Abstract
Objectives:
To assess if subjects with a clinical diagnosis of temporomandibular disorders (TMDs) have a similar prevalence of orthodontic history as a population of TMD-free individuals and to assess if those subjects who have a history of ideal orthodontics have fewer symptoms than those with a history of nonideal orthodontics.
Materials and Methods:
Two groups of age- and sex-matched individuals belonging to either a study (“TMD”) or a control group were recruited. Subjects who underwent orthodontic treatment were classified as having a history of ideal or nonideal orthodontics based on the current presence of normal values in five reference occlusal features.
Results:
The correlation with a history of orthodontic treatment was not clinically significant for any of the TMD diagnoses (ie, muscle pain, joint pain, disc displacement, arthrosis), with Phi (Φ) coefficient values within the −0.120 to 0.058 range. Within the subset of patients with a history of orthodontics, the correlation of ideal or nonideal orthodontic treatment with TMD diagnoses was, in general, not clinically relevant or was weakly relevant.
Conclusions:
Findings confirmed the substantial absence of clinically significant effects of orthodontics as far as TMD is concerned. The very low correlation values of a negative or positive history of ideal or nonideal orthodontics with the different TMD diagnoses suggest that orthodontic treatment could not have a true role for TMD.
Keywords: Orthodontics, Temporomandibular disorders
INTRODUCTION
The focus of etiological theories on temporomandibular disorders (TMDs) has progressively shifted from peripheral to central factors.1 Based on such an ongoing paradigm change, a much-diminished role is assigned to the features of natural dental occlusion as risk factors for TMD, in favor to central factors (ie, psychological and psychosocial factors, pain sensitivity, genetic determinants).2–4
Based on findings from some investigations5–8 that may show a higher prevalence of TMD in malocclusion patients compared to the normal population, there are still some communities of professionals claiming9,10 that the correction of purported abnormalities of dental occlusion should be recommended to manage and prevent TMD. Such an approach is actually not supported, and systematic reviews of the literature provide evidence-based recommendations that there is a lack of causal relationship between TMD and occlusion; they also offer evidence that irreversible occlusal treatments are not more useful than conservative treatment alone to either manage or prevent TMD.11–14
The literature15–17 on the effects of orthodontic treatment supports the neutral effects on the temporomandibular joint (TMJ). In particular, a recent systematic review16 concludes that there are insufficient research data on the relationship between active orthodontic intervention and TMD on which to base our clinical practice.
In the clinical setting, it appears that the development/alleviation of TMD signs and symptoms in orthodontic patients is unpredictable. However, it must also be pointed out that not all orthodontic treatments provide an “ideal” outcome in terms of occlusal goals and that the literature has never addressed the relationship between TMD and a history of “nonideal” orthodontics.
Indeed, most past investigations were based on a simple history-taking concerning past orthodontic treatments. This implies a failure to consider the true orthodontic results of treatments (ie, if orthodontics actually led to a good interarch relationship and occlusion). Thus, it seems that a further increase to the available knowledge could be made by discrimination between the relationship of TMD with “ideal” orthodontics (ie, achieving good occlusal parameters) versus “nonideal” orthodontics (ie, not achieving good occlusal parameters).
Based on this premise, the present cross-sectional investigation assessed the hypothesis that orthodontic treatments that achieve or do not achieve good occlusal parameters have different relationships with TMD. Thus, this study was designed to answer the following two clinical research questions: (1) Is there a relationship between a history of orthodontics and the presence of TMD?; (2) In the subset of individuals who have undergone orthodontic treatment, is a history of ideal orthodontics correlated with a lower prevalence of TMD symptoms than is correlated with nonideal orthodontics?
MATERIALS AND METHODS
Study Sample and Design
Participants to the study comprised two groups of age- and sex-matched individuals belonging to either a study (“TMD”) or a control group. The study group comprised patients seeking for TMD treatment at the Temporomandibular Disorders Clinic, while the control group included TMD-free subjects seeking dental care at the School of Dentistry of the University of Padova (Padova, Italy).
TMD patients were recruited consecutively during the years 2011 through 2012 and were included in the study if they met the following criteria: (1) age between 30 and 40 years; (2) presence of at least 24 teeth, with interarch antagonism within the right to left first molars; (3) if a history of orthodontic treatment existed, orthodontics had been performed more than 10 years earlier; and (4) absence of any past major (ie, more extensive than single crowns) prosthetic treatments.
