Abstract
Background
Recent studies have indicated that disrespectful/abusive/coercive service by skilled care providers in health facilities that results in actual or perceived poor quality of care is directly and indirectly associated with adverse maternal and newborn outcomes. According to the 2016 Ethiopian Demography and Health Survey, only 26% of births were attended by qualified clinicians, with a maternal mortality rate of 412 per 100,000 live-births. Using seven categories developed by Bowser and Hill (2010), this study looked at disrespect and abuse experienced by women in labor and delivery rooms in health facilities of Borena Ddistrict, South Wollo, Ethiopia.
Methods
A facility-based cross-sectional study was conducted among 374 immediate postpartum women in Borena District from January 12 to March 12, 2020. Systematic sampling was used to access respondents to participate in a structured, pre-tested face-to-face exit interview. Data were entered into EpiData version 4.6 and exported to SPSS version 25 for analysis. Finally, bivariable and multivariable logistic regression analysis were performed to declare statistically significant factors related to maternal disrespect and abusive care in Borena District at a p-value of < 0.05 and at 95% CI.
Result
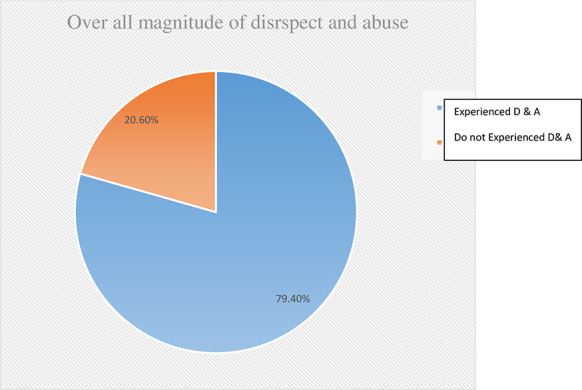
Almost four out of five (79.4%) women experienced at least one type of disrespect and abuse during facility-based childbirth. The most frequently reported type of disrespect and abuse was non-consented care 63.7%. Wealth index [AOR = 3.27; 95% CI: (1.47, 7.25)], type of health facility [AOR = 1.96; 95% CI: (1.01, 3.78)], presence of companion(s) [AOR = 0.05; 95% CI: (0.02, 0.12)], and presence of complications [AOR = 2.65; 95% CI: (1.17, 5.99)] were factors found to be significantly related to women experiencing disrespect and abuse.
Conclusion
The results showed that wealth index, type of health facility, presence of companion(s), and birth complications were found to be significant factors. Therefore, health personnel need to develop interventions that integrate provider’s behavior on companionship and prevention of complications across facilities to reduce the impact of disrespectful and abusive care for laboring women.
Background
Disrespect and abuse (D&A) is described as mistreatment, obstetric violence, or dehumanized care, and is a violation of a woman’s rights during maternity care [1]. According to Brower and Hills, disrespect and abuse is divided into seven major categories: physical abuse, non-confidential care, non-dignified care, non-consented care, discrimination, detention, abandonment/neglect of care [2, 3].
Because motherhood is particular to women, issues of gender equity sit at the core of maternity care. It is essential that the idea of safe motherhood be extended beyond the prevention of morbidity or mortality to include respect for women’s basic human rights, including respect for women’s autonomy, dignity, feelings, choices, and preferences, including decisions about who is present at a birth [4, 5].
A key component of the strategy to lessen maternal morbidity and mortality has been to increase numbers of skilled birth attendants and facility-based childbirths. While global skilled birth attendance rates have risen by 12% in developing regions over the past two decades, almost one-third of women in these regions still deliver without a skilled birth attendant [6]. For that reason, maternal health efforts worldwide are shifting from an emphasis on boosting service utilization to improving quality of care. This alteration has been supplemented by a emergent body of work on respectful maternity care during facility-based childbirth [7].
Respectful maternity care (RMC) is a universal human basic right that is due to every childbearing woman in every health system around the world and to be provided to all women in a way that preserves their dignity, privacy, and confidentiality, safeguards freedom from harm and mistreatment, and empowers informed choice and uninterrupted care during maternity care [8].
Globally, RMC is gaining much-deserved recognition and attention from experts working in the field of reproductive health. Disrespect and abuse in maternal and child health care delivery prevents women from seeking proper health services [1]. The laboring process is an experience with deeply personal, cultural, and psychological significance, and because motherhood is specific to women, gender equity and gender violence are also at the core of maternity care [9].
Even though significant improvement in maternal health was observed between 1990 and 2015, maternal mortality continues to be a public health problem globally. In 2015, an estimated 303,000 women lost their lives due to easily avoidable pregnancy and childbirth-related problems worldwide, 99% of which occurred in low- and middle-income countries [10].
In sub-Saharan Africa (SSA), over 162,000 women still die each year during pregnancy and childbirth. Most of those deaths are within 24 hours after delivery [11]. The Ethiopian maternal mortality rate (MMR) is one of the highest in the world. According to EDHS, about 412 mothers die for each 100,000 live births in Ethiopia whereby the majority of deaths occur within 48 hours after delivery [12].
Globally, maternity care often fails to go beyond the prevention of morbidity or mortality to encompass respect for women’s basic human rights. For example, 56%, 50%, and 46% of respondents in one study reported a lack of privacy, lack of informed consent, and verbal abuse, respectively [13]. In Africa, 62% of health providers do not explain procedures to women before delivery [14]. In SSA countries, the overall prevalence of D & A reported across the five studies ranged from 15% to 98% [15]. Moreover, studies done in Ethiopia revealed rates of D&A that ranged from 40% to 92.5% and that approximately 4% to 39% women were disrespected and abused specifically by non-consented care (lack of informed consent) before delivery procedures and abandonment/neglect of care (women is left without care/attention) respectively [14, 16–19].
Disrespect and abuse of women during facility-based maternity care has multiplicative effects. First, it can lead to a human rights violation; second, it can prevent women from utilizing maternal health services in health facilities; third, it may also erode satisfaction and trust in the health system and lead to poor pregnancy outcomes [6, 20–22] On the other hand, respectful maternity care can contribute to the timely provision of care, improved patient–provider communication, and increased adherence to treatments and maternal health service utilization, all of which can improve maternal and neonatal effects [22–25].
The World Health Organization (WHO) quality-of-care dimension recommends respectful maternal care during facility-based maternity care as a key strategy for improvement of quality of maternity services, to reduce disrespect and abuse as well as maternal mortality and morbidity [26]. But evidence shows that there is increasing disrespect and abuse and mistreatment of women during labor, delivery, and post-delivery and this is the main barrier to seeking skilled maternity care throughout the world [15, 22, 27].
Although there has been an improvement in maternity health services in Ethiopia—antenatal care (ANC) coverage increased from 62% to 74% however, only 34% of new mothers attended postnatal skilled care, a rate that is still low [12, 28]. It shows that maternal health service access only not guaranteed for ensured maternal satisfaction and quality care during childbirth and postnatal care without quality health care and maintain women’s right to health [29, 30].
