Abstract
Objective:
To determine the consensus among studies that adhesive resin application improves the bond strength of orthodontic brackets and the association of methodological variables on the influence of bond strength outcome.
Materials and Methods:
In vitro studies were selected to answer whether adhesive resin application increases the immediate shear bond strength of metal orthodontic brackets bonded with a photo-cured orthodontic adhesive. Studies included were those comparing a group having adhesive resin to a group without adhesive resin with the primary outcome measurement shear bond strength in MPa. A systematic electronic search was performed in PubMed and Scopus databases.
Results:
Nine studies were included in the analysis. Based on the pooled data and due to a high heterogeneity among studies (I2 = 93.3), a meta-regression analysis was conducted. The analysis demonstrated that five experimental conditions explained 86.1% of heterogeneity and four of them had significantly affected in vitro shear bond testing. The shear bond strength of metal brackets was not significantly affected when bonded with adhesive resin, when compared to those without adhesive resin.
Conclusions:
The adhesive resin application can be set aside during metal bracket bonding to enamel regardless of the type of orthodontic adhesive used.
Keywords: Dental bonding, Orthodontic brackets, Shear strength
INTRODUCTION
The spotlight in orthodontic bonding with attainment of satisfactory strengths has focused on the decrease in clinical steps and hence, the cost of materials.1 Thus, two-step orthodontic adhesives, without prior application of adhesive resin, has appeared on the market in order to decrease the procedure time of bracket bonding.2 These composites, called flowable resins, have a smaller amount of inorganic filler and therefore have low viscosity compared with conventional resins.3 Furthermore, a previous report has shown that adhesive resins have greater cytotoxicity for gingival fibroblasts.4
Although proper bonding should decrease microleakage, little information is available relating microleakage and direct bracket bonding to enamel with orthodontic composites. Nevertheless, some authors5,6 have found no association between microleakage and shear bond strength of orthodontic brackets to enamel. Moreover, absence of prior adhesive resin may diminish enamel wetness, decreasing the amount of adhesive left on the tooth after bracket removal.3
Several studies have reported that to achieve adhesion to enamel by mechanical retention requires prior application of adhesive resin. However, recent in vitro studies have shown that orthodontic adhesives without priming reached bond strength comparable to that found with previous primer application.2,7 The consensus in the orthodontic literature2,8 about the factors that might influence bracket bond strength are the base surface area, specimen storage time, enamel conditioning procedures, type of adhesive and resin used, and bracket base design. Nevertheless, many studies did not properly report significant test conditions.9
Several studies have evinced the bond strength success of orthodontic brackets without prior application of adhesive resin, so we wish to ascertain the necessity of using adhesive resin before bracket bonding. Furthermore, understanding the factors that play a major role in the bracket/tooth interface is essential for standardizing the experimental variables. Such knowledge could improve in vitro conditions that indeed affect bond strength outcome. Therefore, the aim of this systematic review was to evaluate the association between adhesive resin and shear bond strength of orthodontic brackets to enamel and to analyze the association among other experimental variables.
MATERIALS AND METHODS
This study was reported according to the PRISMA Statement where applicable.10
In vitro studies were selected to answer whether adhesive resin application influences the immediate shear bond strength of metal orthodontic brackets bonded with a photo-cured orthodontic adhesive. Studies included were those comparing a group with adhesive resin application to a group without adhesive resin application and that the primary outcome measurement was shear bond strength in MPa. There was no language or date restriction. The search limit was publication status (only studies published in journals were considered).
A systematic electronic search was performed in PubMed and Scopus databases using the following search strategy: “(Orthodontic) OR Orthodontics) AND (primer) OR liquid resin) OR bond optimizer) OR primer based system) OR adhesion promoting agent) OR bond enhancing primer) OR intermediate bond resin) OR fluid unfilled resin) OR resin sealant) OR sealant) AND (bonding system) OR adhesive) OR resin composite) OR flowable composites) AND (bond strength).” The last search was performed in August 2014. In addition, the references of the identified articles were manually searched for other relevant studies.