During the first 3 months of the year 2012, a control group of TMD-free subjects was recruited according to the same criteria. As described in the details below, the Research Diagnostic Criteria for TMD (RDC/TMD) guidelines were adopted to assess TMD patients as well as to screen controls for the absence of TMD signs and symptoms.18 All participants were assessed by one of the two trained examiners.
The study protocol was reviewed and approved by the Institutional Review Board of the University of Padova, and each participant gave written informed consent to take part to the investigation.
Occlusal and History of Orthodontics Evaluation
All subjects underwent an assessment of dental occlusion based on protocols adopted in previous studies.19–21 The assessment focused on the detection of the following occlusal features:
Posterior unilateral inverse horizontal relationship (ie, cross-bite), recorded when the buccal cusps of any of the maxillary premolars and molars totally occluded lingually to the buccal cusps of the antagonist mandibular teeth;
Anterior horizontal overlap (ie, overjet), recorded as “normal” if the maxillary central incisors were anteriorly positioned with respect to the mandibular central incisors for up to 3 mm and as “excessive” when ≥4 mm;
Anterior vertical overlap (ie, overbite), recorded as “normal” if the maxillary central incisors overlapped the crown of the mandibular central incisors for up to 3 mm and as “excessive” when ≥4 mm (ie, deep bite);
Anterior open bite, recorded when no overlap was seen between the maxillary and mandibular incisors, including an edge-to-edge relationship; and
Centric relation to maximum intercuspation (RCP-MI) slide length, calculated in the three spatial axes after manual mandibular distraction. The RCP-MI slide values of <2 mm were considered “normal” and as “present” when ≥2 mm.
For those individuals who had undergone orthodontic treatment, the current presence of normal values in all of the above-mentioned occlusal features was considered a marker for a history of “ideal” orthodontics. On the contrary, those subjects showing abnormal values in any of the above occlusal features were considered to have a history of “nonideal” orthodontics.
TMD Assessment
In the TMD group, clinical assessment for TMD was performed according to the RDC/TMD guidelines18 by the same two trained examiners with expertise in TMD clinical assessment and research methodology.22
The assessment focused mainly on diagnosing the presence of muscle pain (ie, RDC/TMD diagnosis of myofascial pain), joint pain (ie, RDC/TMD diagnosis of arthralgia), disc displacement (ie, RDC/TMD diagnosis of disc displacement with or without reduction), and arthrosis (ie, RDC/TMD diagnosis of temporomandibular joint [TMJ] osteoarthrosis; viz, degenerative joint disease). Selected imaging techniques were prescribed, when needed, to support the clinical assessment.
Statistical Analysis
Within the whole study sample, the prevalence of each of the above specific TMD diagnoses was compared between subjects with or without a history of orthodontic treatment by means of the Phi (Φ) coefficient.
The same strategy was adopted within the subset of subjects with a history of orthodontics to compare the TMD prevalence between the individuals with a history of ideal or nonideal orthodontic treatment.
The Φ coefficient is a measure of the degree of association between two binary variables and is similar to the correlation coefficient in its interpretation. The values range from −1.0 to +1.0, indicating different levels of negative or positive correlation. As a general rule for correlation analyses, values higher than 0.7 are considered supportive of a strong positive correlation.23 For each comparison, odds ratios (ORs) for the TMD diagnoses were assessed to evaluate the relative risk for disease associated with a negative or positive history of orthodontics as well as with a history of ideal vs nonideal orthodontics. According to literature suggestions,24 the OR was considered clinically relevant for values lower than 0.5, indicating the potentially protective role of orthodontic treatment with respect to TMD, or higher than 2, suggesting that orthodontic treatment may even be potentially associated with TMD at a clinically meaningful level. In the case that OR values fell within the 0.5–2 range, orthodontic treatment was not to be considered to have had clinically relevant effects as far as its relationship with TMD was concerned.
All statistical procedures were performed with the software Statistical Package for the Social Sciences (SPSS Inc, Chicago, Ill).
RESULTS
The TMD group included 505 patients (75% females; mean age 38.7 ± 6.6 years), and the age- and sex-matched control group comprised 97 subjects (78% females; mean age 36.4 ± 8.6 years).
The percentage of individuals with a history positive for orthodontic treatment in the whole sample was up to 32.7% (n = 197). The average time span since the end of orthodontic treatment was 14.3 ± 6.1 years. History of orthodontics was positive for 32.1% of subjects without and 36.1% of subjects with TMD (Φ = −0.031; P = .442).
