Abstract
Objective:
To evaluate the capability of both cervical vertebral maturation (CVM) stages 3 and 4 (CS3-4 interval) and the peak in standing height to identify the mandibular growth spurt throughout diagnostic reliability analysis.
Materials and Methods:
A previous longitudinal data set derived from 24 untreated growing subjects (15 females and nine males,) detailed elsewhere were reanalyzed. Mandibular growth was defined as annual increments in Condylion (Co)–Gnathion (Gn) (total mandibular length) and Co–Gonion Intersection (Goi) (ramus height) and their arithmetic mean (mean mandibular growth [mMG]). Subsequently, individual annual increments in standing height, Co-Gn, Co-Goi, and mMG were arranged according to annual age intervals, with the first and last intervals defined as 7–8 years and 15–16 years, respectively. An analysis was performed to establish the diagnostic reliability of the CS3-4 interval or the peak in standing height in the identification of the maximum individual increments of each Co-Gn, Co-Goi, and mMG measurement at each annual age interval.
Results:
CS3-4 and standing height peak show similar but variable accuracy across annual age intervals, registering values between 0.61 (standing height peak, Co-Gn) and 0.95 (standing height peak and CS3-4, mMG). Generally, satisfactory diagnostic reliability was seen when the mandibular growth spurt was identified on the basis of the Co-Goi and mMG increments.
Conclusions:
Both CVM interval CS3-4 and peak in standing height may be used in routine clinical practice to enhance efficiency of treatments requiring identification of the mandibular growth spurt.
Keywords: Orthodontics, Cervical vertebrae, Standing height, Mandibular growth, Diagnosis, Accuracy
INTRODUCTION
Several dentofacial orthopedic treatments on growing patients have been shown to have their maximal effect if performed during specific skeletal maturational phases, such as the circumpubertal growth spurt.1,2 This is particularly true for skeletal Class II malocclusion patients, in whom functional appliances may have increased skeletal effects if treatment is performed during peak \mandibular growth.2,3 In this regard, chronological age has been shown not to be a valid predictor of skeletal maturation phases.4,5 Indeed, the clinical applicability of chronological age as an indicator of the onset of the pubertal growth spurt in the individual patient is limited, as the growth spurt is influenced by several other factors, including genetics, ethnicity, nutrition, and socioeconomic status.6
Previous studies have focused on the correlations between clinical indicators of growth phase, including cervical vertebral maturation (CVM) and standing height, and mandibular growth spurt. These studies were either cross sectional7 or longitudinal8–15 (for review, see Flores-Mir et al.5).
In spite of these studies, the diagnostic reliability of the interval between CVM stages 3 and 4 (CS3-4)1 and the peak in standing height in the identification of the mandibular growth spurt on an individual basis is yet undetermined. Indeed, correlations between parameters do not necessarily imply diagnostic accuracy.16,17 From a clinical standpoint, diagnostic accuracy on individual patients, rather than correlation on a group of subjects, has major implications.
Only one study7 has reported on the diagnostic capability of the CVM method in the identification of the mandibular growth spurt by using receiver operating characteristics (ROC) curves. ROC curve analysis can be used to evaluate the capability of a test to discriminate “diseased cases” from “normal cases.” However, this study7 was based on a cross-sectional sample and was limited to the analysis of the area under the curve.
One of the reasons underlying this noteworthy lack of data may be the difficulty associated with obtaining diagnostic parameters, such as sensitivity, specificity, and accuracy, from longitudinal data in a subset of selected subjects all with a predetermined condition (mandibular growth spurt) or a diagnostic outcome (a given CVM stage). Yet the identification of a mandibular growth spurt requires longitudinal data, and it is defined according to time intervals rather than being a cross-sectional recording.
To overcome such limitations in the present study, individual CVM stages and increments in standing height and mandibular growth recorded longitudinally were analyzed in a group of untreated subjects according to different predetermined annual (chronological) age intervals. Therefore, a full comparative diagnostic reliability analysis, including sensitivity, specificity, positive and negative predictive values (PPVs and NPVs), and accuracy, of the CS3-4 interval and the peak in statural height in the identification of the mandibular growth spurt initially was considered.
MATERIALS AND METHODS
The original data set used herein is from the files of the University of Michigan Elementary and Secondary School Growth Study (UMGS), as detailed in a previous article.9
Subjects
Briefly, the sample used in the original study9 and reanalyzed herein included 24 growing subjects (15 females and 9 males; age range 7–17 years) from the UMGS archives who provided longitudinal data for standing height corresponding to the consecutive cephalograms for all the examined subjects. Such subjects were included because they had six consecutive annual recordings that encompassed all CVM stages from 1 to 6, regardless of chronological age.