Two reviewers screened independently the titles and abstracts of the retrieved citations to exclude noneligible articles. Disagreement between reviewers was resolved by consensus meetings. Full texts of eligible articles were read to determine whether they met the criteria. Articles that used thermocycling as an aging process were excluded.
For each study, data on sample size, type of teeth (human premolar, human molar, or bovine), bracket base area (mm2), bracket base design, conditioning time, photo-curing time, storage time before shear test, local force application, load type, crosshead speed of tester, bond strength (MPa) and standard deviation, year of publication, and country of included studies were obtained. Missing data were requested of corresponding authors whenever necessary.
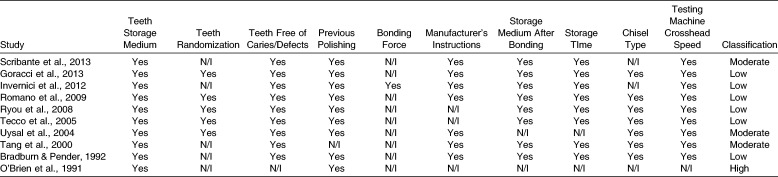
To assess individual risk of bias of each study, 10 methodological items were analyzed: (1) citation of teeth storage medium after extraction, (2) teeth randomization, (3) screening for caries and cracks on teeth, (4) previous enamel polishing, (5) standardization of force applied on bracket during bonding, (6) using materials according to manufacturer’s instructions, (7) citation of storage medium after bonding, (8) time of tooth storage before debonding, (9) citation of chisel type, and (10) crosshead speed of the testing machine. After collecting these items, we classified the studies as high, moderate, or low risk of bias. Studies that failed to report seven items or more were classified as high risk, those failing to report four to six items were classified as moderate risk, and those not reporting three items or less were classified as low risk. Studies classified as high risk of bias were excluded from the analysis.
Statistical Analysis
The pooled mean bond strength of all groups from all included studies was determined by random linear meta-analysis using the DerSimonian-Laird random-effects method. Then, because of their high heterogeneity, the data were analyzed in linear meta-regression with the restricted maximum likelihood estimator to obtain between-study variance (tau2). P values were estimated with Monte Carlo simulation (with 1000 permutations from the 31 groups included) to obtain more precise estimates. Bivariate associations were performed, and we set the P level at <.25 for the variable to enter in the multivariate analysis model and a P < .20 to remain in the final model. Diagnostic procedures were performed to check for outliers, leverage, and normality of residuals. All analyses were performed in Stata 13.1.
RESULTS
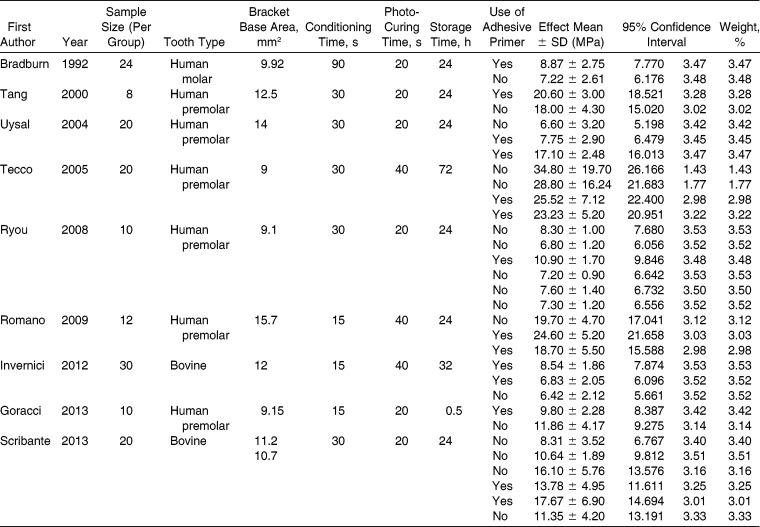
Progress through the stages of systematic review is presented in Figure 1. A total of 808 titles and abstracts were screened after removing the duplicates. After bias risk analysis (Table 1), one study11 was excluded due to its high risk of bias. Nine studies2,3,8,12–17 were included; descriptive data, random-effect means, confidence interval, and weight of each study are shown in Table 2. The lowest mean for bond strength in a group was 6.42 MPa; the highest value was 34.8 MPa, with 50% of the groups’ means being lower than 11.0 MPa.
