Abstract
Objective:
To explore the impact of fixed labial orthodontic appliances on speech sound production.
Materials and Methods:
Speech evaluations were performed on 23 patients with fixed labial appliances. Evaluations were performed immediately prior to appliance insertion, immediately following insertion, and 1 and 2 months post insertion. Baseline dental/skeletal variables were correlated with the ability to accommodate the presence of the appliances.
Results:
Appliance effects were variable: 44% of the subjects were unaffected, 39% were temporarily affected but adapted within 2 months, and 17% of patients showed persistent sound errors at 2 months. Resolution of acquired sound errors was noted by 8 months post–appliance removal. Maladaptation to appliances was correlated to severity of malocclusion as determined by the Grainger’s Treatment Priority Index. Sibilant sounds, most notably /s/, were affected most often.
Conclusions:
(1) Insertion of fixed labial appliances has an effect on speech sound production. (2) Sibilant and stopped sounds are affected, with /s/ being affected most often. (3) Accommodation to fixed appliances depends on the severity of malocclusion.
Keywords: Orthodontic appliances, Speech sound production, Malocclusion, Speech adaptation and Grainger’s Treatment Priority Index (GTPI)
INTRODUCTION
The maxillary and mandibular arches are directly involved in the production of certain individualized sounds, or phonemes /t,d,n,l/, and indirectly in others (/s,z,f,v,th/). They also act as structural boundaries for the lips in the production of the bilabial phonemes/m,p,b/.1 When a structural malformation occurs, consonant production may be disrupted and errors in sound production affecting speech intelligibility may occur.
Studies exploring the relationship between fixed orthodontic appliance placement and speech sound production are scant, with most (1) focusing on the impact of lingual appliances on articulation2–5; (2) focused on children with factors such as digit habits, tongue thrust, and developing speech6; and (3) focused across languages.6–13 Such studies have described a transient effect, with acquired errors resolved within 2 to 3 months.2–4,14 The phonemes acknowledged to present lingering difficulties with articulation are /s/,/f/,/v/,/t/,/r/,/n/, and /l/ phonemes.5,6,14
Feldman15 presented the sole article containing data on the effects of labial fixed appliances in 1956 and reported an increase in errors immediately after appliance insertion, with resolution within weeks. Though useful, this study presents several shortcomings: small sample size, appliance variability, lack of sound error type and uniformity in evaluating sample readings, a lack of adult patients, and, finally, a lack of attention to malocclusions that may predispose one to maladaptation.
The purpose of this study was to examine the effects of fixed labial appliances on English spoken speech sound production in a mature population and to identify malocclusal or treatment variables that may predispose patients to be maladaptive.
MATERIALS AND METHODS
Institutional review board approval was granted to conduct this study. Twenty-three patients assessed as needing fixed labial appliance therapy not requiring lingual or palatal anchorage devices were consecutively recruited over the course of 8 months. Exclusion criteria included the following: (1) overt dysmorphology, such as cleft lip and/or palate, (2) neurologic disorders, (3) tongue thrust habits, (4) hearing deficits, (5) prior orthodontic treatment, and (6) history of speech or hearing therapy.
The appliances used were all metal brackets. All of the bracket dimensions were measured, and differences were found to be negligible (ie, <0.05 mm) among the various bracket types; therefore, appliances were viewed as one group for the purposes of this study. The dental criteria evaluated included Angle classification (molar), overjet, overbite/open bite, crowding/spacing, and anterior/posterior crossbite. A Grainger’s Treatment Priority Index (GTPI) score was tabulated for each patient. Cephalometric data included skeletal classification, vertical relationship (SN/MP), upper and lower incisor inclination (U1/PP and L1/MP), and facial divergency. Skeletal classification and divergency were determined by performance of the quadrilateral and mesh analyses. Cephalographs were taken prior to treatment with a fixed head-to-film distance of 13 cm. Initial archwire size and composition were recorded. For patients undergoing extractions, the time of extractions was noted.