Within the TMD group, 35.1% of patients had muscle pain, 40.6% had joint pain, 54% had disc displacement, and 18.3% had arthrosis.
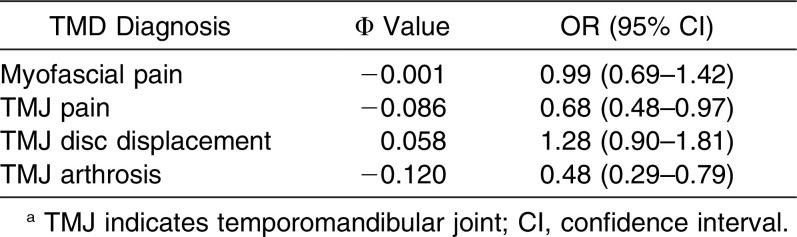
The correlation with a history of orthodontic treatment was not clinically relevant for any of the TMD diagnoses. Φ values were within the −0.120 to 0.058 range, while the OR values ranged from 0.48 (95% confidence interval [CI], 0.29–0.79) for TMJ arthrosis to 1.28 (95% CI, 0.90–1.81) for disc displacement (Table 1).
Table 1.
History of Orthodontic Treatment; Correlation Values and Odds Ratios (ORs) for the Different Temporomandibular Disorder (TMD) Diagnoses. Data Based on the Whole Sample (N = 612)a
As expected, the prevalence of the occlusal features under assessment was generally lower in the subjects who had undergone orthodontic treatment. An excessive overjet was found in 9.5% of subjects with and in 12.6% of those without a history of orthodontics; a RCP-MI slide was detected in 36.9% and 45.4%, a deep bite in 18.3% and 22.2%, and an anterior open bite in 5.6% and 8.2%, respectively. The only exception is cross bite, which was present in 31.5% of subjects with and 22.7% of those without a history of orthodontics. Based on the above, a history of previous orthodontics was successful in providing an occlusion without any of the assessed “malocclusal” features (ie, “ideal” orthodontics) only in 32.8% of subjects (64/195).
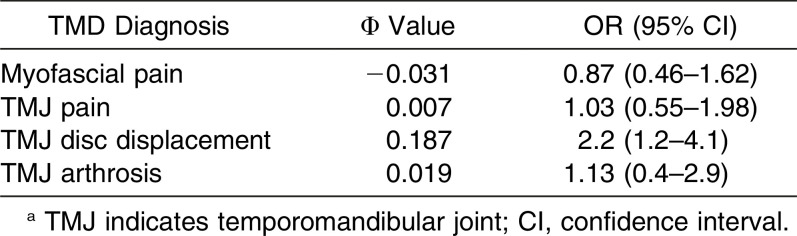
Within the subset of patients with a history of orthodontics, the correlation of ideal or nonideal orthodontic treatment with the presence of TMD was not significant, with 61.8% of subjects without TMD and 68.3% of subjects with TMD reporting a history of nonideal orthodontics (Φ = 0.053; P = .459). In general, the correlation values with specific TMD diagnoses were not clinically relevant or were weakly relevant. Φ values were within the −0.031 to 0.187 range, while the OR values ranged from 0.87 (95% CI, 0.46–1.62) for TMJ arthrosis to 2.23 (95% CI, 1.21–4.13) for disc displacement (Table 2).
Table 2.
History of Ideal Orthodontic Treatment; Correlation Values and Odds Ratios (ORs) for the Different Temporomandibular Disorder (TMD) Diagnoses. Data Based on the Subsample of Patients with a History Positive for Previous Orthodontic Treatment (N = 195)a
DISCUSSION
The role of abnormalities of dental occlusion as risk factors for TMDs has been progressively dismantled over the years.25 As a consequence, all strategies aiming to correct purported malocclusions and/or to pursue ideal gnathological schemes are discouraged as a treatment option for TMD.13,26,27
The existing literature28,29 suggests that, in general, orthodontic treatment does not provide any further advantages for TMD management or prevention with respect to conservative treatments. Based on that, orthodontics cannot be considered a valuable and recommendable treatment with which to manage TMD and is commonly believed to neither decrease nor increase the risk for TMD.16,17
Notwithstanding that, some aspects of the relationship between orthodontics and TMD are yet to be clarified as a result of the very scarce information that the literature has provided for use at the individual level. In particular, most studies are based on the simple recording of a positive self-reported history of orthodontic treatment; some other investigations, even if longitudinal in nature, do not describe properly the achievement of an orthodontic treatment goal in terms of dental alignment and interarch relationship corrections. Furthermore, selected groups of patients with specific malocclusions have been often chosen as study populations.
