Abstract
Background
To determine the distribution of the near point of convergence (NPC) and its related factors in an elderly population in Tehran, Iran.
Methods
This population-based cross-sectional study was conducted on the elderly population (60 years of age and over) of Tehran, Iran in 2019. The samples were selected using stratified random cluster sampling. The examinations included the measurement of uncorrected and best-corrected visual acuity, objective and subjective refraction, unilateral and alternate cover test, ocular health examination, and NPC measurement.
Results
The mean age of the participants was 65.90 ± 4.56 years and 59.6% of them were females. The mean (95% CI) NPC in the total sample was 7.84 cm (95% CI: 7.65–8.03). The mean (95% CI) NPC in males and females was 7.92 cm (7.63–8.21) and 7.75 cm (7.54–7.97) (P = 0.338), respectively. The mean NPC increased from 7.8 cm (95% CI: 7.55–8.05) in the age group 60–64 years to 8.83 cm (95% CI: 7.47–10.2) in the age group ≥ 80 years (P > 0.05). The mean (95% CI) NPC in emmetropic, myopic, and hyperopic individuals was 7.67 cm (95% CI: 7.33–8.02), 7.96 cm (7.56–8.37), and 7.87 cm (7.63–8.11), respectively (P = 0.378). There was no statistically significant relationship between NPC with education level, smoking, diabetes mellitus (DM), and hypertension (HT).
Conclusions
The NPC values found in this study were significantly lower (less remote) than the values reported in previous studies in similar age groups. The NPC had no significant relationship with age, sex, education level, smoking, DM, and HT.
Subject terms: Epidemiology, Health care
Introduction
The near point of convergence (NPC) is the nearest point in space where an individual can maintain single binocular vision [1]. This parameter represents the maximum convergence ability (gross convergence) and consists of four major components of the vergence system, including the tonic vergence, the accommodative vergence, the fusional vergence, and the proximal vergence [2, 3]. NPC measurement is one of the routine binocular vision examinations, which is of special value in the diagnosis of convergence insufficiency (CI) as the most common binocular visual anomaly [4, 5]. A remote NPC is the most consistent finding in patients with CI and is used in making the final diagnosis of CI by the majority of practitioners [6, 7]. NPC recession is associated with an increase of vision-related symptoms during close work [8]. Therefore, information about normal NPC values in the general population is important to increase its diagnostic value and improve clinical interpretation of this index. Several studies have addressed the distribution of NPC and its related factors in different populations [1, 2, 9–19]. However, most of the available studies were non-population-based studies, conducted on selected clinical populations and mostly targeted children and young adults. To the best of our knowledge, no study in the literature has evaluated the distribution of NPC specifically in the elderly population. Some previous studies have shown an increase in NPC with age [2, 9, 18], with these changes being more pronounced in the elderly (over 60 years of age) [2, 18]. Given the age-related changes in NPC, the use of existing recommendations (mainly reported for children and young adults) to interpret this finding in the elderly population is debatable and may lead to misinterpretation of the index. Life expectancy is increasing in most countries of the world, so that according to the World Health Organization (WHO), the percentage of the population over the age of 60 years in the world will increase from 12% in 2015 to 22% in 2050 [20]. Therefore, there is a need to conduct a study on NPC distribution specifically in the elderly. The present population-based study aimed to describe the distribution of NPC and its related factors in a large sample of an Iranian elderly population.
Material and methods
This report was a part of the Tehran Geriatric Eye Study (TGES); a population-based cross-sectional study that was conducted in 2019 in Tehran, the capital of Iran, using stratified multistage random cluster sampling method. The target population in TGES was all residents of Tehran over 60 years of age. 165 clusters were randomly selected proportionally to size from 22 strata of Tehran city. After identifying each cluster, a sampling team went to the address of that cluster and performed the sampling based on the predetermined protocol. All individuals over the age of 60 years were invited to participate in the study after explaining the purpose of the study and ensuring that their information would remain confidential. Within a predetermined day, all participants were transferred to the examination site free of charge, and in the first stage, a consent form was obtained. After obtaining consent and explaining the goal and steps of the study, a preliminary interview was performed to record information regarding smoking, education level, any history of previous eye examinations, ocular and systemic disease, ocular trauma, previous ocular surgery, and use of ocular or systemic medications. The blood pressure was then measured, and a blood sample was taken, followed by optometric examinations.