Figure 1.
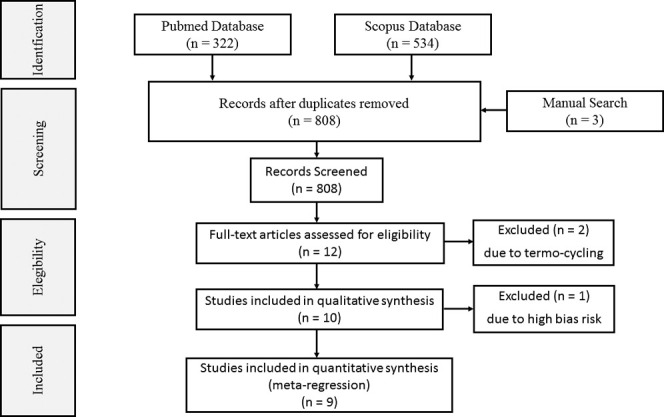
Systematic review flow chart of studies comparing shear bond strength of metal brackets bonded to enamel with and without adhesive resin application.
Table 1.
Bias Risk Analysis
Table 2.
Descriptive Data, Random Effects, Confidence Interval, and Weight of Studies
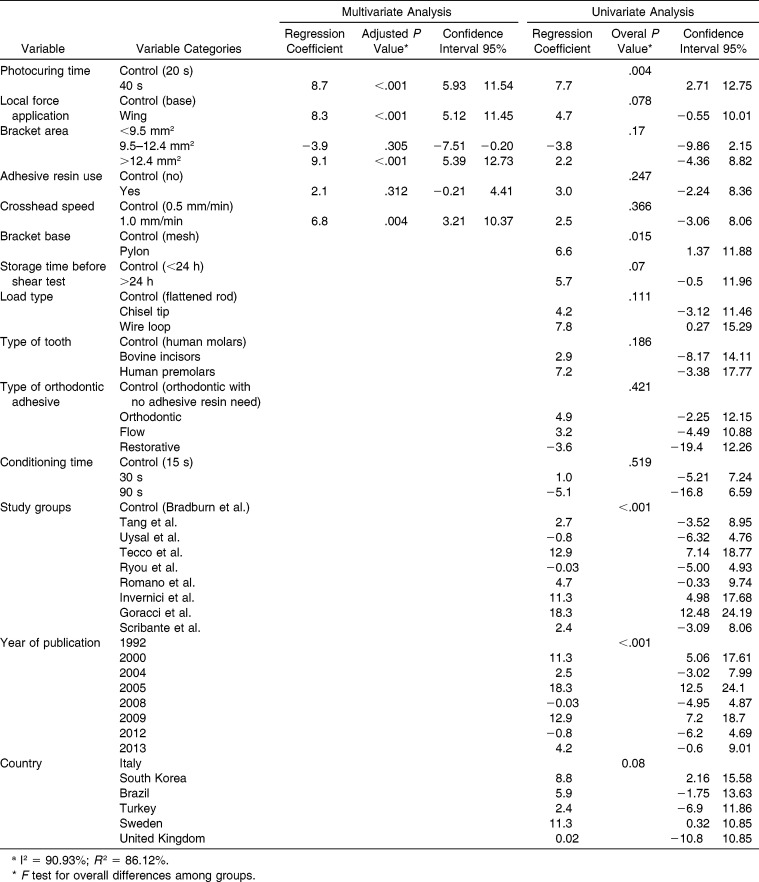
Based on the pooled data and due to a high heterogeneity among studies (I2 = 93.3), a meta-regression analysis was conducted. Results of the uni- and multivariate tests are presented in Table 3. Results from the nine included studies were based on the means and standard errors of 31 groups from 530 specimens.
Table 3.
Multivariate and Univariate Analysis of All Variables with SBS as the Dependent Variablea
The diagnostic of the final model showed that it explained 86.1% of the between-groups variance (if the model has a value of 100%, then the outcome can be perfectly predicted by the covariates in the model). Moreover, the within-groups variance was significant (P < .001). The studentized residuals were not homoscedastic or normally distributed; there were no influences of outliers or leverage.