Speech samples were administered at the following intervals: time point 1: immediately prior to appliance insertion; time point 2: immediately following appliance insertion; time point 3: 4–5 weeks post insertion; and time point 4: 8–10 weeks postinsertion. All dental measurements were assessed and recorded on two separate occasions by the principal investigator using study casts. Skeletal measurements were obtained via cephalometric tracings by the investigator and were compared to those made by the treating orthodontists.
Speech Data Collection
Speech samples were obtained in a video imaging room with a reduced-noise environment. The patient was seated in an upright position with a mounted video camera recorder (Sony™ Camera, Model No. CCD-TR700, Park Ridge, NJ) positioned 12–18 inches away from the patient's face. The camera’s image was viewed on the monitor of a computer screen linked to the video recorder for imaging purposes.
Each image, incorporating the subject’s mouth and perioral structures extending from subnasale to menton, was focused to fit into a 3 × 2.5-inch window on the computer screen. Zoom capabilities facilitated careful assessment of the labial and lingual movements made during sound production and recorded for speech assessments at a later date. To enhance acoustic proficiency an omni-directional microphone (Sony™ F-V5) was positioned at shoulder height, 2 inches below the patient’s chin level.
At each time point, the subjects were asked to repeat a standard English language speech sample via imitation. The investigator stated the desired sound or utterance that was then repeated by the subject. A practice utterance was established prior to data recording. The examiner was allowed to repeat the utterance if so desired by the subject. The patient was instructed to look directly into the camera lens. During this process, the investigator stood behind the patient so as to not offer any visual cues and to eliminate any bias of using a visual model for the speech sample.
Certain specific target sounds were examined. These were /t/,/p/,/f/,/s/,/sh/,/ch/,/dz/,/k/,/th/,/l/, and /m/. These consonants were chosen because the areas covered by the appliances are employed in the production of these consonants. Voiced sounds such as /d/, /b/, /v/, and /z/ were not directly studied as a result of the common manner and placement shared with their corresponding targeted sounds /t/, /p/, /f/, and /s/.16
Two speech pathologists and one speech physiologist performed assessments. Each assessment was scored randomly through arbitrary assignment by the principal investigator and via panel analysis by the three examiners. The evaluations entailed perceptual, visual, and physiologic assessment of articulatory data, with target sounds analyzed at the isolated sound, syllable, word, phrase, conversational, and counting levels. The following speech sound variables were considered for each target sound: (1) Placement: anatomic location of sound placement (ie, interdental, dental edge, or labial); (2) Manner: integrity of oral airflow and air pressure (ie, lateralized, weak, or with increased anterior air); and (3) Error: type of speech sound disorder (ie, substitution, distortion, or deletion).
Statistical Analysis
For continuous variables such as age, dental millimetric measurements, and skeletal angular measurements, associations with immediate adaptation and adaptation over time were tested with a t-test. Since the GTPI scale was ordinal, the association for GTPI scores with each sound production variable was tested for significance using a Wilcoxon rank sum test. For associations with categorical variables, such as gender type, Angle classification, skeletal classification, and appliance type, a Chi-square test or Fisher’s exact test was performed, depending on the amount of categories in each variable. Relative frequency distributions were calculated for each type of sound production variable as well as for categorical malocclusion and treatment variables. Means and standard deviations (SDs) or medians and ranges were calculated for each continuous variable, as appropriate. All tests of significance were two-tailed and performed using a Type I error of .05.
