Abstract
The monthly dapivirine vaginal ring has proven efficacious in reducing HIV incidence in two Phase 3 clinical trials. When considering the potential future availability of the ring to the public, key questions remain about the feasibility of integrating the ring as an HIV prevention intervention into women’s lives. We conducted qualitative mapping interviews (n = 66) among women enrolled in MTN-025/HOPE, an open-label trial conducted in Malawi, South Africa, Uganda and Zimbabwe, to examine how home environments influenced use of the dapivirine vaginal ring. Most women had secure places to store their rings including wardrobes, suitcases, and bags. The primary concerns for ring storage were potential tampering from children or rodents. Household overcrowding limited the privacy some women had which made removal and insertion of vaginal rings challenging. Despite these challenges, ring storage, insertion, and removal was feasible across social and living contexts.
Keywords: Vaginal ring, HIV prevention, Women, Home environment, Qualitative
Introduction
Women in Sub-Saharan Africa (SSA) are disproportionately affected by HIV and account for 59% of new cases in the region (1). In the last decade, significant advances in HIV prevention research have resulted in the development and evaluation of new biomedical products, including the dapivirine vaginal ring, a monthly, discreet, and woman-initiated HIV prevention technology. Women have found vaginal rings for a range of indications to be highly acceptable (2). Two randomized controlled trials conducted in Sub-Saharan Africa demonstrated that the dapivirine vaginal ring is well tolerated and reduced HIV risk. In the MTN-020/ASPIRE trial, a phase 3 randomized, double-blind, placebo-controlled trial of the dapivirine vaginal ring, overall HIV incidence was 27% lower among women using the active product rings (3) and a post-hoc, non-randomized analysis estimated risk reduction as high as 75% among those with high levels of adherence (4). Similarly, in IPM 027/The Ring Study, active product vaginal ring use was associated with a 35% reduction in HIV incidence (5, 6). In subsequent open-label trials of the vaginal ring, modeling data estimated 39–63% reductions in HIV risk (7, 8). Recently, the European Medicines Agency adopted a positive scientific opinion for the ring’s use among women aged 18 and older in developing countries who cannot or choose not to use oral PrEP (9).
Household members such as intimate partners and other personal relationships have had a significant impact on the persistent use of HIV prevention products (10, 11). In the MTN-020/ASPIRE trial, women’s experiences with the vaginal ring were highly influenced by their relationships with sexual partners (11). Power imbalances in the relationship sometimes resulted in forcible removal of the ring, demands to discontinue study participation, and limited ability to negotiate safer sex or contraception use (10). Additionally, household members’ perceptions of product attributes also impacted use patterns. In several PrEP trials, women using oral PrEP reported experiencing PrEP-related stigma and often concealed their use of PrEP from members of their household (12, 13). Rattling noise of pill bottles (12) concerns about people finding PrEP containers (14) or mistaking PrEP for HIV treatment (12, 13, 15, 16), have been found to impact PrEP use.
Less is known about how features of the physical home environment influence use of HIV prevention tools. For oral PrEP or vaginal microbicides, special packages and containers have been developed for young women to help ensure increased privacy (17). However, vaginal rings present different challenges; they require a private space for insertion and removal, as well as a secure place to store unused rings and discard used rings. Additionally, some users have concerns about keeping rings hygienic to prevent the risk of vaginal odor or infection (18). Often, women with the highest risk of HIV in Sub-Saharan Africa live in low-resource communities characterized by crowded homes and limited access to clean, running water, which may present barriers to ring use (19). Developing strategies to make the vaginal ring feasible for at home use for women in SSA requires an in-depth understanding of the context in which rings are used at home. The purpose of this paper was to examine how the social and physical home environment impacted storage and use of the vaginal ring in the context on an open-label trial where participants were given the option to take three rings to store and change at home.
Methods
MTN‑025/HOPE Parent Study and Qualitative Component
The HOPE study, an open label extension to the ASPIRE trial, assessed the continued safety of and adherence to the dapivirine vaginal ring for the prevention of HIV-1 acquisition in former ASPIRE participants (ClinicalTrials.gov number NCT01617096 and NCT02858037) (7, 20). Briefly, 1456 women were enrolled at 14 sites in Malawi, South Africa, Uganda and Zimbabwe, and were followed for up to 12 months from July 2016 to October 2018. To be eligible for HOPE, women had to: (1) be HIV negative; (2) not pregnant or breastfeeding; and (3) agree to use contraception during the study. HOPE participants were given a choice to accept a dapivirine ring as part of their HIV prevention strategy or rely solely on other HIV prevention approaches that were offered to all participants as part of the study’s standard HIV prevention package (i.e. condoms, monogamy, partner circumcision, oral PrEP, partner testing and STI treatment, etc.). Participants could change their minds at any time during the trial. Participants were seen monthly for the first 3 months of HOPE and then quarterly thereafter (at months 6, 9, and 12). At each quarterly visit, participants who agreed to use the vaginal rings were given the option to take 3 rings at a time for monthly replacement at home. Those who chose to take 3 rings home were provided with a discreet small cloth purse to store the rings (Fig. 1), as well as plastic bags to separate used and unused rings hygienically. Used rings were returned to the clinic at participant visits for assessment of residual drug levels (21). Participants could change their mind about their preferred HIV prevention method(s), including ring use, at any time throughout HOPE follow-up.
Fig. 1.
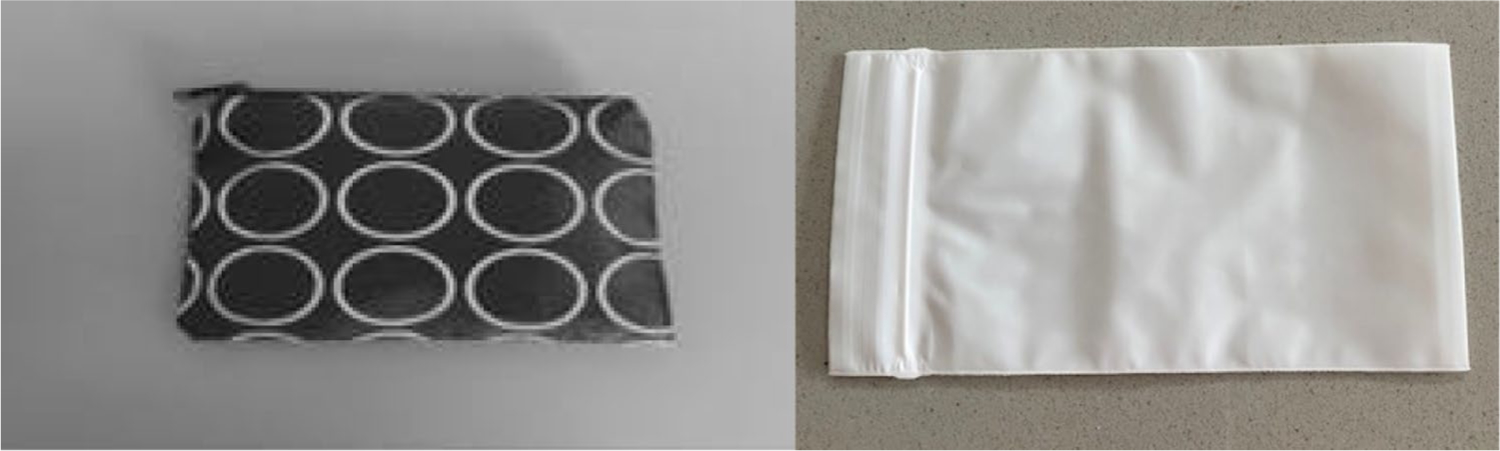
Ring storage purse and plastic bag. Ring storage purse (left) and plastic ring disposal bag (right)
A qualitative component was embedded in HOPE to explore the larger socio-behavioral and cultural context influencing women’s acceptability and use of the vaginal ring. Participants were recruited from six of the study sites across the four HOPE participating countries representing varying urban and peri-urban settings. Descriptions of qualitative study sites are included in Table 1.
