Introduction
The pacemaker device stimulation threshold by definition is the minimal amount of electrical energy required to induce consistent capture outside the refractory period of the heart. The difference between the threshold and the programmed device output reflects the reserve or pacing safety factor.1 It is affected by a multitude of factors, including physiologic variants, use of certain pharmacologic agents, and pathologies such as hypoxia, hypothermia, poorly controlled diabetes, and myocardial ischemia.2,3 This novel case presents an illustration of acute threshold changes directly correlating with disease progression in a case of recently diagnosed multiple myeloma (MM) in a patient with a previously implanted pacemaker leading to progressively higher pacemaker device thresholds, with subsequent improvement of the device thresholds after initiation of systemic therapy for the MM. To the best of our knowledge, this appears to be the first reported case exhibiting a clear correlation of light chain levels correlating with dynamic and reversible pacemaker device threshold changes.
Case report
A 59-year-old woman presented to the emergency department (ER) for evaluation of dizziness in the setting of increasing pacemaker device thresholds over the past 5 months. She has an extensive cardiac history that consists of sick sinus syndrome with sinus asystole requiring pacemaker implantation 5 years ago, atrial fibrillation/flutter status post maze procedure and multiple ablations, and aortic and mitral valvular disease owing to rheumatic fever, requiring valve replacement.
Upon device implantation 5 years prior, interrogation of the Medtronic Advisa dual-chamber pacemaker demonstrated stable right atrial (RA) lead parameters with a threshold of 0.75 V at 0.4 ms and stable right ventricular (RV) lead parameters with a threshold of 1.375 V at 0.4 ms, which remained stable until 5 months ago. The device was programmed at baseline to Managed Ventricular Pacing with Rate Response (MVPR) with a lower heart rate of 60 beats per minute and an upper heart rate of 130 beats per minute. Atrial pacing occurred 97.3% of the time with atrial asystole when the device was turned off. The programmed device outputs were 2.5 V at 0.4 ms in the RA lead and 2.75 V at 0.40 ms in the RV lead.
Four weeks prior to her ER presentation, she was being evaluated for macrocytic anemia and hemolysis. The patient had a bone marrow biopsy as part of the initial work-up and was diagnosed with standard-risk MM based on a bone marrow biopsy showing about 70% CD138-positive plasma cells by immunohistochemistry. Serum protein electrophoresis and immunofixation showed an elevated monoclonal protein with a Lambda light chain subtype and an abnormal free light chain ratio showing an elevated lambda serum level of 2531 mg/L (reference range 5.7–26.3 mg/L). Her oncologic plan included induction systemic therapy with bortezomib, lenalidomide, and dexamethasone. The patient was also referred to a tertiary care center for an autologous bone marrow transplantation evaluation. Unfortunately, chemotherapy initiation was delayed owing to the COVID-19 pandemic.
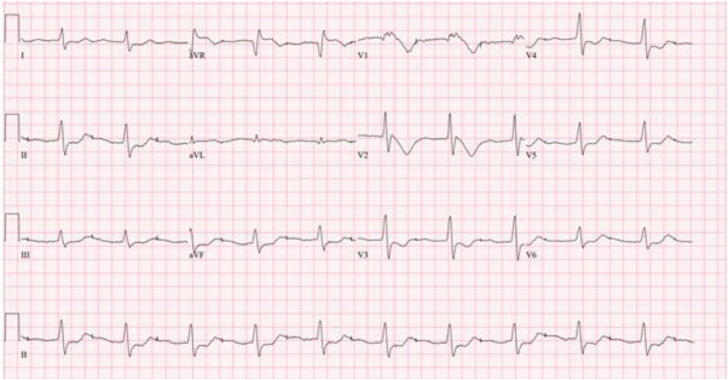
The patient presented to the hospital ER with a 2-week history of dizziness. An electrocardiogram (ECG) was performed showing atrial capture with a prolonged PR interval (Figure 1). Laboratory evaluation revealed a brain natriuretic peptide of 97 and troponin I of <0.03. A chest radiograph was obtained and showed no acute abnormality, stable mild cardiomegaly, aortic and mitral valvuloplasty, and left chest wall dual lead pacemaker (Supplemental Figure S1). Device interrogation confirmed atrial capture with prolonged AV conduction delay resulting in a significant first-degree AV block and ventricular noncapture (Figure 2). Further interrogation revealed RA lead threshold of 2.25 V at 0.4 ms and RV lead threshold of >5 volts at 0.4 ms, which was above the chronic programmed output for the RV lead. As both leads had shown a parallel increase in thresholds over time with minimal change in impedance, it was felt that this was likely owing to MM causing amyloid light-chain cardiac amyloidosis resulting in lead threshold increases. In this setting, it was felt that a lead revision would not be successful and the best course of action would be to initiate chemotherapy as soon as possible. The device was reprogrammed to maximum output of 6 V / 1.5 ms in both the RA and RV leads in order to maintain capture while chemotherapy was initiated.