Examination protocol
All optometric examinations were performed in an examination room with standard lighting conditions. First, the uncorrected distance visual acuity was measured by a LED visual acuity chart (Smart LC 13, Medizs Inc., Korea) at a distance of 6 meters (m). Objective refraction was then performed using an auto-refractometer (ARK-510A, Nidek Co. LTD, Aichi, Japan). The optimal distance optical correction was determined by the subjective refraction and the best-corrected distance visual acuity (BCVA) was recorded. Also, the amount of appropriated near addition lenses was determined using the near subjective refraction. In the next step, the unilateral and alternate cover tests were performed to assess the binocular alignment at 6 m and 40 cm, respectively, and any deviation (tropia or phoria) was measured using a prism bar. The near cover test was done through addition lenses. The NPC was measured using a single letter on the near Snellen chart one line above the BCVA along the subject’s midline. The target was gradually moved toward the subject from a distance of 50 cm at a recommended constant rate of about 1 cm/s. The subject was asked to keep the target as single as possible, and to report whenever the target became double. At the point where diplopia was reported by the individual, or the examiner objectively observed the loss of binocularity, the target’s distance was measured from the spectacle plane by a large millimeter ruler. To increase the reliability of the test, the NPC measurement was measured five times and the average of 5 measurements was recorded as the final NPC finding. Finally, all participants underwent ocular health examination by an ophthalmologist using slit-lamp biomicroscopy and +90 lens. Exclusion criteria included BCVA less than 20/30 in either eye, strabismus, amblyopia, history of any intraocular surgery, any active ocular pathology affecting binocular vision, and history of ocular trauma.
Definitions
Refractive errors were defined based on the spherical equivalent (SE) of subjective refraction. The values of near exophoria and esophoria were considered positive and negative, respectively. Myopia was defined as a SE of −0.50 or more and hyperopia as +0.50 or more. Diabetes mellitus (DM) was considered based on a previous diagnosis or hemoglobinA1c level of 6.5% or greater. Hypertension (HT) was defined based on a previous diagnosis or a systolic pressure ≥135 mm Hg or a diastolic pressure ≥85 mm Hg.
Statistical analysis
NPC was summarized as mean and standard deviation (SD) in the total sample and groups categorized by age, sex, refractive errors, education level, DM, and HT. To calculate the mean values, the results were directly standardized according to the latest census on the population aged 60 years and over in Tehran. Cluster sampling was considered in calculating the confidence interval. Possible relationships were assessed using simple and multiple linear regressions. The correlation between near heterophoria and NPC was examined by Pearson correlation test. A P value < 0.05 was considered statistically significant.
Results
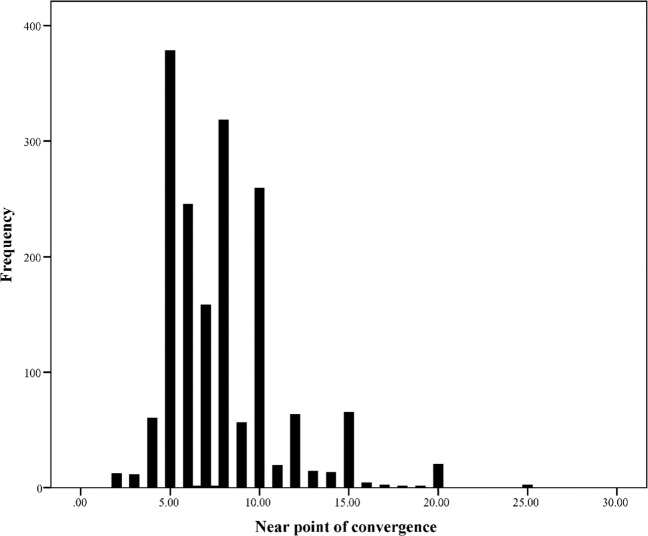
3310 of the 3791 invitees participated in this study (response rate: 87.3 percent). After applying exclusion criteria, statistical analysis was performed with the data from 1784 individuals. The reasons for exclusion included: best-corrected visual acuity less than 20/30, amblyopia or active anterior or posterior ocular disease: 585 individuals, a history of ocular surgery: 751 individuals, a history of ocular trauma: 22 individuals, strabismus: 115 individuals, use of drugs affecting binocular vision: 44 individuals, physical inability to attend for testing: 9 individuals. The mean age of the participants was 65.90 ± 4.96 (60–95 years) and 59.6% (1063) of them were females. Figure 1 shows the distribution of NPC in study participants. Overall, the mean NPC was 7.84 cm (95% CI: 7.65–8.03). The mean (95% CI) of NPC values in different groups of study variables has been shown in Table 1. According to the simple linear regression (Table 2), there was no significant relationship between NPC and all study variables including age, sex, education level, smoking, DM, HT, and refractive errors (all P values > 0.05). The association between NPC and these variables was also investigated in a multiple linear regression model (Table 2). As seen in Table 2, none of these variables had a statistically significant relationship with NPC in the presence of each other. There was a significant positive correlation between near heterophoria and NPC; increased (more remote) NPC was associated with a statistically significant increase in near exophoria (correlation coefficient: 0.78, P < 0.001).
