Abstract
Syndactyly is one of the most common congenital limb malformations, second only to polydactyly. Syndactyly is treated with surgical intervention. During separation, free skin grafting or skin flap transplantation is required to allow for adequate skin closure. We introduce a novel application method of the Pennig external fixation device for the management of pediatric syndactyly without skin grafting. The Pennig minifixator was used in syndactyly to expand the web space soft tissue in order to allow a Z-plasty to be performed in a second operation. All patients had developed sufficient skin tissue from the external fixation. No infection, cutaneous necrosis or nonunion was noted in any of the patients. All patients had a satisfactory outcome in terms of final appearance and digit function. On the basis of the principle of strain-stress, use of the Penning external minifixator allows development of sufficient tissue in the web space for a second phase of reconstruction in syndactyly. The need for skin grafting and risk of blood vessel damage were avoided in this study, and, the incidence of skin necrosis and scar formation was reduced. Both the patients’ families and our research members expressed high satisfaction with the postoperative function and appearance. Overall, application of the Pennig external fixation frame in our novel method is effective for the management of syndactyly and should be studied further.
Level of Evidence: Level IV, case series.
Key Words: child, syndactyly, pennig minifixator, surgical technique, external fixation
Syndactyly is one of the most common congenital limb malformations, second only to polydactyly, the excess number of digits.1,2 In syndactyly, adjacent digits fail to separate during limb development resulting in a webbed appearance.3 Various classification schemes have been proposed, with the most commonly used scheme based on the types of tissues and structures that fail to separate.1 Specifically, simple syndactyly, otherwise known as cutaneous syndactyly, describes the deformity when only soft tissues fail to separate. Complex syndactyly, otherwise known as osseous syndactyly, refers to connections between both the bones and the soft tissues (Figs. 1, 2).4 Syndactyly not only impacts the function of the digits, limiting physical ability, but is also esthetically displeasing which likely affects the psychology of patients.5
FIGURE 1.

Preoperative appearance of the syndactyly deformity.
FIGURE 2.

Preoperative x-ray of the syndactyly deformity.
Currently, simple syndactyly is treated with surgical intervention. During separation, free skin grafting or skin flap transplantation is required to allow for adequate skin closure.5 This procedure has been noted to result in scar flexion and contracture, which can impact postoperative appearance and function. On the basis of the Tension-Stress rule,6 researchers have been able to obtain sufficient skin by stretching the intervening web space between the syndactyly digits through internal or external fixtures, avoiding the need for skin grafting.7–9
In this study we propose a novel method of use of the Pennig external fixation frame (Fig. 3), applying it in such a way so as to minimize osteum damage while maximizing soft tissue expansion for syndactyly treatment.
FIGURE 3.
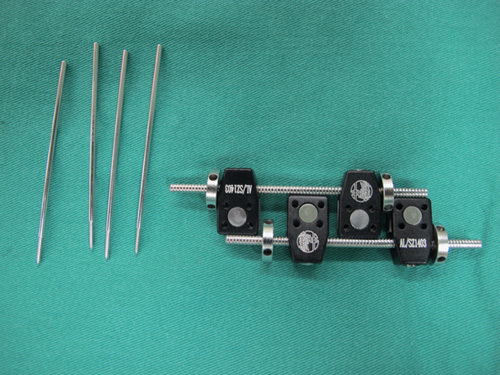
Pennig external fixation frame with its fixation pins.
ANATOMY
Syndactyly is one of the most common congenital upper limb malformations, which most often occurs in the middle and ring finger. Adjacent soft tissues with or without osseous elements fail to separate during limb development resulting in a webbed appearance (complex syndactyly or simple syndactyly).
INDICATIONS/CONTRAINDICATIONS
The indications include simple and complex syndactyly, especially complex syndactyly which connected with osseous components besides soft tissues. This syndactyly release technique is more convenient to perform without skin grafting. Contraindications for this procedure are children under 2 years old. We consider that the phalanges and soft tissue of these children are small and inconvenient for this technique. Patients with partial syndactyly also may not require this procedure.
TECHNIQUE
All surgeries are performed under general anesthesia and a pneumatic tourniquet. The entire procedure is split into 2 stages.
