Abstract
Extracellular vesicles (EVs) exert their biological functions by delivering proteins, metabolites, and nucleic acids to recipient cells. EVs play important roles in cancer development. The anti-tumor effect of EVs is by their cargos carrying proteins, metabolites, and nucleic acids to affect cell-to-cell communication. The characteristics of cell-to-cell communication can potentially be applied for the therapy of cancers, such as gastric cancer. In addition, EVs can be used as an effective cargos to deliver ncRNAs, peptides, and drugs, to target tumor tissues. In addition, EVs have the ability to regulate cell apoptosis, autophagy, proliferation, and migration of cancer cells. The ncRNA and peptides that were engaged with EVs were associated with cell signaling pathways in cancer development. This review focuses on the composition, cargo, function, mechanism, and application of EVs in cancers.
Keywords: EVS, Cancer, ncRNA, drug loading, target
Introduction
EVs are 40–100 nm extracellular vesicles that are released by cells (Kahlert and Kalluri, 2013). EVs were initially observed in sheep reticulocytes in the 1980s (Raposo and Stoorvogel, 2013). Recently, studies have focused on the source of their endocytosis and on distinguishing them from micro-vesicles (Théry et al., 2002). EVs have anti-tumor functions associated with the development of a variety of cancers, such as breast, stomach, liver, and lung cancers (Table 1).
TABLE 1.
The function of EVs in cancers.
| Name | Fatality rate (%) | Function of EVs | References |
|---|---|---|---|
| Lung cancer | 89 | Diagnosis | Kahlert and Kalluri, (2013) |
| Liver cancer | 60–70 | Inhibited cell growth | Raposo and Stoorvogel, (2013) |
| gastric cancer | 12.4 | Induce cell apoptosis | Théry et al. (2002) |
| Colon cancer | 12 | Inhibited EMT | Kowal et al. (2016) |
| Breast cancer | 6.6 | Plasma biomarkers | Kahlert et al. (2014) |
The Biogenesis and Composition of EVs
Mammalian cell, EVs are highly heterogeneous. They contain lipid membranes, proteins, RNAs, and DNAs (Kowal et al., 2016). The lipid membrane of EVs carries the ligands and receptors from the source cells and has a role in cell-to-cell communication (Valadi et al., 2007; Kahlert et al., 2014). Due to the specificity of the lipid membrane, EVs can invade target cells through biogenesis (Balaj et al., 2011). The components on the membrane also play a key role in cell-to-cell communication (Wu et al., 2021). EVs use lipid membranes to enter recipient cells to release cargo and affect recipient cells. These characteristics indicate that EVs have potential applications in regulating cancer development.
The Formation of EVs
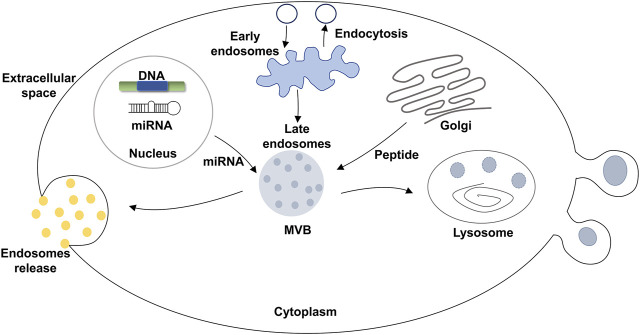
Many EVs formed from normal and pathological cells. In contrast to micro-vesicles, EVs are mainly derived from multivesicular bodies (MVBs) that are formed by intracellular lysosomal particles. EVs are released into the extracellular matrix through the fusion of the outer membrane of the MVBs with the membrane of source cells (Figure 1). Specifically, EVs are formed through the endosomal pathway. First, the endosome is formed by the invasion of the plasma membrane during cell maturation process (Harding et al., 1983). The endosome is a membrane-encapsulated vesicular structure and includes both early and late endosomes. Early endosomes are usually located outside of the cytoplasm. In contrast, late endosomes are located inside of the cytoplasm, near the nucleus. Endosomes are acidic vesicles without lysosomal enzymes (Bainton and Farquhar, 1968). The invasion of endosomes produces MVBs which contain 40–150 nm vesicles. The inner membrane forms intraluminal vesicles (ILV). Finally, the late lysosome melts or fuses with the plasma membrane of the source cell and degrades MVBS to release EVs (Harding et al., 1983). This process is known as EV biogenesis and is different from apoptotic bodies (Taylor and Gercel-Taylor, 2008). EVs are widely observed in tumor cells, mesenchymal stem cells, fibroblasts, neurons, endothelial cells (ECs), and epithelial cells (Kalluri, 2016). Previous reports have suggested that the tumor cells can specifically absorb their own secreted EVs (Kahlert and Kalluri, 2013). This implies that during the formation of EVs, specific biomarkers are formed on the surface of the EVs. These biomarkers are the cues that render EVs to be absorbed by specific cells.
FIGURE 1.
Formation of EVs.