RESULTS
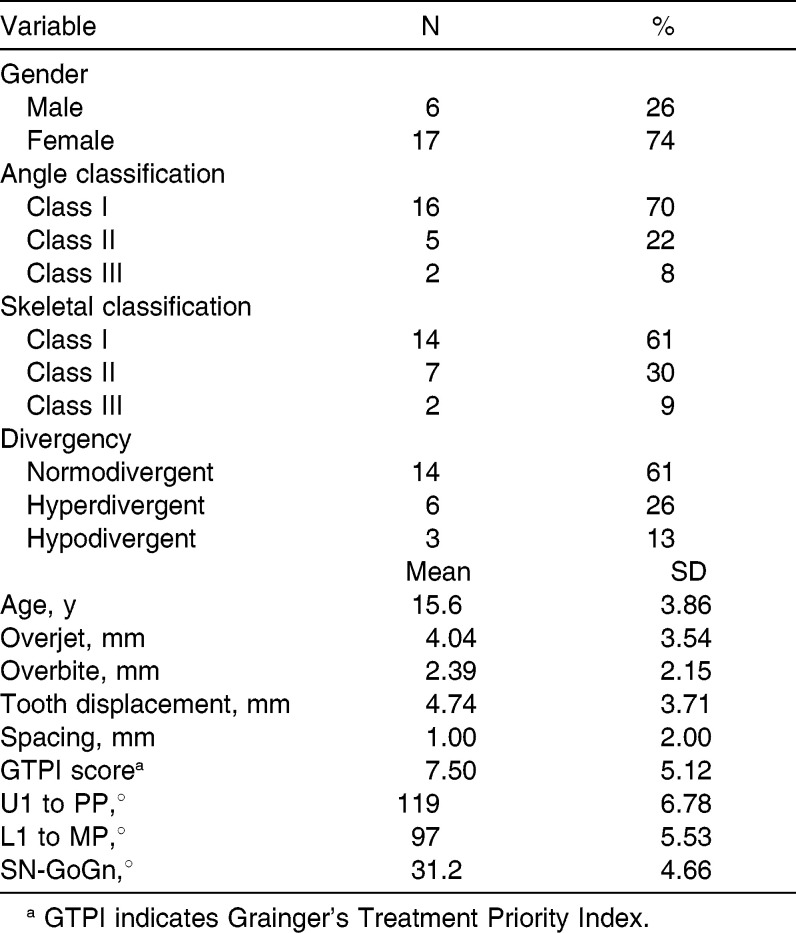
Subject Profile (Table 1)
Table 1.
Demographic and orthodontic characteristics of our study sample: Inclusive of their average age, number per gender, as well as, selected average dental & skeletal measurements for the sample group studied.
The subject pool comprised six males (26%) and 17 females (74%) ranging from 11 years to 24 years 11 months in age (mean = 15.6 years, SD = 3.86 years). Sixteen (70%) subjects had an Angle Class I malocclusion, five (22%) had a Class II division 1 malocclusion, and two subjects (8%) had a Class III malocclusion.
General Findings (Figure 1)
Figure 1.
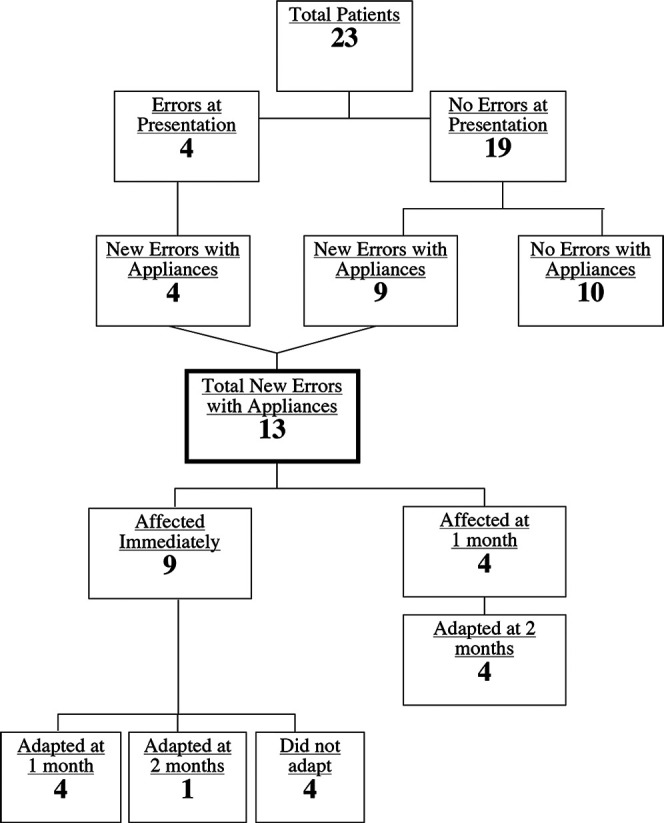
Distribution of study patients.