Fig. 1.
The distribution of the near point of convergence (cm) in the study participants.
Table 1.
The mean and 95% confidence interval (CI) of the near point of convergence (cm) in the present study according to the different study variables.
| Mean (95% CI) | ||
|---|---|---|
| Total | 7.84 (7.65–8.03) | |
| Sex | Male | 7.92 (7.63–8.21) |
| Female | 7.75 (7.54–7.97) | |
| Smoking | Yes | 7.64 (7.18–8.09) |
| No | 7.88 (7.68–8.07) | |
| Diabetes | Yes | 7.78 (7.43–8.14) |
| No | 7.85 (7.64–8.05) | |
| Hypertension | Yes | 7.74 (7.48–8.01) |
| No | 7.88 (7.67–8.10) | |
| Age | 60–64 | 7.80 (7.55–8.05) |
| 65–69 | 7.84 (7.56–8.12) | |
| 70–74 | 7.97 (7.56–8.38) | |
| 75–79 | 7.51 (6.87–8.14) | |
| ≥80 | 8.83 (7.47–10.2) | |
| Education level | Illiterate | 8.19 (7.62–8.76) |
| Primary | 7.74 (7.40–8.09) | |
| Guidance | 7.66 (7.28–8.03) | |
| High | 7.80 (7.51–8.08) | |
| College | 8.07 (7.60–8.53) | |
| Refractive errors | Emmetropia | 7.67 (7.33–8.02) |
| Myopia | 7.96 (7.56–8.37) | |
| Hyperopia | 7.87 (7.63–8.11) | |
Table 2.
The association between the near point of convergence and the studied variables by simple and multiple linear regression.
| Simple | Multiple | ||||
|---|---|---|---|---|---|
| Coefficient (95% CI) | P value | Coefficient (95% CI) | P value | ||
| Age | 60–64 | 1 | 1 | ||
| 65–69 | 0.04 (−0.29 to 0.37) | 0.815 | 0.05 (−0.28 to 0.39) | 0.750 | |
| 70–74 | 0.17 (−0.28 to 0.62) | 0.453 | 0.13 (−0.33 to 0.59) | 0.572 | |
| 75–79 | −0.29 (−0.97 to 0.38) | 0.392 | −0.35 (−1.05 to 0.36) | 0.333 | |
| ≥80 | 1.03 (−0.32 to 2.38) | 0.133 | 1.06 (−0.38 to 2.50) | 0.148 | |
| Sex | Male/female | −0.16 (−0.50 to 0.17) | 0.338 | −0.22 (−0.60 to 0.15) | 0.246 |
| Education | Illiterate | 1 | 1 | ||
| Primary | −0.45 (−1.09 to 0.20) | 0.175 | −0.46 (−1.13 to 0.22) | 0.185 | |
| Guidance | −0.53 (−1.20 to 0.13) | 0.112 | −0.49 (−1.17 to 0.19) | 0.159 | |
| High | −0.39 (−1.02 to 0.23) | 0.218 | −0.39 (−1.06 to 0.27) | 0.245 | |
| College | −0.12 (−0.88 to 0.64) | 0.748 | −0.15 (−0.94 to 0.63) | 0.698 | |
| Smoking | No | 1 | 1 | ||
| Yes | −0.24 (−0.70 to 0.22) | 0.308 | −0.39 (−0.91 to 0.13) | 0.140 | |
| Diabetes | No | 1 | 1 | ||
| Yes | −0.06 (−0.43 to 0.31) | 0.742 | −0.03 (−0.42 to 0.35) | 0.862 | |
| Hypertension | No | 1 | 1 | ||
| Yes | −0.14 (−0.42 to 0.15) | 0.348 | −0.14 (−0.45 to 0.17) | 0.367 | |
| Refractive errors | Emmetropia | 1 | 1 | ||
| Myopia | 0.29 (−0.23 to 0.81) | 0.277 | 0.22 (−0.32 to 0.77) | 0.421 | |
| Hyperopia | 0.19 (−0.20 to 0.59) | 0.334 | 0.19 (−0.22 to 0.59) | 0.363 | |
CI confidence interval.
