Abstract
Objective:
This study examines whether and how parenthood status is associated with two key aspects of health— mental well-being and smoking— among sexual minority adults across three gender identity groups: cisgender gay men, cisgender lesbian women, and transgender gay/lesbian adults.
Background:
Parents tend to report worse health than non-parents due to elevated stress associated with parenting. However, most existing scholarship de facto examines parental status and health among cisgender heterosexual adults. Little research has employed an intersectional approach to focus on parenthood and health differences within sexual minority adults across varying gender identities.
Method:
OLS and logistic regression models were used to analyze data from the 2010 Social Justice Sexuality Project (N = 2,803), a survey of racially diverse sexual and gender minority adults residing in all 50 US states and Puerto Rico.
Results:
In a sample composed predominantly of people of color, parenthood status is related to both mental well-being and smoking status among gay and lesbian adults, but this relationship is inconsistent across cisgender and transgender groups. OLS regression models show that parenthood is positively related to mental well-being among gay and lesbian transgender people, whereas logistic regression results find that parenthood is associated with higher odds of smoking among cisgender gay men.
Conclusion:
These findings suggest that among a sample of sexual and gender minorities composed mostly of people of color, parenthood status is connected with the health and well-being of gay and lesbian adults in ways that depend on gender identity.
Keywords: parents, stress, mental health, behavioral health, LGBTQ, transgender
Parents tend to report worse health and well-being than adults without children in part due to the emotional, physical, and financial stress of childrearing (Umberson et al., 2010). However, this basic finding is becoming increasingly complex as scholarship shows that parenting stressors differ by social contexts such as parental socioeconomic status, gender, race/ethnicity, and family-related policies (Nomaguchi & Milkie, 2020). In particular, a minority stress framework suggests that racial-ethnic and sexual minority parents may experience elevated stress compared to white and heterosexual parents due to higher levels of discrimination experienced in various social interactions and social institutions (Meyer, 2003). Therefore, scholars have called for research that extends beyond a white heterosexual context to examine the effects of parenthood on sexual minority parent families and especially sexual minority parents of color (Reczek, 2020; Thomeer et al., 2018).
In response to this call, existing research shows that gay and lesbian parents tend to have similar or higher levels of stress than heterosexual parents (Bos et al., 2018; Goldberg et al., 2014). The parenting stress and minority stress experienced by gay and lesbian parents are also connected to their mental well-being and health behaviors (Goldberg et al., 2019). However, the majority of this research is limited in that sexual orientation is often based on the designated sex of adults matched to their co-residing partners (i.e., same-sex or different sex couples) rather than direct inquiries about sexual identity. This does not allow for people to self-identify as lesbian, gay, bisexual, or queer (LGBQ), and only accounts for people in same-sex relationships, failing to account for unpartnered gay and lesbian people who make up the majority of the LGBQ population (Gorman et al., 2015). Furthermore, this body of work is limited to a focus on samples predominantly made of white same-sex parents with few studies using samples of people of color. This prevents a full view of how people of color in LGBQ communities are subject to multiple types of minority stress and how this experience may affect their lives as parents and their well-being.
In addition to the importance of examining a sample of sexual minorities that is predominantly composed of racial minorities, intersectional scholars further assert that it is not just sexuality and race, but also a more complex view of gender that is needed to fully understand the relationship between parenthood and health (Thomeer et al., 2018). In this intersectional view, gender identity likely shapes how parenthood influences health among sexual minority people, with previous scholarship consistently demonstrating that in general cisgender mothers experience more parenting stress and have worse health than cisgender fathers (Umberson et al., 2010) (cisgender: people whose gender identity corresponds with their birth sex; hereafter referred to as “cis”). This dynamic in turn contributes to gender disparities in health outcomes between cisgender men and women (Read & Gorman, 2010). While differences between cisgender men and women are important, the vast majority of past research is limited in that it conceptualizes gender as a binary variable of man or woman (often as a proxy for sex, measured as male/female). Instead, a much more complex view of gender identity has emerged in recent intersectional scholarship to include transgender identities (hereafter referred to as “trans”) (Reisner et al., 2016). However, a gap remains in our understanding of how cis and trans gender status matters in the relationship between parenthood and health among gay and lesbian adults.
To address these research gaps, our study applies intersectional and minority stress perspectives to examine how parenthood status matters for well-being among a gender diverse sample of gay- and lesbian-identified adults that are predominantly people of color from the 2010 Social Justice Sexuality Project (SJSP). Specifically, we focus on two indicators of stress: mental well-being and smoking status. We further test the role of gender in these associations across three gender identity groups: cisgender gay men, cisgender lesbian women, and transgender gay/lesbian adults. A focus on how parenthood shapes health with attention to gender variation within a gay and lesbian, predominantly people of color population is an important next step in showing how parenthood experiences vary by the intersection of both gender and sexuality among a sample of mostly racial-ethnic minorities. SJSP allows us to extend existing work based mostly on majority white and partnered samples, considering that gay, lesbian, and transgender populations are more racially diverse than the general population (Gates, 2013) and many prior studies could not examine single parents (e.g., Bos et al., 2018). Notably, this study is not able to examine bisexual parenthood because most existing datasets and in particular the large-scale surveys (including SJSP) do not have sufficient samples of bisexual parents (see Manley & Ross, 2020).
Background
Stress, Parenthood, and Health
Guided by a stress process perspective and based on samples composed mostly of cisgender heterosexual and white adults, recent scholarship establishes that parents have worse mental and physical well-being than the childless due to sustained parenting stress (Evenson & Simon, 2005; Pearlin, 1989; Umberson et al., 2010). All parents are exposed to stressors associated with childrearing including daily hassles, emotional and physical fatigue, economic constraints, increased strain between parenting partners, and work-family conflicts (Nomaguchi & Milkie, 2020; Umberson et al., 2010). Notably, parents of color experience additional stressors such as fears that their child may experience violence at the hands of law enforcement or discrimination at school (see Colen et al., 2019). Prolonged exposure to these stressors can change mental health and health behaviors such as smoking (Evenson & Simon 2005; Mezuk et al., 2017).
Both parenting practices and health-related responses to stress are strongly gendered. We draw on the stress process theory to emphasize that indicators of stress can be both internalized, such as global mental health outcomes, and externalized through health behaviors (Pearlin, 1989; Nomaguchi & Milkie, 2020). This body of work shows that these responses to stress are strongly gendered, at least in the cisgender population. Prior work has shown that when faced with stress, (presumably cisgender) women are more likely to report more internalized problems such as less mental well-being whereas (presumably cisgender) men tend to regulate emotional distress through externalized behaviors such as increased smoking (Mezuk et al., 2017; Rosenfield et al., 2005). Therefore, the present study focuses on two health outcomes that are responsive to stress—a global indicator of mental well-being and the health behavior of smoking.
Past research has focused on gender differences in a binary way between men and women. But recent scholarship has showed that gender is much more complicated in at least two ways. First, how men and women experience stress and parenthood differs by their sexual identity such that gay men and lesbian women may have unique experiences of stress and parenthood and thus different health outcomes in stressful parenting situations. Second, whether one identifies as transgender or cisgender shapes the experiences of both stress and of parenthood. However, past research has only begun to examine how variation across gay and lesbian cis and trans parenthood matters for mental and physical well-being. Additionally, most research, especially the quantitative work has used samples that are predominantly white (see Reczek, 2020), missing key aspects of both the sexual minority and transgender parenthood experience that may be unique to people of color. We explore these possibilities in turn below.
Minority Stress Theory, Parenthood and Health: How Sexual Identity Matters
According to recent population-based surveys, about 4% of U.S. adults identify as lesbian, gay, bisexual, or transgender (Gates, 2014). Additionally, an estimated 37% of gay, lesbian, and bisexual adults report having a child in their lives, and 19% of same-sex couples were raising a child under age 18 in 2011 (Gates, 2013). A wealth of scholarship suggests that children raised by gay and lesbian adults, often characterized as same-sex parent households, do not have different education and health outcomes from children raised by different-sex parents once sociodemographic characteristics are considered (Manning et al., 2014; Reczek et al., 2016). Given that recent cohorts of Americans are more likely to identify as gay and lesbian and more gay and lesbian adults are having children than ever before (Gates, 2014), it is imperative that we understand the relationship between gay and lesbian parenthood and health. The existing research that addresses this question uses designated sex of adults and their co-residing partners to identify same-sex couples; much of this research also uses minor children in the household to capture parenthood status without direct inquiry on parent-child relationship (e.g., Bos et al., 2018; Denney et al., 2013). Moreover, these studies do not have large enough samples of racial-ethnic minority groups to make strong claims regarding the experiences of Black, Latinx, and other people of color. These practices result in analyses of only cohabiting adults, neglecting sexual identity among both single and partnered parents as well as the experiences of people of color.