DISCUSSION
Some factors tend to play a major role in bracket/tooth interfaces.2,8,9 Thereby, in contrast to previous studies,12,14,15 no significant difference of the pooled results of this meta-regression was shown between use and nonuse of adhesive resin. As heterogeneity among the included studies was high (I2 = 93.32), a meta-regression analysis was performed to relate the “adhesive resin use” variable with other variables tested. Results from the meta-regression in this systematic review indicated that the laboratory conditions of photo-curing time, local force application, bracket area, adhesive resin used, and crosshead speed of the testing machine significantly influenced the bond strength of metal brackets.
The high heterogeneity within orthodontic bond strength studies had been previously shown in systematic reviews9,18 and experimental researches.19,20 This variation occurred mostly because of different methodological approaches used in each study (R 2 = 83.15). Moreover, in our multivariate model, the five aforementioned variables explained 86.1% of this heterogeneity; this result could serve as a standardization guide for further in vitro studies.
The prior application of adhesive resin to bracket bonding increased, on average, 2.1 MPa with no statistical difference when compared with no adhesive resin application. Our result corroborates other studies.7,21,22 This might imply that after acid etching, the surface tension of enamel seems to play a major role in enhancing the mechanical interlocking between demineralized prisms and resin. Jendresen and Glantz23 showed an increase of this superficial tension after enamel etching. Hence, the achievement of desirable shear strength does not depend on the requirement of adhesive resin wettability. This consideration may be valid for both as flowable,24 orthodontic,17 or restorative resins, since no significant differences in bond strength were found among them (P = .42), and this adhesive variable did not interfere with the ones included on the multivariate test. According to Shahabi et al.,21 another suggestion of adhesive resin application to protect enamel against debonding force25 is not unanimous, owing to their findings that the application had no effect on the quality or quantity of cracks whether it was applied in one or two layers. Although uncured adhesive resins have proven to have greater cytotoxicity for gingival fibroblasts,4 they generate oxidative stress or induce a pathophysiological increase in cellular calcium level, killing their target cells by apoptosis.26 Regarding microleakage under bonded stainless steel brackets, several studies have demonstrated relevant effects related to the etching method whereas the type of adhesive made no difference.27,28
Photo-activation time of 40 seconds increased bond strength by 8.7 MPa. Since metal brackets are opaque, polymerization of resin may not be complete.29 The mouth has a harsh environment, and light activation for 20 seconds may not be enough to adequately convert the orthodontic resin.30 In our study, each second of photo-activation increased bond strength by 0.43 MPa; this was more intense than the 0.077 MPa increase found by Finemma et al.9 Nevertheless, these results suggest that longer activation cycles yield higher shear bond strengths, thus higher degrees of conversion and, consequently, higher likelihood of resin polymerization.
The third condition that significantly altered the shear bond strength was the local force application. Loading the wings resulted in an increase of 8.3 MPa on bond strength, contradicting a previous study20 that found higher shear bond strength on the bracket base compared with the wings. One specific study,3 in which mean values of the shear test were much higher than in other studies, might influence this finding. Another factor that might be involved is the difficulty of performing a pure shear test. Different force directions of debonding may occur as bracket bases are not all flat, so the force is easier to apply on the ligature groove or bracket wings leading to shear and tension loads.
The shear bond strength of brackets with an area between 9.5 mm2 and 12.4 mm2 was 3.9 MPa lower than that of brackets having <9.5 mm2 of area. This might have occurred owing to the different shapes of the bracket bases. Normally, brackets with areas ranging from 9.5 mm2 to 12.4 mm2 are used specifically in premolars; hence, their bases are curved, leading to different resin thickness between the enamel and bracket. Increased adhesive thickness is a critical parameter that results in a weak interface due to greater polymerization shrinkage and thermal expansion of the resin matrix.31 As reported previously,32 different shear bond strength values were obtained when the thickness changed from 0.99 mm to 0.72 mm. A bracket base area >12.4 mm2 increases the bond strength to 9.1 MPa. Bracket areas over 12.4 mm2 are generally used on central incisors. Thus, several authors12,33,34 have shown that bond strength obtained on anterior teeth are higher than that on posteriors.