Discussion
In the present study, we evaluated the distribution of NPC in a relatively large sample of Iranian elderly population aged 60 years and over. The associations between NPC and some factors including sex, age, refractive errors, education level, smoking, DM, and diabetes were also investigated. Among the strengths of this study is the relatively large sample size and also the sampling method, which increases the generalizability of the results.
The mean NPC was 7.84 in the total sample. As mentioned earlier, several studies have examined the distribution of NPC,1-2,9-19 but most of these studies were performed on children and young adult populations whose results cannot be compared with the present study. A review of the literature found only two studies reporting the distribution of NPC in the elderly population over 60 years of age [2, 18]. However, the age range of these two studies was wide, and individuals over the age of 60 years included a small portion of the overall sample. The mean NPC found in the age groups 60–69 years and more than 70 years in the present study was significantly closer (less remote) than the values reported in similar age groups in the study by Ostadimoghaddam et al. (11.98 and 13.06 cm, respectively) [2], and Hashemi et al. (9.53 and 10.44 cm, respectively) [18]. These differences may be due to subtle differences in NPC testing instructions, for example “tell me when the target becomes double” versus “try to keep the target single as much as possible and report whenever diplopia occurs”. This difference in NPC values among studies can also be attributed to racial factors. These three studies were conducted in different geographic parts of Iran. Maples and Hoenes studied the distribution of NPC in elementary school children and found that the NPC values were significantly different between white and black Americans [11]. Given that the present study was conducted specifically on the elderly population, its results could provide a better picture of the distribution of NPC in this age group.
No statistically significant relationship was found between the NPC and gender. This finding is in line with the results of a study by Hashemi et al. In the study conducted by Ostadimoghaddam et al., a statistically significant difference in NPC values was found between males and females. However, the authors pointed out that this difference could be ignored due to the small effect size, and that the amount of NPC in both sexes was clinically comparable [2].
Age is one of the influential factors on the NPC and age-related recession of NPC has been reported in different studies [2, 9, 18]. It seems that these age-related changes are mainly due to a decrease in the accommodative effort along with reduced accommodative amplitude and subsequently a decrease in the accommodative vergence [2]. In the study by Ostadimoghaddam et al., most NPC changes occurred around the age of presbyopia [2]. However, no significant relationship was found between NPC and age in the present study. One reason for this finding may be the age range of the participants in this study. Given that after the age of 60 years, the average amplitude of accommodation is practically zero, it is not expected that there will be significant changes in the accommodative vergence. Overall, it can be concluded that after the age of 60 years, the NPC is not affected by age.
In the present study, there was no significant association between NPC and refractive errors. There are conflicting results about the relationship between NPC and refractive errors in the literature. In the study by Ostadimoghaddam et al., the refractive error did not show a significant effect on NPC changes after removing the effects of age and sex [2]. Studies in children have reported that NPC values were lower (less remote) in myopic individuals, and this finding has been linked to a higher accommodative convergence/accommodation (AC/A) ratio in myopes [16, 21, 22]. A high AC/A ratio is associated with an increase in accommodative convergence and thus an increase in gross convergence, leading to lower (closer) NPC values. Since the effect of accommodative convergence is eliminated in the elderly, it is expected that the refractive error will not be a factor influencing the NPC values in this age group.