Stage 1: Surgery
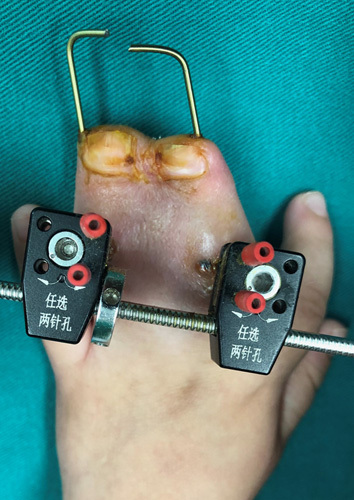
First, a 1.2 mm Kirschner wire is used to penetrate the syndactyly fingers from the fingertips to the base of the proximal phalanx. The 2 minifixators are fixated on the dorsal middle phalanx of the syndactyly fingers through 4 skeletal pins (d=1.6 mm). The minifixator is gradually extended to expand the skin and tissue. The digit tips are fixed with gypsum to prevent the exit of the Kirschner wire as well as prohibit the children form scratching (Figs. 4, 5).
FIGURE 4.

Postoperative setup of the Pennig external fixation frame.
FIGURE 5.

Kirschner wire and phalanx pins schematic diagram (red line=Kirschner wire, green point=phalanx pin).
Stage 1: Postoperative Management
Five days after surgery, stretching with the minifixator is started at a pace of 0.25 mm every 6 hours.10 The peripheral blood supply is monitored throughout the stretching period. The horizontal distance of the stretching web space is calculated using Vladimir ’s method with the formula A=πD/2 (Fig. 6), where A is the horizontal distance of the web space between the syndactyly fingers to be stretched, D is the syndactyly digits’ thickness from palmaris to dorsalis, and π is 3.14.5 Once satisfactory web space is achieved, the patient undergoes a 3-week fixing period in preparation for stage 2 of the surgery (Fig. 7).
FIGURE 6.
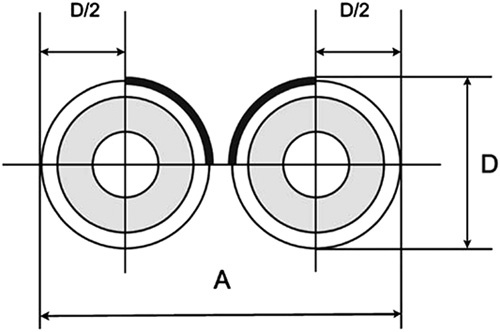
The horizontal distance of Vladimir’s method.
FIGURE 7.
Appearance before stage 2 of the surgery with the skin and subcutaneous tissues fully stretched.
Stage 2: Surgery
In the second stage the minifixator is removed, and the syndactyly digits are separated using a Z-shaped incision. A dorsal metacarpal flap is designed to reconstruct the web of the dorsum at the interphalangeal space (Figs. 8, 9). The flap is sutured with 5-0 nylon sutures, which are removed 14 days later.
FIGURE 8.
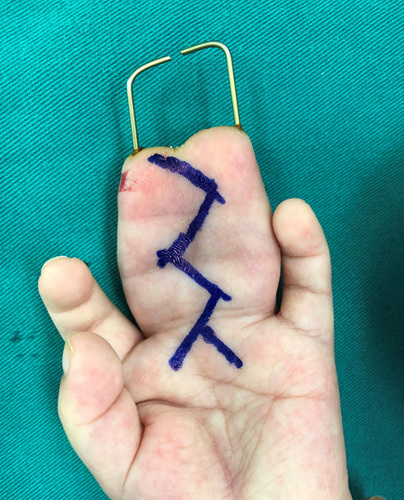
Design of the Z-plasty for stage 2 of the surgery.
FIGURE 9.

Appearance after stage 2 of the surgery.
OUTCOMES
From September 2014 to June 2016 7 cases of congenital cutaneous syndactyly (2 girls, 5 boys) were recruited. The age range was 2 to 4 years old (mean: 3.2 y). One case was a complete triple-syndactyly of the right index, middle and ring digits concomitant with a middle digit polydactyly deformity. Five cases were a middle and ring digit complete syndactyly and the final case was a right ring and little digit incomplete syndactyly concomitant with a polydactyly deformity of the little digit. Three cases had left hand involvement and 4 had right hand involvement. All cases were simple syndactylies.