The last condition included in the multivariate analysis was the crosshead speed of the testing machine. Our study showed an increase of 6.8 MPa for a speed increase of 0.5 mm/min. This result was similar to the findings of Finemma et al.,9 and no clear physicochemical explanation was found for the discrepancies with other studies.35,36 The increase of 0.5 mm/min seems to be low to be related to the elimination of the viscoelastic response of the polymeric adhesive and a consequent induction of a stiff body response.37 One suggestion is that, with 0.5 mm/min speed, the chisel would be in contact with the body for a longer time, increasing the strains in the bond interface, whereas the contact period of the 1.0 mm/min speed would be shorter, decreasing strain and thus increasing bond strength.
Other important variables cited in previous studies8,17 were included solely for the univariate model. We included studies that used bovine or human teeth, with no significant difference between them. For this reason, bovine enamel has been demonstrated to be a reliable substitute for human enamel in shear bonding studies, as previously.38 The bracket base design showed a significant difference (P < .05) with increased shear bond strength by 6.6 MPa with the pylon base. This difference can be explained by a discrepancy in the surface roughness between mesh and pylon bases2 and the amount of penetration of the adhesive material.39 It is worth mentioning that in our study the adhesive types and storage time before testing had no significant influence on the shear bond strength. The behavior of each type of adhesive has been related to its polymerization shrinkage and wettability properties.8 Notwithstanding, lower bond strengths of the flowable composites were not because of a weak bond with the enamel, but rather a consequence of their inferior mechanical properties.15
Most studies presented low risk of bias, but four included studies presented moderate risk and one study was excluded due to high risk of bias. Moderate bias risk may represent a limitation of this study. On the other hand, inclusion of moderate-risk-of-bias studies did not influence results, as no outlier or leverage groups were found. In addition, exclusion of such studies would reduce the power of our study.
The current literature has been systematically reviewed for in vitro studies that either used or avoided adhesive resins. However, this study presents limitations, as heterogeneity seems to be intrinsically linked to the lack of standardization of methodological reports of in vitro bond strength studies. Another possible limitation of this study is that many in vitro studies of orthodontic bond strength fail to report test conditions that could affect their outcomes.9 Furthermore, different test conditions could lead to different bond strength values as shown elsewhere.40 Further in vitro study reports need standardization to achieve more translational and comparable data.
It is not possible to predict the clinical use of a material based only on its in vitro shear bond strength. There have been attempts to establish a bond strength value that could predict clinical outcome,41–43 but no such value has been established. There is evidence that indicates an association of in vitro bond strength and restoration longevity.44 Given the wide range of numerical outcomes and high variation of test parameters, it is difficult to determine values. Moreover, different forces acting on brackets may play an important role in clinical bond strength values, such as occlusal interferences and masticatory forces.45 For all that, taking restorations as a parameter, the greater the bond strength, greater the longevity. Furthermore, in the field of dental materials is required to develop new materials and explain the mechanisms involved in the phenomena.46
CONCLUSIONS
The prior application of adhesive resin does not influence the bond strength of orthodontic adhesives. Thus, this step could be set aside during metal bracket bonding to enamel regardless of the type of orthodontic adhesive used.
The variables that significantly do influence in vitro bond strength are photo-curing time, force location, bracket area, and crosshead speed of the testing machine.