In addition to geographic, financial, and cultural barriers to care, disrespect and abuse are serious obstacles to utilization of maternal health services. They are associated with women’s feelings of being overlooked, being informed of difficult news without proper preparation, being subjected to repetitive examinations without a reason being properly communicated, companions being disallowed, and being left unattended during facility-based maternity care [31]. Moreover, disrespect and abuse during childbirth are attributed to service delivery level factors such as lack of infrastructure and lack of responsibility mechanisms in the facility, and individual-level factors including the mothers’ socio-demographic characteristics, lack of autonomy, obstetric history and the provider’s perspectives [32–38].
Access to health care facilities has radically improved over the past in Ethiopia. However, the utilization of maternal health care services has remained significantly low [12, 28, 39]. Therefore, the provision of compassionate and respectful maternity care is one of the key factors to promote use of facility-based maternity care [26]. Currently, the Ethiopian federal minister of health (FMOH) aspires to provide compassionate and respectful maternity care (CRC) by reducing the prevalence of disrespect and abuse during delivery and postpartum care in health facilities [40, 41]. Nevertheless, the magnitude of disrespect and abuse and associated factors during facility-based childbirth in Ethiopia is not well known; this study was focused on adding its findings to this knowledge.
Methods and materials
Study design and setting
A facility-based cross-sectional study was conducted in Borena public health facilities from January 12 to March 12, 2020. Borena is one of the 23 districts (woredas) in the South Wollo zone. It is surrounded by other districts, by Leganbo to the east, Gojjam to the west, Wagdi to the south, and Saint to the north. The total land area of Borena is 5560km2 of which 65% is highland area. The total population was 202,832 in 2012 E.C. (Ethiopian Calendar) as projected from the 2007 census. In Borena is the town of Mekane-Selam, which is located 180 km from Dessie (the city of South Wollo); 281 km from Bahir-Dar (the center of the Amhara region) and 581 km from Addis Ababa (the capital city of Ethiopia). There are 39 kebeles (4 urban and 35 rural) and one primary hospital, 7 health centers (one urban and 6 rural), and 36 health posts. A total of 5,283 mothers gave birth in Borena health facilities in the 2011 budget year (Borena Woreda Health Office Annual Report, 2011).
Population
All women living in Borena were the source population of the study while all women who gave birth in selected public health facilities of Borena during the data collection period were used as the study population. Those women who were critically ill and referred to others health facilities were excluded from the study.
Sample size determination and sampling procedures
The sample size required for the first specific objective was calculated based on a single population proportions formula with the following assumptions: Prevalence of disrespect and abuse during labor and delivery 67.1% [17], 95% confidence level, 10% non- response, 5% margin of error.
Thus, the final sample size found was 374 after adding 10% non-response rate.
The sample size for the second specific objective was determined using Epi-info version 7.1 software by considering three variables from previous studies but the final sample sizes determined by this software were less the above sample size determined (374). Therefore, the final sample size used for this study was 374.
In Borena there were 8 public health facilities, of which 5 (Mekane-Selam Hospital (187) n1 = 185; Mekane-Selam Health Center (30) n2 = 29; Tewa Health Center (45) n3 = 44; Galemot Health Center (60) n4 = 58; and Dilfrie Health Center (60) n5 = 58) were selected for the study by simple random sampling. From these five public health facilities, the delivery numbers from February and March, 2011 E.C. were taken from the facilities’ registration books and then the calculated sample size was proportionally allocated based on number of deliveries in those two months in each facility. Finally, using systematic random sampling, every 3rd woman who was eligible and available during the data collection period was included in an exit interview at each respective health facility.
Study variables
The dependent variable of this study was disrespect and abuse (yes/no) while the independent variables were socio-demographic related factors including age, residence, marital status, religion, educational background, economic status; obstetric history including ANC follow-up, parity, complications during labor and delivery, time of delivery, mode of delivery; health care providers- and facility type-related factors including sex of health care provider, type of health facilities, type of health professionals; and individual-related factors including HIV status, history of previous institutional delivery, intention to deliver at health facilities, presence of companion, and decision making power on health issues.
Operational definitions
Disrespect and abuse (D & A) were measured by seven performance standards (types of disrespect and abuse) including physical abuse, non-consented care, non-confidential care, non-dignified care, discriminated care, neglect of care, and detention in the health facility. Accordingly, those women who replied ‘yes’ to at least one form of disrespect and abuse were labeled as being subjected to disrespect and abuse during labor and delivery services. A total of 22 verification criteria of D & A were used to measure the seven performance standards in the composite scale [42].
Physical abuse
Women who were not protected from physical harm or ill-treatment [2]. Measured by 5 verification criteria including 1. A health provider physically hit or slapped, pinched or pushed the mother and/or 2. A health provider verbally insulting the mother and/or 3. A health provider restricted the mother from drinking any fluid throughout the labor course unless medically necessitated and/or 4. The birth attendant pushed a mother’s tummy down to deliver the baby (used fundal pressure) and/or 5. The care providers did not allow the mother to assume the position of her choice during the birth. A woman who answered ‘yes’ to at least one criterion was considered to have been physically abused at the time of childbirth.
Non-consented care
Women’s right to information, informed consent, and choices/preferences were not protected. Measured by 5 standard verification criteria including 1. The care provider did not introduce themselves and greet mother and her support person and/or 2. The provider did not encourage the mother and her companion to ask questions and/or 3. The provider did not respond to the mother’s question with politeness and/or 4. The provider did not explain what was being done and what to expect throughout labor and during examinations; and/or 5. a health care provider did not obtain consent or permission before any procedure. If a woman answered ‘yes’ to at least one of the criteria, she was considered as having been abused by non-consented care at the time of childbirth.
Non-confidential care
A woman’s confidentiality and privacy was not protected, measured by 3 criteria including 1. The provider did not use drapes or covering to protect the mother’s privacy during any procedure and/or 2. Health providers discussed a mother’s private health information in a manner that others might hear and/or 3. Other persons apart from the care providers were allowed in the room while the mother was giving birth who were able to observe a mother while she was naked on the bed. If A woman answered ’yes’ to at least one of the above criteria, she was considered to have been abused by non-confidential care at the time of childbirth.
Non-dignified care
A woman w not treated with dignity and respect, measured by 3 criteria. 1. A health provider shouted at or scolded the mother and/or 2. The care provider blamed the mother for getting pregnant or for shouting/crying due to the pain of delivery and/or 3. The care providers did not allow the mother’s companion to enter the delivery room. If a woman answered ’yes’ to at least one of the criteria, she was considered as being abused by non-dignified care at the time of childbirth.
Discrimination
A woman received not equitable care, not free from discrimination. Measured by 2 criteria. If 1. A health care provider discriminated by ethnicity, religion, age, and being rural and/or 2. A health care provider discriminated by HIV-positive status. If a woman answered ’yes’ to at least one of the criteria, she was considered to have been abused in discriminatory care at the time of childbirth.