Table 1.
Study sites
| City | Country | Description | Population density |
|---|---|---|---|
| Lilongwe | Malawi | Peri-urban | 1541 people per km2 |
| Kampala | Uganda | Urban | 8800 people per km2 |
| Chitungwiza | Zimbabwe | Urban, peri-urban | 7279 people per km2 |
| Cape Town | South Africa | Urban | 1530 people per km2 |
| Durban | Urban | 1502 people per km2 | |
| Johannesburg | Urban—inner city residential neighbourhood | 48 000 people per km2 |
Recruitment and Data Collection Procedures
A systematically selected sample of women who either accepted the ring (ring acceptors; n = 35) or did not (ring non-acceptors; n = 31) at enrollment were recruited for serial (2–3) qualitative interviews across the six study sites. Ring non-acceptors were oversampled in the qualitative component, as 73% of participants accepted the ring throughout the HOPE study period (7). Interviews took place around month 1, after receiving their first drug level feedback from counselors (at or after month 3), and around their Product Use End Visit (PUEV) (about one month prior to study exit). Interviews followed semi-structured guides administered by trained social scientists and lasted an average of 2 h. The present study focused on the PUEV interviews. Categories of ring acceptance or non-acceptance used for the PUEV interviews focused on whether participants had accepted the ring or not in the past three months prior to that interview. Thirty-four participants received non-acceptor interview guides and 32 received ring-acceptor interview guides. Ring acceptor PUEV interview guides broadly covered women’s experience using the ring and how it fit into their daily lives and home environments and ring non-acceptor PUEV guides focused on reasons for not using the vaginal ring and general experiences in the HOPE trial. During both ring acceptor and non-acceptor PUEV interviews, participants engaged in a home mapping activity. Participants were asked to draw and label a map of their homes, indicating actual and hypothetical ring storage areas. Ring acceptors were also asked to indicate where they removed and inserted their rings. Participants were given the option of drawing the maps on their own or being assisted by the interviewer. See Figs. 2, 3, 4 for examples.
Fig. 2.
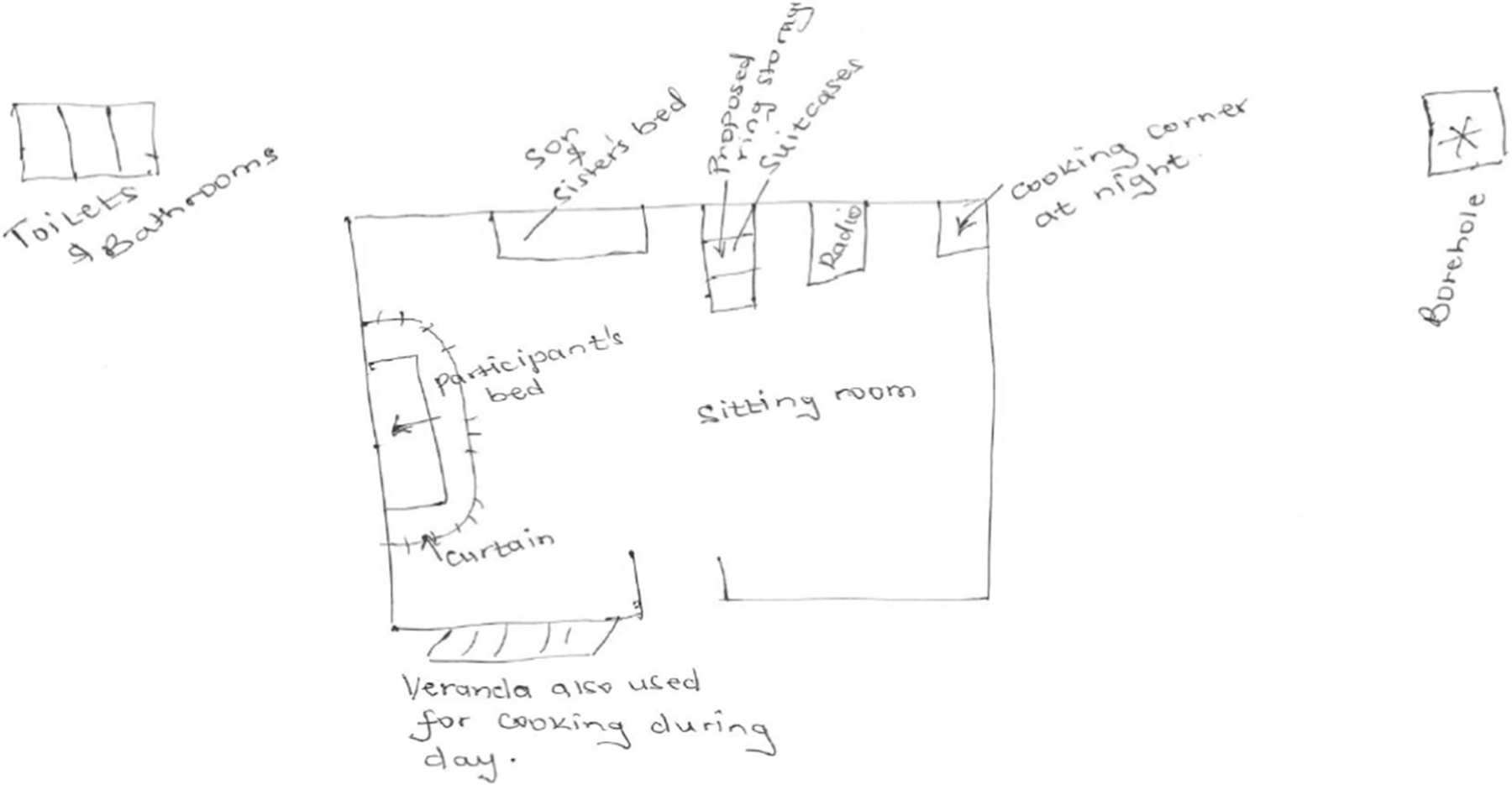
Ring Non-Acceptor, Kampala. Participant lives in a single room home that she shares share with her sister and nephew. A curtain separates her bed from the other part of the room where her sister and nephew sleep. Her proposed ring storage location is her suitcase
Fig. 3.