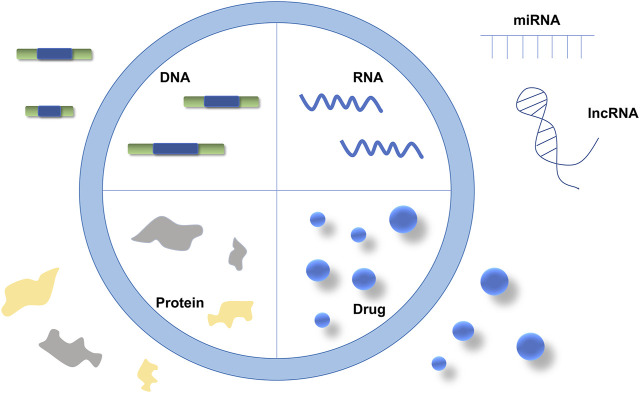
EVs Cargo
Nucleic acids such as DNAs or RNAs, proteins, or drugs can be carried in EVs as cargo to be delivered for cell-to-cell communication (Figure 2). In the past decades, miRNAs and mRNAs have been found to be major components of EVs. The improvement of EV detection techniques has allowed more RNA species, including transfer RNAs (tRNAs), long non-coding RNAs (lncRNAs), and viral RNAs, to be observed (Valadi et al., 2007; Su et al., 2021). An increasing amount of data suggests that these RNAs, such as lncRNA, have crucial functions that affect the development of cancer cells (Gusachenko et al., 2013). Moreover, numerous studies have demonstrated that the abnormal expressions of miRNAs, lncRNAs, and mRNAs are associated with cancer development (Chan and Tay, 2018; Huang et al., 2020). Hence, these RNAs, that are contained within EVs, can either preserve or degrade their target genes.
FIGURE 2.
The contents of EVs.
Cancers develop because of the expression and interaction of numerous genes or proteins. EVs can express proteins through genetic engineering (Silva et al., 2021). The EVs were obtained from the source cells that were transfected with the target gene plasmids. These EVs contain the synthesized proteins or peptides through cell culture (Perin et al., 2011). There is evidence that fusing the exosomally-enriched membrane protein (Lamp 2b) with the ischemic myocardium‐targeting peptide (IMTP) can be used to inhibit cancer development by molecular cloning lentiviral packaging protocols (Fernández et al., 2002). EVs secreted by tumor cells can be taken up by the same tumor cell with specificity. Some molecules (such as Let-7a) can be easily introduced to donor cells through EVs, and tumor targeting EVs carrying these molecules can be used for cancer treatment (Wu et al., 2021). In addition, EVs can carry various chemotherapeutic drugs and materials for targeted treatment of cancers (Wang et al., 2019a).
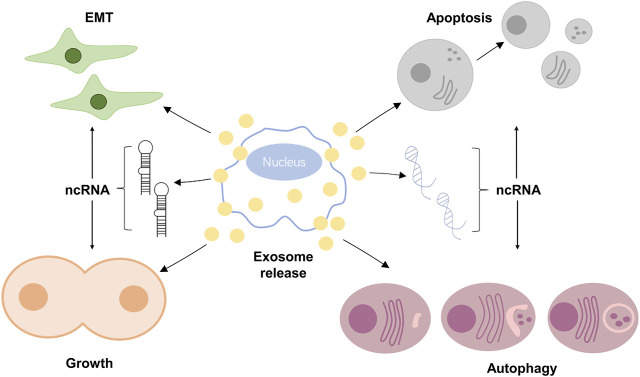
EVs can Decide Cell Fate
The function of EVs depends on the source cells, such as tumor cells or stem cells (Draganov et al., 2019; Dzobo et al., 2020). The EVs released from these source cells can affect the apoptosis, growth, cell cycle, migration, invasion, and differentiation of recipient cells. Previous studies have indicated that tumor-released EVs could deliver genetic information to the recipient cells for cell-to-cell communication (Valadi et al., 2007). This process promotes cell growth, invasion, and active angiogenesis in a tumor microenvironment (Figure 3).
FIGURE 3.
EVs decide cell fate.
Initially, EVs were considered to be “garbage bags” that could not affect other cells (Kalluri, 2016). However, it was found that EVs could be absorbed by target cells and their cargos could be released to affect cell signaling transduction, therefore determining the fate of the recipient cells (Pan et al., 1985). Additional evidence suggested that tumor cells released EVs that promoted tumor growth and invasion in vivo (Ramírez-Ricardo et al., 2020). EVs that carried tumor suppressors, such as let-7a, could inhibited tumor growth (Melo et al., 2014).
The Function of EVs in Cell Proliferation
Indefinite proliferation is a key feature of tumor cells. The abnormal cell cycle of tumor cells is associated with un-controlled cell growth. Previous reports confirmed that miRNA-122 was involved in the cell cycle as well as the proliferation of hepatocellular carcinoma (HCC) cells (Fernández et al., 2002; Xu et al., 2011). A recent report showed that the EVs carrying circRNA plays a role in the proliferation of HCC cells (Xue et al., 2017). In addition, arsenite could increase the expression of circRNA_100284 carried by EVs, altering the cell cycle and their proliferation by acting on miR-217 (Lu et al., 2015). The expression of the cell proliferation biomarkers E2H2 and cyclin D1 were regulated by the circRNA_100284 contained within EVs, and the expression of circRASSF2 was increased in laryngeal squamous cell carcinoma (LSCC) tissue compared to paracancerous tissue. The circRASSF2 carried by EVs promoted LSCC cell growth via the miR-302B-3p/IGF-1R axis (Tian et al., 2019). Thus, EVs have the ability to regulate cell proliferation through their cargos.
The Function of EVs in Epithelial-Mesenchymal Transition
The cell-to-cell communication in tumors might promote EMT of cancers. Previous data has shown that the EV-released circRNA PED8A was associated with increased lymphatic invasion, TNM staging, and low survival rate of patients. Furthermore, the circRNA PED8A from EVs promoted tumor cell growth by activating MET, which is a tyrosine kinase receptor (Luna et al., 2019). In addition, the release of circRNA PED8A contained within EVs into the blood circulation promotes invasion and metastasis through the MACC-MET-ERK or AKT pathway. More evidence indicated that EV-released circRNA NRIP1 promoted proliferation, migration, and metastasis through AKT1/mTOR signaling pathway in gastric cancer. The involvement of this pathway has also been confirmed in breast cancer cells in patients (Wang et al., 2019b; Zhang et al., 2019). The circPTGR1 carried in EVs was found to contribute to the metastasis of hepatocellular carcinoma (Wang et al., 2019c). Interestingly, knock out of circPTGR1 in the source cells, their EVs inhibited invasion and migration of cancer cells. The increased expression of EV-released circ-IARS is related to the EMT of pancreatic cancer (Li et al., 2018). Therefore, EVs can act as messenger vehicles for cell-to-cell communication, releasing ncRNAs that contribute to the EMT in cancers.