REFERENCES
- 1.Bishara SE, VonWald L, Laffoon JF, Warren JJ. Effect of a self‐etch primer/adhesive on the shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2001;119:621–624. doi: 10.1067/mod.2001.113269. [DOI] [PubMed] [Google Scholar]
- 2.Scribante A, Sfondrini MF, Fraticelli D, Daina P, Tamagnone A, Gandini P. The influence of no‐primer adhesives and anchor pylons bracket bases on shear bond strength of orthodontic brackets. BioMed Res Int. 2013;2013:1–6. doi: 10.1155/2013/315023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tecco S, Traini T, Caputi S, Festa F, de Luca V, D’Attilio M. A new one‐step dental flowable composite for orthodontic use: an in vitro bond strength study. Angle Orthod. 2005;75:672–677. doi: 10.1043/0003-3219(2005)75[672:ANODFC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Tang AT, Liu Y, Bjorkman L, Ekstrand J. In vitro cytotoxicity of orthodontic bonding resins on human oral fibroblasts. Am J Orthod Dentofacial Orthop. 1999;116:132–138. doi: 10.1016/s0889-5406(99)70209-x. [DOI] [PubMed] [Google Scholar]
- 5.James JW, Miller BH, English JD, Tadlock LP, Buschang PH. Effects of high‐speed curing devices on the shear bond strength and microleakage of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2003;123:555–561. doi: 10.1067/mod.2003.S0889540602000197. [DOI] [PubMed] [Google Scholar]
- 6.Shahabi M, Ahrari F, Mohamadipour H, Moosavi H. Microleakage and shear bond strength of orthodontic brackets bonded to hypomineralized enamel following different surface preparations. J Clin Exp Dent. 2014;6:e110–e115. doi: 10.4317/jced.51254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naidu E, Stawarczyk B, Tawakoli PN, Attin R, Attin T, Wiegand A. Shear bond strength of orthodontic resins after caries infiltrant preconditioning. Angle Orthod. 2013;83:306–312. doi: 10.2319/052112-409.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goracci C, Margvelashvili M, Giovannetti A, Vichi A, Ferrari M. Shear bond strength of orthodontic brackets bonded with a new self‐adhering flowable resin composite. Clin Oral Investig. 2013;17:609–617. doi: 10.1007/s00784-012-0729-x. [DOI] [PubMed] [Google Scholar]
- 9.Finnema KJ, Ozcan M, Post WJ, Ren Y, Dijkstra PU. In‐vitro orthodontic bond strength testing:a systematic review and meta‐analysis. Am J Orthod Dentofacial Orthop. 2010;137:615–622. doi: 10.1016/j.ajodo.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG; Prisma Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 11.O’Brien KD, Watts DC, Read MJ. Light cured direct bonding: is it necessary to use a primer. Eur J Orthod. 1991;13:22–26. doi: 10.1093/ejo/13.1.22. [DOI] [PubMed] [Google Scholar]
- 12.Bradburn G, Pender N. An in vitro study of the bond strength of two light‐cured composites used in the direct bonding of orthodontic brackets to molars. Am J Orthod Dentofacial Orthop. 1992;102:418–426. doi: 10.1016/s0889-5406(05)81188-6. [DOI] [PubMed] [Google Scholar]
- 13.Tang AT, Bjorkman L, Adamczak E, Andlin‐Sobocki A, Ekstrand J. In vitro shear bond strength of orthodontic bondings without liquid resin. Acta Odontol Scand. 2000;58:44–48. doi: 10.1080/000163500429424. [DOI] [PubMed] [Google Scholar]
- 14.Uysal T, Sari Z, Demir A. Are the flowable composites suitable for orthodontic bracket bonding? Angle Orthod. 2004;74:697–702. doi: 10.1043/0003-3219(2004)074<0697:ATFCSF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Ryou DB, Park HS, Kim KH, Kwon TY. Use of flowable composites for orthodontic bracket bonding. Angle Orthod. 2008;78:1105–1109. doi: 10.2319/013008-51.1. [DOI] [PubMed] [Google Scholar]