Each of the 23 subjects had some degree of malocclusion: four (17%) demonstrated a baseline sound production, while the remaining had no sound error at baseline. Within 2 months, an additional nine (39%) subjects exhibited errors following the insertion of appliances, yielding 13 (56%) subjects with new sound errors after appliance insertion. Ten subjects (44%) never exhibited any sound errors throughout the study.
Among the 13 patients with errors following insertion, nine (69%) demonstrated changes at the time point immediately following insertion, while the remaining four (31%) patients first showed changes 1 month later.
Four of the nine patients who produced new sound errors after appliance placement resolved these sound errors at the 1-month interval, one (11%) patient had resolution at the 2-month interval, and four (44%) patients continued with sound errors at the 2-month time point. All (100%) of the four patients who exhibited new errors 1 month after appliance placement resolved their sound errors at 2 months.
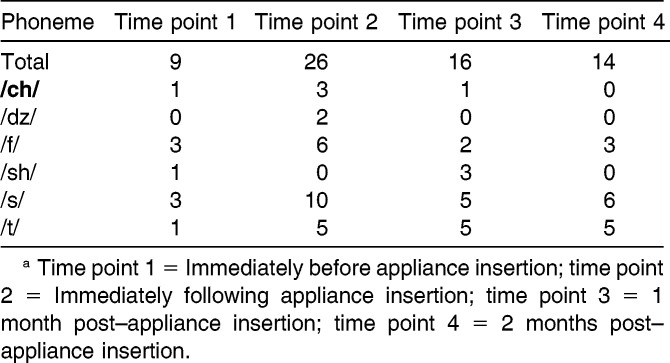
Phonemic Findings (Table 2)
Table 2.
Number and type of phonemis errors observed at the various time points throughout the course of our study.a
Only six of the 11 speech sounds examined resulted in sound errors (ie, /ch/, /dz/, /sh/, /f/, /s/, and /t/). Nine sound errors were seen at the initial evaluation, while 26 errors were detected immediately following appliance insertion, reflecting a threefold increase in errors. The number of errors decreased to 16 at the 1-month mark and to 14 at the 2-month mark. Among the six phonemes found with errors at baseline, the /s/ and /sh/ sounds were most commonly defective (ie, three of each type). At time point 2 the most affected sounds were /s/ and /t/, with increases of seven and four errors respectively. After 2 months, most sound errors had resolved, save for the /s/ and /t/ sounds, which continued to have increases of three and four errors, respectively.
Mechanism of Errors in Sound Production
Certain patients (ie, 11 of them, or 85%) exhibited anterior tongue movements during sound production, with sounds produced dentally (fronting), while one patient (7.5%) displayed a retracted mandibular position. One patient (7.5%) had variable changes that did not indicate a specific pattern. In distinguishing between sibilant and stopp consonant sounds among the 11 patients with dentalized sounds, eight (73%) showed dentalization for both the stopp consonant and sibilant sounds and three (27%) showed fronting for the sibilants only. The primary sounds affected were /s/ in the sibilant group and /t/ in the stopp consonant group.
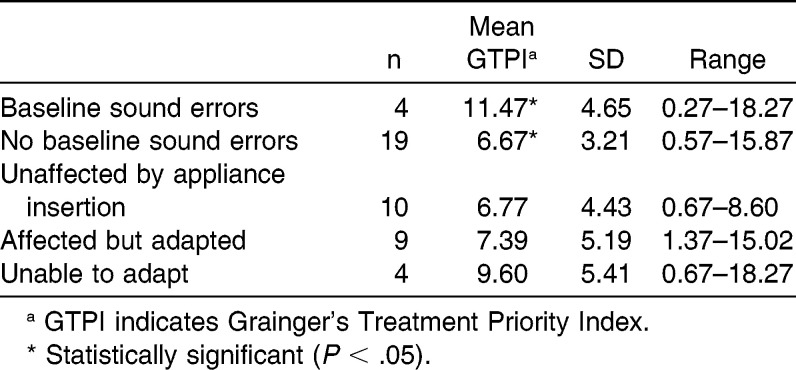
Association with the Malocclusion Variables
No relationship was detected with any of the major malocclusion variables studied. The only statistically significant correlation seen was with the GTPI (Table 3). The mean GTPI among the patients who did not demonstrate errors following appliance insertion was 6.77 (n = 10, SD = 4.43). For those patients who demonstrated sound errors, the mean GTPI was 8.07 (n = 13, SD = 5.12). Interestingly, the mean GTPI for those patients who had sound errors at baseline was 11.47 (n = 4, SD = 4.65), compared to a mean GTPI of 6.67 (n = 19, SD = 3.21) for those without sound errors at baseline.