The Function of EVs in Apoptosis and Autophagy
Cell apoptosis and autophagy are programmed cell death, both of them are abnormal in cancers. Previous reports have indicated that EVs containing anti-tumor drugs can induce cell apoptosis in HCCs (Slomka et al., 2020). Furthermore, EVs containing miRNA mimics such as let-7a have been found to induce cell apoptosis in breast cancer (Ahmed et al., 2021). In addition, EVs have the ability to regulate autophagy. There is evidence that EVs can enhance autophagy in glioblastoma (GBM) (Pavlyukov et al., 2018). These findings suggest that EVs play a role in cell apoptosis and autophagy.
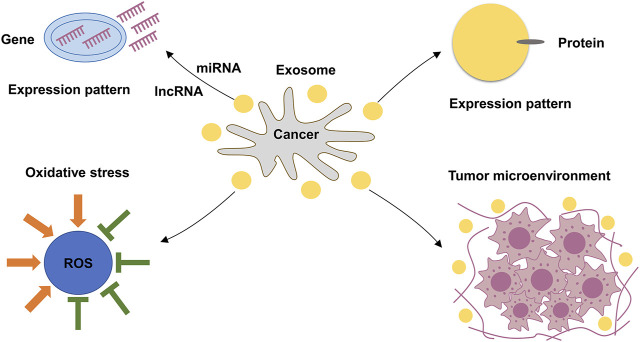
EVs Stimulate Oxidative Stress
Studies have shown that low levels of reactive oxygen species (ROS) were observed in the stem cells of liver cancer and breast cancer (Shi et al., 2012). The EVs of SV-HUC-1 cells were found to mediate the P38/NF-kB signaling pathway, enhancing the levels of OS (Xi et al., 2020). This suggests that EVs were involved in OS, that may contribute to the development of cancers (Figure 4).
FIGURE 4.
The function of EVs.
EVs Regulate the Expression of lncRNA
LncRNA usually acts as a regulator of nuclear transcription factors (Wu et al., 2021). An increasing amount of data has shown that long non-coding RNAs (lncRNAs) are associated with the development of cancers (Huang et al., 2021a). EVs containing lncRNA-APC1 inhibited tumor growth in colorectal cancer (CRC). lncRNA-APC1 is an important mediator of APC development through the APC1/RAB5B axis (Wang et al., 2021). The increased expression of lncRNA H19, which is normally regulated by DNA methylation, was observed in numerous cancers (Yang et al., 2021). Previous studies have suggested that EV-contained H19 promotes cell migration and invasion in CRC (Ren et al., 2018). The abnormal expression of XIST, a key factor in the X chromosome inactive (XCI) process, was observed in gastric cancer (Chen et al., 2016; Huang et al., 2021a; Huang et al., 2021b). EV-contained XIST was found to stimulate cell growth in breast cancer (Xing et al., 2018).
To investigate the role of EVs that contained lncRNAs in cancers, appropriate EVs were collected. The EVs were mostly obtained from the cells that were enriched in expressed lncRNA, such as the A549 cell line which exhibited increased H19 expression (Hao et al., 2017). In addition, the EVs were cultured in an environment that encouraged the increased expression of lncRNAs (Born et al., 2020).
EVs Regulate the Expression of miRNA
In contrast to lncRNAs, miRNAs are 20–22 nucleotides long. Both miRNAs and lncRNAs are single-stranded, endogenous RNAs, and play roles in the development of cancers. Some miRNAs, such as let-7a and the miR29 family, are involved in EMT, metastasis, migration, invasion, cell cycle, proliferation, and apoptosis of numerous cancers (Rostas et al., 2014; Song et al., 2020). A few miRNAs have been confirmed to be post-transcriptional regulators for target mRNAs. They can be used as the potential biomarkers for classification, prognosis, chemotherapy, and radiotherapy resistance in triple-negative breast cancer (TNBC) (Ding et al., 2019). Results show that miRNA of EVs have a curing effect on breast cancer (Ohno et al., 2013). MiRNAs can be coated by EVs and delivered to target cells, affect the H19/MAPK/ERK pathways (Ding et al., 2018; Wu et al., 2021).
A database indicated that EVs are enriched in miRNAs, lncRNAs, and proteins (Berardocco et al., 2017). In contrast to transfected mimics or miRNAs inhibitors, EVs that obtained from source cells can specifically and accurately deliver these miRNAs endogenously (Table 2). Considering the characteristics of EVs, therapies using EVs could be a potential approach for cancer treatment.
TABLE 2.
The miRNA of EVs in cancers.