We examined the relationship between DM and NPC in the present study but did not find a significant relationship. We also found no significant association between NPC and HT. Only one study in the literature was found on the relationship between NPC and HT [23]. That study found that patients with HT had more remote NPC values, but the study population was between the ages of 18 and 55 years.
One of the limitations of the present study is the lack of evaluation of the vision-related symptoms, considering that this evaluation requires a valid and reliable assessment tool such as the convergence insufficiency symptom survey (CISS) and the Persian version of CISS is not present. Another limitation of this study is that the amount of close work was not considered and we were not able to investigate the effects of this parameter on the NPC finding. One issue that can be raised based on the findings of the present study is the prevalence of CI. However, such evaluation requires further extensive analysis taking into account other parameters such as the magnitude of far and near heterophoria, the accommodative convergence/accommodation (AC/A) ratio, and the positive fusional vergence. It is also necessary to compare the prevalence of CI with previous similar studies to reach a meaningful conclusion in this regard. Therefore, considering the extent of this issue, we intend to evaluate the prevalence of CI and its related factors in detail in a separate study.
In conclusion, the NPC values found in this study were significantly lower (less remote) than the values reported in previous studies in similar age groups. The results of this study are important in that we should not expect very different amounts of NPC in the elderly population compared to other age groups. The NPC had no significant relationship with age, sex, education level, smoking, DM, and HT.
Summary
What was known before
Near point of convergence is an important clinical index used by clinicians for the analysis of binocular vision performance As the NPC is influenced by age it is important to have information about the distribution and normal values of this parameter among all age groups.
What this study adds
The near point of convergence values found in this study were significantly lower (less remote) than the values reported in previous studies in similar age groups. The near point of convergencehad no significant relationship with age, sex, education level, smoking, diabetes, and blood pressure.
Funding
This project was supported by National Institute for Medical Research Development (NIMAD) affiliated with the Iranian Ministry of Health and Medical Education (Grant No: 963660).
Author contributions
Design and conduct of the study (MK, PN, HH); collection, management of the data (MP, AY, MAg, MAs, MK); analysis, and interpretation of the data (MK and PN); and preparation, review, and approval of the manuscript (HH, PN, AJ, MP, AY, MAg, MAs, MK).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of National Institute for Medical Research Development affiliated with the Iranian Ministry of Health and Medical Education. The tenets of the Helsinki Declaration were followed, and informed consent was obtained from all participants (Grant No: 963660).
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Scheiman M, Gallaway M, Frantz KA, Peters RJ, Hatch S, Cuff M, et al. Nearpoint of convergence: test procedure, target selection, and normative data. Optom Vis Sci. 2003;80:214–25. doi: 10.1097/00006324-200303000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Ostadimoghaddam H, Hashemi H, Nabovati P, Yekta A, Khabazkhoob M. The distribution of near point of convergence and its association with age, gender and refractive error: a population‐based study. Clin Exp Optom. 2017;100:255–9. doi: 10.1111/cxo.12471. [DOI] [PubMed] [Google Scholar]
- 3.Siderov J, Chiu SC, Waugh SJ. Differences in the nearpoint of convergence with target type. Ophthalmic Physiol Opt. 2001;21:356–60. doi: 10.1046/j.1475-1313.2001.00609.x. [DOI] [PubMed] [Google Scholar]
- 4.Rouse MW, Borsting E, Deland PN. Reliability of binocular vision measurements used in the classification of convergence insufficiency. Optom Vis Sci. 2002;79:254–64. doi: 10.1097/00006324-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Pang Y, Gabriel H, Frantz KA, Saeed F. A prospective study of different test targets for the near point of convergence. Ophthalmic Physiol Opt. 2010;30:298–303. doi: 10.1111/j.1475-1313.2010.00731.x. [DOI] [PubMed] [Google Scholar]
- 6.Scheiman M, Wick B. Clinical management of binocular vision: heterophoric, accommodative, and eye movement disorders. Lippincott Williams & Wilkins: United State; 2008.