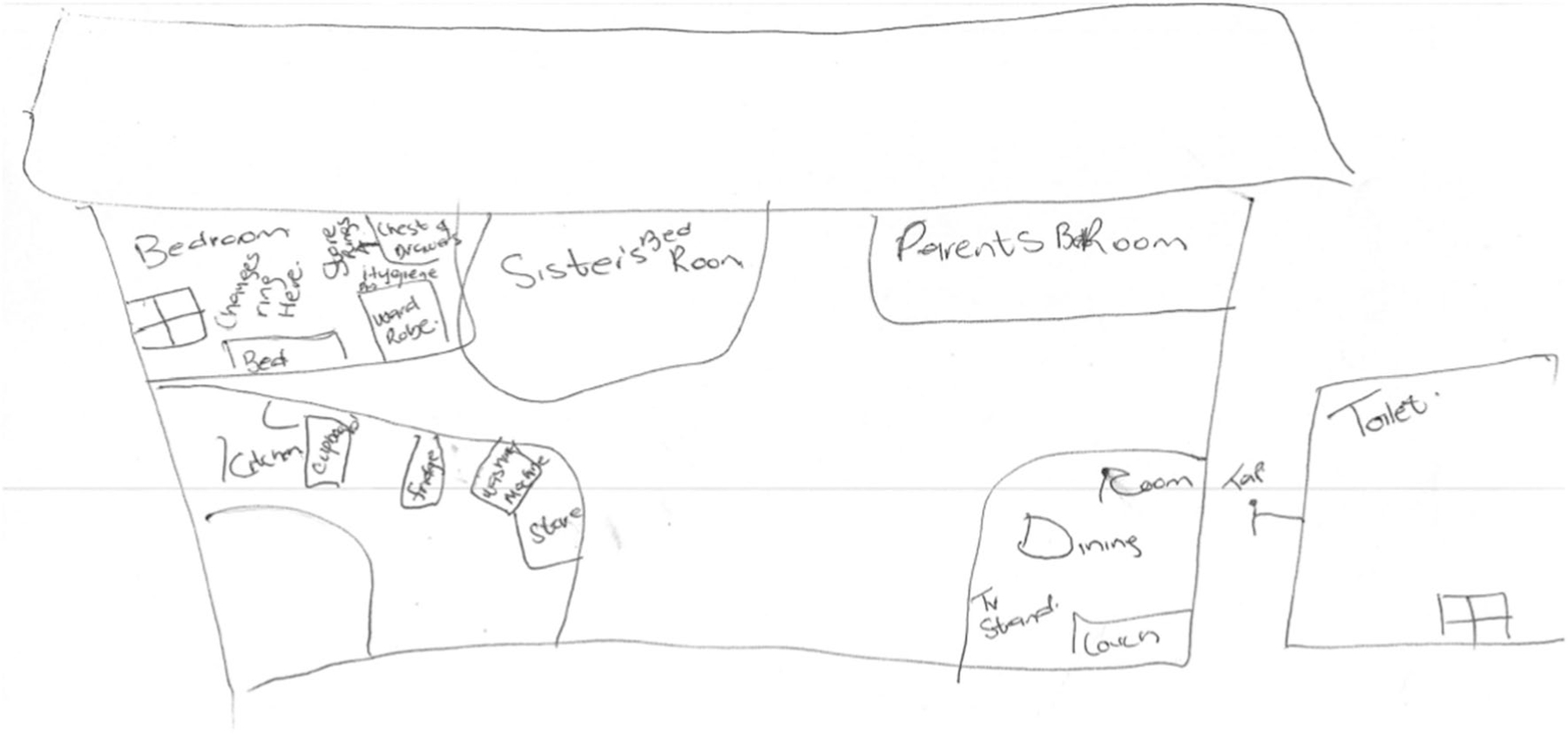
Ring Acceptor, Cape Town. Participant lives in a three-bedroom home with parents and sister. She has her own bedroom. She stores her ring in her chest of drawers and changes her ring in her bedroom
Fig. 4.