Abandonment/neglect of care
A woman did not get timely care or was left alone without care, measured by 3 criteria. 1. A health provider ignored a mother’s call for help and/or 2. A mother was alone when she gave birth in the health institution because the care providers were not around her and/or 3. A mother encountered a life-threatening condition for which she had shouted for help but could not get anyone to reach her in time. A woman who answered ’yes’ to at least one of the criteria was considered to have been abused by abandonment/neglect of care at the time of childbirth.
Detention in a health facility
A woman was detained or confined against her will, measured by 1 criterion 1. Health care providers detained a mother in the health facility because of payment issues when she had posed damage to the property of the health institution. A woman who answered ’yes’ to this criterion was considered to have been abused by detention at the time of childbirth.
Wealth index
The wealth index is a composite measure of a household’s cumulative living standard. The wealth index is calculated using easy-to-collect data on a household’s ownership of selected assets, such as televisions, radio, materials used for housing construction; and types of water access and sanitation facilities; pets and others.
Data collection tools and procedures
The outcome variable was measured using seven performance standards (types of D & A) and their corresponding verification criteria established by the Maternal and Child Health Integrated Program (MCHIP) [42]. A total of 22 verification criteria for disrespect and abuse were used. For independent variables, questionnaires were adapted after reviewing various literature [16, 17, 43–49]. Generally, the tools consists of three sections; the first section was used to assess socio-demographic characteristics of the mother, the second section was used to assess obstetric and individual-related factors of participants and the third section was used to assess categories of disrespect of women during labor and delivery.
The data were collected by trained collectors using a pretested, structured questionnaire in a face-to-face exit interview from the postnatal care unit. The questionnaire was translated to the local language (Amharic) by language experts before the actual data collection period. Six diploma-holding midwives and three BSC nurses were trained as data collectors and supervisors respectively. The data collectors were assigned to health facilities where they collected the data on each respective participant according to the orientation they had been given on data collection procedures; supervisors and investigators checked the processes and questionnaire responses for consistency and completeness.
Data processing and analysis
Before starting the actual data collection processes, to assure the data quality, high emphasis was given to designing data collection instruments during and after data collection. Questionnaires were developed in English, translated to Amharic, then translated back into English to ensure consistency. Six female diploma-holding midwives were selected to collect the data, and three BSC nurses were recruited as supervisors from non-study area health facilities. One day of training was given to data collectors and supervisors on the aim of the study, the content of the questionnaire, how to ensure confidentiality and privacy and the techniques of the interview. Then, the questionnaires were pre-tested on 5% (19) of the total sample size in the Billi Health Center from outside of study area. After pre-testing, no further adjustments to the data collection tools were made because there were no findings to do so. During data collection process all of the questionnaires were checked for completeness and accuracy onsite.
The collected data were compiled, checked for any inconsistency and missed value, coded, and entered into Epi-data version 4.6 software and exported into SPSS version 25 for data management and analysis. The data were cleaned for missing values through running frequencies and crosstabs. The findings of this study were described using frequencies, percentages, tables, and graphs. Variables with p-value less than 0.25 in bivariable logistic regression were fitted to multivariable logistic regression model. The Hosmer and Lemeshow test was used to check the final model fitness (p-value was > 0.05). Adjusted odds ratio with 95% confidence interval was computed to assess the degree of association between the outcome and independent variables. Finally, variables with a p-value less than 0.05 in the multivariable logistic regression were considered to have a statistically significant association with the outcome variable.
Ethical considerations
Ethical clearance was obtained from Wollo University, College of Health Sciences, and School of Public Health Ethical Review Committee (ERC). A etter of permission to conduct the study was obtained from the administrative office of Borena District Health Office. A letter of permission was also obtained from South Wollo Zonal Health Department and given to the district and health facilities. Written informed consent was obtained from all participants before data collection. They were informed that participating in the study was voluntary and their right to withdraw from the study at any moment during the interview was assured. No personal identifiers were used on data collection forms. The recorded data were not accessed by any third person except the principal investigator, and was kept confidentially and anonymously.
Results
Socio-demographic characteristics of study participants
A total of 369 postnatal women were interviewed with a response rate of 98.7%. About 104 (28.2%) of participants were between 25–29 years old with a mean (±SD) age of 30.05 (±6.42) years. A majority of the women 254 (68.8%) were married and about 219 (59.3%) were Muslim and more than half (62.1%) were housewives by occupation. About 194 (52%) of the women had never attended any formal education whereas nearly one-fifth (21.7%) had attended college and above (Table 1).
Table 1. Socio-demographic characteristics of participating women in Borena District, Amhara Region, Ethiopia, 2020 (n = 369).
| Variable | Category | Frequency (n) | Percent (%) |
|---|---|---|---|
| Age | 15–19 | 11 | 3.0 |
| 20–24 | 64 | 17.3 | |
| 25–29 | 104 | 28.2 | |
| 30–34 | 92 | 24.9 | |
| ≥ 35 | 98 | 26.6 | |
| Marital status | Married | 254 | 68.8 |
| Single | 48 | 13.0 | |
| Divorced | 34 | 9.2 | |
| Widowed | 25 | 6.8 | |
| Separated | 8 | 2.2 | |
| Religion | Muslim | 219 | 59.3 |
| Orthodox | 145 | 39.3 | |
| Protestant | 5 | 1.4 | |
| Ethnicity | Amhara | 354 | 95.9 |
| Oromo | 15 | 4.1 | |
| Educational status | Unable to read and write | 85 | 23.0 |
| Able to read and write | 109 | 29.5 | |
| Primary school (grades 1–8) | 48 | 13.0 | |
| Secondary school (grades 9–12) | 47 | 12.7 | |
| College or above | 80 | 21.7 | |
| Occupation | Housewife | 229 | 62.1 |
| Government employee | 72 | 19.5 | |
| Private business | 23 | 6.2 | |
| Student | 29 | 7.9 | |
| Other* | 16 | 4.3 | |
| Residence | Urban | 224 | 60.7 |
| Rural | 145 | 39.3 | |
| Wealth index | Poor | 147 | 39.8 |
| Medium | 74 | 20.1 | |
| Rich | 148 | 40.1 |
Note:
* = daily laborer, farmer.
Obstetric history of participants
The majority of the participants 346 (93.8%) had ANC follow up during their most recent pregnancy from those, more than half (51.2%) had ANC visit at the health center and about 210 (56.9%) attended all ANC visits (≥4 visits). 188 (50.9%) of women had delivered at a health center for their most recent previous pregnancy, 174 (47.2%) women were allowed their choice to have families/companions enter the labor room during labor and delivery and the majority (64%) of participants had a history of previous delivery at a health facility. The majority (55%) of participants were delivered by spontaneous vaginal delivery for their most recent delivery, and of them, 29% of women had developed some form of complications during delivery/immediately after delivery (Table 2).