According to a minority stress framework, gay and lesbian people are exposed to unique stressors including discrimination and stigma at the individual, interpersonal, and institutional levels (Meyer, 2003). In U.S. society, parenthood is still considered a heteronormative institution based on the union between a cisgender man and a cisgender woman (Biblarz & Savci, 2010). Challenging traditional assumptions of heteronormative parenthood, gay and lesbian parents experience substantial stress as they confront social scrutiny and tackle internal stigma (Carroll, 2018; Tornello et al., 2011). A recent study found that parenting stress and minority stress were associated with health behaviors and mental health among gay and lesbian parents (Goldberg et al., 2019). However, much remains unknown in terms of whether and how gay and lesbian parents and non-parents have different health behaviors and mental health outcomes. Additionally, little is known about the differences in mental well-being and smoking status among gay and lesbian adults with different gender identities, especially in relation to parenthood status; nor is much known about parents of color who are also gender and sexual minorities (see Moore & Stambolis-Ruhstorfer, 2013).
Recent work suggests that white gay fathers encounter significant discrimination as their identity challenges the heteronormative notion of parenthood in which mothers are the most important caretakers for children (Stacey, 2011). Gay fathers who are presumably cisgender experience elevated stress due to additional scrutiny and even legal restrictions when transitioning to parenthood via adoption and/or surrogacy (Goldberg et al., 2014). While caring for their children, white gay fathers are under constant and substantial social suspicion about their childrearing capacity from friends, family, and strangers (Carroll, 2018). Other work shows that fathers in same-sex partnerships feel less competent as parents and experience greater losses in self-care time than fathers in different-sex households (Augustine et al., 2017; Bos et al., 2018). Notably, virtually none of these works explore these questions with a sample of predominantly racial minority fathers, but research suggests that Black gay fathers experience even greater scrutiny, causing additional stress (Randles, 2020). Overall, parenting as a gay father appears to introduce substantial stress. Thus, we hypothesize (H1) that cisgender gay fathers may experience worse mental well-being and higher odds of smoking than childless cisgender gay men.
Similar to gay fathers, cisgender lesbian mothers experience discrimination and stress as sexual minorities (Reczek, 2020). Yet, compared to gay fathers, lesbian mothers encounter fewer institutional barriers to parenthood through non-heterosexual reproduction, due to the availability of various types of donor insemination for women (Biblarz & Savci, 2010). Scholarship on heterosexual parent families shows that women’s primary responsibility of housework and childcare as well as the inequality in labor division take a toll on women’s well-being (Goldberg & Perry-Jenkins, 2004; Umberson et al., 2010). Lesbian couples have a more egalitarian division of housework and child care than heterosexual couples (Goldberg, 2013). Additionally, some lesbian mothers continued to receive social support from family and friends who recognized their identity as mothers (Glass & Few-Demo, 2013). This support may relieve some parenting stress for these lesbian mothers. Most existing work on lesbian mothers uses predominantly white samples. Among the few exceptions, Moore (2011) found that Black lesbian parent families’ ideologies on family work originated more from Black culture; these Black lesbian mothers paid more attention to the gendered dynamics of family work and constantly redefined housework in a same-sex relationship (Moore, 2011). We thus alternatively hypothesize (H2) that compared to childless cisgender lesbian women, lesbian mothers may have similar or better mental well-being and similar or lower odds of smoking.
Intersectional Minority Stress Theory
Exploring Gender Variation by Comparing Cisgender Men and Women
Family scholars are increasingly utilizing an intersectional framework to examine the health effects of parenthood, and alongside race/ethnicity, gender is often a central variable in this research (Few-Demo & Allen, 2020; Thomeer et al., 2018). An intersectional approach posits that multiple social positions (e.g., gender, sexuality, race) represent a unique combination of structural advantage and oppression, which results in varying health outcomes for individuals with intersectional identities (Bowleg, 2012). The varying combinations of structural advantages and disadvantages associated with parenthood status and sexual minority status are linked with potentially distinct health profiles. An intersectional approach also suggests that cisgender gay men and cisgender lesbian women likely experience different types of parenting stress and have varying health outcomes (Few-Demo & Allen, 2020). In fact, parenthood appears to have different associations with health for men and women in same-sex relationships (Augustine et al., 2017; Denney et al., 2013). Goldberg et al. (2019) found that (presumably) cisgender gay fathers not only had greater odds of depression than (presumably) cisgender lesbian mothers, the former group might also react to high parenting stress with worse health behaviors such as reduced regular exercise than the latter.
Taken together, prior work suggests that the relationship between parenthood and health may differ for cisgender gay men and cisgender lesbian women. (Of note is that most studies of gay men and lesbian women do not specify the gender identity of their participants, thus we do not refer to these gay and lesbian adults as cisgender unless the authors specify their gender identity.) On average, gay men report more discriminatory treatment than lesbian women (Herek, 2009; Institute of Medicine, 2011). Further, a Dutch study suggested that fathers in same-sex relationships might have more worries about childrearing than same-sex mothers (Bos et al., 2018). The gender disparity in same-sex parents’ childrearing worries may further translate into gender differences in mental health—for example, Goldberg et al. (2019) used a majority white sample and found that gay fathers had higher odds of depression than lesbian mothers. Parenting stress may further alter individual health behaviors, but little research has directly compared the health behaviors of gay and lesbian parents (see Pollitt et al., 2020). One study suggests that men in same-sex households with children might spend less time on self-care than same-sex women living with children (Augustine et al., 2017). The lack of self-care may reflect parenting strain and also generate more parenting stress, which can ultimately damage well-being and increase unhealthy behaviors. Again, most existing work uses majority white samples. Yet, the limited works that examine Black gay fathers and Black lesbian mothers separately seem to suggest that the former group experience more parenting stress whereas the latter receive more support from both their partners and the community (Moore, 2011; Randles, 2020). Thus, we hypothesize (H3) that parenthood may be associated with worse mental health and more smoking among cisgender gay men than cisgender lesbian women.
Exploring Gender Variation by Cisgender and Transgender Identity
While past work has made important advances on how gender and sexuality intersect to differentially shape the relationship between parenthood and health in cisgender men and women, very few studies have examined the effect of parenthood on health by transgender and cisgender status—especially among a sample composed predominantly of people of color. Current work on sexual minority parenthood tends to ignore gender variation across cis and trans populations—leaving the intersections of these gender and sexual identities largely unexamined (Reczek, 2020). In this study, we seek to further contribute to this scholarship by focusing on gay and lesbian adults with varying gender identities and parenthood statuses. Due to an increased number of individuals identifying as transgender in recent cohorts (Meerwijk & Sevelius, 2017) and given the varying contexts that cisgender and transgender people experience in the social world (Reisner et al., 2016), it is likely that the relationship between parenthood and health differs not only by men and women, but also by cis or transgender status. Notably, little research has been conducted on transgender parent families across racial-ethnic groups in North America (Pfeffer & Jones, 2020). Therefore, we use extra caution in theorizing the association between parenthood, gender identity, and well-being for a sexual minority sample that consists mostly of racial minorities.
According to an intersectional minority stress approach, within the gay and lesbian sexual identity categories, gender matters not only by identities of man or woman as discussed above but also by cis or transgender status. While research focuses on presumably cisgender gay men and cisgender lesbian women, there is a non-trivial number of transgender gay/lesbian adults (Galupo et al., 2016). Due to the complex ways in which privilege and marginalization may vary within communities of sexual and gender minorities (SGM), current research suggests a number of competing possibilities regarding the relationship between parenthood, health, and gender identity among gay and lesbian adults. For example, recent work suggests that transgender adults report worse health than cisgender adults (Reisner et al., 2016), making them among the most health disadvantaged groups in our population. Transgender parents face unique challenges, including family rejection and transphobia as they navigate gender transitions and reconfigure their roles as parents (Pfeffer & Jones, 2020; Pyne et al., 2015). Transgender parents also report more institutional barriers in public settings such as health services and school systems (Chapman et al., 2012; Haines et al., 2014). The effects of minority stress may be especially felt among transgender parents of color due to the interlocking systems of oppression of racism and of cisgenderism. Therefore, we hypothesize that transgender parents with an additional minority status of being gay or lesbian may experience even more stress (H4A): Transgender gay/lesbian parents may have worse mental well-being and higher odds of smoking than childless cisgender gay/lesbian adults. Yet, research on trans parents, while limited, suggests alternate relationship between parenthood and well-being among transgender adults. For instance, Pyne et al. (2015) found that white Canadian transgender parents and non-parents reported similar levels of stress. Dierckx et al. (2017) used a Belgian sample and found that transgender parents and their children were generally able to cope with the stress related to parents’ gender transition. As such, we hypothesize (H4B) that compared to childless transgender gay/lesbian adults, transgender parents may have similar or better mental well-being and similar or lower odds of smoking.