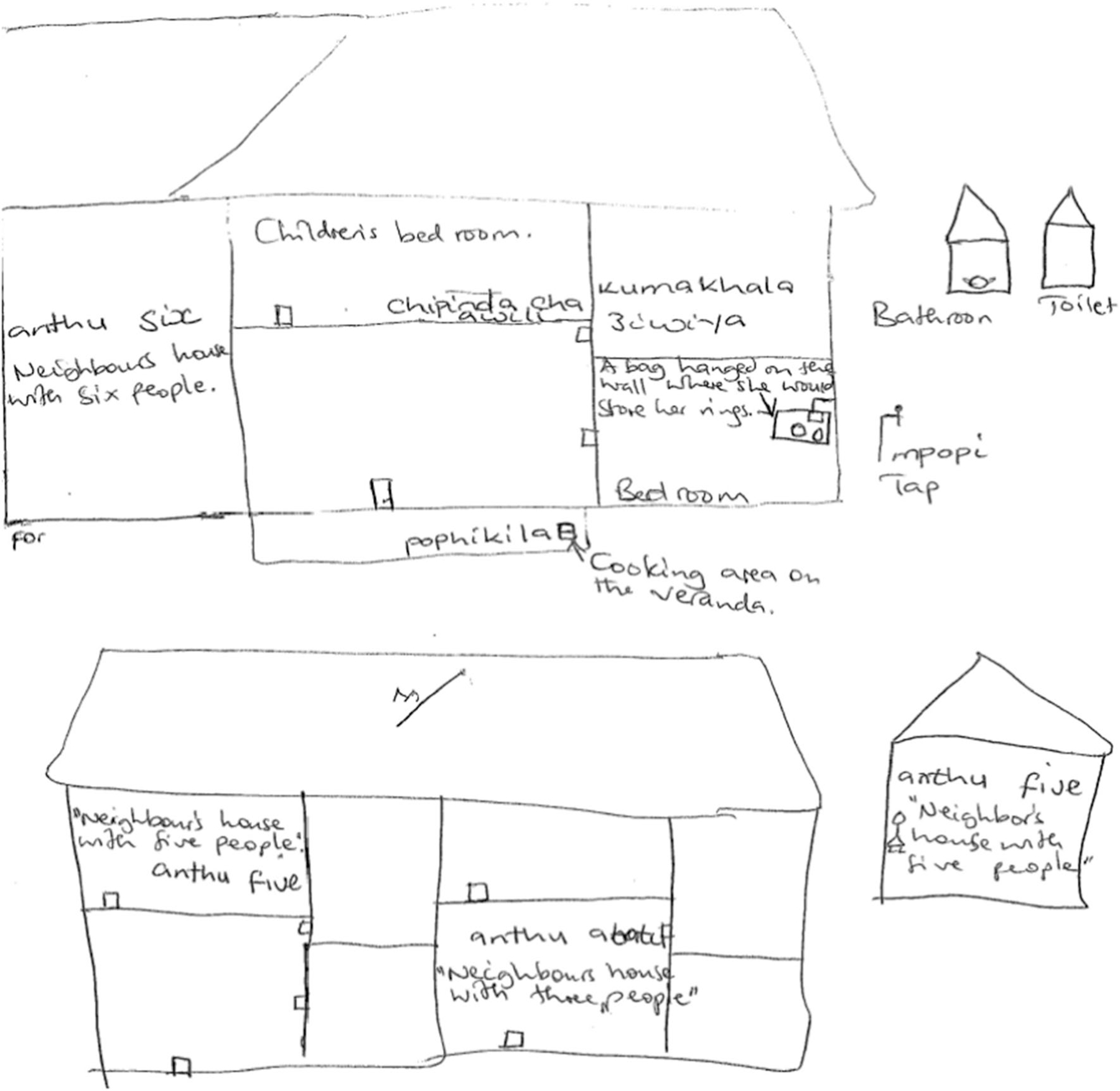
Ring Acceptor, Lilongwe. Participant lives with her husband and two children. She shares the room with her husband. Her home is in a compound that is shared with other families. She stores her rings in a bag hung on her wall in her bedroom
Data Management and Analysis
All participants who participated in serial IDIs were included in the analysis. We used descriptive statistics to summarize sociodemographic characteristics of the study participants at baseline for the entire sample and by site. Analyses were conducted using Stata version 16.1 (Stata-Corp, College Station, TX).
Interviews were audio-recorded, transcribed verbatim, and translated from local languages (Xhosa, Luganda, Zulu, Chichewa, and Shona) into English. The coding team consisted of five United States and South Africa-based analysts with backgrounds in anthropology, public health, and qualitative methods. Transcripts were coded using a codebook developed iteratively through a deductive and inductive process. Data were coded and analyzed using Dedoose Version 8.0.42 (Los Angeles, CA: SocioCultural Research Consultants, LLC). Intercoder reliability was confirmed using the Dedoose training center at an average mean kappa score of 0.68 for key codes among 10% of interviews. The coding team met weekly for five months to discuss emerging themes and issues, discuss code application queries and reach consensus on final coding. A thematic approach was used to guide analysis (22).
Home maps were analyzed systematically. A purposeful sample of 10 maps representing different sites were selected. These maps were assessed for similarities and differences to arrive at a set of key home characteristics to capture across maps. Researchers then met to discuss and refine the home characteristics. The final list of home characteristics (e.g., number of bedrooms, location of toilet and portable water, ring storage and changing place) were then captured for all maps (n = 65) and summarized in a table. Home characteristics were compared across sites and between ring acceptors and ring non-acceptors.
Data from transcripts and home maps were analyzed separately and then integrated to arrive at final interpretations. Coded data were summarized in tables to compare women’s decision-making regarding ring storage and ring change based on ring-acceptance status and study site. Analytic memos were written to describe the impact of home environments on ring storage and ring removal and insertion location.
Ethics
Written informed consent was obtained from all participants. The study was approved by the Institutional Review Boards at RTI International, and at each study site and regulated by the U.S. National Institutes of Health and the Microbicide Trials Network.
Results
Description of Sample
Demographic characteristics of the sample by study site are included in Table 2. The median age of the sample was 30.5 years (Interquartile range: 27–35). Half of participants were single and most had one or more children (86%). The majority had a secondary education or higher (82%). A third of participants reported experiencing food insecurity in the past month. There was some variation in socioeconomic status across sites. Ring non-acceptors were more likely to have electricity and a car/motorcycle. Additionally, non-acceptors had a longer travel time to clinic with 45% travelling an hour or more to get to a clinic compared to 28% of ring acceptors.
Table 2.
Demographic characteristics
| Past 3 Months Non-Acceptor | Past 3 Months Acceptor | Total | |||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| N | % | N | % | N | % | ||
| Age [N / median, (IQR)] | 34 | 29 (25–33) | 32 | 32 (28–36) | 66 | 30.5 (27–35) | |
| Marital status | |||||||
| Single | 18 | 53 | 15 | 47 | 33 | 50 | |
| Married / Living together | 16 | 47 | 17 | 53 | 33 | 50 | |
| Parity | |||||||
| No children | 6 | 18 | 3 | 9 | 9 | 14 | |
| 1–2 children | 20 | 59 | 16 | 50 | 36 | 55 | |
| 3 or more children | 8 | 24 | 13 | 41 | 21 | 32 | |
| Education level | |||||||
| Primary school/no schooling | 5 | 15 | 7 | 22 | 12 | 18 | |
| Secondary school (partial or complete) | 27 | 79 | 23 | 72 | 50 | 76 | |
| Attended college or university | 2 | 6 | 2 | 6 | 4 | 6 | |
| Food insecure | |||||||
| Never | 22 | 65 | 22 | 69 | 44 | 67 | |
| Rarely, sometimes, or often | 12 | 35 | 10 | 31 | 22 | 33 | |
| Assets | |||||||
| Electricity | 31 | 91 | 24 | 75 | 55 | 83 | |
| Radio/TV | 32 | 94 | 29 | 91 | 61 | 92 | |
| VCR/DVD player/Digital music player | 23 | 68 | 21 | 66 | 44 | 67 | |
| Mobile phone | 33 | 97 | 32 | 100 | 65 | 98 | |
| Table/Sofa | 31 | 91 | 29 | 91 | 60 | 91 | |
| Bicycle | 5 | 15 | 5 | 16 | 10 | 15 | |
| Car/motorcycle | 10 | 29 | 6 | 19 | 16 | 24 | |
| Travel time to clinic | |||||||
| Less than 30 min | 11 | 32 | 8 | 25 | 19 | 29 | |
| 30–60 min | 8 | 24 | 15 | 47 | 23 | 35 | |
| 1–2 h | 14 | 41 | 6 | 19 | 20 | 30 | |
| Greater than 2 h | 1 | 3 | 3 | 9 | 4 | 6 | |
Among the non-acceptors at baseline (n = 31), primary reasons for ring non-acceptance included preference for an alternative HIV prevention method, lack of interest in the ring, and being undecided or not ready to use the ring.