| EVs source | miRNA | Mimics/Inhibitor | Function | Cancer | References |
|---|---|---|---|---|---|
| LIM1863 cells | miR-106b-3p | Mimics | Inhibits cell growth | CRC | Valadi et al. (2007) |
| LIM1863 cells | miR-126–3p | Inhibitor | Inhibits metastasis | Breast cancer | Balaj et al. (2011) |
| LIM1863 cells | miR-126–5p | Mimics | Inhibits EMT | Prostate cancer | Wu et al. (2021) |
| LIM1863 cells | miR-355–3p | Mimics | Inhibits cell growth | CRC | Harding et al. (1983) |
| Urine | FOLH1 | Mimics | Diagnostic | Prostate cancer | Bainton and Farquhar, (1968) |
| Urine | HPN | Mimics | Diagnostic | Prostate cancer | Bainton and Farquhar, (1968) |
| Urine | ITSN1 | Mimics | Diagnostic | Prostate cancer | Bainton and Farquhar, (1968) |
| Urine | CFD miR-21 | Inhibitor | Diagnostic | Prostate cancer | Bainton and Farquhar, (1968) |
| PDAC cell lines | miR-195 | Mimics | Diagnostic | PDAC | Taylor and Gercel-Taylor, (2008) |
| PDAC cell lines | Mimics | Diagnostic | PDAC | Taylor and Gercel-Taylor, (2008) |
EVs Regulate Gene Expression by siRNA
SiRNAs are produced by short, exogenous double-stranded RNAs (dsRNAs) as an RNA interference (RNAi) tool (Kim et al., 2018; Dharamdasani et al., 2020; Feng et al., 2020). SiRNA can be used to effectively silence target genes. A recent study showed that the use of siRNA, such as siRNA-027 can inhibit cell growth and induce apoptosis in numerous cancers (Chen et al., 2020). Hence, siRNA can be used to potentially analyze the development of cancers. A barrier to the RNAi-based therapy of cancers is the low specificity of siRNA delivery. EVs are nano-scale vesicles that can be used to deliver siRNAs as cargos to the target cells by cell-to-cell communication. Previous reports have suggested that the EVs of human plasma cells can deliver siRNA to monocytes and lymphocytes that can silence the expression of mitogen-activated protein kinase 1 (Wahlgren et al., 2012). This suggests that EVs can be used as gene delivery vehicles (GDV) to transport exogenous siRNA in cancer research. Consequently, EVs combined with siRNA are more effective and demonstrate higher specificities than traditionally siRNA delivery in cancer treatment.
EVs Regulate the Expression of Protein
The mitochondrial proteins contained in EVs can promote tumorigenesis by cell-to-cell communication (Al-Nedawi et al., 2008; Demory Beckler et al., 2013). The expression of MET (also known as hepatocyte growth factor receptors) associated with circulating EVs and phosphorylated MET (Tyr1349) was increased in patients with stage 3 and stage 4 melanoma compare to control (Peinado et al., 2012). This finding indicates that EVs can be used to detect the development of cancer (Costa-Silva et al., 2015). This assumption was confirmed when the expression of MIF and GPC-1 proteins in EVs was detected in cancer patients, allowing them to analyze the prognosis of cancer (Melo et al., 2015). Furthermore, phospholipid-binding proteins-carrying EVs can inhibit cell growth and induced apoptosis in numerous cancers (Dhondt et al., 2020). Thus, the proteins contained in EVs were useful for the detection and prognosis of cancers.
The Function of EVs in the Tumor Micro-environment
EVs are a key component of the tumor microenvironment. Tumor heterogeneity includes genomic heterogeneity in both tumor cells and non-cancerous microenvironments. Moreover, the tumor nanoenvironment (TNE) is a special nano-scale tumor microenvironment that possesses complex structures and unique components (Eguchi et al., 2018). The TNE includes EVs and apoptotic bodies. EVs released by tumor cells were absorbed by other cells in the tumor microenvironment, influencing the development of cancer through tumor heterogeneity (Tredan et al., 2007). EVs thus contribute to the formation of the tumor microenvironment in the form of cell-to-cell communication.
Discussion
Considering that EVs can carry any cargos, including nucleic acids and proteins, EVs can thus be used as clinical diagnostic biomarkers. For example, the detection of tumor-specific RNAs in EVs can be used as biomarkers for cancer diagnosis (Gurunathan et al., 2019). Furthermore, proteins contained within EVs such as TSG101, RAS-related protein RAB-11B (RAB11B), CD63, and CD81 can be used as biomarkers for diagnosis of HCCs and other cancers (Möbius et al., 2003; Valadi et al., 2007). In contrast to traditional diagnostic methods such as peripheral blood or histopathology, the accuracy and specificity of EVs were more closely associated with the development of cancers.
EVs can be combined with engineered materials to specifically affect cancer cells. Gold nanoparticles (AuNPs) can mediate photothermal therapy (PPT) to inhibit cell growth and induce cell death (Hu et al., 2020). However, most AuNPs have low specificity. EVs combined with AuNPs can increase their specificity and accelerate the release of their cargos, enhancing the anti-tumor effect of PTT (Nasseri et al., 2020). This could be an important form of therapy for the treatment of cancers in the future. Due to the endogenous nature of EVs, their cargos can escape the immune system and accurately and effectively target tumor cells. In addition, as nano-vesicles, EVs can bypass the blood-brain barrier (Yin et al., 2012). The EVs of immature dendritic cells have been engineered to contain proteins that can target tumors originated from the neuroendothelial and nerve cells in the brain (Federici et al., 2014). Therefore, EVs as nano-vesicles can be used to cross the blood-brain barrier in cancer treatment.
EVs containing anti-cancer drugs, such as therapeutic agents, can be used in the treatment of cancers. In contrast to liposomes, EVs injected in vivo can be absorbed without the interference of the immune system (Ferguson and Nguyen, 2016; Kalluri, 2016; Barile and Vassalli, 2017; Fitts et al., 2019; Liao et al., 2019). Furthermore, EVs are safe and are tolerable in vivo. Recent studies have demonstrated that repeatedly injected mesenchymal cells (MHC) or the IPCs of EVs do not induce toxicity (Zhu et al., 2017; Mendt et al., 2018).