Little scholarship has examined parenthood’s association with well-being between transgender gay/lesbian adults and cisgender gay/lesbian adults. One study found that transgender parents and their families often felt unwelcomed and were sometimes denied access to parenting resources in sexual minority communities (Ryan, 2009). Transgender gay/lesbian parents may thus experience even more stress due to their multiple intersecting minority identities than cisgender gay and lesbian parents. As such, we hypothesize (H5A) that compared to cisgender gay men and cisgender lesbian women, parenthood may be associated with worse mental health and more smoking among transgender gay/lesbian adults. Conversely, transgender gay/lesbian parent families are likely the least institutionalized (e.g., fewer social norms to follow, less rigid social roles for the family members) among the three groups examined in the study. Researchers have noticed the resilience of transgender-parent families, the members of which manage to embrace more fluid gender norms and offer each other more support (Pfeffer & Jones, 2020; Pyne et al., 2015). Thus, transgender parents may be better positioned to counteract stress through strong connections with their children than their childless peers and cisgender gay and lesbian parents. Thus, we alternatively hypothesize (H5B) that compared to cisgender gay men and cisgender lesbian women, parenthood may be associated with similar or better mental health and similar or less smoking among transgender gay/lesbian adults.
Data and Methods
Data
We use data from the Social Justice and Sexuality Project (SJSP) to examine how parenthood intersects with gender identity in predicting cisgender and transgender gay and lesbian adults’ mental health and smoking status. Collected in 2010, SJSP is one of the largest national surveys of sexual and gender minorities residing in all 50 U.S. states as well as Washington D.C. and Puerto Rico. The sample consists of 4,953 individuals, including 4,358 sexual minorities, 450 gender minorities, and 3,679 racial minorities. This diversity of respondents was recruited via sampling at LGBT events, snowball sampling, the internet, and other respondent-driven sampling strategies. Even though our analyses do not necessarily align with SJSP goals of celebrating SGM people of color and analyzing how race and ethnicity matters in SGM lives (Battle et al., 2010) – SJSP is an important dataset for family scholars to examine how family ties and other social connections relate to health and well-being for SGM adults.
We aim to extend beyond the cisgender heterosexual context by examining the association between parenthood and health among a group of sexual minority adults, with additional consideration of transgender and cisgender identity. For our analytical sample, we focused on gay and lesbian adults (n =3,206), which made up 65% of the original SJSP sample. We then restricted the analysis to 2,999 gay and lesbian adults with no missing information on gender identity and parenthood status. Lastly, we limited the sample to those aged 18 and above and with valid dependent measures. This results in a final sample size of n=2,803 for analyses of mental well-being and n=2,842 for analyses of smoking. Regrettably, samples of other sexual minorities groups were too small for an intersectional analysis that simultaneously considers gender identity and parenthood status. We discuss our sampling strategy and its implications further in the discussion section.
Outcome measures
Mental health.
The measure of mental well-being derives from four questions: “Over the past week, how often have your felt: (1) That you were just as good as other people; (2) Hopeful about the future; (3) Happy; and (4) That you enjoyed life.” For each question, respondents chose answers from “never,” “sometimes,” “a lot of the time,” or “most of the time.” We combined answers and generated an index of mental well-being, with higher values (range: 4-16) denoting better mental health (Cronbach’s alpha = 0.88). The distribution of the index was slightly skewed to the right so we ran separate sensitivity analyses (not shown) with a log transformed mental well-being index and a dichotomized mental health variable. The results were similar to those presented in the text.
Smoking status.
Following the question “Do you now smoke cigarettes?”, respondents can choose an answer from “Not at all”, “Some days,” and “Every day.” We collapsed answers for “Some days” and “Every day” and generated a dichotomous measure of currently smoking (=1) in comparison to not smoking (=0).
Predictor measures
Sexual identity.
Following the question: “Which one label comes closest to how you describe your sexual identity?”, respondents can choose from options including gay, lesbian, bisexual, straight/heterosexual, queer, and other options (e.g., two spirit, same gender loving). Considering that people of color tend to use other terms to describe their monosexual identity for loving people of their same gender (e.g., Moore, 2011), the analytical sample included those who identity as gay, lesbian, “same gender loving,” and “in the life.” In the original SJSP sample, gay and lesbian adults were the dominant sexual identity group (65%), followed by bisexual (11%) and queer people (6%). Samples of bisexual and queer adults were too small for separate analyses that simultaneously considers gender identity and parenthood status.
Gender identity.
Following prior research, we determined gender identity using a two-step process with two questions (Conron et al., 2014). The first question is: “What is your current gender identity?”, the answers to which include “male, female, transgender (male to female), transgender (female to male), and other.” The second question is: “What was the sex on your original birth certificate?”, the answers to which include “male, female, and I don’t know.” Respondents who had different answers to these two questions (gender identity and sex at birth) were categorized as multigender transgender adults (hereafter referred to as “transgender” adults). Although we did not have a large enough sample (111 transgender adults for the analysis of mental well-being, and 114 transgender adults for the analysis of smoking status) to further stratify our sample into male-to-female transgender adults and female-to-male transgender people, we included a control variable for this in all models for transgender adults. Taken together, the constructed gender identity variable has three categories—cisgender men, cisgender women, and transgender adults.
Parenthood status.
This measure was based on the question: “Which of the following describes your role as parent or guardian?” Respondents could check all of the following options that apply: (1) I have at least one biological child; (2) I have parented my partner’s child; (3) I have parented at least one child; (4) I have adopted at least one child; and (5) I have no children. (Of note is that SJSP did not differentiate biological children born through heterosexual unions and children conceived through donor insemination and surrogacy.) Respondents who said yes to any of the first four questions on parenting experience were considered parents and the others were categorized as non-parents. The most common type of parents across all gender identity groups is parents to biological children—about 51% of cisgender gay fathers, 60% of cisgender lesbian mothers, and 43% of transgender parents had at least one biological child. In sensitivity analyses (available upon request), we tested how each specific type of parenthood status (i.e., biological parent, step parent, adoptive parent) interacted with gender identity in predicting mental well-being and smoking status, but sample sizes were small and no significant relationships were found.
Control variables
Sociodemographic controls include age (in years), race/ethnicity (White, Black, Latinx, and other), relationship status (married, partnered, no partner), educational attainment (high school or less, some college, bachelor degree or more), total household income last year (below $30,000, $30,000 or more), and health insurance (1=insured, 0=not insured). We also controlled for two measures particularly relevant to sexual minority parents and their well-being—whether one had come out to all of their family members, and whether one felt completely supported by their family. In supplemental analyses (not shown), we also examined a measure of nativity (i.e., whether one was born in the U.S.); it did not explain variation in either dependent variable in relation to the independent variables and was dropped.
Analytic Strategy
We first present the descriptive statistics for the full sample that includes all gay and lesbian adults, followed by statistics stratified by gender identity. Next, we present results from OLS regressions for the analysis of mental well-being and logistic regressions for the analysis of smoking status. For both sets of the analyses, we present the results for the full sample, followed by results stratified by gender identity. To maximize available information, we used multiple imputation with chained equations to impute the missing values (Allison, 2010). Among respondents with no missing values on the main dependent and independent variables, the proportion of missingness for each control variable ranged from 0.5 to 3.1 percent. Following prior research (Von Hippel, 2007), our imputation models included those who had missing values on the dependent variables (mental well-being and smoking status), but following imputation we dropped these missing cases from the subsequent descriptive and multivariate analyses. All results were estimated using Stata 15.0.
Results
Descriptive Findings
Descriptive results for full sample and the sample stratified by gender identity are presented in Table 1. Significance tests (p < 0.05) were used to assess differences across gender identities. Cisgender gay men made up more than half of the sample (56%); 40% and 4% of the respondents identified as cisgender lesbian women and transgender gay/lesbian adults, respectively. The average score of mental well-being was 13.12. Cisgender gay men and cisgender lesbian women reported similar levels of mental health, and both were significantly higher than the mental health of transgender gay/lesbian adults. Turning to smoking status, 28% of respondents were current smokers and smoking differed significantly by gender identity. Smoking was highest among transgender gay/lesbian adults (45%), followed by 30% of cisgender lesbian women, and 26% cisgender gay men. Parenthood also varied across gender identity groups; 46% of transgender gay/lesbian adults were parents, compared to 38% of cisgender lesbian women and 14% of cisgender gay men.