Table 3.
The average GTPI scores of our study sample related to errors noted throughout the course of our study.
In comparing the GTPI scores of patients showing resolution of new sound errors and those showing continued sound errors throughout the 2-month study period, it was noted that the mean GTPI score for patients showing resolution was 7.39 (n = 9, SD = 5.19). The mean GTPI score for those subjects continuing to demonstrate new errors was 9.60 (n = 4, SD = 5.41). Both patients with anterior open bites were among those patients who continued to show additional errors at the 2-month evaluation.
DISCUSSION
Our study results showed that the insertion of labial fixed appliances did have a negative impact on speech sound production in a majority of patients (57%). Surprisingly, 17% of all patients, or 31% of affected patients, continued to show changes in sound errors after 2 months. These results document a greater impact generated by labial appliance insertion than was noted in Feldman’s study. However, our findings were consistent with those of the Khattab et al.14 randomized controlled study (although to a lesser degree than those treated with lingual appliances), in which all of patients accommodated the appliances within weeks.6,14
As in earlier studies,16–18 the phonemic errors seen,/s/ and /t/, were most commonly affected by the presence of labial fixed appliances. There are differences between how obstructions are caused by malocclusion and by labial appliances, but comparisons can be made, as /s/ and /t/ were the most affected phonemes in this study as well as in other studies. Moreover, /s/ and /t/ findings were the most frequent sound error across languages as well.6–13
In a study by Leavy et al.,16 lingual protrusion was found to be the most common visual inaccuracy among patients with malocclusions. As Subtelny and coworkers17 noted, the articulatory error of /s/can be a result of excessive fronting of the tongue. Comparable results were seen in the present study, supporting the hypothesis that any irregularity, particularly in the anterior region of the mouth, can provoke a forward placement of the tongue. This was also noted in a parallel study10 exploring the impact of retainer insertion on speech. Clearly this doesn’t always happen, as 44% of our patients were unaffected.
Attempts at correlating occlusal variables with appliance insertion were rather fruitless. One malocclusion variable stood out significantly and that was GTPI: specifically, the disparity seen between the GTPI scores of those patients with baseline sound errors and those without (Table 3). Such differences support the observations by others16 who established a relationship between severity of malocclusion and speech sound errors without appliances.
Similarly, a higher GTPI score was seen among those patients who were unable to adapt to the appliances when compared to those who were able to accommodate to their presence. Although not statistically significant, a trend was seen in that the more severe malocclusions could lend themselves to maladaptation, initially as well as over time. A limiting factor of our study was that we did not control for changes in tongue posture, articulatory precision, and strength of contact due to discomfort and pain resulting from appliance insertion and/or maintenance. Khattab et al.14 reported on differences in discomfort based on whether a lingual or labial appliance was used (lingual appliances caused more discomfort than labial); however, their study did not comment on whether there was a relationship related to sound errors associated with the type of appliance used.
The four patients who continued to show acquired sound errors during later months were recalled after 6–8 months, and all showed resolution of the acquired errors and reported spontaneous resolution. Perhaps the further correction of the malocclusion over time, particularly among the open-bite patients, contributed to this resolution, but that is a question for another study. Although our study period of 8–10 weeks was three times longer than those of prior studies, ideally a longer-term study might have provided useful information regarding the long-term effects of orthodontic treatment on speech.