Data Collection
A modified version of the original method for assessment of CVM developed by Lamparski18 was adopted, with adjustments allowing for the appraisal of skeletal age, as previously reported by Franchi et al.9 Further details of the data recording and cephalometric tracing method are reported in the original article.9 For the present study, data on mandibular size, defined as Condylion (Co)–Gnathion (Gn) (total mandibular length) and Co–Gonion Intersection (Goi) (ramus height), were used. In addition, a mean mandibular growth (mMG) parameter defined as the arithmetic mean of Co-Gn and Co-Goi (Figure 1) also was considered.
Figure 1.
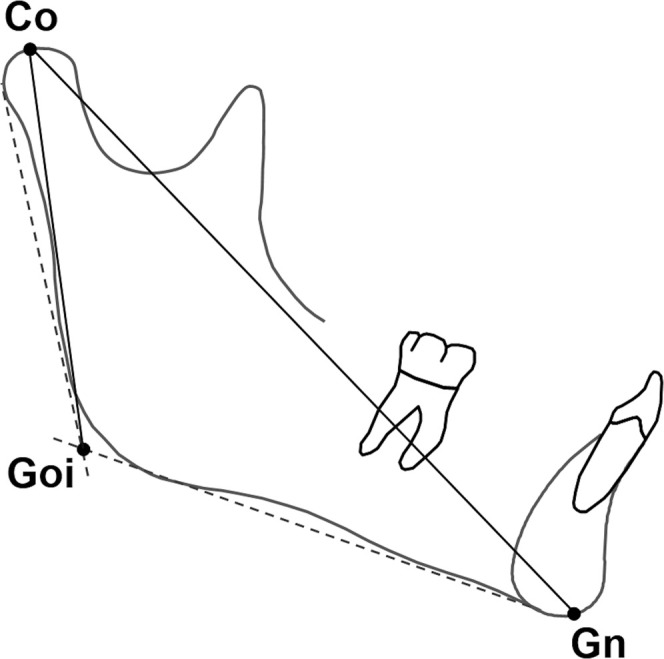
Mandibular growth parameters. Identified landmarks: Co, Condylion; Goi, Gonion Intersection; and Gn, Gnathion. Goi was defined as the point of intersection between the mandibular and ramus planes.
The method error for the cephalometric tracing ranged from 0.15 to 0.81 mm, and inter-/intraoperator agreement levels in the assessment of the CVM stages were above 98%.9 Descriptive statistics of the examined parameters according to each CVM stage have been reported elsewhere.9
Definition of Standing Height Peak and Mandibular Growth Spurt
Annual or annualized increments of standing height, Co-Gn, Co-Goi, and mMG, were calculated for each subject according to annual age intervals from 7–8 years to 15–16 years of age. The individual CVM stage at the beginning of each annual age interval also was identified. Finally, the annual age interval of maximum individual increment for each standing height, Co-Gn, Co-Goi, and mMG, was identified as the one displaying the greatest increment of the whole series (ie, peak in standing height and mandibular growth spurt) and subsequently was used for the diagnostic reliability analysis. For descriptive purposes, median CVM stage and means (± standard deviations) of standing height, Co-Gn, Co-Goi, and mMG were calculated according to each annual age interval for females and males.
Diagnostic Reliability Analysis
Diagnostic reliability analysis included sensitivity, specificity, PPVs, NPVs, and accuracy19 and was calculated for each annual age interval, while overall PPVs were also calculated for the group as a whole. This analysis evaluated the capability of the CS3-4 interval or standing height peak in the identification of the maximum individual increments of Co-Gn, Co-Goi, and mMG. Each diagnostic parameter has been presented as mean and 95% confidence interval.
In particular, “sensitivity” is the probability that CS3-4 or standing height peak is present when the mandibular growth spurt is taking place (true-positive rate); “specificity” is the probability that CS3-4 or standing height peak is absent when the mandibular growth spurt is not present (true-negative rate); “accuracy” represents the proportion of true results (both true positive and true negative); and “PPV” is the proportion of positive test subjects (positive for the CS3-4 or standing height peak) on the true-positive subjects (undergoing the mandibular growth spurt). On the contrary, “NPV” is the proportion of test-negative subjects (ie, negative for the CS3-4 or standing height peak) on the true-negative subjects (not undergoing the mandibular growth spurt).