Scaring was evaluated using the Vancouver scar scale11 with specific evaluation criteria detailed in Table 1.
TABLE 1.
The Vancouver Scar Scale
| Pigmentation | Erythema | Thickness | Pliability | Score |
|---|---|---|---|---|
| Normal | Normal | Flat | Normal | 0 |
| Hypopigmented | Pink | <2 mm | Supple-flexible with minimal resistance | 1 |
| Mixed | Red | 2-5 mm | Yielding-giving way to pressure | 2 |
| Hyperpigmented | Purple | >5 mm | Firm-inflexible, not easily moved, resistant to manual pressure | 3 |
| >4 mm | Banding: rope-like tissue that blanches with scar extension | 4 | ||
| Contracture: permanent shortening of scar, producing deformity or distortion | 5 |
Web creep was assessed using a 5-point scale system.12 Specifically web creep was assessed based on its extension from the palmar metacarpophalangeal (MCP) to the proximal interphalangeal (PIP) joint crease. Scores were 0 for normal web space, 1 for thickening of the web without advancement, 2 for one-third web creep of distance from the palmar MCP to the PIP joint crease, 3 for two-thirds web creep distance from the palmar MCP to the PIP joint crease, and 4 for length of web advancement to the PIP joint crease. Among these scores, level 0 to 1 indicates effective treatment, 2 to 3 indicates minor efficacy of the treatment, and 4 indicates no benefit achieved with re-operation required.
Evaluation of the digits and joints was based on the Strickland and Glogovac standards.13 Specifically, total active range of motion (ROM)=inflection degree of the proximal finger knuckle+inflective degree of the distal finger knuckle−extension degree of above 2 knuckles. Through this, 4 levels can be obtained, excellent (>150 degrees), fine (125 to 149 degrees), mean (90 to 124 degrees), and poor (<90 degrees).
Appearance and overall function were scored on a spectrum from 0 for almost normal, satisfactory appearance to 10 for completely unsatisfactory appearance. Finally, for function 0 indicates no limit to digit activity and 10 indicates seriously limited activity.
All cases were simple syndactylies that underwent homogeneous tissue expansion with the Pennig external fixation frame in stage 1 and a cutaneous intervention with Z-plasty in stage 2. All 7 cases had normal wound healing, with no noted incision infection, delayed healing or nonhealing. Entry point infection was noted in 2 cases, and the entry point completely healed after removal of the Pennig minifixator. The average follow-up time was 13.5 months (range=12 to 16 mo). Tendon function was good, and no bone or cartilage developmental disorders were observed during follow up.
On Vancouver scar scale analysis, 5 cases scored a total of 0, and 2 cases scored a total of 2 (average score 0.8). All the cases had normal web space postoperatively. The web space creep degree was 0 with effective treatment. Six cases had excellent ROM on postoperative assessment, with 1 case having fine ROM. Appearance was scored 0 for 2 cases, 2 for 2 cases, and 1 for the remaining 3 cases. Function was scored 0 for 3 cases, 1 for 1 case, and 2 for the remaining 3 cases (Table 2, Figs. 10, 11).
TABLE 2.
Postoperative Assessment of the 7 Patients
| Vancouver Scar Scale | Joint Activity (Digit) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case No. | Color | Vascular Distribution | Thickness | Softness | Total | Web Creep | Middle (Degrees) | Ring (Degrees) | Fifth (Degrees) | Physical Appearance | Function |
| 1 | 0 | 0 | 1 | 1 | 2 | 0 | 149 | 160 | 2 | 2 | |
| 2 | 0 | 0 | 0 | 0 | 0 | 0 | 165 | 158 | 0 | 0 | |
| 3 | 0 | 0 | 0 | 0 | 0 | 0 | 162 | 154 | 0 | 1 | |
| 4 | 1 | 1 | 0 | 0 | 2 | 0 | 156 | 160 | 1 | 2 | |
| 5 | 0 | 0 | 0 | 0 | 0 | 0 | 160 | 162 | 1 | 0 | |
| 6 | 1 | 0 | 1 | 0 | 2 | 0 | 150 | 152 | 2 | 2 | |
| 7 | 0 | 0 | 1 | 0 | 1 | 0 | 158 | 160 | 1 | 0 | |
| Mean | 0.28 | 0.14 | 0.43 | 0.14 | 1 | — | 156.5 | 159 | 154 | 1 | 1 |
FIGURE 10.