Table 1.
Sample Characteristics
| Full Sample | Cisgender Gay Men | Cisgender Lesbian Women | Multigender Transgender | |
|---|---|---|---|---|
| Mean or % | Mean or % | Mean or % | Mean or % | |
| Mental Well-being (Mean) | 13.12 | 13.08 | 13.26 | 12.26 |
| Mental Well-being (SD) | 2.88 | 2.85 | 2.86 | 3.28 |
| Smoke at least some days | 28.29 | 25.54 | 30.45 | 44.74 |
| Gender Identity | ||||
| Cisgender Gay Men | 55.55 | / | / | / |
| Cisgender Lesbian Women | 40.49 | / | / | / |
| Multigender Transgender | 3.96 | / | / | / |
| Parent to a bio, adopted, or/and partner’s child(ren) | 25.12 | 14.39 | 37.80 | 45.95 |
| Age | 37.02 | 37.08 | 37.07 | 35.62 |
| Race/Ethnicity | ||||
| White (ref) | 23.03 | 22.50 | 23.98 | 20.54 |
| Black | 36.13 | 37.11 | 34.63 | 37.84 |
| Latinx | 15.12 | 15.26 | 14.77 | 16.76 |
| Other | 25.72 | 25.13 | 26.63 | 24.86 |
| Relationship status | ||||
| Legal partner (ref) | 9.67 | 5.38 | 15.15 | 13.69 |
| Partnered | 43.04 | 36.01 | 53.23 | 37.48 |
| No partner | 47.29 | 58.61 | 31.61 | 48.83 |
| Education | ||||
| High school or less (ref) | 13.64 | 12.78 | 13.25 | 29.73 |
| Some college | 37.70 | 35.90 | 40.11 | 38.20 |
| Bachelor’s degree or more | 48.66 | 51.32 | 46.64 | 32.07 |
| Household income less than $30,000 | 33.05 | 31.80 | 33.34 | 47.57 |
| Medical insurance | 78.95 | 80.06 | 78.15 | 71.53 |
| Have come out to all family | 50.80 | 46.96 | 56.11 | 50.27 |
| Have complete family support | 38.14 | 36.45 | 40.56 | 37.12 |
| Gender transition: Male-to-female | / | / | / | 25.23 |
| n | 2,803 | 1,557 | 1,135 | 111 |
Note: Bolded values represent significant (p<.05) differences from multigender transgender adults; italicized values represent cisgender women’s significant (p<.05) differences from cisgender men. Sample sizes presented are for mental well-being; the sample size for the analysis on smoking status differs slightly at n=2,842 (1,582 cisgender men, 1,146 cisgender women, and 114 multigender transgender adults).
Gay and lesbian adults also differed on other characteristics by gender identity. Cisgender gay men were much less likely to have a partner than adults in other gender identity groups. Compared to both cisgender gay men and cisgender lesbian women, transgender gay/lesbian adults reported lower levels of education and less household income. A significantly higher proportion of cisgender lesbian women reported that they were out to all the family members and reported complete family support than cisgender gay men; we found no differences for gay/lesbian transgender adults in comparison to both cisgender gay men and cisgender lesbian women on outness and family support.
Multivariate Findings
Comparing Parents to Non-parents among Cisgender Gay and Lesbian People
Results from OLS regression analyses predicting mental well-being are presented in Table 2, and results for smoking are included in Table 3. According to Model 2 of Table 2, parenthood was not associated with mental well-being among cisgender gay men, failing to support H1. However, looking at results in Model 2 of Table 3, we see that parenthood status was associated with higher odds of smoking among cisgender gay men, offering partial support to H1. On average, the odds of current smoking for cisgender gay fathers were 77% higher (b = 1.77, p < 0.001) than the odds for cisgender childless gay men. As for cisgender lesbian women, Model 3s of Table 2 and Table 3 show that parenthood did not predict variations in their mental health or smoking status. Cisgender lesbian mothers and childless women had similar health profiles in our analysis, which provides evidence for H2.
Table 2.
Results from OLS Regression Models Predicting Mental Well-Being
| Full Sample | Cisgender Gay Men | Cisgender Lesbian Women | Multigender Transgender | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| b. | s.e. | b. | s.e. | b. | s.e. | b. | s.e. | |
| Gender Identity (ref: Cisgender gay men) | ||||||||
| Cisgender lesbian women | 0.02 | 0.13 | / | / | / | |||
| Multigender transgender | −1.30*** | 0.37 | / | / | / | |||
| Parent to a bio, adopted, or partner’s child | −0.14 | 0.20 | −0.12 | 0.21 | −0.03 | 0.19 | 1.76** | 0.59 |
| Gender Identity*parenthood | ||||||||
| Cisgender lesbian women*parent | 0.15 | 0.26 | / | / | / | |||
| Multigender transgender*parent | 1.51** | 0.56 | / | / | / | |||
| Age | 0.01+ | 0.01 | 0.01 | 0.01 | 0.01 | 0.01 | 0.03 | 0.03 |
| Race/Ethnicity (ref: White) | ||||||||
| Black | 0.48*** | 0.14 | 0.45* | 0.19 | 0.55* | 0.22 | −0.28 | 0.76 |
| Latinx | 0.72*** | 0.18 | 0.81*** | 0.24 | 0.71* | 0.28 | −0.09 | 0.94 |
| Other | 0.16 | 0.15 | 0.23 | 0.21 | 0.09 | 0.24 | −0.54 | 0.80 |
| Relationship status (ref: Legal partner) | ||||||||
| Partnered | −0.13 | 0.20 | −0.58+ | 0.34 | 0.10 | 0.26 | 0.51 | 0.90 |
| No partner | −0.54** | 0.21 | −0.98** | 0.33 | −0.31 | 0.28 | −0.18 | 0.89 |
| Education (ref: High school or less) | ||||||||
| Some college | 0.56** | 0.17 | 0.46* | 0.23 | 0.50+ | 0.28 | 1.00 | 0.70 |
| Bachelor’s degree or more | 0.83*** | 0.17 | 0.86*** | 0.23 | 0.58* | 0.28 | 2.46** | 0.82 |
| Household income less than $30,000 | −0.50*** | 0.12 | −0.32+ | 0.17 | −0.70*** | 0.19 | −0.50 | 0.64 |
| Medical insurance | 0.13 | 0.13 | 0.24 | 0.18 | 0.04 | 0.21 | −0.44 | 0.63 |
| Have come out to all family | 0.05 | 0.12 | 0.21 | 0.15 | −0.10 | 0.18 | −1.32* | 0.59 |
| Have complete family support | 1.04*** | 0.12 | 0.98*** | 0.16 | 1.01*** | 0.18 | 2.13*** | 0.62 |
| Gender transition: Male-to-female | / | / | / | −2.04** | 0.65 | |||
| Intercept | 11.83*** | 0.34 | 12.17*** | 0.49’ | 11.94*** | 0.49 | 10.41*** | 1.51 |
| n | 2,803 | 1,557 | 1,135 | 111 | ||||
p<.10
p<.05
p<.01
p<.001.
Table 3.