The Interactive Stats Calculator (http://ktclearinghouse.ca/cebm/practise/ca/calculators/statscalc) was used to perform the statistical analyses.
RESULTS
Results on the diagnostic reliability of the CVM stages and standing height peak in the identification of the mandibular growth spurt for each mandibular growth parameter and according to each annual age interval are summarized in Tables 1 and 2, respectively. Since very few peaks in any parameter were seen at 7–8-, 14–15-, and 15–16-year annual age intervals (ie, very few positive cases with almost all negative cases), these intervals were not used for the diagnostic reliability analysis. The number of cases in which peaks were seen for each standing height, Co-Gn, Co-Goi, and mMG, for the other age intervals ranged from 1 to 8. Generally, the CS3-4 and standing height peak showed similar behaviors, with a slightly better diagnostic reliability seen for Co-Goi and mMG, as compared to that for Co-Gn, and for younger annual age intervals, as compared to those for older age intervals.
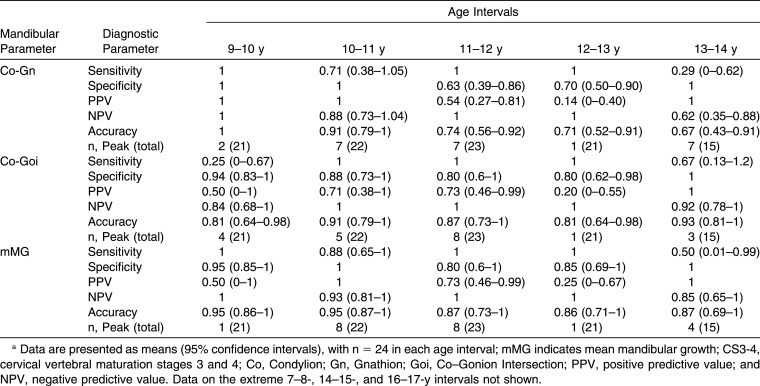
Table 1.
Diagnostic Reliability of the CS3-4 in the Identification of the Mandibular Growth Parameters Peaks According to Each Annual Age Interval from 9 to 14 Yearsa
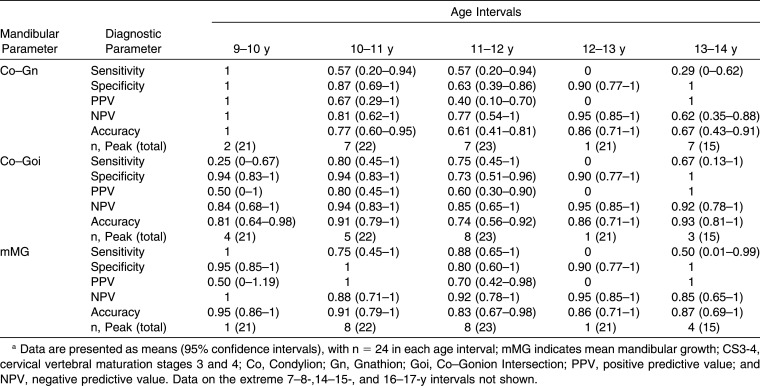
Table 2.
Diagnostic Reliability of the Standing Height Peak in the Identification of the Mandibular Growth Parameters Peaks According to Each Annual Age Interval from 9 to 14 yearsa
By excluding the 9–10 years interval, for which all the parameters were equal to 1, analyses regarding the CS3-4 yielded sensitivity values between 0.29 and 1.0, specificity values between 0.63 and 1.0, PPVs between 0.14 and 1.0 NPVs between 0.62 and 1.0, and accuracy values between 0.71 and 0.95 (Table 1). Analyses regarding the standing height peak yielded sensitivity values between 0 and 0.88, specificity values between 0.63 and 1.0, PPVs between 0 and 1.0, NPVs between 0.62 and 1.0, and accuracy values between 0.61 and 0.95 (Table 2).
Overall PPVs of CS3-4 in the identification of Co-Gn, Co-Goi, and mMG were 0.63 (0.43–0.82), 0.75 (0.58–0.92), and 0.83 (0.68–0.98), respectively. Slightly lower overall PPVs were seen for the standing height peak in the identification of Co-Gn, Co-Goi, and mMG that were 0.50 (0.30–0.70), 0.58 (0.39–0.78), and 0.79 (0.63–0.95), respectively.
