Abstract
Schwannoma is a tumor of soft tissue originating from Schwann cells which rarely appears in the retroperitoneum region. The retroperitoneal schwannoma can grow to a large size slowly without any specific clinical sign or symptoms. We report a 35-year-old woman with ancient schwannoma complaining abdominal pain for three years, which was initially judged as urinary tract infection. Following imaging studies, retroperitoneal mass was found and judged as benign lesion. Partial excision of the tumor was performed, with histology examination showed degenerative changes that was consistent with ancient schwannoma. No evidence of recurrence appeared during follow-up period.
Keywords: Retroperitoneal tumor, Ancient schwannoma, Total excision, Abdominal lesion
1. Introduction
Retroperitoneal tumors represent a combination of sarcomas and other benign and malignant lesions, with sarcomas are the most prevalent entity (roughly 1%–15% of all adults and pediatric neoplasms). Benign retroperitoneal tumors are much less common than retroperitoneal sarcomas, ∼40% of all retroperitoneal tumors are benign, with most cases are found incidentally. The most common benign pathologies encountered in the retroperitoneum include benign neurogenic tumors (schwannomas, neurofibromas), fibromatosis, and renal angiomyolipomas.1
Schwannoma is a tumor of soft tissue originating from Schwann cells of the peripheral nerve sheath. Therefore, it can appear in any Schwann cell of the nervous system, including trunks and extremities, but rarely occurs in the retroperitoneum region (only 0.5%–5% of all schwannomas).2 We report a case of a retroperitoneal mass in 35-year-old female, which was later identified as an ancient Schwannoma.
2. Case presentation
A 35-year-old female patient was referred to the urology clinic for evaluation of the left retroperitoneal mass that had been previously identified by abdominal ultrasonography examination. The chief complaint was recurring pain in the middle to lower left abdomen for the past three years. In the beginning, there was pain and bleeding during urination. The patient was previously diagnosed with urinary tract infection. However, after series of treatment, there was no sign of improvement and the abdominal pain got worsened.
On physical examination, no tenderness or mass was found in palpation. All laboratory examinations, including blood exam, kidney function and urinalysis, were within normal limit.
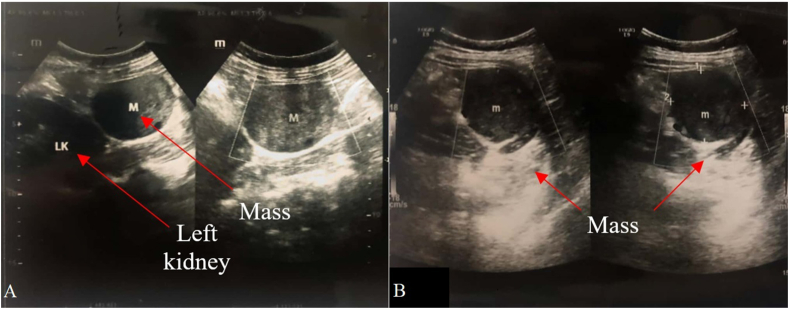
On abdominal ultrasound examination, isoechoic lesion in the lower pole of the left kidney (Fig. 1a) which was measured to be 4.7 × 4.9 cm and intralesional vascularization (Fig. 1b) were found.
Fig. 1.
(a) Well-bordered isoechoic lesions on the lower pole of the left kidney, and (b) lesion measuring 4.7 × 4.9 cm.
On abdominal CT-scan with contrast, a clear and well-bordered and relatively homogeneous isodense lesion was found in the retroperitoneal area, with the size of 4.8 x 5.5 × 5 cm. The tumor was found in the lower left abdomen, anterior to the walls of the left abdomen, posterior to the posterior portion of descending colon. Superiorly, the tumor was contiguous with inferior portion of the kidneys at L2-L3 intervertebral foramina. Inferior part of tumor is at L4-L5 intervertebral foramina. Post contrast scanning showed minimal enhancement. The Hounsfield Unit (HU) pre-contrast phase and post-contrast phase was 9 and 10, respectively. The mass was judged benign by this evaluation.
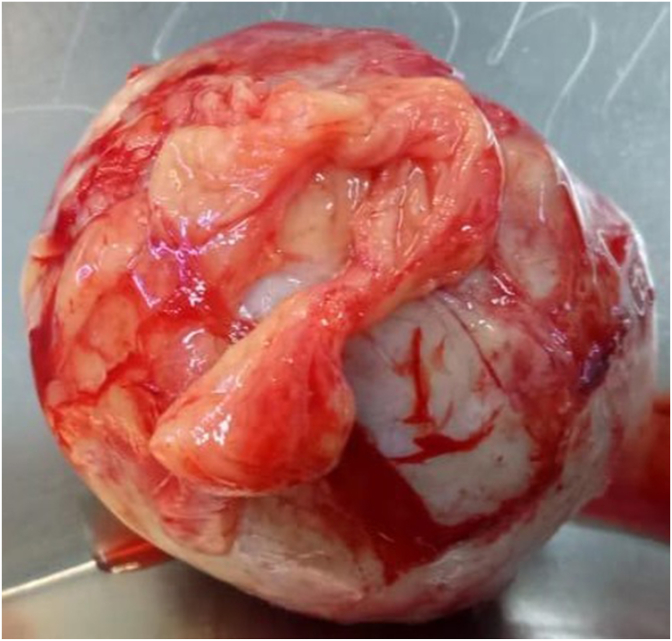
The patient subsequently underwent exploration laparotomy with midline abdominal incision. During the procedure, a mass was found on the retroperitoneal area of the left lower abdomen with size 6 x 5 x 4,5 cm. The encapsulated mass was separated from the surrounding tissue, then excised from the retroperitoneum (Fig. 2).
