. Two-stage open reduction and internal fixation, proposed by Patterson and Cole, are regarded as a method that protects soft tissue and reduces infection rate [14]. This approach involves temporary fixation with external fixators or calcaneal traction, followed by open reduction and internal fixation. However, recent studies have suggested that the time of surgery has few correlations with wound complications, and delayed surgery may increase risk of infection [11, 15]. Moreover, this method leads to a long-term hospital stay and lack of anatomical reduction due to delayed operation [16].
2. Objective
The aim of the systematic review is to answer the PICO question: “Do early and delayed open reduction and internal fixation have different influence on postoperative complications in adult patients with pilon fracture?” The relationship between time to surgical and complication will be discussed to conclude the differences in complications between the two treatment options.
3. Methods
The protocol of this systematic review and meta-analysis has been registered in PROSPERO and will be conducted in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17]. ethical approvals and patient consent are not necessary because the meta-analysis will be based on published research. We will submit our meta-analysis to a peer-reviewed journal for publication.
3.1 Eligibility criteria
3.1.1 Types of studies
All randomized controlled trials (RCTs) and non-randomized studies (cohort studies or case-series) will be included. The included studies will be written in English. Reviews, case reports, conference abstracts, letters, the study protocol will also be excluded.
3.1.2 Types of participants
Participants will be those diagnosed with pilon fractures by radiology. Only adult patients older than 18 will be included. Studies investigating patients with old pilon fractures will be excluded. Old fracture is defined as fracture with the interval between consulting time and injury time exceeding three weeks. There was no restriction on gender and race.
3.1.3 Types of interventions
The surgical approach will be early or delayed ORIF. Early ORIF refers to the one-stage procedure with definitive internal fixation. Delayed ORIF is a temporary fixation of external fixation followed by open reduction and internal fixation.
3.1.4 Outcomes
Primary outcomes: superficial infection and deep infection rate; fracture union time.
Secondary outcomes: nonunion (defined as fracture with a healing time of more than 9 months), metalwork removal, amputation, ankle function grade.
3.2 Search strategy
PubMed, Cochrane Library, Embase, MEDLINE, Web of Science will be searched for literature written in English. Time will be set from the inception of the database to the day on which the search is performed.
We plan to search for literature by free word. Before systemic review and meta-analysis, the database will be searched on a regular basis, and references will be screened to identify additional sources. Final search will be performed before full-text were finished to update results. An example search strategy for Cochrane Library is shown in Table 1.
Table 1. Search strategy for Cochrane Library.
| Search term | |
|---|---|
| 1# | Pilon OR tibial plafond fracture OR distal tibial fracture OR tibial pilon fracture |
| 2# | Primary fixation OR early fixation OR one-stage |
| 3# | delayed fixation OR two-stage treatment |
| 4# | 1# AND 2# AND 3# |
3.3 Study selection, data extraction, and management
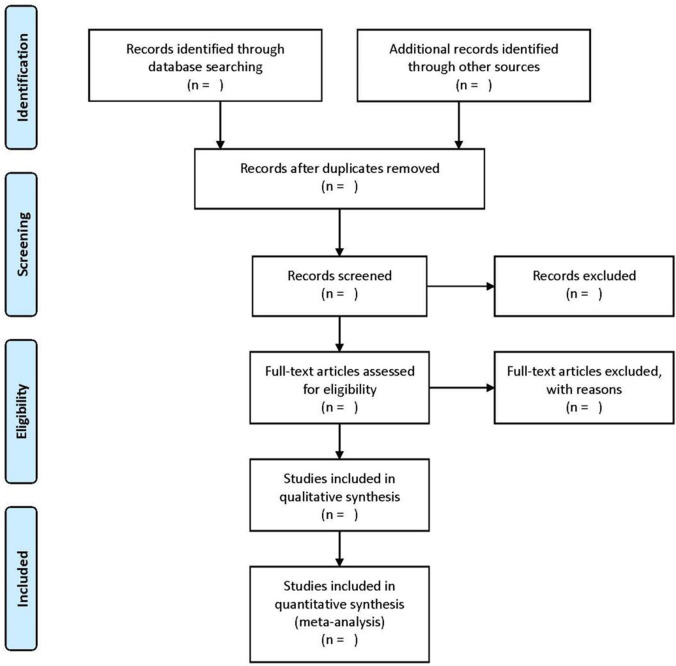
Two reviewers will independently assess the eligibility of the studies according to the pre-defined inclusion and exclusion criteria. After duplications from all the search citations being removed, titles and abstracts of the remaining ones will be screened for their eligibility. The full texts will then be retrieved to determine further if they meet the inclusion and exclusion criteria. Any disagreement will be resolved by the third author. The process of identifying, screening, and including and excluding results will be shown using the flow chart (Fig 1).