Table 2. Obstetric history of women in Borena District, Amhara Region, Ethiopia, 2020 (n = 369).
| Variables | Category | Frequency (n) | Percent (%) |
|---|---|---|---|
| ANC visit | YES | 346 | 93.8 |
| NO | 23 | 6.2 | |
| Place of ANC visit | Hospital | 142 | 38.5 |
| Health center | 189 | 51.2 | |
| Both hospital and HC | 15 | 4.1 | |
| Number of ANC visit | ≥ 4 visits | 210 | 56.9 |
| < 4 visits | 136 | 36.9 | |
| Parity of the women | One | 96 | 26.0 |
| Two | 102 | 27.6 | |
| Three | 69 | 18.7 | |
| Four | 53 | 14.4 | |
| Five and above | 49 | 13.3 | |
| Who made health decisions in the household | Husband | 95 | 25.7 |
| Wife | 82 | 22.2 | |
| Both | 178 | 48.2 | |
| Families/parent | 14 | 3.8 | |
| Type of health facility | Hospital | 181 | 49.1 |
| Health center | 188 | 50.9 | |
| Presence of companions at birth | Yes | 174 | 47.2 |
| No | 195 | 52.8 | |
| History of previous delivery in a health facility | Yes | 236 | 64.0 |
| No | 133 | 36.0 | |
| Sex of health care providers | Female | 129 | 35.0 |
| Male | 127 | 34.4 | |
| Both male and female | 113 | 30.6 | |
| Type/mode of delivery | SVD | 203 | 55.0 |
| Vacuum/forceps delivery | 72 | 19.5 | |
| Cesarean section | 35 | 9.5 | |
| With episiotomy | 59 | 16.0 | |
| Time of delivery | During day time | 170 | 46.1 |
| During night time | 199 | 53.9 |
The magnitude of disrespect and abuse during facility-based childbirth
The results of this study showed that the overall magnitude of disrespect and abuse was 79.4% at 95% CI: (77%, 82%) where four out of five women had experienced at least one form of disrespect during facility-based childbirth (Fig 1).
Fig 1. Overall magnitude of disrespect and abuse (D & A) during facility-based childbirth in Borena District, Amhara region, Ethiopia, 2020 (n = 369).
Categories of disrespect and abuse during facility-based childbirth
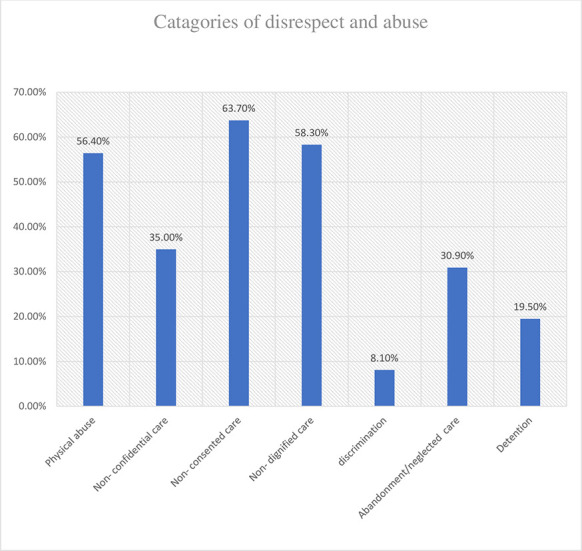
All seven categories of disrespect and abuse with respective standard verification criteria were reported by women in the study. The most reported type of disrespect and abuse was non-consented care 63.7% at 95% CI: (58%, 69%). Under these categories, the most frequently experienced forms of D & A were were having providers who did not introduce themselves or greet the women and her attendant(s) (56.1%), and having providers who did not encourage women or her companion to ask questions (53.1%). The second and third most reported types of disrespect were non-dignified care 58.30% at 95% CI: (53%, 63%), and physical abuse 56.40% at 95%CI: (51%, 61%). Under categories of non-dignified care and physical abuse, the most reported violated criteria were a health care provider’s verbal abuse/insulting language during labor or delivery (40.1%), and not allowing a woman’s companion to enter the delivery room (39.6%). Other types of D & A reported were non-confidential care 35% at 95% CI: (30%, 4%), neglected care 30.9% at 95% CI: (26%, 36%), and detention 19.5% at 95% CI: (15%, 24%). About 8.1% of the women experienced discrimination during facility-based childbirth; for almost half (3.8%) of this group, it was due to their HIV positive status (Table 3) and (Fig 2).
Table 3. Magnitude of disrespect and abuse by verification criteria during facility-based childbirth in Borena District, South Wollo, Amhara region, Ethiopia, 2020 (n = 369).
| Category and type of disrespect and abuse during labor or delivery | Experience | |
| Physical abuse | YES % | NO% |
| Health provider physically hit or slapped, pinched /pushed mother | 83 (22.5) | 286 (77.5) |
| Health provider verbally insulted mother | 148 (40.1) | 221 (59.9) |
| Mother restricted from drinking any fluid unless medically necessitated | 46 (12.5) | 323 (87.5) |
| Birth attendant(s) pushed tummy down to deliver the baby (used fundal pressure) | 95 (25.7) | 274 (74.3) |
| Birth attendant(s) allowed mother to move around (ambulate) during the course of the labor | 143 (38.8) | 226 (61.2) |
| Non-confidential care | ||
| Health providers used curtains or other physical barriers to maintain privacy | 103 (27.9) | 266 (72.1) |
| Health providers discussed mother’s private health information such that others could hear it | 57 (15.4) | 312 (84.6) |
| Person(s) other than the care providers were allowed into the birthing room who could observe mother while naked on the bed | 74 (20.1) | 295 (79.9) |
| Non-consented care | ||
| rovider did not introduce themselves or greet mother | 207 (56.1) | 162 (43.9) |
| providers did not encourage the mother and her companion to ask questions | 196 (53.1) | 173 (46.9) |
| provider did not respond to mother’s question with politeness | 180 (48.8) | 189 (51.2) |
| provider did explain what was being done and what to expect during care | 176 (47.7) | 193 (52.3) |
| Health care provider did not obtain consent or permission before a procedure | 178 (48.2) | 191 (51.8) |
| Non-dignified care | ||
| Health care providers shouted at or scolded mother | 146 (39.6) | 223 (60.4) |
| Care provider blamed mother for getting pregnant or for shouting due to the pain of labor | 101 (27.4) | 268 (72.6) |
| care providers allowed mother’s companion into delivery room | 189 (51.2) | 180 (48.8) |
| Discrimination | ||
| Health care providers discriminated by age, ethnicity, religion, and/or being rural | 23 (6.2) | 346 (93.8) |
| Health care providers discriminated against mother because of HIV+ status | 14 (3.8) | 24 (6.5) |
| Abandonment/neglect of care | ||
| Mother left alone for a period of time without care provider nearby while were in labor | 110 (29.8) | 259 (70.2) |
| Mother gave birth alone because the care providers were not present | 17 (4.6) | 352 (95.4) |
| Mother encountered a life-threatening condition for which she shouted for help but could not get anyone reached you in time | 72 (19.5) | 297 (80.5) |
| Detention in a health facility | ||
| Mother was detained or confined in health facility against her will | 72 (19.5) | 297 (80.5) |
Fig 2. Percentage of each category of disrespect and abuse during facility-based childbirth in Borena District, South Wollo, Amara region, Ethiopia, 2020 (n = 369).