Postoperative appearance.
FIGURE 11.

Postoperative function.
DISSCUSSION
Syndactyly, either congenital or acquired through postburn contracture, is a common limb malformation seen in clinic that impacts both appearance and function. This deformity can also affect patients physiologically and psychologically. Surgical treatments aim to separate the syndactyly digits while achieving the best possible function and appearance outcome. Historically, skin grafts and skin flaps have been used to enable skin closure. Skin grafts are, however, limited because of the need of donor tissue as well as occurrence of scarring in the flap forming area, finger contracture deformity, web space creeping, inappropriate hair growth, and donor site morbidity.
Here we propose and investigate a novel method of applying a commonly used external fixator. The novelty of our treatment lies in the use of microexternal fixation. Previous research by Gudushiauri and Tvaliashvili,7 Shevtsov and Danilkin,8 Kamath et al,9 and Mei et al,14 introduced different external fixation mechanisms that stretch the skin and subcutaneous tissue. On the basis of the Ilizarov tension-stress rule theory,6 when tissue is exposed to sustained tension it expands through active growth and regeneration, just like bone expansion. These methods have reported favorable outcomes, and confirmed success in expanding the soft tissue. These methods have not, however, become well popularized.
In our study, a novel application of the Pennig external fixator allowed gradual application of a corrective force resulting in satisfactory treatment of the digital syndactyly. The Pennig minifixator was invented by the German orthopedic surgeon Dietmar Pennig and was originally used for the treatment of metacarpal and metatarsal fractures.15 The Pennig minifixator has numerous advantages including ease and convenience of use. In total, including its extendable arm and 2 clip locks, it weighs only 150 g. Its accompanying tools are an “L”-shaped tool and an Allen tool, which have a total volume lower than all other external fixators. Furthermore, the device is easy to handle and adjust. Fixing the Pennig device requires penetrating all phalanges with 1.0 to 1.2 mm Kirschner pins inversely from the center of the distal phalanx extremity, then fastening the external fixator at the dorsal middle phalanx of the syndactyly. Frame adjustment is convenient; the “L” wrench loosens the clamp, the Allen wrench rotates the turntable to complete the extension, and then the “L” wrench can be used to tighten the locks. Parents can easily learn and adjust the frame at home. The device also results in minimal trauma. The 1.2 mm Kirschner pins cause minimal injury to the epiphysis when penetrating the phalanges. The Alex pins of the Pennig external fixation frame have a diameter of 1.6 mm which cause minimal impact on the phalanges. The frame setup designed by Shevtsov and Danilkin8 and Mei et al14 required multiple insertion points on the syndactyly phalanges increasing the risk of negative effects on the child’s bony development. The external frame designed by Kamath connects the phalanges by Kirschner pins at the end where the extending fixtures are fastened and causes minimal trauma. This operation, however, is more complicated.
Our technique has notable advantages. Most noteworthy, skin grafting is avoided making the surgical intervention easier and avoiding any donor site complications seen with skin grafting. In addition, it comes without the risk of skin graft failure. The device is small and light, but is sufficiently rigid to allow for stable expansion. Further, previously published external fixation methods for syndactyly treatment, such as those described by Shevtsov and Danilkin8 and Mei et al,14 required multiple points of fixation on the phalanx making it more likely to affect the skeletal development of children. To minimize effects on the phalanx epiphysis we used 1.2 mm Kirschner wire and 1.6 mm fixation screws and no bone or cartilage developmental disorders were observed during follow-up. Finally, the resulting surgical scars are small and hidden in the interdigit space, while functional recovery of the operated digits was excellent.
On the basis of the tension-stress principle, fixation with external frames can stretch the skin and subcutaneous tissue sufficiently to allow for syndactyly treatment without the need of a skin graft. This can also reduce the risk of the postoperative scarring and web space creeping. Among the external fixators, the Pennig external frame appears to be most appropriate in the treatment of syndactyly, as it is light and can be easily operated. In this case series, we showed excellent esthetic and functional recovery highlighting the potential of this novel application in the treatment of syndactyly.