Figure 1.
Twelve-lead electrocardiogram obtained in emergency department after the patient presented with a 2-week history of dizziness, showing atrial capture with prolonged PR interval.
Figure 2.
Device interrogation obtained while in emergency department showing atrial capture with prolonged AV conduction delay resulting in first-degree AV block with intermittent ventricular noncapture.
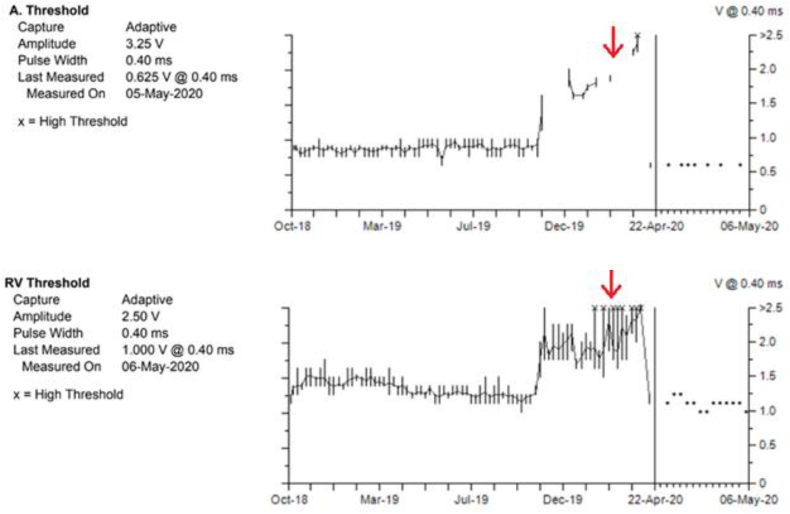
Review of lead trends on device interrogation demonstrated a slow increase in lead thresholds starting approximately 5 months prior to the patient’s presentation in the ER (Figure 3). Her ECG at that time showed an atrial-paced rhythm with prolonged AV conduction; however, when compared to her ECG in the ER the PR interval duration was of shorter duration and there was no widening of the QRS complex (Supplemental Figure S2). An echocardiogram was performed and showed a left ventricular ejection fraction of 72% with a thickened interventricular septum and speckling suggestive of amyloidosis. Other echo findings included atypical septal and apical motion, normal-functioning mechanical aortic valve, normal-functioning mechanical mitral valve, severe tricuspid regurgitation, and severe pulmonary hypertension with pulmonary artery pressure estimated at 65 mm Hg.
Figure 3.
Device threshold trends of right atrial lead (Top) and right ventricular lead (Bottom) over the past 19 months. Red arrow indicates approximate timing of official multiple myeloma diagnosis based on bone marrow biopsy.
After the initiation of chemotherapy, the patient’s light chain levels decreased from 2531 mg/L to 1506 mg/L within 1 week and subsequently to 480 mg/L 2 weeks later. Correspondingly, a repeat pacemaker device interrogation demonstrated a dramatic fall in the lead thresholds. Her RA threshold reduced to 0.625 V at 0.4 ms and the RV threshold was 1.0 V at 0.4 ms. Her device output was 3.25 V / 0.40 ms in the RA lead and 2.50 V / 0.40 ms in the RV lead. A corresponding trend was noted in her lead sensing as well. About 12 months prior to her diagnosis, the measured P/R wave for her RA and RV were 2.0 mV and 8.9 mV, respectively. At the time of initiation of her chemotherapy, the measured P/R wave decreased to 1.3 mV and 6.8 mV for RA and RV, respectively. About 1 month after her chemotherapy, the measured P/R wave was back at 2.1 mV and 7.8 mV for RA and RV. Four weeks after the initiation of chemotherapy, she had an excisional abdominal fat pad biopsy with Congo red staining, which was negative for amyloidosis. A 12-lead ECG was obtained 3 months after starting chemotherapy showing normal sinus rhythm with normalization of the PR interval. The QRS interval is unchanged (Supplemental Figure S3).