Fig 1. A flow chart for the systematic review.
Data will be independently extracted by two authors using a pre-designed standard form involving patient age and gender, fracture type and pilon fracture classification, intervention and operative description, complications encountered, radiological and clinical time to union, ankle function, and documented length of follow-up. Missing information will be obtained by consulting the corresponding author of original studies.
We will upload our protocols, data extraction information, and analytic results on the Open Science Framework website for researchers to control/prove our findings. (https://help.osf.io/hc/en-us).
3.4 Assessment of risk of bias
Two review authors will independently evaluate the risk of bias of included studies. The risk of bias of randomized controlled trials (RCTs) will be rated using the Cochrane quality assessment tool for RCTs. Risk of bias in non-randomized studies of Intervention (ROBINS-I) tool will be used to assess the risk of bias in the included non-randomized studies, and the Newcastle–Ottawa scale (NOS) [18] is planned to be used to assess the quality of case-control and cohort studies. A third reviewer will be introduced as an arbitrator if there is any disagreement among the two review authors. Case-series will be assessed by quality appraisal checklist of case series studies, which was put forward by Institute of Health Economics [19].
3.5 Statistical analysis
If data attracted from eligible literature is available for meta-analyses, Review Manager 5.3 software will be used. Statistical heterogeneity will be determined by I² statistic [20] with significance set at ≥50%, and the Chi2 statistic [21] with significance set at P < 0.10. When significant heterogeneity exists, a random-effects model will be used, otherwise, a fixed-effects model will be utilized.
If RCTs or non-randomized studies are not included, or if the heterogeneity among studies making meta-analysis impossible, the descriptive analysis will be performed. We plan to assess possible sources of heterogeneity by subgroup and sensitivity analyses where data are available.
In the condition of missing or unclear data, study authors will be contacted at the data extraction stage. If data are not acquired, we consider that existing data will be analyzed. The relevant factor will be used to calculate the continuous variable of standard deviation.
3.6 Subgroup analysis
Subgroup analysis will be performed if we want to find the source of heterogeneity among these studies. Fracture classification, compromise of soft tissue, and literature quality will be considered in subgroups of analysis.
3.7 Sensitivity analysis
A sensitivity analysis will be performed to confirm whether the pooled results are robust and credible by excluding highly biased studies or including articles one by one.
3.8 Publication bias
Publication bias will be evaluated by funnel plot (RevMan). If the number of studies exceeds 10, Egger’s test (Stata) will be used to estimate bias quantification.
3.9 Evidence evaluation
The Grading of Recommendations Assessment, Development, and Evaluation system (GRADE) [22] will be used to evaluate the strength of evidence for each outcome.
4. Discussion
The currently available literature has not reached a consensus regarding which of early ORIF and delay ORIF result in less postoperative complications. Therefore, we plan to perform the systemic review and meta-analysis to present a general view of the current literature and quantitatively analyze the data of studies.