It was important to limit observer bias, as examiners could detect the presence of appliances when viewing the speech samples. Samples from a parallel study19 on the effects of removable appliances were mixed with our samples. The variety of appliance types and the multiple time points randomly assorted was helpful in reducing observer bias.
It is apparent that some individuals adapt to the presence of labial appliances more readily than do others. In recent years, attention has been paid to the neural correlates of muscular adaptive and maladaptive changes in response to environmental signals. There have been attempts to understand this adaptive and maladaptive response across individuals as research has been focused on neurologic impairments following adult brain injury.20,21 As Ackerman and Profitt once so eloquently posed the concept of equilibrium, perhaps neural connections may be programmed to maintain “equilibrium” by relearning/accommodating. However, not all adapt to the changes in the same manner.
Very little attention has been paid to neural changes occurring in speech due to dentoskeletal changes. Understanding the adaptive and maladaptive concepts of neural equilibrium will have great impact on rehabilitation interventions. Manifestations of change, plasticity, or adaptation can now be linked to brain activation patterns and learning.22
For individuals seeking orthodontic treatment, it is important that they fully understand the risks that the type of appliance will have in terms of affecting their speech, the types of sound error that may occur, and the period of time during which the errors may exist. In an era during which many professional adults are seeking orthodontic treatment, it is important for the orthodontist to understand and to determine the possible risk factors affecting communication integrity. Perhaps one day we will be able to include in our orthodontic and surgical diagnostic assessment one’s intrinsic adaptability (or lack thereof) to reorganize and change oral function based on environmental change.
CONCLUSIONS
The insertion of fixed labial orthodontic appliances has a variable effect on speech sound production. In some patients, a transient negative change is seen. In others, a more persistent change is seen over a period of 2 months. In approximately 40%, no change is noted.
Both sibilant and stopped sounds are affected by fixed labial appliance insertion. However, the sibilants, most notably /s/, are affected most often.
The ability to accommodate sound production to the presence of fixed labial appliances, immediately and over time, depends to some extent on the severity of the malocclusion.
REFERENCES
- 1.LeBlanc EM, Cisneros GJ. The dynamics of speech and orthodontic management in cleft lip and palate. In: Shprintzen RJ, Bardach J, editors. Cleft Palate Speech Management A Multidisciplinary Approach. St Louis, Mo: Mosby; 1995. pp. 305–326. [Google Scholar]
- 2.Sinclair PM, Cannito MF, Goates LJ, Solomos LF, Alexander CM. Patient responses to lingual appliances. J Clin Orthod. 1986;20:396–404. [PubMed] [Google Scholar]
- 3.Marioti J, Subtelny JD, Baker R, Marioti M. The Speech Effect of the Lingual Appliance. Orange, Calif: ORMCO Co; 1984. [Google Scholar]
- 4.Fillion D. Improving patient comfort with lingual brackets. J Clin Orthod. 1997;31:689–694. [PubMed] [Google Scholar]
- 5.Fujita K. New orthodontic treatment with lingual bracket mushroom arch wire appliance. Am J Orthod Dentofac Orthop. 1979;76:657–675. doi: 10.1016/0002-9416(79)90211-2. [DOI] [PubMed] [Google Scholar]
- 6.Van Lierde KM, Luyten A, D’haeseleer E, Van Maele G, Becue L, Fonteyne E, Corthals P. Articulation and oromyofunctional behavior in children seeking orthodontic treatment. Oral Dis. 2015;21:483–492. doi: 10.1111/odi.12307. [DOI] [PubMed] [Google Scholar]