Based on these observations, this investigation introduces a potentially interesting concept that encourages us to delve deeper into the assessment of the TMD-orthodontics relationship (ie, the discrimination between patients with a history of ideal vs nonideal orthodontic treatment).
The study population included a large sample of adult TMD patients, along with age- and sex-matched TMD-free subjects. All participants reported their history of orthodontics and underwent an occlusal assessment aimed at verifying the presence of some occlusal abnormalities (ie, cross bite, excessive overjet, deep bite, open bite, occlusal instability/slide from RCP to MI) that, if “ideal” orthodontic goals could be achieved, should not be present at the end of treatment. Such an assessment allowed identification of those individuals who—independently by the type of baseline malocclusion and treatment approach—underwent an incomplete orthodontics that for some reason failed to adjust the occlusion (ie, nonideal orthodontics). This design permitted the retrieval of some interesting findings.
First, a history of orthodontics is not correlated with neither TMD as a whole or with any specific TMD diagnoses. Correlation values with the presence/absence of past orthodontics were very low for all of the different TMD diagnoses under investigation. Similarly, ORs for disease in the absence of orthodontic treatment were in general not clinically relevant. The only minor exception was TMJ arthrosis (21% of subjects with a history negative for previous orthodontics received a diagnoses of TMJ arthrosis, compared with 11.6% of subjects who underwent orthodontics), which showed an OR of 0.48. In addition, a positive history of orthodontics was not associated with TMD diagnoses, thus suggesting that orthodontic treatment did not increase relevantly the risk for showing TMD years later. Taken together, these findings add to the amount of existing literature suggesting that orthodontics has neither a protective/therapeutic nor a causative/precipitating role with respect to TMD.16,17,28,29 The clinical implications may be of paramount importance for a twofold reason. Indeed, on one hand, these results confirm that orthodontics is not associated with a decreased TMD prevalence, thus discouraging the routine adoption of any occlusal correction strategies on TMD patients in the clinical setting; on the other hand, the finding that orthodontics is not associated with an increased risk of TMD suggests that co-occurrence of other factors (eg, psychological, parafunctional, genetic, social issues) is implicated in the potential onset of TMD signs and symptoms during or after orthodontic treatment. As a general remark, it is important that this concept is stressed carefully before starting any orthodontic treatment to avoid potential claims.30
Second, within the subset of individuals who underwent previous orthodontic treatment, no clinically relevant differences for the presence of TMD have been found between subjects with a history of ideal vs those with a history of nonideal orthodontics. Again, very low correlation values with the different TMD diagnoses have been described. Also, in general, OR values for disease are not clinically relevant. The only minor exception was the potential increased risk for TMJ disc displacement that was described in individuals who received nonideal orthodontic treatment (OR = 2.2). Notwithstanding this group, it must be remarked that, as in the case of the above-described reduced risk for TMJ arthrosis in subjects with a history of orthodontics, any cause-and-effect speculation is prevented by the cross-sectional data collection adopted in this investigation.
Third, this article may alert researchers that in the everyday clinical practice it is not rare to find patients who reference a positive history of previous orthodontics even if they still show occlusal features such as cross bite, excessive overjet, deep bite, anterior open bite, or even unstable occlusion with centric slides. The retrospective data did not allow us to delve into further speculations as a result of the absence of information on the baseline occlusal conditions of orthodontically treated patients and the subsequent treatment strategy. However, long-term orthodontic success is a much-debated concern that should be managed as an important factor in studies on TMD epidemiology. This means that while studying the relationship between orthodontics and TMD, it may be recommended that the achievement of the orthodontic treatment goals, rather than the management of the variable “history of orthodontics” as a single entity, be assessed.
This investigation has some limitations, such as the absence of detailed information about the specific approach each individual had undergone to align teeth and/or to manage interarch relationships. In an ideal setting, this kind of investigation should have a prospective design, as in the case of the very few studies assessing the onset of TMD symptoms in subjects under orthodontic treatment.29
It must also be remarked that prospective studies conducted for research purposes, while having strong validity to assess the role of orthodontics, are unlikely to detect potential problems associated with nonideal orthodontics; for this reason, they fail to provide a full picture of everyday clinical activity. In addition, it should be noted that independent of the baseline condition, all orthodontic correction strategies have the common goal of achieving a posttreatment occlusion without co-occurrence of any of the five (mal)occlusion features under investigation. A possible strategy to increase the validity of our findings includes the recruitment of older patients to delve deeper into the assessment of TMJ arthrosis. In addition, the inclusion of other risk factors (ie, clenching-type bruxism, facial morphology) could aid in the design of multiple-variable models to provide a better depiction of the biological frame in which the orthodontics-TMD relationship takes place.