COMPLICATIONS
The most disadvantage of this technique is the extended treatment period and the need to undergo 2 procedures. Potential complications include pin-site infections. The risk of pin-site infections can be reduced by administering perioperative and topical antibiotics. In addition, although our setup attempts to minimize the effect on the bones, the external fixator must still be fixed to the phalanx and can have an impact on the bone, whereas traditional skin grafting has no effect bone condition. Last, children are less likely to be careful with their device and the external frame can be damaged by accident. Loosening or breaking of the device may require further surgery and, hence, a longer treatment period.
Footnotes
All patients provided signed informed consent allowing their clinical data to be used for research. Written informed consent was obtained from the parents. This retrospective study was approved by the Ethics Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology.
Conflicts of Interest and Source of Funding: The authors report no conflicts of interest and no source of funding.
Contributor Information
Jin Li, Email: lijin2003@126.com.
Qin Wang, Email: xiaogui520530@126.com.
Adriana C. Panayi, Email: apanayi@bwh.harvard.edu.
Mengfan Wu, Email: mwu27@bwh.harvard.edu.
Xin Tang, Email: 56415607@qq.com.
Pan Hong, Email: 1260762426@qq.com.
Renhao Ze, Email: z9813004@126.com.
REFERENCES
- 1.Michael A. Failure of differentiation part I: syndactyly. Hand Clin. 2009;25:171–193. [DOI] [PubMed] [Google Scholar]
- 2.Moore JL, Joseph A. Complete first ray polydactyly: a case report. J Foot Ankle Surg. 2018;57:1027–1029. [DOI] [PubMed] [Google Scholar]
- 3.Malik A. Syndactyly: phenotypes, genetics and current classification. Eur J Hum Genet. 2012;20:817–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tonkin MA, Tolerton SK, Quick TJ, et al. Classification of congenital anomalies of the hand and upper limb: development and assessment of a new system. J Hand Surg Am. 2013;38:1845–1853. [DOI] [PubMed] [Google Scholar]
- 5.Goldfarb CA, Steffen JA, Stutz CM. Complex syndactyly: aesthetic and objective outcomes. J Hand Surg Am. 2012;37:2068–2073. [DOI] [PubMed] [Google Scholar]
- 6.Ilizarov GA. Clinical application of the tension-stress effect for limblengthening. Clin Orthop Relat Res. 1990;250:8–26. [PubMed] [Google Scholar]
- 7.Gudushauri ON, Tvaliashvili LA. Distraction method of preparing for skin plasty in syndactyly. Ortop Travmatol Protez. 1983;11:25–27. [PubMed] [Google Scholar]
- 8.Shevtsov VI, Danilkin MY. Application of external fixation for management of hand syndactyly. Int Orthop. 2008;32:535–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamath JB, Vardhan H, Naik DM, et al. A novel method of using mini external fixator for maintaining web space after the release of contracture and syndactyly. Tech Hand Up Extrem Surg. 2013;17:37–40. [DOI] [PubMed] [Google Scholar]
- 10.Aronson J. Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. J Bone Joint Surg Am. 1997;79:1243–1258. [DOI] [PubMed] [Google Scholar]
- 11.Oliveira GV, Chinkes D, Mitchell C, et al. Objective assessment of burn scar vascularity, erythema, pliability, thickness, and planimetry. Dermatol Surg. 2005;31:48–58. [DOI] [PubMed] [Google Scholar]
- 12.Lumenta DB, Kitzinger HB, Beck H, et al. Long-term outcomes of web creep, scar quality, and function after simple syndactyly surgical treatment. J Hand Surg Am. 2010;35:1323–1329. [DOI] [PubMed] [Google Scholar]
- 13.Strickland JW, Glogovac SV. Digital function following flexor tendon repair in zone II: a comparison of immobilization and controlled passive motion techniques. J Hand Surg Am. 1980;5:537–543. [DOI] [PubMed] [Google Scholar]
- 14.Mei H, Zhu G, He R, et al. The preliminary outcome of syndactyly management in children with a new external separation device. J Pediatr Orthop B. 2015;24:56–62. [DOI] [PubMed] [Google Scholar]
- 15.Pennig D, Gausepohl T, Mader K, et al. The use of minimally invasive fixation in fractures of the hand—the minifixator concept. Injury. 2000;31:102–112. [DOI] [PubMed] [Google Scholar]