Odds Ratios from Logistic Regression Models Predicting Smoke Status
| Full Sample | Cisgender Gay Men | Cisgender Lesbian Women | Multigender Transgender | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| b. | s.e. | b. | s.e. | b. | s.e. | b. | s.e. | |
| Gender Identity (ref: Cisgender gay men) | ||||||||
| Cisgender lesbian women | 1.34** | 0.15 | / | / | / | |||
| Multigender transgender | 2.48*** | 0.67 | / | / | / | |||
| Parent to a bio, adopted, or partner’s child | 1.77*** | 0.29 | 1.77*** | 0.30 | 1.11 | 0.17 | 0.89 | 0.41 |
| Gender Identity*parenthood | ||||||||
| Cisgender lesbian women*parent | 0.62* | 0.13 | / | / | / | |||
| Multigender transgender*parent | 0.47+ | 0.20 | / | / | / | |||
| Age | 0.98*** | 0.004 | 0.98*** | 0.01 | 0.99+ | 0.01 | 0.98 | 0.02 |
| Race/Ethnicity (ref: White) | ||||||||
| Black | 0.73** | 0.09 | 0.65* | 0.11 | 0.76 | 0.14 | 1.70 | 1.08 |
| Latinx | 1.34* | 0.19 | 1.36 | 0.26 | 1.23 | 0.27 | 3.04 | 2.28 |
| Other | 1.22 | 0.15 | 1.20 | 0.21 | 1.16 | 0.22 | 3.10+ | 2.07 |
| Relationship status (ref: Legal Partner) | ||||||||
| Partnered | 1.05 | 0.17 | 0.56* | 0.15 | 1.41 | 0.30 | 0.83 | 0.61 |
| No partner | 1.18 | 0.20 | 0.73 | 0.19 | 1.44 | 0.34 | 0.63 | 0.46 |
| Education (ref: High school or less) | ||||||||
| Some college | 0.58*** | 0.07 | 0.55*** | 0.10 | 0.56** | 0.11 | 0.61 | 0.34 |
| Bachelor’s degree or more | 0.35*** | 0.05 | 0.32*** | 0.06 | 0.36*** | 0.07 | 0.32+ | 0.21 |
| Household income $30,000 + | 0.90 | 0.09 | 0.74* | 0.11 | 1.11 | 0.17 | 1.29 | 0.66 |
| Medical insurance | 0.84 | 0.09 | 0.93 | 0.14 | 0.70* | 0.11 | 1.80 | 0.98 |
| Have come out to all family | 1.34** | 0.13 | 1.42** | 0.19 | 1.23 | 0.18 | 1.26 | 0.61 |
| Have complete family support | 1.00 | 0.10 | 1.13 | 0.15 | 0.79 | 0.12 | 1.74 | 0.85 |
| Gender transition: Male-to-female | / | / | / | 0.38+ | 0.21 | |||
| n | 2,842 | 1,582 | 1,146 | 114 | ||||
p<.10
p<.05
p<.01
p<.001
Results from Model 1 of Table 2 suggests that parenthood status intersected with gender identity in predicting the mental well-being among gay and lesbian adults. For ease of interpretation, predicted values from Model 1 were generated and plotted in Figure 1. The coefficient of cisgender lesbian women*parent (b = 0.15, p > 0.05) suggests that parenthood’s association with mental health was not different for cisgender gay men and cisgender lesbian women, failing to support H3. Next, we turn to the results on smoking status, reflected in Model 1 of Table 3 and Figure 2. The coefficient of cisgender lesbian women*parent (b = 0.62, p < 0.05) indicates that parenthood was associated with higher odds of smoking among cisgender gay men than cisgender lesbian women, which provides evidence for H3.
Figure 1.
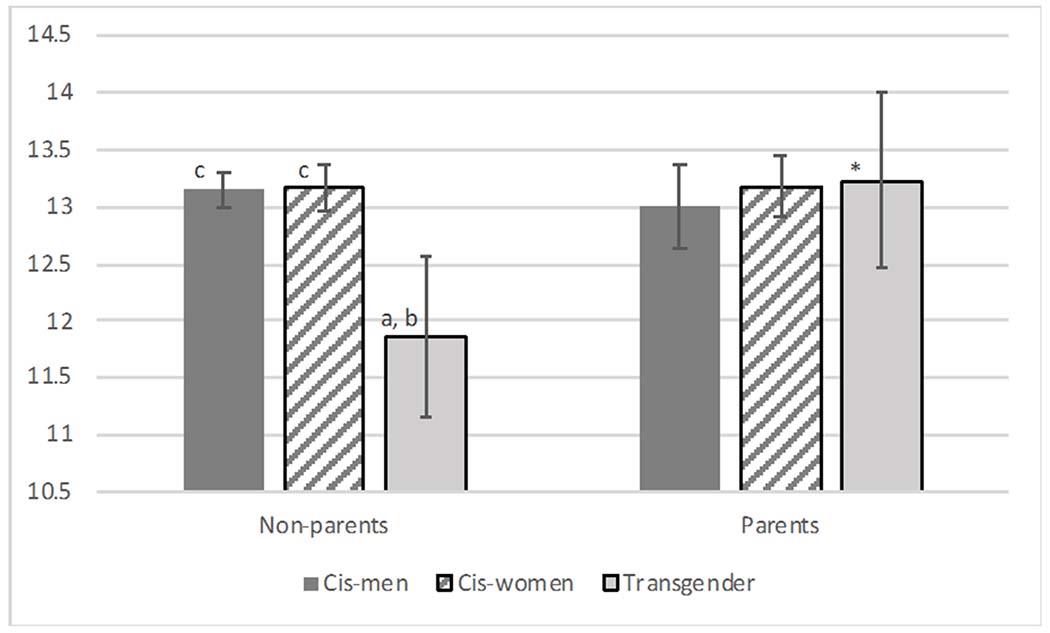
Adjusted Predictions of Mental Well-Being by Parenthood Status and Gender Identity (Values predicted from Model 1, Table 2).
Note. Letters indicate significant pairwise comparison (all at p < .10) across gender groups among non-parents and parents, respectively; a = cisgender men, b = cisgender women, c = transgender adults. * indicates significant pairwise comparison (all at p < .10) between parents and non-parents within each gender identity group.
Figure 2.
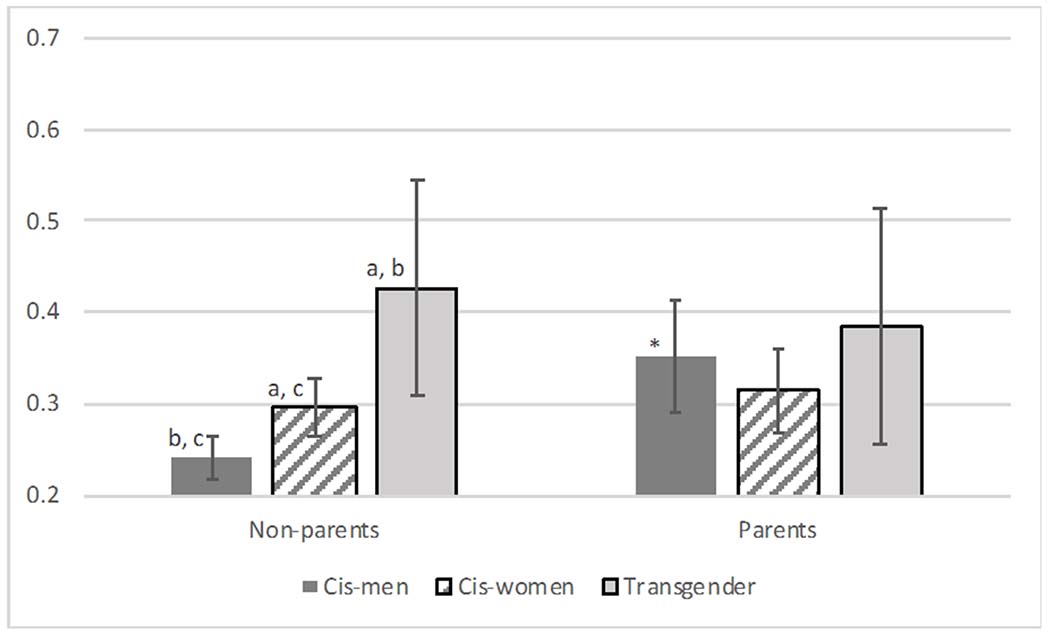
Adjusted Predictive Probability of Smoking by Parenthood Status and Gender Identity (Values predicted from Model 1, Table 3).
Note. Letters indicate significant pairwise comparison (all at p < .10) across gender groups among non-parents and parents, respectively; a = cisgender men, b = cisgender women, c = transgender adults. * indicates significant pairwise comparison (all at p < .10) between parents and non-parents within each gender identity group.
Transgender Gay and Lesbian Parents and Non-parents
Next, we turn to the results for transgender gay/lesbian adults. According to Model 4 of Table 2, being a parent was associated with mental well-being among transgender gay/lesbian adults. Results from Model 4 of Table 3 show that transgender gay/lesbian parents and non-parents had similar odds of smoking, offering support to H4B. According to Model 1 of Table 2, the coefficient of transgender*parent (b = 1.51, p < 0.01) suggests that being a parent was associated with better mental health for transgender gay/lesbian adults than cisgender gay men. Additional results (not shown) indicate that cisgender lesbian women appeared to have a less positive association of parenthood with mental health than transgender adults (b = −1.37, p < 0.05). These results provide evidence for H5B. As for the results on smoke status, the coefficient of transgender*parent (b = 0.47, p < 0.10), included in Model 1 of Table 3, suggests that transgender parenthood might be connected with reduced smoking when compared with cisgender gay fatherhood. Additional analyses (not shown) find that cisgender lesbian women and transgender adults had similar associations between parenthood and smoking, providing support for H5B.