Discussion
Pacing thresholds are the minimum energy required to consistently elicit a myocardial depolarization. Higher thresholds may lead to a decreased or complete cessation of both atrial and ventricular capture in addition to a higher pacing output, causing a shortening of the pacemaker battery life. Lead thresholds can be affected by a variety of factors, including myocardial infarction, hypo/hyperglycemia, hyperkalemia, severe hypoxia, severe acidosis or alkalosis, or antiarrhythmic drugs such as flecainide, propafenone, and sotalol.2 Also, a primary myocardial process causing increased fibrosis or scarring at the lead–tissue interface may cause an increase in pacing threshold.4,5
Amyloidosis is a group of diseases that are characterized by a pathologic deposition of misfolded proteins (in a beta sheet–type structure) in the extracellular space. Currently, there are about 25 different proteins known to cause amyloidosis.6 Immunoglobulin light chain (AL) amyloidosis forms the amyloid protein from fibrils that are composed of fragments of monoclonal light chains (kappa or lambda). The amyloid protein is an amorphous, fibrillar, and proteinaceous material that can then deposit in many organs including the heart. AL amyloidosis can occur independently or, more rarely, in parallel to MM. MM is present in 10%–15% of patients with AL amyloidosis at the time of diagnosis.7 In cardiac amyloidosis, the amyloid deposition causes stiffening of the heart walls without producing a compensatory dilation, which results in a biventricular restrictive pathophysiology that can ultimately lead to heart failure. Atrial amyloid infiltration is nearly always present and commonly causes dysfunctional atrial contraction.8 The amyloid deposition additionally occurs on valves and perivascularly. If untreated, the median survival from onset of heart failure is generally about 6 months, but current therapeutics can put the disease into an extended remission and prolong life by several years. Treatment of AL cardiac amyloidosis consists of optimal therapy for heart failure and systemic therapy directed at eliminating the amyloidogenic plasma cell dyscrasia.8,9
In addition to pump failure, conduction abnormalities are a major cause of morbidity and mortality in cardiac amyloidosis. Although AL amyloidosis is typically more often associated with ventricular arrhythmias and the transthyretin form is more often associated with bradyarrhythmias, both can occur in either form.10 The mechanism of arrhythmias in both transthyretin and AL cardiac amyloidosis is not fully elucidated and likely multifactorial. Oxidative stress–induced cellular damage from deposition of AL light chain, separation of myocytes by amyloid fibrils, and coronary amyloidosis, especially in AL disease, are all potential etiologies of conduction abnormalities.10 The use of implantable cardioverter-defibrillator for management of ventricular arrhythmias is not clear, as studies evaluating the placement of implantable cardioverter-defibrillators, especially in AL amyloidosis, have shown some survival benefit,11 while others have not.12 Symptomatic bradyarrhythmias are common in cardiac amyloidosis. Loss of all atrial activity and AV blocks may be due to amyloid, with AV blocks linked to death in these patients. Despite these findings, cardiac pacing has not been shown to change the overall prognosis, although data are quite limited.13 Cardiac pacing is beneficial for symptomatic relief and is indicated for patients with symptomatic bradyarrhythmias.
Returning to our case, although the patient’s pacemaker was placed well before her diagnosis of MM, it was not until around the time of her MM diagnosis that her device thresholds increased. To our knowledge, there have been no reported cases of MM resulting in changes in pacemaker threshold in the absence of cardiac amyloidosis. The increase in device thresholds corresponded to a rise in her light chain levels, which is suggestive of possible early AL cardiac amyloidosis despite a negative abdominal fat pad biopsy. The sensitivity of abdominal fat pad biopsies has been reported to range from 60% to 80%.14 Furthermore, reduction of the serum light chain levels, in response to therapy, could possibly explain the negative biopsy result as well. A rise in device thresholds in suspected cardiac amyloidosis with subsequent improvement after MM therapy makes sense pathophysiologically, although this appears to be the first reported case showing a clear correlation between changes in device thresholds and light chain levels with subsequent improvement after initiation of systemic therapy.
Conclusion
In this novel case, the progressive increase in both RA and RV lead thresholds in the setting of newly diagnosed MM with concomitant rise in light chain levels was highly suggestive of AL cardiac amyloidosis. The correlation between the rise and subsequent fall in both light chain levels and device thresholds after systemic therapy offers further evidence of AL cardiac amyloidosis as the likely etiology of increasing device thresholds and may have led to loss of device capture.