- 16.Romano FL, Correr AB, Correr Sobrinho L, Magnani MBB, de Siqueira VCV. Shear bond strength of metallic brackets bonded with a new orthodontic composite. Braz Oral J Sci. 2009;8:76–80. [Google Scholar]
- 17.Invernici SM, Maruo IT, Camargo ES, et al. Influence of Ortho Primer Morelli adhesion booster on orthodontic brackets shear bond strength. Dental Press J Orthod. 2012;17:31–39. [Google Scholar]
- 18.Mandall NA, Millett DT, Mattick CR, Hickman J, Worthington HV, Macfarlane TV. Orthodontic adhesives: a systematic review. J Orthod. 2002;29:205–210. doi: 10.1093/ortho/29.3.205. [DOI] [PubMed] [Google Scholar]
- 19.Eliades T, Brantley WA. The inappropriateness of conventional orthodontic bond strength assessment protocols. Eur J Orthod. 2000;22:13–23. doi: 10.1093/ejo/22.1.13. [DOI] [PubMed] [Google Scholar]
- 20.Klocke A, Kahl‐Nieke B. Influence of force location in orthodontic shear bond strength testing. Dent Mater. 2005;21:391–396. doi: 10.1016/j.dental.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Shahabi M, Heravi F, Mokhber N, Karamad R, Bishara SE. Effects on shear bond strength and the enamel surface with an enamel bonding agent. Am J Orthod Dentofacial Orthop. 2010;137:375–378. doi: 10.1016/j.ajodo.2008.03.030. [DOI] [PubMed] [Google Scholar]
- 22.Vicente A, Bravo LA, Romero M, Ortiz AJ, Canteras M. Effects of 3 adhesion promoters on the shear bond strength of orthodontic brackets: an in‐vitro study. Am J Orthod Dentofacial Orthop. 2006;129:390–395. doi: 10.1016/j.ajodo.2004.08.022. [DOI] [PubMed] [Google Scholar]
- 23.Jendresen MD, Glantz PO. Clinical adhesiveness of selected dental materials. An in‐vivo study. Acta Odontol Scand. 1981;39:39–45. doi: 10.3109/00016358109162257. [DOI] [PubMed] [Google Scholar]
- 24.Frankenberger R, Lopes M, Perdigao J, Ambrose WW, Rosa BT. The use of flowable composites as filled adhesives. Dent Mat. 2002;18:227–238. doi: 10.1016/s0109-5641(01)00040-9. [DOI] [PubMed] [Google Scholar]
- 25.Wang WN, Tarng TH. Evaluation of the sealant in orthodontic bonding. Am J Orthod Dentofacial Orthop. 1991;100:209–211. doi: 10.1016/0889-5406(91)70057-4. [DOI] [PubMed] [Google Scholar]
- 26.VandeVannet BM, Hanssens JL. Cytotoxicity of two bonding adhesives assessed by three‐dimensional cell culture. Angle Orthod. 2007;77:716–722. doi: 10.2319/052706-212.1. [DOI] [PubMed] [Google Scholar]
- 27.Li ZM, Chen SH, Liu XQ, Chen J, Li NY. Effect of bonding materials and methods on microleakage around the edge of stainless‐steel brackets: an in vitro study. Shangai Kou Qiang Yi Xue. 2005;14:645–647. [PubMed] [Google Scholar]
- 28.Yagci A, Uysal T, Ulker M, Ramoglu SI. Microleakage under orthodontic brackets bonded with the custom base indirect bonding technique. Eur J Orthod. 2010;32:259–263. doi: 10.1093/ejo/cjp090. [DOI] [PubMed] [Google Scholar]
- 29.Wendl B, Droschl H, Kern W. A comparative study of polymerization lamps to determine the degree of cure of composites using infrared spectroscopy. Eur J Orthod. 2004;26:545–551. doi: 10.1093/ejo/26.5.545. [DOI] [PubMed] [Google Scholar]
- 30.Ilie N, Obermaier J, Durner J. Effect of modulated irradiation time on the degree of conversion and the amount of elutable substances from nano‐hybrid resin‐based composites. Clin Oral Investig. 2014;18:97–106. doi: 10.1007/s00784-013-0934-2. [DOI] [PubMed] [Google Scholar]
- 31.Eliades T, Viazis AD, Eliades G. Bonding of ceramic brackets to enamel: morphologic and structural considerations. Am J Orthod Dentofacial Orthop. 1991;99:369–375. doi: 10.1016/0889-5406(91)70020-W. [DOI] [PubMed] [Google Scholar]