Lastly, we conducted additional analyses combining all the sexual minority (SM) adults together (n=3,798) and tested the association between parenthood and health and how gender identity modified these associations (available upon request). We found that parenthood was not associated with mental well-being. Parenthood was associated with increased odds of smoking among SM cisgender men but not among SM cisgender women or SM transgender adults. Supplemental analyses also show that parenthood had no association with mental well-being or smoking among cisgender bisexual men and women; we were not able to include transgender bisexual adults in this analysis due to small sample sizes. We decided against combining bisexual adults together with those who identified their sexual minority status in other ways since a growing number of studies show that bisexual adults face profound health disadvantages compared to gay, lesbian, and heterosexual adults (Gorman et al., 2015; IOM, 2011).
Discussion
Parents, especially cisgender mothers, tend to have poorer health and well-being than non-parents in part due to childrearing stress (Umberson et al., 2010). One limitation of existing research is that most work focuses on cisgender heterosexual adults with little scholarship studying the heterogeneous effects of parenthood in sexual minorities with varying gender identities (Thomeer et al., 2018). Additionally, even among scholarship that includes gay and lesbian or transgender adults, much work uses majority white data that are not able to identify parental status, adults’ sexual identities, or inclusive gender identities, preventing a clear understanding of the unique challenges facing lesbian, gay, and transgender parents of color and the relevant risk factors for their health. Drawing on a sample made of mostly racial-ethnic minorities from the 2010 SJSP and guided by an integrated perspective of minority stress and intersectionality, we show that cisgender gay fathers may experience elevated stress and have worse health compared to other gender identity groups, whereas transgender gay/lesbian adults may enjoy some health benefits from parenting. In stark contrast to the literature on cisgender heterosexual parent families, we find evidence that motherhood may not be negatively associated with mental well-being and health behaviors among cisgender lesbian women. Below, we discuss our findings and highlight our main contributions.
First, our results indicate that cisgender lesbian parents and lesbian childless women had similar mental well-being and odds of smoking (supporting H2). Prior research has shown that the unequal division of family work in cisgender heterosexual couples, where women undertake the majority of housework and childcare is associated with worse well-being for women (Goldberg & Perry-Jenkins, 2004; Umberson et al., 2010). Compared to heterosexual parents, lesbian couples with children tend to divide family work more equally (Goldberg, 2013). Black lesbian parents paid more attention to gender dynamics and attributed more relationship power to those in charge of household labor (Moore, 2011). The more balanced relationship of lesbian couples may serve to relieve some parenting stress and diminish or even obliterate the well-being differences between childfree cisgender lesbian women and lesbian parents. Furthermore, cisgender gay fathers reported higher odds of smoking than childless cisgender gay men (supporting H1) but cisgender gay fathers and their childless peers had similar mental well-being. We also found that parenthood was associated with higher odds of smoking among cisgender gay men when compared to cisgender lesbian women (supporting H3) but that parenthood had no association with mental health for both cisgender gay men and cisgender lesbian women.
Previous work has shown that men are more likely to self-regulate emotional distress through externalized behaviors such as cigarette smoking than women (Mezuk et al., 2017; Rosenfield et al., 2005), and that fathers in same-sex relationships report less parenting competency and thus likely experience more stress than mothers in same-sex relationships (Bos et al., 2018). Cisgender women’s higher levels of parenting competency may translate into less parenting stress and a reduced tendency to smoke (e.g., as a means of coping with stress) compared to those without children relative to cisgender gay fathers. Moreover, cisgender lesbian women appear more likely to receive social support from individuals and institutions to help with childrearing despite the limited recognition for their sexual minority identity in ways not found for cisgender gay fathers (Glass & Few-Demo, 2013). These findings together also echo prior work showing that gay fathers experience substantial minority stress and parenting stress as their parenthood status challenges conventional definitions of masculinity and the institution of heteronormative family (Carroll, 2018; Goldberg et al., 2014; Tornello et al., 2011). Cisgender gay fathers may be more visibly out than cisgender gay non-fathers, and thus experience more interactions in these domains. Some cisgender gay fathers may also experience more stress due to the limited legal protections that allow them to negotiate non-residential co-parental arrangements and interact with their children (see Nomaguchi & Milkie, 2020). Because our sample consists mostly of racial-ethnic minorities, these results may also reflect the extra stress that cisgender gay fathers of color encounter as a result of their multiple marginalized identities (Randles, 2020). Additionally, even though parents smoke less than non-parents in the general population, parenthood can be associated with increased smoking for single people (Jun & Acevedo-Garcia, 2007). SJSP allows us to include both partnered and single parents from the sexual minority communities. In our sample, cisgender gay men and cisgender gay fathers in particular were more likely to be single than other gay and lesbian adults. Among the cisgender gay men, the unpartnered also reported less mental well-being than those with a legal partner. It is thus likely that some unobserved stressors associated with the combined status of single cisgender gay fatherhood contributed to the elevated risk of smoking among cisgender gay men.
Second, we examine how transgender status modifies the relationship between parenthood and health in gay and lesbian adults. We find that among multigendered transgender gay/lesbian adults, parents had better mental well-being than the childless, offering support to H4B. Additional analysis including all the transgender adults of all sexual identities in SJSP (not shown) finds that parenthood had no association with mental well-being. These results suggest that gay/lesbian transgender parenthood, rather than any type of transgender parenthood, is associated with better mental health. Further, additional analyses (not shown) indicates that 40% of the 50 transgender parents smoked whereas 48% of the 64 childless transgender adults smoked. This data suggests that transgender gay/lesbian parenthood may be linked with reduced smoking, although the significance of this association is constrained by small sample sizes.
Our results further show that the positive association of parenthood with mental health was more prominent among transgender gay/lesbian adults than among cisgender gay men and lesbian women and that the association between parenthood and smoking was stronger among cisgender gay men than among transgender gay/lesbian adults (supporting H5B). Taken together, these results echo recent scholarship on transgender adults’ resilience that transgender parents are able to adopt more fluid gender norms and facilitate support and care for family members (Dierckx et al., 2017; Pfeffer & Jones, 2020). Thus, transgender gay/lesbian parents, especially those of racial-ethnic minorities (considering that our sample contains mostly people of color) may be better able to buffer additional stress and achieve some resilience, as reflected in their higher levels of mental well-being than their childless peers. Furthermore, these findings support an intersectional perspective that the relationship between parenthood and health is shaped by the unique intersections of social positions (Bowleg, 2012; Thomeer et al., 2018). Specifically, the combination of multiple marginalized and stressful positions—for instance, being a transgender gay/lesbian parent, is not necessarily associated with the worst health outcomes. Parenting experience may serve as an especially important bridge for transgender gay/lesbian adults to reach out for social support, reduce stress, and maintain good health.
Limitations
Limitations of this study highlight the need for further research on this topic. First, supplemental power analyses (available upon request) show that other sexuality*gender groups (e.g., cisgender bisexual men, cisgender women with other sexual identities) did not have sufficient sample sizes for an intersectional analysis with parenthood status on health in the current paper, especially the binary outcome of smoking status. Second, about 7% of adults in the SJSP sample on mental well-being identified as transgender (n=308) and we were not able to examine transgender adults with other sexual identities separately (e.g., heterosexual transgender adults) due to sample size constraints. This is unfortunate since scholarship has shown that transgender adults tend to have more diverse and fluid sexual orientations (e.g., Galupo et al., 2016), and our supplemental analysis suggests that parenthood’s relationship with mental health and smoking varied by transgender adults’ sexuality. For reasons discussed above, we limited our sample to gay and lesbian adults. In models restricted to transgender adults, we added a control variable of gender transition (1=male-to-female, 0=other). We found that male-to-female transgender adults had worse mental health but lower odds of smoking than other transgender adults (Model 4 in Tables 2 and 3). Future research should continue to address how gender transition affects parenting experiences and health.
Third, due to small sample sizes in SJSP, we combined all types of parenthood (e.g., biological, adopted, and step) to create one dummy variable of parenthood status, even though these parenthood contexts have varying ramifications for stress and health (Nomaguchi & Milkie, 2020). Notably, SGM adults have more diverse parenthood contexts than cisgender heterosexual adults. For instance, same-sex couples are four times more likely to adopt a child than different-sex couples (Gates, 2013). Fourth, SGM adults’ pathways to parenthood are connected with their coming-out experiences, which are also, regrettably, unavailable in SJSP. Notably, many gay, lesbian, and transgender adults encounter substantial legal obstacles in adoption and gaining child custody despite strong intentions to parent (Pfeffer & Jones, 2020; Reczek, 2020). Therefore, selection is likely at play in our results. Additionally, mothers who later became lesbians and lesbians who later became mothers approach motherhood differently and undertake different childrearing responsibilities (Moore, 2011). A cisgender lesbian mother with biological children may also couple with a cisgender lesbian woman who then becomes a social/adoptive mother to her partner’s children. To add much-needed nuance to this scholarship, we need to recognize that questions in most of the existing large-scale surveys still consider families to be a cisgender heteronormative (nuclear) institution (e.g., sex of respondent, simplified relationship status, presence of children), which makes it hard to measure the diverse family dynamics among SGM communities. Future research should broaden the conceptualization of family and parenthood (e.g., who provides regular support to whom, who is considered a dependent) and examine the stress process and implications for health.