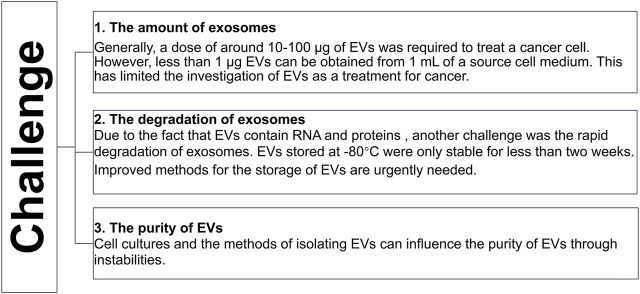
The EVs that carry chemotherapeutics can decide the cell fate by cell-to-cell communication. For example, αv integrin-specific EVs have been shown to have a therapeutic effect on breast cancer (Tian et al., 2014). Another report suggested that paclitaxel surrounding the EVs of macrophages inhibited lung cancer growth in mice (Kim et al., 2016). These reports indicated that chemotherapeutic agent encapsulating EVs have an anti-tumor effect. Recently, studies have shown that the bioavailability of EVs-engineered doxorubicin was improved compared to the free doxorubicin (Tian et al., 2014; Kojima et al., 2018). These studies suggested that as a vesicle, EVs can enhance the efficacy of drugs. Despite the advancements in the understanding of EVs, there are still some challenges that need to be solved (Figure 5).
FIGURE 5.
The challenge of EVs.
Conclusion
EVs are derived from multivesicular bodies formed by intracellular lysosomal particles that are released into the extracellular matrix. The source cells determine the specificity of their EVs. EVs contained RNAs, proteins, and drugs that can play important roles in the development of cancers. EVs have the ability to decide the fate of cells by cell-to-cell communication. EVs have potential applications in anti-cancer treatments in the future.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Funding
This work was supported by the Jilin Health Commission Program under Grant 2020J05S, the Fundamental Research Funds for the Central Universities under Grant 2019JCKT-70, the Jilin Education Department Program under Grant JJKH20200950KJ, and the Jilin Scientific and Technological Development Program under Grant 20190103071JH, 202002006JC, 20210101010JC, and 2020041.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Ahmed S. H., Espinoza-Sánchez N. A., El-Damen A., Fahim S. A., Badawy M. A., Greve B., et al. (2021). Small Extracellular Vesicle-Encapsulated miR-181b-5p, miR-222-3p and Let-7a-5p: Next Generation Plasma Biopsy-Based Diagnostic Biomarkers for Inflammatory Breast Cancer. PLoS One 16, e0250642. 10.1371/journal.pone.0250642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Nedawi K., Meehan B., Micallef J., Lhotak V., May L., Guha A., et al. (2008). Intercellular Transfer of the Oncogenic Receptor EGFRvIII by Microvesicles Derived from Tumour Cells. Nat. Cel Biol 10, 619–624. 10.1038/ncb1725 [DOI] [PubMed] [Google Scholar]
- Bainton D. F., Farquhar M. G. (1968). Differences in Enzyme Content of Azurophil and Specific Granules of Polymorphonuclear Leukocytes. J. Cel Biol 39, 299–317. 10.1083/jcb.39.2.299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balaj L., Lessard R., Dai L., Cho Y.-J., Pomeroy S. L., Breakefield X. O., et al. (2011). Tumour Microvesicles Contain Retrotransposon Elements and Amplified Oncogene Sequences. Nat. Commun. 2, 180. 10.1038/ncomms1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barile L., Vassalli G. (2017). Exosomes: Therapy Delivery Tools and Biomarkers of Diseases. Pharmacol. Ther. 174, 63–78. 10.1016/j.pharmthera.2017.02.020 [DOI] [PubMed] [Google Scholar]
- Berardocco M., Radeghieri A., Busatto S., Gallorini M., Raggi C., Gissi C., et al. (2017). RNA-seq Reveals Distinctive RNA Profiles of Small Extracellular Vesicles from Different Human Liver Cancer Cell Lines. Oncotarget 8, 82920–82939. 10.18632/oncotarget.20503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Born L. J., Harmon J. W., Jay S. M. (2020). Therapeutic Potential of Extracellular Vesicle-Associated Long Noncoding RNA. Bioeng. Transl Med. 5, e10172. 10.1002/btm2.10172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J. J., Tay Y. (2018). Noncoding RNA:RNA Regulatory Networks in Cancer. Int. J. Mol. Sci. 19. 10.3390/ijms19051310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D.-l., Ju H.-q., Lu Y.-x., Chen L.-z., Zeng Z.-l., Zhang D.-s., et al. (2016). Long Non-coding RNA XIST Regulates Gastric Cancer Progression by Acting as a Molecular Sponge of miR-101 to Modulate EZH2 Expression. J. Exp. Clin. Cancer Res. 35, 142. 10.1186/s13046-016-0420-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z., Krishnamachary B., Pachecho-Torres J., Penet M. F., Bhujwalla Z. M. (2020). Theranostic Small Interfering RNA Nanoparticles in Cancer Precision Nanomedicine. Wiley Interdiscip. Rev. Nanomed Nanobiotechnol 12, e1595. 10.1002/wnan.1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa-Silva B., Aiello N. M., Ocean A. J., Singh S., Zhang H., Thakur B. K., et al. (2015). Pancreatic Cancer Exosomes Initiate Pre-metastatic Niche Formation in the Liver. Nat. Cel Biol 17, 816–826. 10.1038/ncb3169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demory Beckler M., Higginbotham J. N., Franklin J. L., Ham A.-J., Halvey P. J., Imasuen I. E., et al. (2013). Proteomic Analysis of Exosomes from Mutant KRAS colon Cancer Cells Identifies Intercellular Transfer of Mutant KRAS. Mol. Cell Proteomics 12, 343–355. 10.1074/mcp.m112.022806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharamdasani V., Mandal A., Qi Q. M., Suzuki I., Bentley M. V. L. B., Mitragotri S. (2020). Topical Delivery of siRNA into Skin Using Ionic Liquids. J. Controlled Release 323, 475–482. 10.1016/j.jconrel.2020.04.038 [DOI] [PubMed] [Google Scholar]