To our knowledge, this will be the first systemic review and meta-analysis investigating the influence of early ORIF versus delay ORIF on postoperative complications. We expect to demonstrate results of the study in several ways. Firstly, we will show infection rate of two surgical ways, including superficial infection and deep infection. Infection is an important factor for assessment of therapeutic effect and can result in skin necrosis and exposure of internal plant [23]. Secondly, time to union, delayed union and nonunion rate will be documented, which are relevant to time of weight-bearing exercise and return to work and activities. Finally, because metalwork removal rate and ankle function grade reflect re-operation rate and quality of life [24], we will present the results in our study. In a word, the study’s findings could provide orthopedists with evidence of the optimal operation time of treatment for pilon fracture. Moreover, it may also demonstrate the hypothesis of the window period of soft tissue.
There are some limitations in this study. Firstly, although we plan to search multidisciplinary databases, some specific databases are likely to be omitted, which can produce bias. Additionally, when data of randomized controlled trials (RCTs) and non-randomized studies are pooled, heterogeneity of articles can have negative effect on conclusion. The Cochrane Handbook for Systematic Reviews of Interventions recommendations will be used and data of literatures of different categories will be pooled respectively to minimize these limitations.
4.1 Amendments
If amendments are necessary, we will state the alteration and reasons, along with each amendment date.
Supporting information
(DOC)
Acknowledgments
The authors acknowledge the meta-analysis concepts and applications workshop manual by Michael Borenstein for his guidelines on reporting Meta-analysis, subgroup analysis and publication bias, (www.meta-analysis-workshops.com).
Abbreviations
- ORIF
open reduction and internal fixation
Data Availability
All relevant data from this study will be made available upon study completion.
Funding Statement
The study was funded by the Beijing University of Chinese Medicine through a grant given to YC (2020-jxs-022). The study also received funding through grants from CACMS Innovation Fund (C12021A02008) and the Capital Characteristic Clinic Project (Z161100000516111) awarded to ZC. The funders had and will not have a role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. the authors have declared that no competing interests exist.
References
- 1.Calori GM, Tagliabue L, Mazza E, de Bellis U, Pierannunzii L, Marelli BM, et al. Tibial pilon fractures: which method of treatment? Injury 2010;41:1183–90. doi: 10.1016/j.injury.2010.08.041 [DOI] [PubMed] [Google Scholar]
- 2.Jacob N, Amin A, Giotakis N, Narayan B, Nayagam S, Trompeter J. Management of high-energy tibial pilon fractures. Strategies Trauma Limb Reconstr 2015;10:137–47. doi: 10.1007/s11751-015-0231-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kottmeier SA, Madison RD, Divaris N. Pilon Fracture: Preventing Complications. Journal of the American Academy of Orthopaedic Surgeons 2018;26:640–51. doi: 10.5435/JAAOS-D-17-00160 [DOI] [PubMed] [Google Scholar]
- 4.Thordarson DB. Complications after treatment of tibial pilon fractures: prevention and management strategies. J Am Acad Orthop Surg 2000;8:253–65. doi: 10.5435/00124635-200007000-00006 [DOI] [PubMed] [Google Scholar]
- 5.McFerran MA, Smith SW, Boulas HJ, Schwartz HS.Complications encountered in the treatment of pilon fractures. J Orthop Trauma 1992;6:195–200. doi: 10.1097/00005131-199206000-00011 [DOI] [PubMed] [Google Scholar]