Factors associated with disrespect and abuse of women during child birth
In the multivariable logistic regression model wealth index, type of health facility, companions/families entering labor & delivery room based on woman’s choice, and facing a labor complication were significantly associated with disrespect and abuse after controlling for the confounding effects of all possible factors at P-value<0.05.
Respondents with the category of poor for wealth index were 3.27 times more likely to be disrespected and abused as compared to those women who were in the richest category [AOR = 3.27; 95%CI: (1.47, 7.25)]. Women who delivered in public health centers were nearly two times more likely to be disrespected and abused than those who gave birth at a public hospital [(AOR = 1.96; 95%CI: (1.01, 3.78)]. Respondents whose companions/attendants were encouraged and allowed to enter the labor and delivery room were 95% less likely to be disrespected and abused than those women whose companions were not allowed [(AOR = 0.05; 95%CI: (0.02, 0.12)]. Moreover, women who were facing a complication in a public health facility were 2.65 times more likely to be disrespected and abused than those women who did not face complications [AOR = 2.65; 95%CI: (1.17, 5.99)] (Table 4).
Table 4. Factors associated with disrespect and abuse among women who delivered in public health facilities of Borena District, Amhara region, Ethiopia, 2020 (n = 369).
| Variables | Disrespect and abuse | COR at 95% CI | AOR at 95% CI | |
|---|---|---|---|---|
| YES (%) NO (%) | ||||
| Marital status | ||||
| Single | 45(15.4) | 3(3.9) | 1.75(0.43, 7.14) | 2.18(0.42, 11.27) |
| Married | 188(64.2) | 66(86.8) | 0.33(0.15, 0.76)** | 0.64(0.24, 1.74) |
| Other1 | 60(20.5) | 7(9.2) | 1 | 1 |
| Educational status | ||||
| No formal education | 71(24.2) | 14(18.4) | 1 | 1 |
| Primary education | 145(49.5) | 30(39.5) | 0.95(0.48, 1.91) | 1.97(0.83, 4.72) |
| Secondary or above | 77(26.3) | 32(42.1) | 0.47(0.23, 0.96)* | 1.70 (0.29, 1.67) |
| Residence | ||||
| Rural | 124(42.3) | 21(27.6) | 1.92(1.11, 3.34)* | 0.70(0.29, 1.73) |
| Urban | 169(57.7) | 55(72.4) | 1 | 1 |
| Wealth index | ||||
| Poor | 132(47.1) | 15(19.7) | 3.72(1.96, 7.06)** | 3.27(1.47, 7.25)** |
| Medium | 57(19.5) | 17(22.4) | 1.42(0.74, 2.71) | 1.25(0.56, 2.77) |
| Rich | 104(35.5) | 44(57.9) | 1 | 1 |
| ANC visit | ||||
| YES | 271(92.5) | 75(98.7) | 0.16(0.02, 1.24) | 0.27(0.03, 2.49) |
| NO | 22(7.5) | 1(1.3) | 1 | 1 |
| Type of health facility | ||||
| Health center | 158(53.9) | 30(39.5) | 1.79(1.07, 3.00)* | 1.96(1.01, 3.78)* |
| Hospital | 135(46.1) | 46(60.5) | 1 | 1 |
| Presence of companions | ||||
| YES | 105(35.8) | 69(90.8) | 0.06(0,03, 0.13)** | 0.05(0.02, 0.12)** |
| NO | 188(64.2) | 7(9.2) | 1 | 1 |
| Mode of delivery | ||||
| CS / Assisted delivery | 138(47.1) | 28(36.8) | 1.53(0.91, 2.57) | 0.99(0.49, 2.04) |
| SVD | 155(52.9) | 48(63.2) | 1 | 1 |
| Faced complication | ||||
| YES | 97(33.1) | 10(13.2) | 3.27(1.61, 6.63)** | 2.65(1.17, 5.99)* |
| NO | 196(66.9) | 66(86.8) | 1 | 1 |
| Time of delivery | ||||
| During day time | 142(48.5) | 28(36.8) | 1.61(0.96, 2.71) | 1.46(0.78, 2.74) |
| During night time | 151(51.5) | 48(63.2) | 1 | 1 |
Note:
* indicate that (p value = <0.05, and
** indicated (p value = <0.01).
Discussion
Among women who delivered at a health facility, nearly four out of five (79.4%) experienced at least one type of disrespect and abuse. Wealth index, type of health facility, companions/families allowed to enter labor room based on a woman’s choice, and facing a complication were found to be significantly associated with the outcome variable. It indicated that there is a high magnitude of disrespect and abuse of women during maternity care in this study area, a situation that needs urgent interventions. This result is consistent with a study conducted in Addis Ababa, Ethiopia that showed that the prevalence of disrespect and abuse was 78% [19]. The reason for the similar findings may be that the standard verification criteria in both studies are very similar and both studies focus on the same kinds of public health facilities.
On the other hand, this study’s finding is lower than that of studies conducted in southern Ethiopia 91.7% [50], Tanzania 85.3% [51], Malawi 93.7%[52], and Pakistan 97% [53]. There may be three possible reasons for that difference. First, there were larger sample sizes and time variation in those previous studies. Second, there was a study population difference in that the previous studies excluded women who had delivered by cesarean section and evidence has shown that women who deliver by cesarean section are less likely to experience disrespect and abuse than those who delivered vaginally [47, 54]. This could be because health care providers tend to devote more attention to women indicated for cesarean delivery, in particular, being more likely to strictly attend to informed consent of this group compared to that of women who delivered vaginally. Third, there were variations in data collection, in that the previous studies used a direct observational method, while the current study used an exit interview method. Interviewing participants may be affected by recall bias while data collected via direct observation may be more reliable for recording every activity.
The magnitude of D & A found by this study was higher than found in Addis Ababa, Ethiopia 17.6% [43], northern Ethiopia 75.1% [16], Kenya 20% [55], northwestern Tanzania 73.1% [56], and urban Tanzania 15% [57]. The possible reasons may be variation in sample size [47, 55, 56, 58]; variation among standard verification criteria to measure disrespect and abuse [43, 55, 56, 59, 60]; study setting difference; health care quality implementation program differences; socio-cultural and socio-economic status disparity; geographical variation, and time variation.
This study showed that poor respondents were three times more likely to be disrespected and abused than those women who had a high wealth index level (rich). This result was consistent with a previous studies conducted in Ethiopia [17, 43, 61, 62] and in Gujrat Pakistan [5] that showed that poor women were more likely to experience disrespect and abuse during facility-based maternity care at facility based childbirth. The reason may be that rich women might be more respected and cared for than poor women by facility-based health care providers.