Fig. 2.
The retroperitoneal mass measuring 6 x 5 × 4.5 cm.
The peritoneal mass histopathological examination showed a partially encapsulated and firmly demarcated tumor mass. Hypercellular and hypocellular areas could be seen. The tumor mass was arranged in a bell-like and whirling pattern, with spindled, oval, wavy, mildly pleomorphic, hyperchromatic nucleuses with eosinophilic cytoplasm. Nuclear palisading appearance was also found, with microcytic areas. Many hyalinized blood vessels with myxoid background could be found. Those findings were consistent with an ancient schwannoma (Fig. 3).
Fig. 3.
Hypocellular (left) and hypercellular (right) area. Spindled, oval, wavy, mildly pleomorphic, hyperchromatic nucleuses of the tumor cells. Some showed myxoid backgrounds accompanied with many hyalinated blood vessels, hemorrhage could be seen.
Six months post-procedure, the patient was in good condition. There was no sign of recurrence. Ultrasound examination also revealed no evidence of mass or lesion.
3. Discussion
Retroperitoneal schwannoma is a solid, encapsulated benign tumor that arises from the paravertebral region. Macroscopically, schwannoma is solitary, well-bordered mass, with a soft surface. Histologically, schwannoma consisted of Schwann cells with hypercellular and hypocellular regions known as Antoni A and Antoni B with positive diffusion of S100 protein. The presence of degenerative changes, such as cyst formation, hemorrhages, calcification, and hyalinization, is a sign of subtype of retroperitoneal schwannoma, namely ancient retroperitoneal schwannoma.2
Due to flexibility of retroperitoneal space, the retroperitoneal schwannoma can grow to a large size slowly without invading adjacent structures. Therefore, in the early stages of development, the retroperitoneal schwannoma is often undetected clinically until suppressing the surrounding organs.2 The chief complaints of retroperitoneal schwannoma was not only abdominal pain, but also non-specific gastrointestinal disorders, such as abdominal pain during defecation and other symptoms, such as hematuria and recurrent renal colic.3 In our case, the manifesting symptom was recurrent pain in the middle to lower left abdomen, with initial symptoms of pain in the left abdomen and hematuria.
Imaging modalities for detecting retroperitoneal schwannoma consist of abdominal ultrasound (US), CT-scan, and MRI.2 Homogeny, regular shaped, and poorly vascularized image can be seen in ultrasound, while another study showed a necrotic heterogeneous central cystic area. In CT-scan, cystic mass with central necrotic could be observed.4,5 In our case, abdominal ultrasound showed isoechoic lesion in the lower pole of the left kidney with intralesional vascularization, while the results of CT-scan showed characteristic features of benign schwannoma, such as homogeneous isodense lesions, solitary mass, and minimal enhancement. To confirm the diagnosis, biopsy and CT-scan-guided fine-needle aspiration biopsy could be performed. However, these procedures aren't recommended preoperatively due to increased risk of bleeding, infection, and spreading of tumor.2
Total excision (including adjacent tissue if needed) is the best therapy for retroperitoneal schwannoma.2, 3, 4, 5 However, other literature showed that simple enucleation or partial excision was sufficient due to rare malignant transformation of retroperitoneal schwannoma.2,5 At our first experience, we performed simple enucleation or partial excision of schwannoma without excision adjacent tissue because imaging studies showed features of the benign retroperitoneal tumor.
Retroperitoneal schwannoma usually has good prognosis with recurrency found in 5–10% of cases, possibly due to incomplete excision.3 Imaging test with CT-scan or MRI, was usually needed 6–12 months post-procedure.3, 4, 5 In our first case experience, we performed partial excision. No evidence of recurrence appeared after 6 months of follow-up. However, further study is still needed to evaluate our practice.
4. Conclusion
Ancient schwannoma is rare subtype of retroperitoneal schwannoma, that is often clinically undetected or misjudged for other diseases. Imaging studies, followed with post-operative histopathological examination can be used to confirm the diagnosis. However, controversy still does exist over the necessity of negative tissue margin during operative treatment.
Declaration of competing interest
There is no conflict of interest in this paperwork.
Acknowledgments
N/A.
Contributor Information
Raga Manduaru, Email: manduaru@gmail.com.
Hendy Mirza, Email: hendy2807@yahoo.com.
References
- 1.Spiess P.E., Leibovici D., Pisters L.L. In: Wein A.J., Kavoussi L.R., Partin A.W., Peters C.A., editors. Elsevier; Philadelphia: 2016. Retroperitoneal Tumors; pp. 1403–1404. (Campbell-walsh Urology eleventh ed.). [Google Scholar]
- 2.Goh B.K., Tan Y.M., Chung Y.F., et al. Retroperitoneum schwannoma. Am J Surg. 2006;192:14–18. doi: 10.1016/j.amjsurg.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 3.Song J.Y., Kim S.Y., Park E.G., et al. Schwannoma in the retroperitoneum. J Obstet Gynaecol Res. 2007;33:371–375. doi: 10.1111/j.1447-0756.2007.00539.x. [DOI] [PubMed] [Google Scholar]
- 4.Meşină C., Mogoantă S.Ş., Cristian D.A., et al. Retroperitoneal ancient schwannoma - case presentation. Rom J Morphol Embryol. 2015;56(4):1517–1522. [PubMed] [Google Scholar]
- 5.Çalişkan S., Gümrükçü G., Kaya C. Retroperitoneal ancient schwannoma: a case report. Rev Urol. 2015;17(3):190–193. [PMC free article] [PubMed] [Google Scholar]