Footnotes
Conflict of interest: The authors declare no conflict of interest. Disclosures: Drs Martinez, Khiatah, Jazayeri, and Oregel have nothing to disclose. Dr Dukes reports consulting for Medtronic and Biotronik, and receives research funding from Boston Scientific and Biotronik. Funding: No funds were received.
Key Teaching Points.
-
•Amyloid light-chain amyloidosis is a potential cause of increased device thresholds, which may lead to capturing failure and severe morbidity.
-
•Prompt initiation of systemic therapy for the treatment of multiple myeloma in patients who are pacer dependent may decrease the risk of capture failure due to increased device thresholds and prolong device battery.
-
•Cardiac amyloidosis can cause both heart failure and dysrhythmias. Early diagnosis and appropriate treatment are critical to improve outcomes.
Appendix. Supplementary data
References
- 1.Mulpuru S.K., Madhavan M., McLeod C.J., Cha Y.M., Friedman P.A. Cardiac pacemakers: function, troubleshooting, and management: part 1 of a 2-part series. J Am Coll Cardiol. 2017;69:189–210. doi: 10.1016/j.jacc.2016.10.061. [DOI] [PubMed] [Google Scholar]
- 2.Dohrmmann M.L., Goldschlager N.F. Myocardial stimulation threshold in patients with cardiac pacemakers: effects of physiologic variables, pharmacologic agents, and lead electrodes. Cardiol Clin. 1985;3:527–537. [PubMed] [Google Scholar]
- 3.Peng H., Sun Z., Zhang H., Ma W. Long-term performance of right ventricular pacing lead: risk factors associated with permanent right ventricular pacing threshold increase. J Interv Card Electrophysiol. 2019;55:349–357. doi: 10.1007/s10840-018-0481-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maisel W.H., Hauser R.G., Hammill S.C., et al. Recommendations from the Heart Rhythm Society Task Force on Lead Performance Policies and Guidelines: developed in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA) Heart Rhythm. 2009;6:869–885. doi: 10.1016/j.hrthm.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Levine P.A. Management of the patient with an acute massive rise in the capture threshold. Indian Pacing Electrophysiol J. 2001;1:35–37. [PMC free article] [PubMed] [Google Scholar]
- 6.Oregel K.Z., Shouse G.P., Oster C., et al. Atypical amyloidosis from a novel gelsolin gene mutation. Am J Case Rep. 2018;19:374–381. doi: 10.12659/AJCR.907550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dubrey S.W., Hawkins P.N., Falk R.H. Amyloid diseases of the heart: assessment, diagnosis, and referral. Heart. 2011;97:75–84. doi: 10.1136/hrt.2009.190405. [DOI] [PubMed] [Google Scholar]
- 8.Falk R.H., Alexander K.M., Liao R., Dorbala S. AL (light-chain) cardiac amyloidosis. J Am Coll Cardiol. 2016;68:1323–1341. doi: 10.1016/j.jacc.2016.06.053. [DOI] [PubMed] [Google Scholar]
- 9.Siddiqi O.K., Ruberg F.L. Cardiac amyloidosis: an update on pathophysiology, diagnosis, and treatment. Trends Cardiovasc Med. 2018;28:10–21. doi: 10.1016/j.tcm.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.John R.M., Stern D.L. Use of implantable electronic devices in patients with cardiac amyloidosis. Can J Cardiol. 2020;36:408–415. doi: 10.1016/j.cjca.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Lin G., Dispenzieri A., Kyle R., Grogan M., Brady P.A. Implantable cardioverter-defibrillators in patients with cardiac amyloidosis. J Cardiovasc Electrophysiol. 2013;24:793–798. doi: 10.1111/jce.12123. [DOI] [PubMed] [Google Scholar]
- 12.Varr B.C., Zarafshar S., Coakley T., et al. Implantable cardioverter-defibrillator placement in patients with cardiac amyloidosis. Heart Rhythm. 2014;11:158–162. doi: 10.1016/j.hrthm.2013.10.026. [DOI] [PubMed] [Google Scholar]
- 13.Webster T., Lin G., Jurrens T., et al. Impact of permanent pacing in patients with cardiac amyloidosis: a single center experience. J Card Fail. 2007;13:s128–s129. [Google Scholar]
- 14.Vaxman I., Gertz M. Recent advances in the diagnosis, risk stratification, and management of systemic light-chain amyloidosis. Acta Haematol. 2019;141:93–106. doi: 10.1159/000495455. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.