- 6.Liu X, An J, Zhang H, Li Y, Chen Y, Zhang W. Autologous Osteochondral Graft for Early Posttraumatic Arthritis of Tibiotalar Joints After Comminuted Pilon Fractures in Young Patients. Foot Ankle Int 2020;41:69–78. doi: 10.1177/1071100719875728 [DOI] [PubMed] [Google Scholar]
- 7.Huebner EJ, Iblher N, Kubosch DC, Suedkamp NP, Strohm PC. Distal tibial fractures and pilon fractures. Acta Chir Orthop Traumatol Cech 2014;81:167–76. [PubMed] [Google Scholar]
- 8.Korkmaz A, Ciftdemir M, Ozcan M, Copuroğlu C, Sarıdoğan K. The analysis of the variables, affecting outcome in surgically treated tibia pilon fractured patients. Injury 2013;44:1270–4. doi: 10.1016/j.injury.2013.06.016 [DOI] [PubMed] [Google Scholar]
- 9.Biz C, Angelini A, Zamperetti M, Marzotto F, Sperotto S P, Carniel D, et al. Medium-Long-Term Radiographic and Clinical Outcomes after Surgical Treatment of Intra-Articular Tibial Pilon Fractures by Three Different Techniques. Biomed Res Int 2018;2018:6054021. doi: 10.1155/2018/6054021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kline A J, Gruen G S, Pape H C, Tarkin I S, Irrgang J J, Wukich D K. Early complications following the operative treatment of pilon fractures with and without diabetes. Foot Ankle Int 2009;30:1042–7. doi: 10.3113/FAI.2009.1042 [DOI] [PubMed] [Google Scholar]
- 11.Rüedi TP, Allgöwer M. Fractures of the lower end of the tibia into the ankle-joint. Injury 1969;1:92–9. [Google Scholar]
- 12.Dillin L, Slabaugh P. Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma 1986;26:1116–9. doi: 10.1097/00005373-198612000-00011 [DOI] [PubMed] [Google Scholar]
- 13.White T O, Guy P, Cooke C J, Kennedy S A, Droll K P, Blachut P A, et al. The results of early primary open reduction and internal fixation for treatment of OTA 43.C-type tibial pilon fractures: a cohort study. J Orthop Trauma 2010;24:757–63. doi: 10.1097/BOT.0b013e3181d04bc0 [DOI] [PubMed] [Google Scholar]
- 14.Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma 1999;13:85–91. doi: 10.1097/00005131-199902000-00003 [DOI] [PubMed] [Google Scholar]
- 15.Riedel M D, Parker A, Zheng M, Briceno J, Staffa S J, Miller C P, et al. Correlation of Soft Tissue Swelling and Timing to Surgery With Acute Wound Complications for Operatively Treated Ankle and Other Lower Extremity Fractures. Foot Ankle Int 2019;40:526–36. doi: 10.1177/1071100718820352 [DOI] [PubMed] [Google Scholar]
- 16.Konrath G, Karges D, Watson J T, Moed B R, Cramer K. Early versus delayed treatment of severe ankle fractures: a comparison of results. J Orthop Trauma 1995;9:377–80. doi: 10.1097/00005131-199505000-00003 [DOI] [PubMed] [Google Scholar]
- 17.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj 2015;350:g7647. doi: 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 18.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. doi: 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 19.Moga C, Guo B, Schopflocher D, Harstall C. Development of a Quality Appraisal Tool for Case Series Studies Using a Modified Delphi Technique.2012. [Google Scholar]
- 20.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 21.Higgins J P, Thompson S G, Deeks J J, Altman D G. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mendoza C, Kraemer P, Herrera P, Burdiles P, Sepúlveda D, Núñez E, et al. Clinical guidelines using the GRADE system (Grading of Recommendations Assessment, Development and Evaluation). Rev Med Chil 2017;145:1463–70. doi: 10.4067/s0034-98872017001101463 [DOI] [PubMed] [Google Scholar]
- 23.Hutson JJ Jr. Salvage of pilon fracture nonunion and infection with circular tensioned wire fixation. Foot Ankle Clin 2008;13:29–68, vi. doi: 10.1016/j.fcl.2007.11.004 [DOI] [PubMed] [Google Scholar]
- 24.Lau T W, Leung F, Chan C F, Chow S P. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop 2008;32:697–703. doi: 10.1007/s00264-007-0384-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data from this study will be made available upon study completion.