- 7.Sahad M, Nahas A, Scavone H, Jr, Jabur LB, Guedes-Pinteo E. Vertical interincisal trespass assessment in children with speech disorders. Pediatr Dent. 2008;22:247–251. doi: 10.1590/s1806-83242008000300010. [DOI] [PubMed] [Google Scholar]
- 8.Leme MS, Barbosa T, Gaviao MBD. Relationship among oral habits, orofacial function an oral health-related quality of life in children. Braz Oral Res. 2013;27:272–278. doi: 10.1590/S1806-83242013000300006. [DOI] [PubMed] [Google Scholar]
- 9.Farronato G, Giannini L, Riva R, Galbiati G, Masperio C. Correlations between malocclusions and dyslalias. Eur J Paediatr Dent. 2012;13:13–18. [PubMed] [Google Scholar]
- 10.Onyeasa CO, Aderinokun GA. The relationship between dental aesthetic index (DAI) and perceptions of aesthetics, function, and speech amongst secondary school children in Ibadan, Nigeria. Int J Pediatr Dent. 2003;13:336–341. doi: 10.1046/j.1365-263x.2003.00478.x. [DOI] [PubMed] [Google Scholar]
- 11.Jindra P, Spidien M, Eber M, Pesak J. Evaluation of speech disorders among children with orthodontic anomaly. Biomed Pap Med Fac Univ Palacky Olomous Czech Repub. 2003;147:243–244. [PubMed] [Google Scholar]
- 12.Dimberg L, Lennartsson B, Soderfeldt B, Bondemark L. Malocclusions in children at 3 and 7 years of age: a longitudinal study. Eur J Orthod. 2013;35:131–137. doi: 10.1093/ejo/cjr110. [DOI] [PubMed] [Google Scholar]
- 13.Grabowski R, Kundt G, Stahl F. Interrelation between occlusal findings and orofacial myofunctional status in primary and mixed dentition. J Orofac Orthop. 2007;68:462–476. doi: 10.1007/s00056-007-0717-y. [DOI] [PubMed] [Google Scholar]
- 14.Khattab TZ, Farah H, Al-Sabbagh R, Hajeer M, Haj-Hamed Y. Speech performance and oral impairments with lingual and labial orthodontic appliances in the first stage of fixed treatment: a randomized controlled trial. Angle Orthod. 2013;83(3):519–526 doi: 10.2319/073112-619.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feldman EW. Speech articulation problems associated with placement of orthodontic appliances. J Speech Hear Disord. 1956;21:34–38. doi: 10.1044/jshd.2101.34. [DOI] [PubMed] [Google Scholar]
- 16.Leavy KM, Cisneros GJ, LeBlanc EM. Malocclusion and its relationship to speech sound production. Am J Orthod Dentofac Orthop. doi: 10.1016/j.ajodo.2015.12.015. In press. [DOI] [PubMed] [Google Scholar]
- 17.Subtelny JD, Mestre JC, Subtelny JD. Comparative study of normal and defective articulation of /s/ as related to malocclusion and deglutition. J Speech Hear Disord. 1964;29:269–285. doi: 10.1044/jshd.2903.269. [DOI] [PubMed] [Google Scholar]
- 18.Vallino LD, Tompson B. Perceptual characteristics of consonant errors associated with malocclusion. J Oral Maxillofac Surg. 1993;51:850–856. doi: 10.1016/s0278-2391(10)80101-6. [DOI] [PubMed] [Google Scholar]
- 19.Paley JS. The Effects of Orthodontic Appliances on Speech Sound Production. Bronx, New York: Montefiore Medical Center; 1999. [graduate thesis] [Google Scholar]
- 20.Ludlow C, Hoit J, Kent R, Ramig L, Sharivastav R, Strand E, Yorkston K, Sapienza C. Translating principles of neural plasticity into research on speech motor control recovery and rehabilitation. J Speech Lang Hear Res. 2008;51:S240–S258. doi: 10.1044/1092-4388(2008/019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zatorre RJ, Belin P, Penhune VB. Structure and function of auditory cortex: music and speech. Trends Cogn Sci. 2002;6(1):37–46. doi: 10.1016/s1364-6613(00)01816-7. [DOI] [PubMed] [Google Scholar]
- 22.Blomgren M, Nagarajan SS. Brain activation patterns in stuttering and nonstuttering speakers: preliminary results and future directions. Sig 1 Perspect Fluency Fluency Disord. 2004;14:13–16. doi: 10.1016/j.jfludis.2003.08.002. [DOI] [PubMed] [Google Scholar]