Another notable issue in relation to parenthood status is that the proportions of parents in our sample, especially cisgender lesbian women (38%) and cisgender gay men (14%), seem to be higher than other estimates. For instance, Gates (2013) used data from the 2010 Census and found that 24% of same-sex women and 10% of same-sex men had coresidential minor children. However, this study could not determine sexual identity or account for single adults. Based on a probability sample of US adults, Assink et al (2021) also found a lower proportion of lesbian parents (24%) than our estimate, likely because SJSP is not probability-based and our sample consists of mostly racial minorities, who tend to have more children than white adults (Passel et al, 2012). We discuss other race-related issues below.
Fifth, SJSP does not have information on child(ren)’s age, parent-child coresidence, and parent-child relationship quality, which have all been shown to have important contextual effects for parent’s well-being (Umberson et al., 2010). Furthermore, gay/lesbian adults’ relationship status is controlled for in the analyses, but their partners’ relationship to respondents’ children and SGM status remain unknown. Parenthood’s association with health is shown to be largely conditioned on union status (Nomaguchi & Milkie, 2020). Additional analyses also suggest that relationship status differed by gender identity, as 55% of cisgender gay fathers, 25% of cisgender lesbian mothers, and 44% transgender parents in our sample reported no partner. However, due to cell size issues we were unable to break down the analyses we presented further.
Sixth, our analysis is constrained by the small sample sizes at the intersections of race, parenthood, and sexual and gender minority statuses. Research has shown that SGM parents are more racially diverse than cisgender heterosexual parents and childless SGM adults (Gates, 2013), yet most of the existing research on SGM primarily relies on white samples. Even though we were not able to focus on race in this study, we found evidence of health benefits for gay/lesbian transgender parenthood using a SJSP sample composed mostly of racial minorities. Additionally, our sensitivity analyses show tentative evidence that parenthood, gender identity, and race may intersect to shape gay and lesbian adults’ mental health and smoking—which remains to be addressed thoroughly by future research.
Next, despite being one of the largest national surveys of SGM adults, our data is not nationally representative and is cross-sectional. We encourage future research to examine the causal links between parenthood and health among SGM adults such as assessing how transition to parenthood (and specifying the type of parenthood) links with changes in health outcomes. Lastly, the binary outcome of smoking status is limited in capturing health response to parenting stress, especially given that most people do not start smoking after they become parents. However, Thomeer et al. (2019) found that people that quit smoking might relapse due to important and potentially stressful transitions in social connections. Future studies should use detailed measures of smoking and incorporate smoking history in this research topic.
Conclusion
Taken together, our study is among the first to examine how parenthood relates to health among gay and lesbian adults that are mostly racial-ethnic minorities across three gender identity groups including transgender adults. Our study adds nuance to the literature on family, health, gender, and sexuality, with implications for health professionals and family policies. As increasing evidence suggests that children in same-sex parent families have similar educational and health outcomes as those raised in heterosexual parent families (Manning et al., 2014; Reczek et al., 2016), policy makers need to offer more recognition and support to marginalized families such as those headed by gay and lesbian adults of various gender identities including transgender people. Such support may help reduce the odds of smoking, a health behavior linked to a wide range of respiratory symptoms and terminal diseases, and introduce other health-promoting effects.
Acknowledgement:
The authors thank Danya Lagos and the Rice Department of Sociology population health lab group for their helpful feedback on this study.
Support for this study was provided by the National Institute of Aging 1R01AG069251-01A1 (MPIs Reczek and Thomeer), and the Ohio State University Institute for Population Research through a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development of the National Institutes of Health, P2CHD058484.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributor Information
Zhe Zhang, Department of Sociology, Rice University, MS-28 Rice University, P.O. Box 1892, Houston, TX 77005
Hai-Yen Chien, Department of Sociology, Rice University, MS-28 Rice University, P.O. Box 1892, Houston, TX 77005.
Kiana Wilkins, Department of Sociology, Rice University, MS-28 Rice University, P.O. Box 1892, Houston, TX 77005.
Bridget K. Gorman, Department of Sociology, Rice University, MS-28 Rice University, P.O. Box 1892, Houston, TX 77005
Rin Reczek, Department of Sociology, The Ohio State University, 238 Townshend Hall, 1885 Neil Avenue, Columbus, OH 43210
REFERENCES
- Allison PD (2010). Missing data. Thousand Oaks, CA: Sage. [Google Scholar]
- Assink M, Rothblum ED, Wilson BD, Gartrell N, & Bos HM (2021). Mental health of lesbian, bisexual, and other-identified parents and non-parents from a population-based study. Journal of Homosexuality, 1–25. 10.1080/00918369.2021.1892401 [DOI] [PubMed] [Google Scholar]
- Augustine JM, Aveldanes JM, & Pfeffer CA (2017). Are the parents alright?: Time in self-care in same-sex and different-sex two-parent families with children. Population Review, 56(2), 49–77. 10.1353/prv.2017.0007 [DOI] [Google Scholar]
- Battle J; Pastrana AJ; Jay J; Daniels J (2010) Social Justice Sexuality Project: 2010 National Survey, Including Puerto Rico (Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2013-08-09. 10.3886/ICPSR34363.v1 [DOI] [Google Scholar]
- Biblarz TJ, & Savci E (2010). Lesbian, gay, bisexual, and transgender families. Journal of Marriage and Family, 72(3), 480–497. 10.1111/j.1741-3737.2010.00714.x [DOI] [Google Scholar]
- Bos HM, Kuyper L, & Gartrell NK (2018). A population-based comparison of female and male same-sex parent and different-sex parent households. Family Process, 57(1), 148–164. 10.1111/famp.12278 [DOI] [PubMed] [Google Scholar]
- Bowleg L (2012). The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. American Journal of Public Health, 102(7), 1267–1273. 10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll M (2018). Managing without moms: Gay fathers, incidental activism, and the politics of parental gender. Journal of Family Issues, 39(13), 3410–3435. 10.1177/0192513X18783229 [DOI] [Google Scholar]
- Chapman R, Wardrop J, Freeman P, Zappia T, Watkins R, & Shields L (2012). A descriptive study of the experiences of lesbian, gay and transgender parents accessing health services for their children. Journal of Clinical Nursing, 21(7-8), 1128–1135. 10.1111/j.1365-2702.2011.03939.x [DOI] [PubMed] [Google Scholar]
- Colen CG, Li Q, Reczek C, & Williams DR (2019). The intergenerational transmission of discrimination: children’s experiences of unfair treatment and their mothers’ health at midlife. Journal of Health and Social Behavior, 60(4), 474–492. 10.1177/0022146519887347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conron K, Lombardi E, & Reisner S (2014). Identifying transgender and other gender minority respondents on population-based surveys: Approaches. In Herman JL (Eds.), Best practices for asking questions to identify transgender and other gender minority respondents on population-based surveys (pp. 9–18). Los Angeles: The Williams Institute. [Google Scholar]
- Denney JT, Gorman BK, & Barrera CB (2013). Families, resources, and adult health: Where do sexual minorities fit?. Journal of Health and Social Behavior, 54(1), 46–63. 10.1177/0022146512469629 [DOI] [PubMed] [Google Scholar]
- Dierckx M, Mortelmans D, Motmans J, & T’Sjoen G (2017). Resilience in families in transition: What happens when a parent is transgender? Family Relations, 66, 399–411. 10.1111/fare.12282 [DOI] [Google Scholar]
- Evenson RJ, & Simon R (2005). Clarifying the relationship between parenthood and depression. Journal of Health and Social Behavior, 46, 341–358. 10.1177/002214650504600403 [DOI] [PubMed] [Google Scholar]