Home Environments
Participants drew and described a variety of home environments. Forty-one percent of participants (n = 27) shared their bedroom and/or bed with family members including children, siblings, mothers, grandmothers, and aunts. About 38% did not share a room or bed and 21% reported sharing a room with primary partners, husbands, or sexual partners.
Location of household toilets and access to running water were used as markers of housing condition. Half of participants (n = 33) had homes with an outdoor toilet. There were some regional differences, with outdoor toilets being more common in Kampala and Lilongwe. Most participants (n = 50) had access to a potable water source near or inside their homes.
Ring Storage
Overall, ring acceptors and non-acceptors reported that they had a place in their homes where they would feel comfortable storing their rings. Personal wardrobes, bags, and suitcases were the preferred actual and hypothetical ring storage locations for both ring acceptors and non-acceptors. Notably, ring non-acceptors were more likely to report suitcases and bags as the places they would hypothetically store their rings (see Figs. 2–4 for ring storage locations). Wardrobes, bags, and suitcases were the chosen locations because these were the place women kept clothing, menstruation and hygiene products, or other important items (e.g., wallets, identification cards). Ring acceptors and non-acceptor’s decisions on where to store rings were similarly motivated by desire to find a place that was confidential and safe from children and rodents and afforded them a sense of privacy.
Children
Finding a place where rings were safe from tampering by children was a primary priority for participants. A large proportion of women lived with children. For some, the presence of young children in the household impacted where and how they stored their rings. A woman who had not accepted the ring in the past three months, discussed where she would hypothetically store her ring:
My child likes to look around, yes. So I would [if I had a ring] place it in the first drawer because it’s higher for him/her.—Cape Town, Ring Non-Acceptor, 28 years old
Women were specifically concerned that children would get hold of rings and play with them or make them dirty, which could potentially make them unusable. Selecting a location where young children could not see or find the rings was important. One woman justified why she decided to store her rings in her wardrobe:
I wanted them to be out of reach of children. You know children; if they can see them, they may be curious to know “What is this…” They may take them outside and start to play with them. They can even wear them as bangles.—Lilongwe, Ring Acceptor, 28 years old.
Another participant noted:
I was scared of them (children) interfering and opening it (the ring package) before I am touching it and according to what I have learned you are not allowed to just touch the ring without washing your hands.— Durban, Ring Acceptor, 40 years old.
However, only a few women reported incidents where children in their homes took their rings. One woman described such an incident where her child took the study issued bag for ring storage:
When I had started MTN [HOPE], the elder child was at [primary school] …I had gone to Emavundleni [study clinic] with my bag and then I forgot my bag on the bed. I don’t know what she was looking for by then she saw the small bag that holds the rings. Then she took the rings inside that bag and threw them down inside my bag and then she took that bag and she put her pens in there.- Cape Town, Ring Acceptor, 31 years old.
The concern about children potentially playing with rings did influence storage. A small proportion of women decided to return to the clinic monthly to change their rings rather than obtain three rings to take home:
He/she [the child] was taking out these things, but I had placed them in their plastic bags. That is when I went to the clinic … I told them there at Emavundleni [study clinic] that I have a child there at home, so how about I come and insert them [the rings] here on that set date and then they said that is not a problem. Cape Town, Ring Acceptor, 36 years old.
For most other women, the concern about children obtaining rings led them to take precautions such as locking their wardrobes or hiding their rings under clothing or other items.
That’s my personal drawer that stays locked. And in my drawer I got like handbags, so in one of those handbags I got my rings.- Durban, Ring Acceptor, 40 years old
In contrast, some women who reported living with young children reported that they were not concerned because of the boundaries they had established with their children not to get into their things. A ring non-acceptor described how she would not be concerned about keeping rings at home if she were to have them because of the rules she had set:
Because of the way I trained them. They cannot touch something that you did not tell them to. -Lilongwe, Ring Non-Acceptor, 31 years old
These participants explicitly discussed how their children had their own separate places where they kept their items.
Rodents
Rodents were an additional tampering risk concerning a few women living in rural communities in Uganda, Lilongwe, and Zimbabwe. Rodents are common household pests and women were concerned that they would damage their rings. One woman expressed how she was initially afraid of taking three rings home at a time because of rats:
At first, I was hesitant about it [taking rings home], because for instance the rings could easily be taken by rats–, where would I keep them? But later I realised that it’s actually a good idea [to take them home].— Chitungwiza, Ring-Acceptor, 40 years old.
When asked why she decided to keep her rings in a closed drawer, a participant responded:
For protection; so that they should not get lost or so that the mice shouldn’t get them.—Ring, Non-Acceptor, Lilongwe, 33 years old
Another woman explained how used rings give off a smell that could potentially attract rodents. She specifically purchased a metal suitcase after enrolling in the study to keep the rings secure:
Interviewer (I): Did you buy it [a suitcase] specifically for keeping vaginal rings?
Respondent (R): I bought it as an emergency for keeping the vaginal rings to avoid rats from biting them.
I: To prevent rats from biting them?
R: Yes…or from taking them since when you remove it out it usually has an odor which might attract rats and take them.—Kampala, Ring Acceptor, 44 years old
Despite these concerns, there were no reports of actual incidents where rodents damaged the rings in these qualitative interviews.
Other Household Members
Overall, participants reported that they were not concerned about other adult family and household members accessing their rings. Some ring acceptors had disclosed their ring use, so there was less concern of other people finding the rings. As one participant noted, her disclosure to her partner enabled her to feel at ease:
R: I may be worried if I can leave the [bedroom] door unlocked but I doubt that someone can enter the bedroom and get the rings where I am keeping them. But it can be no one else apart from my partner.
I: So how worried can you be about your partner finding the rings?
R: I cannot have worries because he knows I am using the ring.—Lilongwe, Ring Acceptor, 27 years old
Similarly, a non-acceptor described how, if she were to store her rings in her toiletry bag, she would not be concerned her sister would find her rings because she would have disclosed her use:
I wouldn’t worry about it much because they would know that I was using it [the ring]. So if they got a hold of it, it wouldn’t be a problem.—Ring Non-Acceptor, Cape Town, 28 years old.