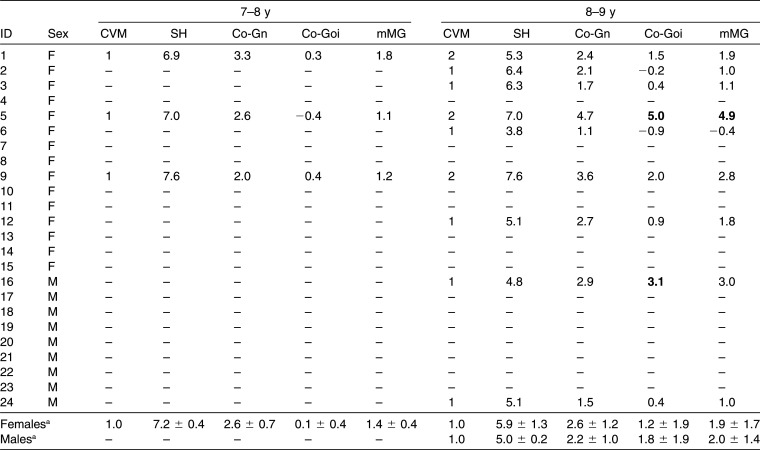
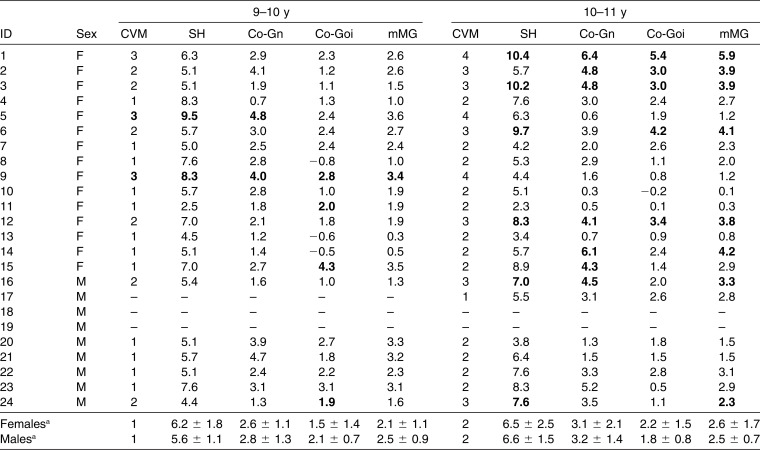
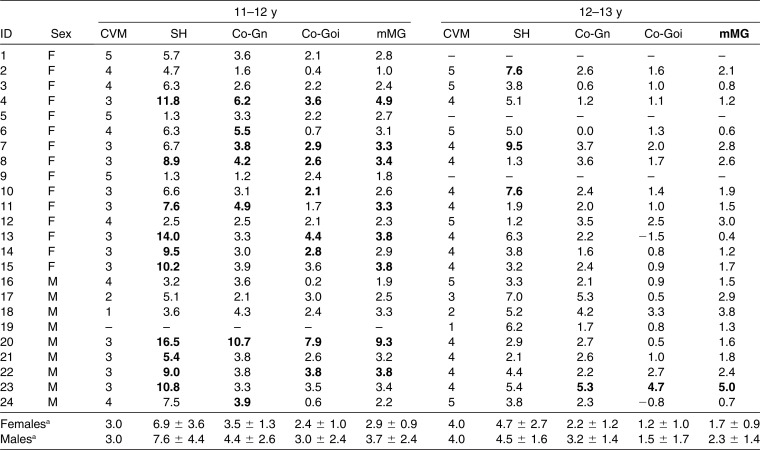
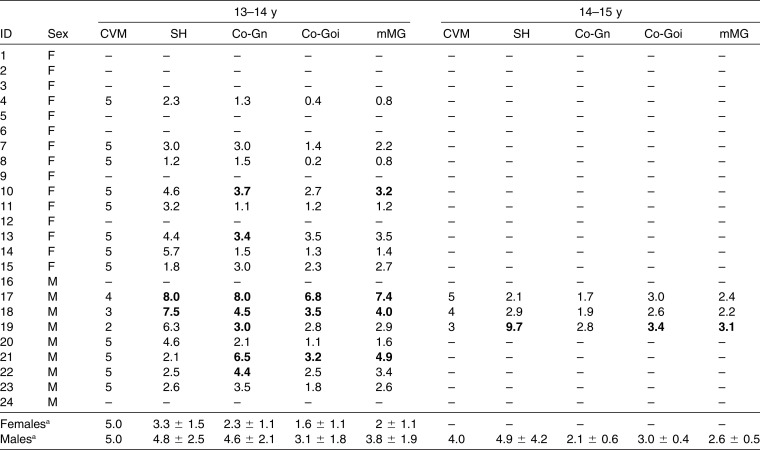
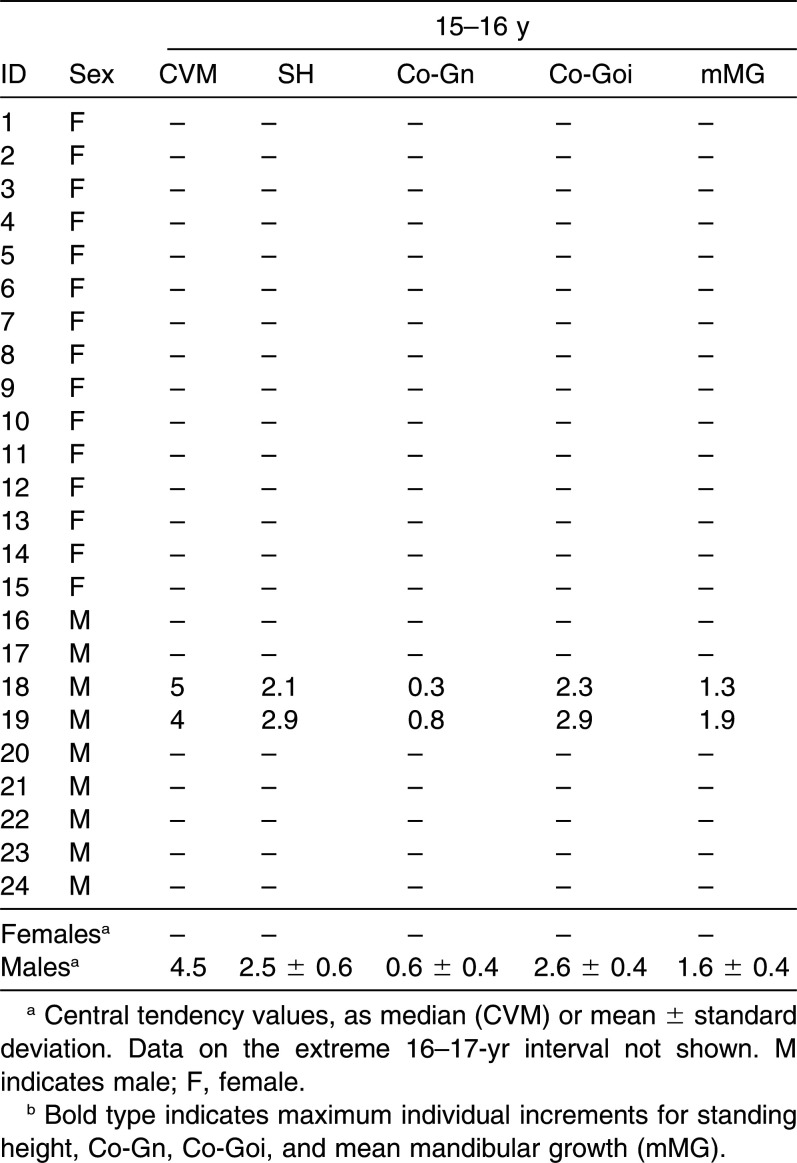
Detailed individual and median/mean data on the CVM stages and corresponding annual increments in standing height, Co-Gn, Co-Goi, and mMG according to the different annual age intervals are summarized in the Appendix.
DISCUSSION
The diagnostic accuracy of the CVM method and of longitudinal measurements of standing height has been based conjecturally on correlation analyses. For the first time, the diagnostic accuracy of both CVM interval CS3-4 and standing height peak in the identification of the mandibular growth spurt has been reported in the current study to range between 0.61 and 0.95, depending primarily on the mandibular growth parameter used.