Those women who delivered in a public health center were nearly twice as likely to be disrespected and abused than those women who delivered in a public hospital. Reasons for this finding by the current study may be that heath service deliver in low-level settings is affected by factors such as a lack of standards; a lack of leadership/supervision; poor clinical care; and a lack of multidisciplinary teams and training compared to the higher-level setting [2]. In contrast to findings of this study, some previous studies done in Ethiopia [17, 18] and northern India [49] showed that women who delivered at a public hospital reported at least one more type of disrespect and abuse than those who gave birth at a health center. The possible reason for this may be that in hospitals with higher case numbers and overflowing referrals of complicated cases leading to overcrowding, care providers may be pushed to perform abusive care in contrast to in health centers where there may be relatively fewer complicated cases and care providers are less stretched.
Respondents whose companions/supporters were encouraged and allowed to enter the labor and delivery room based on her choice were 95% less likely to be disrespected and abused than those women whose companions/supporters were not allowed to enter the labor room. This finding is supported by similar studies done in Ethiopia [63–65], Kenya [56], and Malawi [52]. The reasons may be that families of laboring women have an important role in reducing the impact of D & A. The presence of a companion during labor and delivery is a very effective approach to minimizing D & A by health professionals; it also makes women happier, psychologically ready for good motherhood. On the other hand, women felt disappointed with the health system when they were not allowed to have a support person in the delivery room, leading to their overall dissatisfaction with and reluctance to receive facility-based maternity care.
Women who were facing a complication during delivery in a public health facility were twice as likely to be disrespected and abused as those who did not face any complications. This finding is consistent with a similar study done in northern Ethiopia [48], Tanzania [56], and India [49].
The possible reason may be that women who develop complications have to stay a longer time in the health facility, increasing her contact time with care providers and the opportunities for D & A. These women might suffer secondary pain related to the complication in addition to labor pain. Facing complications can lead to stressed labor and poor maternal health effects as a result of frequent and unnecessary examinations by multiple care providers. Neglect of women by health care providers during labor and delivery or poorly skilled attendants may be a consequence of a poor health system.
This study showed that 30.9% of women were neglected during labor and delivery care; about 29.8% left alone without care provider while in labor and needing help and 4.6% gave birth by themselves because the care providers were not around. It showed the low commitment of health care providers. Overall, these findings show a violation of the right to health, the barrier to institutional health care delivery, and factors related to mothers receiving poor quality health care.
Limitations
The limitations of this study were its quantitative design, being based on interview alone, excluding observational form of data collection, and its cross-sectional design that made it difficult to establish temporal relationships between explanatory variables and the outcome variable.
Conclusion
The magnitude of disrespect and abuse was very high (79.4%) as four out of five of women experienced at least one type of disrespect and abuse during facility-based childbirth. Wealth index, type of health facility, women’s companions/families allowed to enter the delivery room, and facing complications during labor and delivery were found to be significantly associated with the experience of disrespect and abuse. Health care managers and health professionals need to develop interventions to reduce the impact of these factors on women’s health, and to improve compassionate and respectful care by health care providers as part of a strategy for the delivery of quality health care.
Acknowledgments
First we would like to thank all study participants for their cooperation in providing the necessary information. We would also thank managers and employees at different level for cooperation, and data collectors and supervisors for the devotion and quality work during data collection.
Acronyms/abbreviations
- ANC
antenatal care
- AOR
adjusted odds ratio
- CI
confidence interval
- COR
crude odds ratio
- CRC
compassionate and respectful caring
- CS
cesarean section
- D & A
disrespect and abuse
- EDHS
Ethiopian Demography and Health Survey
- ERC
Ethical Review Committee
- FMOH
Federal Minister of Health
- HIV
human immunodeficiency viruses
- MCHIP
Maternal and Child Health Integrated Program
- MMR
maternal mortality rate
- RMC
respectful maternal Care
- SD
standard deviation
- SE
standard error
- SPSS
Statistical Package for Social Sciences
- SSA
Sub-Saharan Africa
- SVD
spontaneous vaginal delivery
- WHO
World Health Organization
Data Availability
Access to the data set used in this study is restricted by the Ethical Review Committee of the College of Medicine and Health Sciences, Wollo University, as it contains sensitive participant information. Data access request should be sent to the committee via Asnakew Molla, at amdessie2007@gmail.com.
Funding Statement
Wollo University provided the fund to the principal author for reason that as for postgraduate student thesis. The grant number at Wollo University was CMHS 741/05/12 on 08/05/2012.
References
- 1.Manning A, Schaaf M. Amy Manning 1 & Marta Schaaf 1, with gracious input from members of the Respectful Maternity Care Council guideline. 2015. p. 1–6. [Google Scholar]
- 2.Bowser D, Hill K. Exploring Evidence for Disrespect and Abuse in Facility-Based Childbirth Report of a Landscape Analysis. Harvard Sch Public Heal Univ Res Co, LLC. 2010;1–57. [Google Scholar]
- 3.Panth A, Kafle P. Maternal satisfaction on delivery service among postnatal mothers in a government hospital, Mid-Western Nepal. Obstet Gynecol Int. 2018;2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sudhinaraset M, Afulani P, Diamond-Smith N, Bhattacharyya S, Donnay F, Montagu D. Advancing a conceptual model to improve maternal health quality: The Person-Centered Care Framework for Reproductive Health Equity. Gates Open Res. 2017;1(0):1–14. doi: 10.12688/gatesopenres.12756.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The White Ribbon Alliance for Safe Motherhood. Respectful maternity care: The universal rights of childbearing women. White Ribb Alliance Safe Mother. 2011;1–6. [Google Scholar]
- 6.Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Med. 2015;12(6):1–32. doi: 10.1371/journal.pmed.1001847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Afulani PA, Moyer CA. Comment Accountability for respectful maternity care. Lancet. 2019;6736(19):10–11. doi: 10.1016/S0140-6736(19)32258-5 [DOI] [PubMed] [Google Scholar]
- 8.The White Ribbon Allience. A Guide for Respectful Maternity Care [Internet]. washigton dicy: USAID; 2013. Available at: www.whiteribbonalliance.org/respectfulcare. Date Accessed: October, 2019. [Google Scholar]
- 9.Hill K, Stalls S, Sethi R, Bazan E, Moffson S. Moving Respectful Maternity Care into Practice in Comprehensive MCSP Maternal and Newborn Programs: Operational Guidance DRAFT. USAID. 2018;1–72. [Google Scholar]
- 10.WHO, UNICEF U and the WB. Trends in Maternal Mortality: 1990 to 2015,Trends in Maternal Mortality: 1990 to 2015. WHO, Geneva. 2015; [Google Scholar]
- 11.Darega B, Dida N, Tafese F, Ololo S. Institutional delivery and postnatal care services utilizations in Abuna Gindeberet District, West Shewa, Oromiya Region, Central Ethiopia: A Community-based cross sectional study. BMC Pregnancy Childbirth. 2016;1–7. doi: 10.1186/s12884-015-0735-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Central Statistical Agency [Ethiopia] and ICF International. Ethiopian Demographic and Health Survey 2016 Key Indicators Report. Ethiopians Water Sector Development Program. 2016. 1–49 p.