For others, study participation was disclosed but not ring use: participants told household members partial details about the study but not that they were using a ring for HIV prevention. One participant reported that she was not concerned about leaving her rings in various places in her home because her family was aware of her study participation.
It [her ring storage location] didn’t affect me because they [family members] knew that I was in the study but they didn’t know what I was keeping at home. Even if a person could find a ring on top of [my wardrobe]. They wouldn’t do anything because they didn’t know what it was for. They only knew it was my things for the study only.—Johannesburg, Ring Acceptor, 21 years old.
Though this participant did not fully disclose her ring use, her family was aware that she was in a study and did not interfere. For others, the lack of concern of household members accessing the rings was primarily driven by the fact that there were established boundaries around privacy and respect of personal belongings, like the ones described for children. When asked why she was not worried her husband might find her ring, a woman discussed how she was confident that her husband would not go through her items,
“I know he doesn’t check in it because I leave this bag there too and he doesn’t check in it- Kampala, Ring Non-Acceptor, 32 years old.
However, there were two accounts of participants experiencing or fearing conflict regarding the rings. One participant described why she hid the rings from her sister:
She would start telling other people about it…The people she has told would start thinking the wrong way [about me].—Lilongwe, Ring Acceptor, 21 years old
Another participant described how she felt like her family interfered with her study participation:
I was scared that maybe some of the family members might get hold of my rings and throw them away, because they always wish the worst for me. They are even jealous of me being in the study even when I return from here they check my bag, I usually ask for results and they take that copy of results and throw them away.—Durban, Ring Acceptor, 38 years old.
Though these events were rare, they do indicate that ring storage was challenging for some participants whose families were not supportive of their decision to use the rings.
Ring Removal and Insertion Locations
Participants primarily reported changing their rings in their bedrooms or the rooms they bathed in. Women with indoor bathrooms/toilets tended to change their rings there, whereas women with outdoor toilets/bathrooms tended to change their rings in their bedrooms. When selecting a place to change rings the primary concern was finding a place which was private from others and met their sanitary needs. A chief requirement was that it was a room that was out of view of others and could be properly closed or locked.
It’s [the bedroom] the only place that is safe; I mean there aren’t any people that see me since I will remove it. So that is why I choose it because I could close it, like in other times there were people on the other side. I will just close the burglar bars and I would be able to remove it from here.—Cape Town, Ring Acceptor, 34 years old.
Additionally, the hygiene of the ring was a consideration when selecting a place to change rings. Women described the process they went through removing and inserting the rings and how it was important to do so in a clean place.
I saw that even if I do it in the bathroom, the bathroom is used by everyone and so it is not good to put the rings on the floor there. Whilst in the bedroom, you know it is just the two of you who sleep there and so you also know how to care for the rings and where you put the rings when you change. Besides that, it does not take much effort in the bedroom because everything I need is in one room.—Lilongwe, Ring Acceptor, 36 years old.
However, others felt like the bathroom would be more sanitary because they changed their rings after bathing. One participant described why she decided to change in the bathroom:
Because after changing it I have to wash my hands so that’s the proper place it was for me to change rings, that’s the only place in the house.—Durban, Ring Acceptor, 24 years old
Because many women lived in crowded homes, finding a private and sanitary place was often difficult. Some women overcame this challenge by waiting until no one else was at home to replace their ring.
I changed the ring in the bedroom when I was alone like in the afternoon or in the morning after my husband left for work so that he wouldn’t see me.—Ring Non-Acceptor, Chitungwiza, 22 years old
Discussion
Effectively reducing HIV incidence among women in Sub-Saharan Africa will require providing women with HIV prevention products that can be easily integrated into their lives (23). Findings from this study capture women’s perspectives on how their home environment influenced their use of the dapivirine vaginal ring. By utilizing a mapping approach, we were able to pinpoint features of the home environment that impacted ring use. We found that participants were primarily concerned with children and rodents tampering with rings, which influenced where and how they stored their rings. Participants’ decision on where to change their rings was based on sense of hygiene and privacy. Results suggest that ring storage, insertion, and removal was feasible in a variety of home environments.
Home environment did not appear to impact women’s decisions on whether to accept the vaginal rings. Although ring non-acceptors reported slightly less secure locations to potential store rings (i.e., suitcases and bags as opposed to lockable wardrobes), the types of concerns raised about ring storage were similar between the two groups. This finding is contrary to results from the Tablets, Ring, Injections as Options (TRIO) study of placebo products, where lack of a private place at home was one of the main predictors of unwillingness to use a vaginal ring in the future (23). While home environments presented some challenges, they were not significant enough to deter participants from accepting the vaginal ring in this study.
Participants reported having a range of locations they considered safe and secure to store their rings including wardrobes, suitcases, and bags. While some locations were accessible to children and may be considered less secure, parents often established or negotiated boundaries with their children which ensured that their children did not go through their personal belongings. The few parents who did not feel like they could store their rings at home chose to not keep additional rings at home and to change rings at the clinic. Improper storage of medicines has been found to be an issue in some rural and urban communities in Sub-Saharan Africa with households storing medicines within reach of children (24, 25). At home storage of antiretroviral therapy (ART) for HIV treatment was raised as a concern during the roll-out of Rwanda’s “Treat for all” strategy in 2016 which provided universal ART coverage for all people living with HIV. Organizations implementing the strategy indicated that at home storage of ART could lead to losses and misuse (26). There is a need for the development of storage options for those who do not have place which can be locked and kept away from children, household members, or pests.
Participants were less concerned about adult household members and partners finding rings. Some reported that this lack of concern was due to their disclosure of their ring use. Disclosure is an important facilitator to utilization of HIV prevention products (12, 27), including the vaginal ring (28). Some studies have found that disclosure can lead to support in remembering to use products such as PrEP (12, 29). There were a few reports of conflict regarding the rings. One participant reported being concerned that her sister may disclose her ring use to others without her consent and another worried that her family was trying to sabotage her participation in the research study. These incidents are indicative of some negative attitudes toward the ring, which has been reported in previous trials (18, 30).
The physical home environment impacted where and how women inserted and removed rings. About 41% of participants shared a bedroom with family members. Though some women chose to change their rings in the bathroom/toilet, it is important to note that half of participants lived in homes with outdoor bathrooms/toilets which were at times shared with other families. Household overcrowding limited privacy for some women. For several, this resorted in waiting for others to leave their homes until they felt comfortable changing. This time-delay is concerning because it may impact adherence. Although rings are designed to be worn continuously for four weeks, women often remove and reinsert the rings during menstruation (18). More frequent removal paired with inconsistent privacy could result in women remaining without their rings for a longer period than recommended, potentially resulting in reduced protection from HIV acquisition (3).