- Dhondt B., Geeurickx E., Tulkens J., Van Deun J., Vergauwen G., Lippens L., et al. (2020). Unravelling the Proteomic Landscape of Extracellular Vesicles in Prostate Cancer by Density‐based Fractionation of Urine. J. Extracellular Vesicles 9, 1736935. 10.1080/20013078.2020.1736935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding K., Liao Y., Gong D., Zhao X., Ji W. (2018). Effect of Long Non-coding RNA H19 on Oxidative Stress and Chemotherapy Resistance of CD133+ Cancer Stem Cells via the MAPK/ERK Signaling Pathway in Hepatocellular Carcinoma. Biochem. Biophysical Res. Commun. 502, 194–201. 10.1016/j.bbrc.2018.05.143 [DOI] [PubMed] [Google Scholar]
- Ding L., Gu H., Xiong X., Ao H., Cao J., Lin W., et al. (2019). MicroRNAs Involved in Carcinogenesis, Prognosis, Therapeutic Resistance and Applications in Human Triple-Negative Breast Cancer. Cells 8, 492. 10.3390/cells8121492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draganov D. D., Santidrian A. F., Minev I., Nguyen D., Kilinc M. O., Petrov I., et al. (2019). Delivery of Oncolytic Vaccinia Virus by Matched Allogeneic Stem Cells Overcomes Critical Innate and Adaptive Immune Barriers. J. Transl Med. 17, 100. 10.1186/s12967-019-1829-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzobo K., Senthebane D. A., Ganz C., Thomford N. E., Wonkam A., Dandara C. (2020). Advances in Therapeutic Targeting of Cancer Stem Cells within the Tumor Microenvironment: An Updated Review. Cells 9, 896. 10.3390/cells9081896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eguchi T., Sogawa C., Okusha Y., Uchibe K., Iinuma R., Ono K., et al. (2018). Organoids with Cancer Stem Cell-like Properties Secrete Exosomes and HSP90 in a 3D Nanoenvironment. PLoS One 13, e0191109. 10.1371/journal.pone.0191109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federici C., Petrucci F., Caimi S., Cesolini A., Logozzi M., Borghi M., et al. (2014). Exosome Release and Low pH Belong to a Framework of Resistance of Human Melanoma Cells to Cisplatin. PLoS One 9, e88193. 10.1371/journal.pone.0088193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng J., Yu W., Xu Z., Hu J., Liu J., Wang F. (2020). Multifunctional siRNA-Laden Hybrid Nanoplatform for Noninvasive PA/IR Dual-Modal Imaging-Guided Enhanced Photogenetherapy. ACS Appl. Mater. Inter. 12, 22613–22623. 10.1021/acsami.0c04533 [DOI] [PubMed] [Google Scholar]
- Ferguson S. W., Nguyen J. (2016). Exosomes as Therapeutics: The Implications of Molecular Composition and Exosomal Heterogeneity. J. Controlled Release 228, 179–190. 10.1016/j.jconrel.2016.02.037 [DOI] [PubMed] [Google Scholar]
- Fernández P. L., Hernández L., Farré X., Campo E., Cardesa A. (2002). Alterations of Cell Cycle-Regulatory Genes in Prostate Cancer. Pathobiology 70, 1–10. 10.1159/000065998 [DOI] [PubMed] [Google Scholar]
- Fitts C. A., Ji N., Li Y., Tan C. (2019). Exploiting Exosomes in Cancer Liquid Biopsies and Drug Delivery. Adv. Healthc. Mater. 8, e1801268. 10.1002/adhm.201801268 [DOI] [PubMed] [Google Scholar]
- Gurunathan S., Kang M. H., Jeyaraj M., Qasim M., Kim J. H. (2019). Review of the Isolation, Characterization, Biological Function, and Multifarious Therapeutic Approaches of Exosomes. Cells 8, 307. 10.3390/cells8040307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gusachenko O. N., Zenkova M. A., Vlassov V. V. (2013). Nucleic Acids in Exosomes: Disease Markers and Intercellular Communication Molecules. Biochem. Mosc. 78, 1–7. 10.1134/s000629791301001x [DOI] [PubMed] [Google Scholar]
- Hao Y., Wang G., Lin C., Li D., Ji Z., Gao F., et al. (2017). Valproic Acid Induces Decreased Expression of H19 Promoting Cell Apoptosis in A549 Cells. DNA Cel Biol. 36, 428–435. 10.1089/dna.2016.3542 [DOI] [PubMed] [Google Scholar]
- Harding C., Heuser J., Stahl P. (1983). Receptor-mediated Endocytosis of Transferrin and Recycling of the Transferrin Receptor in Rat Reticulocytes. J. Cel Biol 97, 329–339. 10.1083/jcb.97.2.329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu X., Zhang Y., Ding T., Liu J., Zhao H. (2020). Multifunctional Gold Nanoparticles: A Novel Nanomaterial for Various Medical Applications and Biological Activities. Front. Bioeng. Biotechnol. 8, 990. 10.3389/fbioe.2020.00990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W., Yan Y., Liu Y., Lin M., Ma J., Zhang W., et al. (2020). Exosomes with Low miR-34c-3p Expression Promote Invasion and Migration of Non-small Cell Lung Cancer by Upregulating Integrin α2β1. Signal. Transduct Target. Ther. 5, 39. 10.1038/s41392-020-0133-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Yuan K., Tang M., Yue J., Bao L., Wu S., et al. (2021). Melatonin Inhibiting the Survival of Human Gastric Cancer Cells under ER Stress Involving Autophagy and Ras‐Raf‐MAPK Signalling. J. Cel Mol Med 25, 1480–1492. 