Previous studies on growth indicators and on the mandibular growth spurt have reported contrasting results of negligible,8,20–22 moderate,7,23,24 or noteworthy13,25 correlations. However, significant differences in study design, cephalometric recordings, and data analysis have to be taken into account; comparisons of the conclusions of the above studies should be undertaken with caution. In several other studies,7,12,14,23–25 the landmark Articulare was used instead of the landmark Condylion to assess the posterior end point of the mandible. The problem with Articulare is that it is not an anatomical landmark that pertains to the mandible exclusively. Other reasons for conflicting results among studies may reside in the repeatability for the CVM staging that was unsatisfactorily reported8 or not reported at all.22
A recent longitudinal investigation by Engel and coworkers8 reported poor capability of the CVM method in the identification of the mandibular growth spurt. This investigation included skeletal Class II females in whom the mandibular growth spurt is expected to be minimal.26 Moreover, this study8 used linear models according to annual age increments, in which the initial stage, rather than corresponding CVM stages, of each interval was considered. Interestingly, the present data indicated that when clustering subjects according to annual age intervals and sex (see Appendix), the corresponding mean mandibular growth increments masked individual spurts as a result of large variation in the age at which the pubertal spurt occurred across subjects.
In the current study, the Co-Goi spurt (ie, mandibular ramus height), appears to be diagnosed more reliably by both the CS3-4 interval and standing height peak as compared to the Co-Gn spurt (ie, total mandibular length; Tables 1 and 2). Moreover, the CS3-4 interval and standing height peak also appear to have a slightly better diagnostic capability in the identification of the mMG spurt. The use of a combined parameter of mandibular growth may have the advantage of taking into account the growth of the mandibular ramus as well, thus overcoming some limitations intrinsic to basic cephalometry.27
Generally, for each mandibular growth parameter, and regardless of the annual age intervals, the standing height peak and CS3-4 interval appeared to have similar specificity and sensitivity (Tables 1 and 2). In addition, the accuracy was similar between these two growth indicators, but lower for the identification of the Co-Gn spurt and greater for the mMG. However, given the sample size and retrieved confidence intervals used in the current study, a differential behavior between these two growth indicators cannot be excluded.
In the present study, NPVs generally were high. This finding was due to the relatively large number of true-negative cases in each annual age interval cluster. Therefore, when dealing with such a situation, an important diagnostic parameter is the PPV, which gives an indication of the capability of a given growth indicator to identify the mandibular growth spurt, regardless of the number of true-negative cases. By analyzing the PPVs in combination with the frequency distributions of the different mandibular growth parameters, a general tendency for the Co-Goi and mMG to be better identified by the growth indicators can be observed (Tables 1 and 2).
According to the overall PPVs of the whole sample, 15, 18, and 20 out of 24 subjects (63%, 75%, and 83%, respectively) showed CS3-4 occurring at the beginning of the annual age interval where Co-Gn, Co-Goi, and mMG, respectively, showed peaks. On the other hand, 12, 14, and 19 subjects (50%, 58%, and 79%, respectively) showed a standing height peak occurring during the same age interval with Co-Gn, Co-Goi, and mMG peaks, respectively.
Overall, both the standing height peak and CS3-4 show a satisfactory capability in the identification of the mandibular growth spurt (defined as Co-Goi or mMG increments), with the mandibular growth spurt being undiagnosed by these parameters in less than in one out of five subjects. Chronological age remains even less reliable according to previous4,28,29 and present evidence. The mandibular growth spurt may occur very early or late in several subjects (see Appendix), making the use of a determined age range22 unreliable.
Of note, fine transitional changes in the cervical vertebral morphology may be responsible for determining a pubertal or nonpubertal stage; training is required to assess CVM stages reliably, especially at stages CS4 and CS5.30 Although the mandibular growth spurt has been seen herein to occur generally the year after the appearance of CS3, in some cases it may occur in the interval between CS4 and CS5 (Appendix). Therefore, a functional orthopedic treatment requiring the inclusion of the mandibular growth spurt in the active treatment period should last until attainment of CS5. The present evidence thus is consistent with recent meta-analyses showing the skeletal responses to functional treatment of Class II malocclusion in pubertal patients according to CVM staging.2,3,31
On the other hand, the use of the standing height requires several measurements repeated at regular intervals to construct an individual curve of growth velocity, but it has the advantage of being noninvasive. From a clinical perspective, therefore, the recording of standing height may be useful when a recent head film is not available or when CVM staging is unclear. However, when CVM staging is unclear or unavailable, the use of further indicators, such as the middle phalanx maturation method,32 may be indicated.
As a limitation, the present investigation was carried out on a limited sample size from old data sets from the UMGS, from which the CVM method was partially derived.1 Nevertheless, provided herein is a simple procedure to elucidate the role of growth indicators in the identification of mandibular growth spurts on an individual basis.
CONCLUSIONS
The CS3-4 interval and the peak in standing height show similar but variable accuracy in the identification of the mandibular growth spurt that reaches satisfactory levels when the Co-Goi and mMG increments are examined.