- 7.Rouse M, Hyman L, Hussein M, Group C. How do you make the diagnosis of convergence insufficiency? Survey results. J Optom Vis Devel. 1997;28:91–7. [Google Scholar]
- 8.Hamed M-M, David AG, Marzieh E. The relationship between binocular vision symptoms and near point of convergence. Indian J Ophthalmol. 2013;61:325–8. doi: 10.4103/0301-4738.97553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abraham NG, Srinivasan K, Thomas J. Normative data for near point of convergence, accommodation, and phoria. Oman J Ophthalmol. 2015;8:14–8. doi: 10.4103/0974-620X.149856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hayes GJ, Cohen BE, Rouse MW, De PL. Normative values for the nearpoint of convergence of elementary schoolchildren. Optom Vis Sci. 1998;75:506–12. doi: 10.1097/00006324-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Maples WC, Hoenes R. Near point of convergence norms measured in elementary school children. Optom Vis Sci. 2007;84:224–8. doi: 10.1097/OPX.0b013e3180339f44. [DOI] [PubMed] [Google Scholar]
- 12.Capobianco NM. The subjective measurement of the near point of convergence and its significance in the diagnosis of convergence insufficiency. Am Orthop J. 1952;2:40–2. doi: 10.1080/0065955X.1952.11981061. [DOI] [PubMed] [Google Scholar]
- 13.Cohen A, Lieberman S, Stolzberg M, Ritty JM. The NYSOA vision screening battery-a total approach. J Am Optom Assoc. 1983;54:979–84. [PubMed] [Google Scholar]
- 14.Jang JU, Park I-J, Jang JY. The distribution of near point of convergence, near horizontal heterophoria, and near vergence among myopic children in South Korea. Taiwan J Opthalmol. 2016;6:187–92. doi: 10.1016/j.tjo.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yekta A, Hashemi H, Ostadimoghaddam H, Haghighi B, Shafiee H, Mehravaran S, et al. Strabismus and near point of convergence and amblyopia in 4–6 year-old children. Strabismus. 2016;24:113–9. doi: 10.1080/09273972.2016.1205103. [DOI] [PubMed] [Google Scholar]
- 16.Hashemi H, Nabovati P, Khabazkhoob M, Yekta A, Emamian MH, Fotouhi A. Near point of convergence in iranian schoolchildren: normative values and associated factors. Strabismus. 2018;26:126–32. doi: 10.1080/09273972.2018.1475493. [DOI] [PubMed] [Google Scholar]
- 17.Hashemi H, Pakbin M, Ali B, Yekta A, Ostadimoghaddam H, Asharlous A, et al. Near points of convergence and accommodation in a population of university students in Iran. J Ophthalmic Vis Res. 2019;14:306–14. doi: 10.18502/jovr.v14i3.4787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hashemi H, Pakzad R, Yekta A, Asharlous A, Aghamirsalim M, Ostadimoghaddam H, et al. The distribution of near point of convergence in an Iranian rural population: A population-based cross-sectional study. Saudi J Ophthalmol. 2019;33:148–52. doi: 10.1016/j.sjopt.2019.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sayın N, Akar S, Gökyiğit B, Kaynak P, Sayın DT, Demirok A. Near point of convergence break for different age groups in Turkish population with normal binocular vision: Normative data. Türk Oftalmoloji Dergisi. 2013;43:402–6. doi: 10.4274/tjo.78700. [DOI] [Google Scholar]
- 20.United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights (ST/ESA/SER.A/430) 2019.
- 21.Mutti DO, Jones LA, Moeschberger ML, Zadnik K. AC/A ratio, age, and refractive error in children. Investig Ophthalmol Vis Sci 2000;v:2469–78. [PubMed]
- 22.Gwiazda J, Grice K, Thorn F. Response AC/A ratios are elevated in myopic children. Ophthalmic Physiol Opt. 1999;19:173–9. doi: 10.1046/j.1475-1313.1999.00437.x. [DOI] [PubMed] [Google Scholar]
- 23.Pongsachareonnont P, Uramphorn N, Hounnaklang N. Association between visual status and mental health status in Thai rural elderly: a community-based study. Int J Ophthalmol. 2018;11:852–7. doi: 10.18240/ijo.2018.05.23. [DOI] [PMC free article] [PubMed] [Google Scholar]