10.1111/jcmm.16237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhou Z., Zhang J., Hao Z., He Y., Wu Z., et al. (2021). lncRNA MALAT1 Participates in Metformin Inhibiting the Proliferation of Breast Cancer Cell. J. Cel Mol Med 25, 7135–7145. 10.1111/jcmm.16742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahlert C., Kalluri R. (2013). Exosomes in Tumor Microenvironment Influence Cancer Progression and Metastasis. J. Mol. Med. 91, 431–437. 10.1007/s00109-013-1020-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahlert C., Melo S. A., Protopopov A., Tang J., Seth S., Koch M., et al. (2014). Identification of Double-Stranded Genomic DNA Spanning All Chromosomes with Mutated KRAS and P53 DNA in the Serum Exosomes of Patients with Pancreatic Cancer. J. Biol. Chem. 289, 3869–3875. 10.1074/jbc.c113.532267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri R. (2016). The Biology and Function of Exosomes in Cancer. J. Clin. Invest. 126, 1208–1215. 10.1172/jci81135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H. J., Yi Y., Kim A., Miyata K. (2018). Small Delivery Vehicles of siRNA for Enhanced Cancer Targeting. Biomacromolecules 19, 2377–2390. 10.1021/acs.biomac.8b00546 [DOI] [PubMed] [Google Scholar]
- Kim M. S., Haney M. J., Zhao Y., Mahajan V., Deygen I., Klyachko N. L., et al. (2016). Development of Exosome-Encapsulated Paclitaxel to Overcome MDR in Cancer Cells. Nanomedicine: Nanotechnology, Biol. Med. 12, 655–664. 10.1016/j.nano.2015.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kojima R., Bojar D., Rizzi G., Hamri G. C.-E., El-Baba M. D., Saxena P., et al. (2018). Designer Exosomes Produced by Implanted Cells Intracerebrally Deliver Therapeutic Cargo for Parkinson's Disease Treatment. Nat. Commun. 9, 1305. 10.1038/s41467-018-03733-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowal J., Arras G., Colombo M., Jouve M., Morath J. P., Primdal-Bengtson B., et al. (2016). Proteomic Comparison Defines Novel Markers to Characterize Heterogeneous Populations of Extracellular Vesicle Subtypes. Proc. Natl. Acad. Sci. USA 113, E968–E977. 10.1073/pnas.1521230113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Li Z., Jiang P., Peng M., Zhang X., Chen K., et al. (2018). Circular RNA IARS (Circ-IARS) Secreted by Pancreatic Cancer Cells and Located within Exosomes Regulates Endothelial Monolayer Permeability to Promote Tumor Metastasis. J. Exp. Clin. Cancer Res. 37, 177. 10.1186/s13046-018-0822-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao W., Du Y., Zhang C., Pan F., Yao Y., Zhang T., et al. (2019). Exosomes: The Next Generation of Endogenous Nanomaterials for Advanced Drug Delivery and Therapy. Acta Biomater. 86, 1–14. 10.1016/j.actbio.2018.12.045 [DOI] [PubMed] [Google Scholar]
- Lu L., Luo F., Liu Y., Liu X., Shi L., Lu X., et al. (2015). Posttranscriptional Silencing of the lncRNA MALAT1 by miR-217 Inhibits the Epithelial-Mesenchymal Transition via Enhancer of Zeste Homolog 2 in the Malignant Transformation of HBE Cells Induced by Cigarette Smoke Extract. Toxicol. Appl. Pharmacol. 289, 276–285. 10.1016/j.taap.2015.09.016 [DOI] [PubMed] [Google Scholar]
- Luna J., Boni J., Cuatrecasas M., Bofill-De Ros X., Núñez-Manchón E., Gironella M., et al. (2019). DYRK1A Modulates C-MET in Pancreatic Ductal Adenocarcinoma to Drive Tumour Growth. Gut 68, 1465–1476. 10.1136/gutjnl-2018-316128 [DOI] [PubMed] [Google Scholar]
- Melo S. A., Luecke L. B., Kahlert C., Fernandez A. F., Gammon S. T., Kaye J., et al. (2015). Glypican-1 Identifies Cancer Exosomes and Detects Early Pancreatic Cancer. Nature 523, 177–182. 10.1038/nature14581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melo S. A., Sugimoto H., O’Connell J. T., Kato N., Villanueva A., Vidal A., et al. (2014). Cancer Exosomes Perform Cell-independent microRNA Biogenesis and Promote Tumorigenesis. Cancer Cell 26, 707–721. 10.1016/j.ccell.2014.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendt M., Kamerkar S., Sugimoto H., McAndrews K. M., Wu C. C., Gagea M., et al. (2018). Generation and Testing of Clinical-Grade Exosomes for Pancreatic Cancer. JCI Insight 3, e99263. 10.1172/jci.insight.99263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Möbius W., van Donselaar E., Ohno-Iwashita Y., Shimada Y., Heijnen H. F. G., Slot J. W., et al. (2003). Recycling Compartments and the Internal Vesicles of Multivesicular Bodies Harbor Most of the Cholesterol Found in the Endocytic Pathway. Traffic 4, 222–231. 10.1034/j.1600-0854.2003.00072.x [DOI] [PubMed] [Google Scholar]