- 32.Jain M, Shetty S, Mogra S, Shetty VS, Dhakar N. Determination of optimum adhesive thickness using varying degrees of force application with light‐cured adhesive and its effect on the shear bond strength of orthodontic brackets: an in vitro study. Orthodontics. 2013;14:40–49. doi: 10.11607/ortho.919. [DOI] [PubMed] [Google Scholar]
- 33.Knoll M, Gwinnett AJ, Wolff MS. Shear strength of brackets bonded to anterior and posterior teeth. Am J Orthod. 1986;89:476–479. doi: 10.1016/0002-9416(86)90003-5. [DOI] [PubMed] [Google Scholar]
- 34.Pender N, Dresner E, Wilson S, Vowles R. Shear strength of orthodontic bonding agents. Eur J Orthod. 1988;10:374–379. doi: 10.1093/ejo/10.4.374. [DOI] [PubMed] [Google Scholar]
- 35.Bishara SE, Soliman M, Laffoon J, Warren JJ. Effect of changing a test parameter on the shear bond strength of orthodontic brackets. Angle Orthod. 2005;75:832–835. doi: 10.1043/0003-3219(2005)75[832:EOCATP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 36.Eliades T, Katsavrias E, Zinelis S, Eliades G. Effect of loading rate on bond strength. J Orofac Orthop. 2004;65:336–342. doi: 10.1007/s00056-004-0327-x. [DOI] [PubMed] [Google Scholar]
- 37.Chabrier F, Lloyd CH, Scrimgeour SN. Measurement at low strain rates of the elastic properties of dental polymeric materials. Dent Mater. 1999;15:33–38. doi: 10.1016/s0109-5641(99)00011-1. [DOI] [PubMed] [Google Scholar]
- 38.Nakamichi I, Iwaku M, Fusayama T. Bovine teeth as possible substitutes in the adhesion test. J Dent Res. 1983;62:1076–1081. doi: 10.1177/00220345830620101501. [DOI] [PubMed] [Google Scholar]
- 39.Knox J, Hubsch P, Jones ML, Middleton J. The influence of bracket base design on the strength of the bracket‐cement interface. J Orthod. 2000;27:249–254. doi: 10.1179/ortho.27.3.249. [DOI] [PubMed] [Google Scholar]
- 40.Collares FM, Rodrigues SB, Leitune VC, Celeste RK, Borba de Araujo F, Samuel SM. Chlorhexidine application in adhesive procedures: a meta‐regression analysis. J Adhes Dent. 2013;15:11–18. doi: 10.3290/j.jad.a28732. [DOI] [PubMed] [Google Scholar]
- 41.Eminkahyagil N, Arman A, Cetinsahin A, Karabulut E. Effect of resin‐removal methods on enamel and shear bond strength of rebonded brackets. Angle Orthod. 2006;76:314–21. doi: 10.1043/0003-3219(2006)076[0314:EORMOE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 42.Retief DH. Failure at the dental adhesive‐etched enamel interface. J Oral Rehabil. 1974;1:265–284. doi: 10.1111/j.1365-2842.1974.tb01438.x. [DOI] [PubMed] [Google Scholar]
- 43.Scougall‐Vilchis RJ, Ohashi S, Yamamoto K. Effects of 6 self‐etching primers on shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2009;135:424.e1–e7. doi: 10.1016/j.ajodo.2008.12.005. discussion 24–25. [DOI] [PubMed] [Google Scholar]
- 44.Van Meerbeek B, Peumans M, Poitevin A, Mine A, Van Ende A, Neves A, et al. Relationship between bond‐strength tests and clinical outcomes. Dent Mater. 2010;26:e100–e121. doi: 10.1016/j.dental.2009.11.148. [DOI] [PubMed] [Google Scholar]
- 45.Elsaka SE, Hammad SM, Ibrahim NF. Evaluation of stresses developed in different bracket‐cement‐enamel systems using finite element analysis with in vitro bond strength tests. Prog Orthod. 2014;15:33. doi: 10.1186/s40510-014-0033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Collares FM, Klein M, Santos PD, Portella FF, Ogliari F, Leitune VC, et al. Influence of radiopaque fillers on physicochemical properties of a model epoxy resin‐based root canal sealer. J Appl Oral Sci. 2013;21:533–539. doi: 10.1590/1679-775720130334. [DOI] [PMC free article] [PubMed] [Google Scholar]