On July 24, 2020, the European Medicines Agency gave a positive opinion on the vaginal ring for use among cisgender women ages 18 and over in developing countries who cannot or choose not to use oral PrEP (9), paving the way for World Health Organization recommendation (31) and now progressing towards country regulatory approvals. As vaginal rings for HIV prevention become more widely available, important consideration should be taken to ensure that women feel comfortable using them at home. Providing additional products along with vaginal rings such as more durable containers to keep rings safe from children and pests, or hygiene products to remove odors from rings, may help support vaginal ring use. Additionally, for women in living arrangements that offer limited privacy, exploring options for discreet environments for ring insertion and removal (e.g., clinic-based options) may help facilitate use. Additionally, women interested in using vaginal rings should receive counseling to better understand the potential challenges with privacy related to ring storage, insertion, and removal so they can develop strategies to overcome these challenges and maintain their monthly ring changing schedule.
Several limitations must be considered in interpreting study results. First, all participants included in the study already had previous experience with the dapivirine vaginal ring due to their previous participation in MTN-020/ASPIRE. Thus, they may have already developed strategies to disclose and/or conceal ring use and they may have had practice inserting and removing the rings during menstruation or prior to sex. Second, data presented here are from participant’s PUEV interviews which occurred after ring-acceptors had been using the rings at home for at least one year during HOPE. It is possible that their comfort with at home use increased over the course of the study and we may have missed some challenges that occurred earlier on.
Questions remain about the feasibility of ring storage, removal, and insertion in rural areas. Participants in this study were primarily recruited from urban and peri-urban communities, with 64% reporting traveling less than an hour to the study clinic. Women using the ring in rural areas may experience different barriers that were not captured in this study. Additionally, HOPE participants were required to return used rings to the clinic for adherence testing, thus it was not possible to glean how women will be able to dispose of rings in light of concerns about children and rodents. Future studies should explore ring use storage in rural communities and disposal in both rural and urban settings.
Despite these limitations, this study includes several notable strengths. First, this study is amongst the first to explore how the physical home environment impacts the use of a biomedical HIV prevention. Studies to date have primarily explored partner, family member, and community responses to HIV prevention products. Second, the study utilized both visual and interview transcript data to understand the role of physical home environment allowing for the triangulation of information across sources (32). Third, participants were sampled from six different cities, in four different countries in Sub-Saharan Africa, increasing the transferability of study findings.
Conclusion
We found that women’s ability to properly store and change rings was shaped by their social and physical home environment. Although women reported some concerns with ring storage, they were able to overcome these challenges both by creating physical barriers or relying on pre-set boundaries with children and household members. Ring removal and insertion was impacted by overcrowding and limited privacy. Efforts to improve practicality of vaginal rings for home use should focus on secure ring storage, hygiene, and privacy.
Acknowledgements
The authors acknowledge with gratitude the MTN-025/HOPE participants who shared their stories, and the staff that contributed to this study. We would also like to MTN-025/HOPE Study Team lead by Jared Baeten (protocol chair), Thesla Palanee-Phillips (protocol co-chair), Nyaradzo Mgodi (protocol co-chair), Elizabeth Brown (protocol statistician), Ashley Mayo (FHI 360), and Lydia Soto-Torres (DAIDS medical officer). We additionally thank the qualitative protocol co-chairs Kenneth Ngure (Jomo Kenyatta University of Agriculture and Technology) and Ariane van der Straten (RTI International), and site leaders including: Malawi, Blantyre site (Johns Hopkins University, Queen Elizabeth Hospital): Bonus Makanani; Malawi, Lilongwe site (University of North Carolina, Chapel Hill): Lameck Chinula; South Africa, Cape Town site (University of Cape Town): Gonasagrie Nair; South Africa, Durban – Botha’s Hill, Chatsworth, Isipingo, Tongaat, Verulam sites (South African Medical Research Council): Gita Ramjee, Logashvari Naidoo, Dishiki Kalonji, Samantha Siva, Nishanta Singh; South Africa, Durban, eThekwini site (Center for the AIDS Programme for Research in South Africa): Leila Mansoor; South Africa, Johannesburg site (Wits RHI): Thesla Palanee-Phillips ; Uganda, Kampala site (John Hopkins University, Makerere University): Brenda Gati Mirembe; Zimbabwe, Chitungwiza and Harare—Zengeza, Seke South and Splihaus sites (University of Zimbabwe Clinical Trials Research Centre (UZ-CTRC): Nyaradzo Mgodi, Portia Hunidzarira, and Felix Mhlanga. Data management was provided by The Statistical Center for HIV/AIDS Research & Prevention (Fred Hutchinson Cancer Research Center, Seattle, WA) and site laboratory oversight was provided by the Microbicide Trials Network Laboratory Center (Pittsburgh, PA). For qualitative data, management was provided by the Women’s Global Health Imperative Program (RTI International, San Francisco, CA).
Funding The study was designed and implemented by the Microbicide Trials Network (MTN) and funded by the National Institute of Allergy and Infectious Diseases (UM1AI068633, UM1AI068615, UM1AI106707), with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health, all components of the U.S. National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The vaginal rings used in this study were developed and supplied by the International Partnership for Microbicides (IPM).
Footnotes
Data Availability Not Applicable.
Declarations
Conflict of Interest The authors declare that they have no conflict of interest.
Ethical Approval The study was approved by the Institutional Review Boards at RTI International, and at each study site and regulated by the U.S. National Institutes of Health and the Microbicide Trials Network.
Consent to Participate Written informed consent was obtained from all participants.
Consent for Publication Not Applicable.