- 13.Sukmaningrum PS, Performance F, Insurance I, Pendahuluan I, Belakang L, Mohd Hussin MY, et al. Maternal health and respectful maternity care, fact sheet. In: Jurnal Teknologi. 2014. p. 69–73. [Google Scholar]
- 14.Rosen HE, Lynam PF, Carr C, Reis V, Ricca J, Bazant ES. Direct observation of respectful maternity care in five countries: a cross-sectional study of health facilities in East and Southern Africa. BMC Pregnancy Childbirth. 2015;15(396):1–11. doi: 10.1186/s12884-015-0728-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sando D, Abuya T, Asefa A, Banks KP, Freedman LP, Kujawski S, et al. Methods used in prevalence studies of disrespect and abuse during facility based childbirth: Lessons learned Prof. Suellen Miller. Reprod Health. 2017;14(1):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mihret MS. Obstetric violence and its associated factors among postnatal women in a Specialized Comprehensive Hospital, Amhara Region, Northwest Ethiopia. BMC Res Notes. 2019;1–7. doi: 10.1186/s13104-018-4038-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wassihun B, Deribe L, Worede N, Gultie T. Prevalence of disrespect and abuse of women during child birth and associated factors in Bahir Dar town, Ethiopia. Epidemiol Health. 2018;40:e2018029. doi: 10.4178/epih.e2018029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ukke GG, Gurara MK, Boynito WG. Disrespect and abuse of women during childbirth in public health facilities in Arba Minch town, south Ethiopia–a cross-sectional study. PLoS One. 2019;14(4):1–17. doi: 10.1371/journal.pone.0205545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asefa A, Bekele D. Status of respectful and non-abusive care during facility-based childbirth in a hospital and health centers in Addis Ababa, Ethiopia. Reprod Health. 2015;12(1):1–9. doi: 10.1186/s12978-015-0024-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moran AC, Jolivet RR, Chou D, Dalglish SL, Hill K, Ramsey K, et al. A common monitoring framework for ending preventable maternal mortality, 2015–2030: phase I of a multi-step process. BMC Pregnancy Childbirth. 2016;1–13. doi: 10.1186/s12884-015-0735-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Afulani PA, Phillips B, Aborigo RA, Moyer CA. Articles Person-centred maternity care in low-income and middle-income countries: analysis of data from Kenya,. Lancet Glob Heal. 2018;7(1):e96–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–92. doi: 10.1016/S0140-6736(16)31472-6 [DOI] [PubMed] [Google Scholar]
- 23.Downe S, Lawrie TA, Finlayson K, Oladapo OT. Effectiveness of respectful care policies for women using routine intrapartum services: A systematic review. Reprod Health. 2018;15(1):1–13. doi: 10.1186/s12978-017-0439-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Molina RL, Patel SJ, Scott J, Schantz-Dunn J, Nour NM. Striving for Respectful Maternity Care Everywhere. Matern Child Health J. 2016; 12(23):1–7. doi: 10.1007/s10995-016-2004-2 [DOI] [PubMed] [Google Scholar]
- 25.Chou D, Daelmans B, Jolivet RR, Kinney M, Say L. Ending preventable maternal and newborn mortality and stillbirths. BMJ. 2015;351:19–22. doi: 10.1136/bmj.h4255 [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. The prevention and elimination of disrespect and abuse during facility-based childbirth: WHO statement. World Heal Organ. 2015;4. [Google Scholar]
- 27.Sadler M, Santos MJ, Ruiz-Berdún D, Rojas GL, Skoko E, Gillen P, et al. Moving beyond disrespect and abuse: addressing the structural dimensions of obstetric violence. Reprod Health Matters. 2016. May 1;24(47):47–55. doi: 10.1016/j.rhm.2016.04.002 [DOI] [PubMed] [Google Scholar]
- 28.Institute E public health, ICF. Mini Demographic and Health Survey: key indictors [Internet]. Handbook of Federal Countries, 2005. 2019. 136–148 p. Available at: www.DHSprogram.com. Date Accessed: October, 2019. [Google Scholar]
- 29.Berhe A, Bayray A, Berhe Y, Teklu A, Desta A, Araya T, et al. Determinants of postnatal care utilization in Tigray, Northern Ethiopia: A community based cross-sectional study. PLoS One. 2019;14(8):e0221161. doi: 10.1371/journal.pone.0221161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LeFevre A, Mpembeni R, Kilewo C, Yang A, An S, Mohan D, et al. Program assessment of efforts to improve the quality of postpartum counselling in health centers in Morogoro region, Tanzania. BMC Pregnancy Childbirth. 2018;18(1):1–13. doi: 10.1186/s12884-017-1633-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Care MatNdwiga, Charity Charlotte Warren, Abuya Timothy, Lucy Kanya A, et al. PROMOTING RESPECTFUL MATERNITY CARE A TRAINING GUIDE FOR FACILITY-BASED. New York, Population Council. 2014. [Google Scholar]
- 32.USAID. Respectful Maternity Care: Evidence from East and Southern Africa. Jhpiego; 2015.
- 33.Shakibazadeh E, Namadian M, Bohren MA, Vogel JP, Rashidian A, Nogueira Pileggi V, et al. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG An Int J Obstet Gynaecol. 2018;125(8):932–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morton CH, Simkin P. Can respectful maternity care save and improve lives? Birth. 2019;(June):391–5. doi: 10.1111/birt.12444 [DOI] [PubMed] [Google Scholar]
- 35.Nyirenda HT, Mulenga D, Nyirenda T, Choka N, Agina P, Mubita B, et al. Status of Respectful Maternal Care in Ndola and Kitwe Districts of Zambia. Clin Mother Child Heal. 2018;15(2). [Google Scholar]
- 36.Deki S, Choden J. Assess Knowledge, Attitude and Practices of Respectful Maternity Care among nurse midwives in Referral Hospitals of Bhutan. 2018;4(1):1–7. [Google Scholar]
- 37.Orpin J, Puthussery S, Davidson R, Burden B. Women’s experiences of disrespect and abuse in maternity care facilities in BenueState, Nigeria. BMC Pregnancy Childbirth. 2018;18(1):1–9. doi: 10.1186/s12884-017-1633-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shannon A McMahon1*, Asha S George1, Joy J Chebet1, Idda H Mosha2 RNM and PJW. Experiences of and responses to disrespectful maternity care and abuse during childbirth; a qualitative study with women and men in Experiences of and responses to disrespectful maternity care and abuse during childbirth; a qualitative study with women. BMC Pregnancy Childbirth. 2016;(September):1–13. doi: 10.1186/s12884-015-0735-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.CSA. DHS_Ethiopia_20111. Cent Stat Agency Addis Ababa, Ethiop ICF Int Calverton, Maryland, USA. 2011; [Google Scholar]
- 40.Conference A. Proceeding of the 27th Annual Conference of the Ethiopian Public Health Association. 2016; [Google Scholar]
- 41.Bradley S, McCourt C, Rayment J, Parmar D. Midwives’ perspectives on (dis)respectful intrapartum care during facility-based delivery in sub-Saharan Africa: a qualitative systematic review and meta-synthesis. Reprod Health. 2019;16(1):1–16. doi: 10.1186/s12978-018-0662-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.USAID. Respectful Maternity Care Standards, child birth. 2011; Available at: https://www.k4health.org/RMC_Standards. Date Accessed: October, 2019.