CONCLUSIONS
Findings of this study confirm the substantial absence of clinically significant effects of orthodontics as far as TMD is concerned. Indeed, the two clinical research questions underlying this investigation (ie, Is there a relationship between a history of orthodontics and the presence of TMD? Is a history of ideal orthodontics correlated with a lower prevalence of TMD symptoms than is associated with nonideal orthodontics?) should be answered “No.”
The cross-sectional design does not allow the formulation of any cause-and-effect speculations. However, the very low correlation values between a negative history of orthodontics and the different TMD diagnoses suggested that orthodontic treatment could not have a true role in TMD.
Based on the above finding, the possible clinical finding of TMD improvement with orthodontic treatment as well as of TMD sign and symptom onset during orthodontic treatment could be viewed as examples of “casual” (ie, achieved by chance) rather than “causal” findings.
Within these confines, in general our findings support the view that orthodontics is TMD-neutral.
REFERENCES
- 1.Greene CS. The etiology of temporomandibular disorders: implications for treatment. J Orofac Pain. 2001;15:93–105. [PubMed] [Google Scholar]
- 2.Manfredini D, Perinetti G, Guarda-Nardini L. Dental malocclusion is not related to temporomandibular joint clicking: a logistic regression analysis in a patient population. Angle Orthod. 2014;84:310–315. doi: 10.2319/041613-295.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009;23:153–166. [PubMed] [Google Scholar]
- 4.Greenspan JD, Slade GD, Bair E, et al. Pain sensitivity and autonomic factors associated with development of TMD: the OPPERA prospective cohort study. J Pain. 2013;14(12 suppl):T63–T74. doi: 10.1016/j.jpain.2013.06.007. e1–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Celic R, Jerolimov V, Panduric J. A study of influence of occlusal factors and parafunctional habits on the prevalence of signs and symptoms of TMD. Int J Prosthod. 2002;15:43–48. [PubMed] [Google Scholar]
- 6.Miller JR, Burgess JA, Critchlow CW. Association between mandibular retrognathia and TMJ disorders in adult females. J Public Health Dent. 2004;64:157–163. doi: 10.1111/j.1752-7325.2004.tb02746.x. [DOI] [PubMed] [Google Scholar]
- 7.Egermark I, Magnusson T, Carlsson GE. A 20-year follow-up of signs and symptoms of temporomandibular disorders and malocclusions in subjects with and without orthodontic treatment in childhood. Angle Orthod. 2003;73:109–115. doi: 10.1043/0003-3219(2003)73<109:AYFOSA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Abrahamsson C, Henrikson T, Nilner M, Sunzel B, Bonermark I, Ekberg EC. TMD before and after correction of dentofacial deformities by orthodontic and orthognathic treatment. Int J Oral Maxillofac Surg. 2013;42:752–758. doi: 10.1016/j.ijom.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 9.Alanen P. Occlusion and temporomandibular disorders (TMD): still unsolved question. J Dent Res. 2002;81:518–519. doi: 10.1177/154405910208100803. [DOI] [PubMed] [Google Scholar]
- 10.Monaco A, Petrucci A, Marzo G, Necozione S, Gatto R, Sgolastra F. Effects of correction of Class II malocclusion on the kinesiographic pattern of young adolescents: a case- control study. Eur J Paediatr Dent. 2013;14:131–134. [PubMed] [Google Scholar]
- 11.Türp JC, Schindler H. The dental occlusion as a suspected cause for TMDs: epidemiological and etiological considerations. J Oral Rehabil. 2012;39:502–512. doi: 10.1111/j.1365-2842.2012.02304.x. [DOI] [PubMed] [Google Scholar]
- 12.Pullinger A. J Oral Rehabil. Vol. 40. I:TM joint anatomic relationships; 2013. Establishing better biological models to understand occlusion; pp. 296–318. [DOI] [PubMed] [Google Scholar]