Both the CS3-4 interval and standing height peak may be used in routine clinical practice to enhance efficiency of treatments requiring the inclusion of the mandibular growth spurt in the active treatment period.
Appendix.
The Individual Cervical Vertebral Maturation (CVM) Stages and Corresponding Following Annual Increments in Standing Height (SH; in cm), Condylion (Co)–Gnathion (Gn), Co–Gonion Intersection (Goi), and Mean Mandibular Growth (mMG; in mm) According to Each Annual Age Intervala
Appendix.
Extended.
Appendix.
Extended.
Appendix.
Extended.
Appendix.
Extended.
REFERENCES
- 1.Baccetti T, Franchi L, McNamara JA., Jr The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 2.Perinetti G, Primožič J, Furlani G, Franchi L, Contardo L. Treatment effects of fixed functional appliances alone or in combination with multibracket appliances: a systematic review and meta-analysis. Angle Orthod. 2015;85:480–492. doi: 10.2319/102813-790.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Franchi L, Contardo L. Treatment Effects of Removable Functional Appliances in Pre-Pubertal and Pubertal Class II Patients: A Systematic Review and Meta-Analysis of Controlled Studies. PLoS One. 2015;28:10:e0141198. doi: 10.1371/journal.pone.0141198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baccetti T, Franchi L, De Toffol L, Ghiozzi B, Cozza P. The diagnostic performance of chronologic age in the assessment of skeletal maturity. Progr Orthod. 2006;7:176–188. [PubMed] [Google Scholar]
- 5.Flores-Mir C, Nebbe B, Major PW. Use of skeletal maturation based on hand-wrist radiographic analysis as a predictor of facial growth: a systematic review. Angle Orthod. 2004;74:118–124. doi: 10.1043/0003-3219(2004)074<0118:UOSMBO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon JP. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr Rev. 2003;24:668–693. doi: 10.1210/er.2002-0019. [DOI] [PubMed] [Google Scholar]
- 7.Soegiharto BM, Moles DR, Cunningham SJ. Discriminatory ability of the skeletal maturation index and the cervical vertebrae maturation index in detecting peak pubertal growth in Indonesian and white subjects with receiver operating characteristics analysis. Am J Orthod Dentofacial Orthop. 2008;134:227–237. doi: 10.1016/j.ajodo.2006.09.062. [DOI] [PubMed] [Google Scholar]
- 8.Engel TP, Renkema AM, Katsaros C, Pazera P, Pandis N, Fudalej PS. The cervical vertebrae maturation (CVM) method cannot predict craniofacial growth in girls with Class II malocclusion. Eur J Orthod. 2015 doi: 10.1093/ejo/cju085. doi: [DOI] [PubMed] [Google Scholar]
- 9.Franchi L, Baccetti T, McNamara JA., Jr Mandibular growth as related to cervical vertebral maturation and body height. Am J Orthod Dentofacial Orthop. 2000;118:335–340. doi: 10.1067/mod.2000.107009. [DOI] [PubMed] [Google Scholar]
- 10.Mitani H, Sato K. Comparison of mandibular growth with other variables during puberty. Angle Orthod. 1992;62:217–222. doi: 10.1043/0003-3219(1992)062<0217:COMGWO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Fudalej P, Bollen AM. Effectiveness of the cervical vertebral maturation method to predict postpeak circumpubertal growth of craniofacial structures. Am J Orthod Dentofacial Orthop. 2010;137:59–65. doi: 10.1016/j.ajodo.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 12.Bishara SE, Jamison JE, Peterson LC, DeKock WH. Longitudinal changes in standing height and mandibular parameters between the ages of 8 and 17 years. Am J Orthod. 1981;80:115–135. doi: 10.1016/0002-9416(81)90213-x. [DOI] [PubMed] [Google Scholar]
- 13.Gu Y, McNamara JA., Jr Mandibular growth changes and cervical vertebral maturation. a cephalometric implant study. Angle Orthod. 2007;77:947–953. doi: 10.2319/071006-284.1. [DOI] [PubMed] [Google Scholar]
- 14.O'Reilly MT, Yanniello GJ. Mandibular growth changes and maturation of cervical vertebrae—a longitudinal cephalometric study. Angle Orthod. 1988;58:179–184. doi: 10.1043/0003-3219(1988)058<0179:MGCAMO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Moore RN, Moyer BA, DuBois LM. Skeletal maturation and craniofacial growth. Am J Orthod Dentofacial Orthop. 1990;98:33–40. doi: 10.1016/0889-5406(90)70029-C. [DOI] [PubMed] [Google Scholar]