- Few-Demo AL, & Allen KR (2020). Gender, Feminist, and Intersectional Perspectives on Families: A Decade in Review. Journal of Marriage and Family, 82(1), 326–345. 10.1111/jomf.12638 [DOI] [Google Scholar]
- Galupo MP, Henise SB, & Mercer NL (2016). “The labels don’t work very well”: Transgender individuals’ conceptualizations of sexual orientation and sexual identity. International Journal of Transgenderism, 17(2), 93–104. 10.1080/15532739.2016.1189373 [DOI] [Google Scholar]
- Gates G (2013). LGBT parenting in the United States. Retrieved from http://williamsinstitute.law.ucla.edu/wp-content/uploads/LGBT-Parenting.pdf [Google Scholar]
- Gates G (2014). LGBT demographics: Comparisons among population-based surveys. Retrieved from http://williamsinstitute.law.ucla.edu/wp-content/uploads/lgbt-demogs-sep-2014.pdf [Google Scholar]
- Glass VQ, & Few-Demo AL (2013). Complexities of informal social support arrangements for Black lesbian couples. Family Relations, 62(5), 714–726. 10.1111/fare.12036 [DOI] [Google Scholar]
- Goldberg AE (2013). “Doing” and “undoing” gender: The meaning and division of housework in same-sex couples. Journal of Family Theory & Review, 5(2), 85–104. 10.1111/jftr.12009 [DOI] [Google Scholar]
- Goldberg AE, Gartrell NK, & Gates G (2014). Research report on LGB-parent families. Retrieved from https://williamsinstitute.law.ucla.edu/wp-content/uploads/LGB-Parent-Families-Jul-2014.pdf [DOI] [PubMed] [Google Scholar]
- Goldberg AE, & Perry-Jenkins M (2004). Division of labor and working-class women’s well-being across the transition to parenthood. Journal of Family Psychology, 18(1), 225. 10.1037/0893-3200.18.1.225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg AE, Smith JZ, McCormick NM, & Overstreet NM (2019). Health behaviors and outcomes of parents in same-sex couples: An exploratory study. Psychology of Sexual Orientation and Gender Diversity, 6(3), 318–335. 10.1037/sgd0000330 [DOI] [Google Scholar]
- Gorman BK, Denney JT, Dowdy H, & Medeiros RA (2015). A new piece of the puzzle: Sexual orientation, gender, and physical health status. Demography, 52(4), 1357–1382. 10.1007/s13524-015-0406-1 [DOI] [PubMed] [Google Scholar]
- Haines BA, Ajayi AA, & Boyd H (2014). Making trans parents visible: Intersectionality of trans and parenting identities. Feminism & Psychology, 24(2), 238–247. 10.1177/0959353514526219 [DOI] [Google Scholar]
- Herek GM (2009). Hate crimes and stigma-related experiences among sexual minority adults in the United States: Prevalence estimates from a national probability sample. Journal of Interpersonal Violence, 24(1), 54–74. 10.1177/0886260508316477 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2011). The Health of Lesbian, Gay, Bisexual and Transgender People: Building a Foundation for a Better Future. Washington, DC: The National Academic Press. [PubMed] [Google Scholar]
- Jun HJ, & Acevedo-Garcia D (2007). The effect of single motherhood on smoking by socioeconomic status and race/ethnicity. Social Science & Medicine, 65(4), 653–666. 10.1016/j.socscimed.2007.03.038 [DOI] [PubMed] [Google Scholar]
- Manley MH, & Ross LE (2020). What do we now know about bisexual parenting? A continuing call for research. In: Goldberg A & Allen K (Eds.,) LGBTQ-Parent Families. Springer, Cham: (pp. 65–83). [Google Scholar]
- Manning WD, Fettro MN, & Lamidi E (2014). Child well-being in same-sex parent families: Review of research prepared for American Sociological Association Amicus Brief. Population Research and Policy Review, 33(4), 485–502. 10.1007/s11113-014-9329-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meerwijk EL, & Sevelius JM (2017). Transgender population size in the United States: a meta-regression of population-based probability samples. American Journal of Public Health, 107(2), e1–e8. 10.2105/AJPH.2016.303578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice as stress: conceptual and measurement problems. American Journal of Public Health, 93(2), 262–65. 10.2105/AJPH.93.2.262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B, Ratliff S, Concha JB, Abdou CM, Rafferty J, Lee H, & Jackson JS (2017). Stress, self-regulation, and context: Evidence from the health and retirement survey. SSM-Population Health, 3, 455–463. 10.1016/j.ssmph.2017.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore MR (2011). Two sides of the same coin: Revising analyses of lesbian sexuality and family formation through the study of Black women. Journal of Lesbian Studies, 15(1), 58–68. 10.1080/10894160.2010.508412 [DOI] [PubMed] [Google Scholar]
- Moore MR, & Stambolis-Ruhstorfer M (2013). LGBT sexuality and families at the start of the twenty-first century. Annual Review of Sociology, 39, 491–507. 10.1146/annurev-soc-071312-145643 [DOI] [Google Scholar]
- Nomaguchi K, & Milkie MA (2020). Parenthood and well-being: A decade in review. Journal of Marriage and Family, 82(1), 198–223. 10.1111/jomf.12646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passel J, Livingston G, & Cohn D (2012). Explaining why minority births now outnumber white births. https://www.pewresearch.org/social-trends/2012/05/17/explaining-why-minority-births-now-outnumber-white-births/
- Pearlin LI (1989). The sociological study of stress. Journal of Health and Social Behavior, 30(3), 241–256. [PubMed] [Google Scholar]
- Pfeffer CA & Jones KB. (2020). Transgender-Parent Families. In: Goldberg A, Allen K (eds) LGBTQ-Parent Families. Springer, Cham: (pp. 199–214). [Google Scholar]
- Pollitt AM, Reczek C, & Umberson D (2020). LGBTQ-Parent Families and Health. In: Goldberg A &Allen K (Eds.,) LGBTQ-Parent Families. Springer, Cham: (pp. 125–140) [Google Scholar]
- Pyne J, Bauer G, & Bradley K (2015). Transphobia and other stressors impacting trans parents. Journal of GLBT Family Studies, 11(2), 107–126. 10.1080/1550428X.2014.941127 [DOI] [Google Scholar]
- Randles JM (2020). Essential Dads: The Inequalities and Politics of Fathering. University of California Press. [Google Scholar]
- Read JNG, & Gorman BK (2010). Gender and health inequality. Annual Review of Sociology, 36, 371–386. 10.1146/annurev.soc.012809.102535 [DOI] [Google Scholar]
- Reczek C, Spiker R, Liu H, & Crosnoe R (2016). Family structure and child health: Does the sex composition of parents matter?. Demography, 53(5), 1605–1630. 10.1007/s13524-016-0501-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reczek C (2020). Sexual-and gender-minority Families: A 2010 to 2020 decade in review. Journal of Marriage and Family, 82(1), 300–325. 10.1111/jomf.12607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, … & Baral SD (2016). Global health burden and needs of transgender populations: a review. The Lancet, 388, 412–436. 10.1016/S0140-6736(16)00684-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfield S, Lennon MC, & White HR (2005). The self and mental health: Self-salience and the emergence of internalizing and externalizing problems. Journal of Health and Social Behavior, 46(4), 323–340. 10.1177/002214650504600402 [DOI] [PubMed] [Google Scholar]
- Ryan M (2009). Beyond Thomas Beatie: Trans men and the new parenthood. In Epstein R (Ed.), Who’s your daddy? And Other Writing on Queer Parenting (pp. 139–150). Toronto: Sumach Press. [Google Scholar]
- Stacey J (2012). Unhitched: Love, marriage, and family values from West Hollywood to Western China. NYU Press. [Google Scholar]
- Thomeer MB, Paine EA, & Bryant C (2018). Lesbian, gay, bisexual, and transgender families and health. Sociology Compass, 12(1), e12552. 10.1111/soc4.12552 [DOI] [Google Scholar]
- Thomeer MB, Hernandez E, Umberson D, & Thomas PA (2019). Influence of social connections on smoking behavior across the life course. Advances in Life Course Research, 42. 10.1016/j.alcr.2019.100294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tornello SL, Farr RH, & Patterson CJ (2011). Predictors of parenting stress among gay adoptive fathers in the United States. Journal of Family Psychology, 25(4), 591–600. 10.1037/a0024480 [DOI] [PubMed] [Google Scholar]
- Umberson D, Pudrovska T, & Reczek C (2010). Parenthood, childlessness, and well-being: A life course perspective. Journal of Marriage and Family, 72(3), 612–629. 10.1111/j.1741-3737.2010.00721.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Hippel PT (2007). Regression with missing Ys: An improved strategy for analyzing multiply imputed data. Sociological Methodology, 37, 83–117. 10.1111/j.1467-9531.2007.00180.x [DOI] [Google Scholar]