- 13.Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. Cochrane Database Syst Rev. 2003;1:CD003812. doi: 10.1002/14651858.CD003812. [DOI] [PubMed] [Google Scholar]
- 14.Forssell H, Kalso E. Application of principles of evidence-based medicine to occlusal treatment for temporomandibular disorders: are there lessons to be learned. J Orofac Pain. 2004;18:9–22. [PubMed] [Google Scholar]
- 15.McNamara JA., Jr Orthodontic treatment and temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:107–117. doi: 10.1016/s1079-2104(97)90100-1. [DOI] [PubMed] [Google Scholar]
- 16.Luther F, Layton S, McDonald F. Orthodontics for treating temporomandibular joint (TMJ) disorders. Cochrane Database Syst Rev. 2010;7:CD006541. doi: 10.1002/14651858.CD006541.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Michelotti A, Iodice G. The role of orthodontics in temporomandibular disorders. J Oral Rehabil. 2010;37:411–429. doi: 10.1111/j.1365-2842.2010.02087.x. [DOI] [PubMed] [Google Scholar]
- 18.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 19.Perinetti G, Cordella C, Pellegrini F, Esposito P. The prevalence of malocclusal traits and their correlations in mixed dentition children: results from the Italian OHSAR Survey. Oral Health Prev Dent. 2008;6:119–129. [PubMed] [Google Scholar]
- 20.Manfredini D, Vano M, Peretta R, Guarda-Nardini L. Jaw clenching effects in relation to two extreme occlusal features: patterns of diagnoses in a TMD patient population. J Craniomandib Sleep Pract. 2014;32:45–50. doi: 10.1179/0886963413Z.0000000009. [DOI] [PubMed] [Google Scholar]
- 21.Manfredini D, Visscher C, Guarda-Nardini L, Lobbezoo F. Occlusal factors are not related with self-reported bruxism. J Orofac Pain. 2012;26:163–167. [PubMed] [Google Scholar]
- 22.Manfredini D, Ahlberg J, Winocur E, Guarda-Nardini L, Lobbezoo F. Correlation of RDC/TMD axis I diagnoses and axis II pain-related disability. A multicenter study. Clin Oral Investig. 2011;15:749–756. doi: 10.1007/s00784-010-0444-4. [DOI] [PubMed] [Google Scholar]
- 23.McNemar Q. Psychological Statistics. New York, New York: Wiley; 1962. [Google Scholar]
- 24.Pullinger AG, Seligman DA. Quantification and validation of predictive values of occlusal variables in temporomandibular disorders using a multifactorial analysis. J Prosthet Dent. 2000;83:66–75. doi: 10.1016/s0022-3913(00)70090-4. [DOI] [PubMed] [Google Scholar]
- 25.Türp JC, Greene CS, Strub JR. Dental occlusion: a critical reflection on past, present and future concepts. J Oral Rehabil. 2008;35:446–453. doi: 10.1111/j.0305-182X.2007.01820.x. [DOI] [PubMed] [Google Scholar]
- 26.Manfredini D, Bucci MB, Montagna F, Guarda-Nardini L. Temporomandibular disorders assessment: medicolegal considerations in the evidence-based era. J Oral Rehabil. 2011;38:101–119. doi: 10.1111/j.1365-2842.2010.02131.x. [DOI] [PubMed] [Google Scholar]
- 27.Greene CS, Obrez A. Treating temporomandibular disorders with permanent mandibular repositioning: is it medically necessary. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:489–498. doi: 10.1016/j.oooo.2015.01.020. [DOI] [PubMed] [Google Scholar]
- 28.Imai T, Okamoto T, Kaneko T, Umeda K, Yamamoto T, Nakamura S. Long-term follow-up of clinical symptoms in TMD patients who underwent occlusal reconstruction by orthodontic treatment. Eur J Orthod. 2000;22:61–67. doi: 10.1093/ejo/22.1.61. [DOI] [PubMed] [Google Scholar]
- 29.Henrikson T, Nilner M. Temporomandibular disorders, occlusion and orthodontic treatment. J Orthod. 2003;30:129–137. doi: 10.1093/ortho/30.2.129. [DOI] [PubMed] [Google Scholar]
- 30.Jerrold L, Kandasamy S, Manfredini D. In: TMD and its medicolegal considerations in contemporary orthodontic practice. TMD and Orthodontics A Clinical Guide for the Orthodontist. Kandasamy S, Rinchuse D, Greene CS, Stockstill JW, editors. New York, New York: Springer; 2015. pp. 133–141. [Google Scholar]