- 16.Perinetti G, Contardo L, Gabrieli P, Baccetti T, Di Lenarda R. Diagnostic performance of dental maturity for identification of skeletal maturation phase. Eur J Orthod. 2012;34:487–492. doi: 10.1093/ejo/cjr027. [DOI] [PubMed] [Google Scholar]
- 17.Flores-Mir C, Burgess CA, Champney M, Jensen RJ, Pitcher MR, Major PW. Correlation of skeletal maturation stages determined by cervical vertebrae and hand-wrist evaluations. Angle Orthod. 2006;76:1–5. doi: 10.1043/0003-3219(2006)076[0001:COSMSD]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Lamparski DG. Skeletal Age Assessment Utilizing Cervical Vertebrae [dissertation] Pittsburgh, PA: The University of Pittsburgh; 1972. [Google Scholar]
- 19.Greenhalgh T. How to read a paper. Papers that report diagnostic or screening tests BMJ. 1997;315:540–543. doi: 10.1136/bmj.315.7107.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ball G, Woodside D, Tompson B, Hunter WS, Posluns J. Relationship between cervical vertebral maturation and mandibular growth. Am J Orthod Dentofacial Orthop. 2011;139:e455–e461. doi: 10.1016/j.ajodo.2010.01.035. [DOI] [PubMed] [Google Scholar]
- 21.Beit P, Peltomaki T, Schatzle M, Signorelli L, Patcas R. Evaluating the agreement of skeletal age assessment based on hand-wrist and cervical vertebrae radiography. Am J Orthod Dentofacial Orthop. 2013;144:838–847. doi: 10.1016/j.ajodo.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 22.Mellion ZJ, Behrents RG, Johnston LE., Jr The pattern of facial skeletal growth and its relationship to various common indexes of maturation. Am J Orthod Dentofacial Orthop. 2013;143:845–854. doi: 10.1016/j.ajodo.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 23.Grave KC. Timing of facial growth: a study of relations with stature and ossification in the hand around puberty. Aust Orthod J. 1973;3:117–122. [PubMed] [Google Scholar]
- 24.Tofani MI. Mandibular growth at puberty. Am J Orthod. 1972;62:176–195. doi: 10.1016/0002-9416(72)90141-8. [DOI] [PubMed] [Google Scholar]
- 25.Fishman LS. Radiographic evaluation of skeletal maturation. A clinically oriented method based on hand-wrist films. Angle Orthod. 1982;52:88–112. doi: 10.1043/0003-3219(1982)052<0088:REOSM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Stahl F, Baccetti T, Franchi L, McNamara JA., Jr Longitudinal growth changes in untreated subjects with Class II division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2008;134:125–137. doi: 10.1016/j.ajodo.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 27.Bookstein FL. On the cephalometrics of skeletal change. Am J Orthod. 1982;82:177–198. doi: 10.1016/0002-9416(82)90138-5. [DOI] [PubMed] [Google Scholar]
- 28.Fishman LS. Chronological versus skeletal age, an evaluation of craniofacial growth. Angle Orthod. 1979;49:181–189. doi: 10.1043/0003-3219(1979)049<0181:CVSAAE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Hagg U, Taranger J. Maturation indicators and the pubertal growth spurt. Am J Orthod. 1982;82:299–309. doi: 10.1016/0002-9416(82)90464-x. [DOI] [PubMed] [Google Scholar]
- 30.Perinetti G, Caprioglio A, Contardo D. Visual assessment of the cervical vertebral maturation stages: a study of diagnostic accuracy and repeatability. Angle Orthod. 2013;84:951–956. doi: 10.2319/120913-906.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franchi L, Contardo L, Primožič J, Perinetti G. Clinical alteration of mandibular growth: what we know after 40 years. In: McNamara JA Jr, editor. The 40th Moyers Symposium Looking Back … Looking Forward Craniofacial Growth Series Center for Human Growth and Development University of Michigan. Ann Arbor, Mich: Needham Press; 2014. pp. 263–285. [Google Scholar]
- 32.Perinetti G, Perillo L, Franchi L, Di Lenarda R, Contardo L. Maturation of the middle phalanx of the third finger and cervical vertebrae: a comparative and diagnostic agreement study. Orthod Craniofac Res. 2014;17:270–279. doi: 10.1111/ocr.12052. [DOI] [PubMed] [Google Scholar]