References
- 1.UNAIDS. We’ve got the power: Women, adolescent girls, and the HIV response Geneva, Switzerland: UNAIDS; 2020. [Google Scholar]
- 2.Griffin JB, Ridgeway K, Montgomery E, Torjesen K, Clark R, Peterson J, et al. Vaginal ring acceptability and related preferences among women in low- and middle-income countries: A systematic review and narrative synthesis. PLoS One 2019;14(e11):0224898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baeten JM, Palanee-Phillips T, Brown ER, Schwartz K, Soto-Torres LE, Govender V, et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med 2016;375(22):2121–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown E, Palanee-Philips T, Marzinke M, Hendrix C, Dezutti C, Soto-Torres L, et al. , editors. Residual dapivirine ring levels indicate higher adherence to vaginal ring is associated with HIV-1 protection 21st International AIDS Society; 2016; Durban, South Africa. [Google Scholar]
- 5.Nel A, van Niekerk N, Kapiga S, Bekker L-G, Gama C, Gill K, et al. Safety and efficacy of a dapivirine vaginal ring for HIV prevention in women. N Engl J Med 2016;375(22):2133–43. [DOI] [PubMed] [Google Scholar]
- 6.Dapivirine Vaginal Ring 25 mg H-W-2168: Summary of Product Characteristics [press release] 2020. [Google Scholar]
- 7.Baeten J, Palanee-Phillips T, Mgodi N, Ramjee G, Gati B, Mhlanga F, et al. , editors. High adherence and sustained impact on HIV-1 incidence: Final results of an open-label extension trial of the dapivirine vaginal ring 10th International AIDS Society Conference on HIV Science; 2019; Mexico City, Mexico. [Google Scholar]
- 8.Nel A, Malherbe M, Mans W, Van Baelen B, Van Niekerk N, Louw C, editors. Safety, adherence and HIV-1 seroconversion in DREAM—an open-label dapivirine vaginal ring trial. 9th South African AIDS Conference; 2019. [DOI] [PubMed] [Google Scholar]
- 9.Vaginal ring to reduce the risk of HIV infection for women in non-EU countries with high disease burden [press release] 2020. [Google Scholar]
- 10.Pleasants E, Tauya T, Reddy K, Mirembe BG, Woeber K, Palanee-Phillips T, et al. Relationship type and use of the vaginal ring for HIV-1 prevention in the MTN 020/ASPIRE trial. AIDS Behav 2020;24(3):866–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Montgomery ET, van der Straten A, Chitukuta M, Reddy K, Woeber K, Atujuna M, et al. Acceptability and use of a dapivirine vaginal ring in a phase III trial. AIDS 2017;31(8):1159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Velloza J, Khoza N, Scorgie F, Chitukuta M, Mutero P, Mutiti K, et al. The influence of HIV-related stigma on PrEP disclosure and adherence among adolescent girls and young women in HPTN 082: a qualitative study. J Int AIDS S 2020;23(3):e25463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van der Straten A, Stadler J, Luecke E, Laborde N, Hartmann M, Montgomery ET, et al. Perspectives on use of oral and vaginal antiretrovirals for HIV prevention: the VOICE-C qualitative study in Johannesburg, South Africa. J Int AIDS Soc 2014;17:19146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shapley-Quinn MK, Manenzhe KN, Agot K, Minnis AM, van der Straten A. “We are not the same”: African women’s view of multipurpose prevention products in the TRIO clinical study. Int J Womens Health 2019;11:97–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Camlin CS, Koss CA, Getahun M, Owino L, Itiakorit H, Akatukwasa C, et al. Understanding demand for PrEP and early experiences of PrEP use among young adults in rural Kenya and Uganda: a qualitative study. AIDS Behav 2020;24(7):2149–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Golub SA. PrEP stigma: implicit and explicit drivers of disparity. Curr HIV/AIDS Rep 2018;15(2):190–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scorgie F, Stadler J, Baron D, Ju S, Ikaneng T, Mabude Z, et al. “It was not my aim to sleep there”: the impact of timing and location of sex on adherence to coitally-dependent HIV pre-exposure prophylaxis. AIDS Behav 2018;22(11):3692–704. [DOI] [PubMed] [Google Scholar]
- 18.Montgomery ET, Stadler J, Naidoo S, Katz AWK, Laborde N, Garcia M, et al. Reasons for nonadherence to the dapivirine vaginal ring: narrative explanations of objective drug-level results. AIDS 2018;32(11):1517–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gichane MW, Moracco KE, Pettifor AE, Zimmer C, Maman S, Phanga T, et al. Socioeconomic predictors of transactional sex in a cohort of adolescent girls and young women in malawi: a longitudinal analysis. AIDS Behav 2020;24(12):3376–84. [DOI] [PubMed] [Google Scholar]
- 20.Baeten JM, Palanee-Phillips T, Mgodi NM, Mayo AJ, Szydlo DW, Ramjee G, et al. Safety, uptake, and use of a dapivirine vaginal ring for HIV-1 prevention in African women (HOPE): an open-label, extension study. The Lancet HIV 2021;8(2):e87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van der Straten A, Katz A, Balán IC, Reddy K, Etima J, Woeber K, et al. , editors. A Qualitative Evaluation of Women’s Experience Receiving Drug Feedback in MTN-025/HOPE-An HIV Prevention Open-Label Trial of the Dapivirine Vaginal Ring 22nd International AIDS Conference; 2018; Amsterdam, Netherlands. [Google Scholar]
- 22.Guest G, MacQueen KM, Namey EE. Applied thematic analysis: sage publications; 2011. [Google Scholar]
- 23.van der Straten A, Agot K, Ahmed K, Weinrib R, Browne EN, Manenzhe K, et al. The Tablets, Ring, Injections as Options (TRIO) study: what young African women chose and used for future HIV and pregnancy prevention. J Int AIDS Soc 2018;21(3):e25094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wondimu A, Molla F, Demeke B, Eticha T, Assen A, Abrha S, et al. Household Storage of Medicines and Associated Factors in Tigray Region, Northern Ethiopia. PLoS One 2015;10(8):e0135650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teni FS, Surur AS, Belay A, Wondimsigegn D, Gelayee DA, Shewamene Z, et al. A household survey of medicine storage practices in Gondar town, northwestern Ethiopia. BMC Public Health 2017;17(1):238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nsanzimana S, Remera E, Ribakare M, Burns T, Dludlu S, Mills EJ, et al. Phased implementation of spaced clinic visits for stable HIV-positive patients in Rwanda to support Treat All. J Int AIDS Soc 2017;20:21635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Montgomery ET, van der Straten A, Chidanyika A, Chipato T, Jaffar S, Padian N. The importance of male partner involvement for women’s acceptability and adherence to female-initiated HIV prevention methods in Zimbabwe. AIDS Behav 2011;15(5):959–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts ST, Nair G, Baeten JM, Palanee-Philips T, Schwartz K, Reddy K, et al. Impact of male partner involvement on women’s adherence to the dapivirine vaginal ring during a phase III HIV prevention trial. AIDS Behav 2019;24:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amico KR, Wallace M, Bekker L-G, Roux S, Atujuna M, Sebastian E, et al. Experiences with HPTN 067/ADAPT study-provided open-label PrEP among women in cape town: facilitators and barriers within a mutuality framework. AIDS Behav 2017;21(5):1361–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chitukuta M, Duby Z, Katz A, Nakyanzi T, Reddy K, Palanee-Phillips T, et al. Negative rumours about a vaginal ring for HIV-1 prevention in sub-Saharan Africa. Cult Health Sex 2019;21(11):1209–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. Guidelines: updated recommendations on HIV prevention, infant diagnosis, antiretroviral initiation and monitoring Geneva: World Health Organization; 2021. p. 2021. [PubMed] [Google Scholar]
- 32.Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum 2014;41(5):545–7. [DOI] [PubMed] [Google Scholar]