- 43.Kitaw M, Tessema M. Respectful maternity care and associated factors among mothers in the immediate post–partum period, in public health facilities of Addis Ababa,. 2019;5(1). [Google Scholar]
- 44.Dynes MM, Twentyman E, Kelly L, Maro G, Msuya AA, Dominico S, et al. Patient and provider determinants for receipt of three dimensions of respectful maternity care in Kigoma Region, Tanzania-April-July, 2016 Prof. Suellen Miller. Reprod Health. 2018;15(1):1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.USAID, Population Council. Promoting Respectful Maternity Care: A Training Guide for Facility-Based Workshops. Popul Counc USAID. 2015; Available at: WWW.Popcouncil.org. Date Accessed: October, 2019. [Google Scholar]
- 46.Azhar Z, Oyebode O, Masud H. Disrespect and abuse during childbirth in district Gujrat, Pakistan: A quest for respectful maternity care. PLoS One. 2018;13(7):1–11. doi: 10.1371/journal.pone.0200318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nawab T, Uzma Erum AA, Najam Khalique, Mohammed A. Ansari AC. Disrespect and abuse during facility‑based childbirth and its sociodemographic determinants–A barrier to healthcare utilization in rural population. J Fam Med Prim Care. 2019;6(2):169–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.B. W, S. Z. Compassionate and respectful maternity care during facility based child birth and women’s intent to use maternity service in Bahir Dar, Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):1–9. doi: 10.1186/s12884-018-1909-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bhattacharya S, Sundari Ravindran TK. Silent voices: Institutional disrespect and abuse during delivery among women of Varanasi district, northern India. BMC Pregnancy Childbirth. 2018;18(1):1–8. doi: 10.1186/s12884-017-1633-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Siraj A, Teka W, Hebo H. Prevalence of disrespect and abuse during facility based child birth and associated factors, Jimma University Medical Center, Southwest Ethiopia. BMC Pregnancy Childbirth. 2019;19(1):1–9. doi: 10.1186/s12884-018-2145-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sando D, Kendall T, Lyatuu G, Ratcliffe H, McDonald K, Mwanyika-Sando M, et al. Disrespect and abuse during childbirth in Tanzania: Are women living with HIV more vulnerable? J Acquir Immune Defic Syndr. 2014;67:S228–34. doi: 10.1097/QAI.0000000000000378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sethi R, Gupta S, Oseni L, Mtimuni A, Rashidi T, Kachale F. The prevalence of disrespect and abuse during facility-based maternity care in Malawi: Evidence from direct observations of labor and delivery. Reprod Health. 2017;14(1):1–10. doi: 10.1186/s12978-016-0263-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hameed W, Avan BI. Women’s experiences of mistreatment during childbirth: A comparative view of home- and facility-based births in Pakistan. PLoS One. 2018;13(3):1–17. doi: 10.1371/journal.pone.0194601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abuya T, Ndwiga C, Ritter J, Kanya L, Bellows B, Binkin N, et al. The effect of a multi-component intervention on disrespect and abuse during childbirth in Kenya. BMC Pregnancy Childbirth. 2015;15(224):1–14. doi: 10.1186/s12884-015-0645-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abuya T, Warren CE, Miller N, Njuki R, Ndwiga C, Maranga A, et al. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PLoS One. 2015;10(4):1–13. doi: 10.1371/journal.pone.0123606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bishanga DR, Massenga J, Mwanamsangu AH, Kim YM, Eorge J, Kapologwe NA, et al. Women’s experience of facility-based childbirth care and receipt of an early postnatal check for herself and her newborn in Northwestern Tanzania. Int J Environ Res Public Health. 2019;16(3):2–16. doi: 10.3390/ijerph16030481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sando D, Ratcliffe H, Mcdonald K, Spiegelman D, Lyatuu G, Mwanyika-sando M, et al. The prevalence of disrespect and abuse during facility-based childbirth in urban Tanzania. BMC Pregnancy Childbirth. 2016;1–10. doi: 10.1186/s12884-015-0735-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Abuya T, Sripad P, Ritter J, Ndwiga C, Warren CE. Measuring mistreatment of women throughout the birthing process: implications for quality of care assessments. Reprod Health Matters. 2018;26(53):48–61. doi: 10.1080/09688080.2018.1502018 [DOI] [PubMed] [Google Scholar]
- 59.Alageswari A. 1Prof. Dr. Manju Bala and 2Prof. Dr. A. Felicia Chitra, 1Msc. Knowledge and Perception of Postnatal Mothers on Respectful Maternity Care–An Explorative Study. 2019;7(3):106–11. [Google Scholar]
- 60.Ogunlaja OA, Fehintola OA, Ogunlaja IP, Popoola G, Idowu A, Awotunde OT, et al. “Respectful maternity care” or “Disrespect and abuse during maternity care”; experience of pregnant women in Ogbomoso, South West Nigeria. Rwanda Med J. 2017;74(3):6–9. [Google Scholar]
- 61.Getachew A, Mph D, Hailemariam NW, Fulasa TB. Respectful Maternity care: A qualitative study on the experience of healthcare providers in public health facilities. Ethiop J Reprodcutive Heal. 2019;11(1):42–51. [Google Scholar]
- 62.Mekonnen A. Disrespectful and abusive maternity care during childbirth in Bale zone Public Hospitals, southeast Ethiopia: Cross- sectional study. Clin Pract. 2019;16:1273, 80. [Google Scholar]
- 63.Gebremichael MW, Worku A, Medhanyie AA, Berhane Y. Mothers ‘ experience of disrespect and abuse during maternity care in northern Ethiopia. Glob Health Action. 2018;11(00):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bobo FT, Kasaye HK, Etana B, Woldie M, Feyissa TR. Disrespect and abuse during childbirth in Western Ethiopia: Should women continue to tolerate? PLoS One. 2019;14(6):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sheferaw ED, Bazant E, Gibson H, Fenta HB, Ayalew F, Belay TB, et al. Respectful maternity care in Ethiopian public health facilities Prof. Suellen Miller. Reprod Health. 2017;14(60):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Access to the data set used in this study is restricted by the Ethical Review Committee of the College of Medicine and Health Sciences, Wollo University, as it contains sensitive participant information. Data access request should be sent to the committee via Asnakew Molla, at amdessie2007@gmail.com.