- Nasseri B., Turk M., Kosemehmetoglu K., Kaya M., Pişkin E., Rabiee N., et al. (2020). The Pimpled Gold Nanosphere: A Superior Candidate for Plasmonic Photothermal Therapy. Ijn Vol. 15, 2903–2920. 10.2147/ijn.s248327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohno S.-i., Takanashi M., Sudo K., Ueda S., Ishikawa A., Matsuyama N., et al. (2013). Systemically Injected Exosomes Targeted to EGFR Deliver Antitumor MicroRNA to Breast Cancer Cells. Mol. Ther. 21, 185–191. 10.1038/mt.2012.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan B. T., Teng K., Wu C., Adam M., Johnstone R. M. (1985). Electron Microscopic Evidence for Externalization of the Transferrin Receptor in Vesicular Form in Sheep Reticulocytes. J. Cel Biol 101, 942–948. 10.1083/jcb.101.3.942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlyukov M. S., Yu H., Bastola S., Minata M., Shender V. O., Lee Y., et al. (2018). Apoptotic Cell-Derived Extracellular Vesicles Promote Malignancy of Glioblastoma via Intercellular Transfer of Splicing Factors. Cancer Cell 34, 119–135. 10.1016/j.ccell.2018.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peinado H., Alečković M., Lavotshkin S., Matei I., Costa-Silva B., Moreno-Bueno G., et al. (2012). Melanoma Exosomes Educate Bone Marrow Progenitor Cells toward a Pro-metastatic Phenotype through MET. Nat. Med. 18, 883–891. 10.1038/nm.2753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perin E. C., Silva G. V., Henry T. D., Cabreira-Hansen M. G., Moore W. H., Coulter S. A., et al. (2011). A Randomized Study of Transendocardial Injection of Autologous Bone Marrow Mononuclear Cells and Cell Function Analysis in Ischemic Heart Failure (FOCUS-HF). Am. Heart J. 161, 1078–1087. 10.1016/j.ahj.2011.01.028 [DOI] [PubMed] [Google Scholar]
- Ramírez-Ricardo J., Leal-Orta E., Martínez-Baeza E., Ortiz-Mendoza C., Breton-Mora F., Herrera-Torres A., et al. (2020). Circulating Extracellular Vesicles from Patients with Breast Cancer Enhance Migration and Invasion via a Src-dependent P-athway in MDA-MB-231 B-reast C-ancer C-ells. Mol. Med. Rep. 22, 1932–1948. 10.3892/mmr.2020.11259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raposo G., Stoorvogel W. (2013). Extracellular Vesicles: Exosomes, Microvesicles, and Friends. J. Cel Biol 200, 373–383. 10.1083/jcb.201211138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren J., Ding L., Zhang D., Shi G., Xu Q., Shen S., et al. (2018). Carcinoma-associated Fibroblasts Promote the Stemness and Chemoresistance of Colorectal Cancer by Transferring Exosomal lncRNA H19. Theranostics 8, 3932–3948. 10.7150/thno.25541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rostas J. W., 3rd, Pruitt H. C., Metge B. J., Mitra A., Bailey S. K., Bae S., et al. (2014). microRNA-29 Negatively Regulates EMT Regulator N-Myc Interactor in Breast Cancer. Mol. Cancer 13, 200. 10.1186/1476-4598-13-200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi X., Zhang Y., Zheng J., Pan J. (2012). Reactive Oxygen Species in Cancer Stem Cells. Antioxid. Redox Signaling 16, 1215–1228. 10.1089/ars.2012.4529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva A. M., Lazaro-Ibanez E., Gunnarsson A., Dhande A., Daaboul G., Peacock B., et al. (2021). Quantification of Protein Cargo Loading into Engineered Extracellular Vesicles at Single-Vesicle and Single-Molecule Resolution. J. Extracellular Vesicles 10, e12130. 10.1002/jev2.12130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slomka A., Mocan T., Wang B., Nenu I., Urban S. K., Gonzales-Carmona M., et al. (2020). EVs as Potential New Therapeutic Tool/Target in Gastrointestinal Cancer and HCC. Cancers (Basel) 12, 3019. 10.3390/cancers12103019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song X., Liang Y., Sang Y., Li Y., Zhang H., Chen B., et al. (2020). circHMCU Promotes Proliferation and Metastasis of Breast Cancer by Sponging the Let-7 Family. Mol. Ther. - Nucleic Acids 20, 518–533. 10.1016/j.omtn.2020.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su C. Y., Zhang J. Y., Yarden Y., Fu L. W. (2021). The Key Roles of Cancer Stem Cell-Derived Extracellular Vesicles. Signal. Transduct Tar 6, 109. 10.1038/s41392-021-00499-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor D. D., Gercel-Taylor C. (2008). MicroRNA Signatures of Tumor-Derived Exosomes as Diagnostic Biomarkers of Ovarian Cancer. Gynecol. Oncol. 110, 13–21. 10.1016/j.ygyno.2008.04.033 [DOI] [PubMed] [Google Scholar]
- Théry C., Zitvogel L., Amigorena S. (2002). Exosomes: Composition, Biogenesis and Function. Nat. Rev. Immunol. 2, 569–579. 10.1038/nri855 [DOI] [PubMed] [Google Scholar]
- Tian L., Cao J., Jiao H., Zhang J., Ren X., Liu X., et al. (2019). CircRASSF2 Promotes Laryngeal Squamous Cell Carcinoma Progression by Regulating the miR-302b-3p/IGF-1R axis. Clin. Sci. (Lond) 133, 1053–1066. 10.1042/cs20190110 [DOI] [PubMed] [Google Scholar]
- Tian Y., Li S., Song J., Ji T., Zhu M., Anderson G. J., et al. (2014). A Doxorubicin Delivery Platform Using Engineered Natural Membrane Vesicle Exosomes for Targeted Tumor Therapy. Biomaterials 35, 2383–2390. 10.1016/j.biomaterials.2013.11.083 [DOI] [PubMed] [Google Scholar]
- Tredan O., Galmarini C. M., Patel K., Tannock I. F. (2007). Drug Resistance and the Solid Tumor Microenvironment. JNCI J. Natl. Cancer Inst. 99, 1441–1454. 10.1093/jnci/djm135 [DOI] [PubMed] [Google Scholar]
- Valadi H., Ekström K., Bossios A., Sjöstrand M., Lee J. J., Lötvall J. O. (2007). Exosome-mediated Transfer of mRNAs and microRNAs Is a Novel Mechanism of Genetic Exchange between Cells. Nat. Cel Biol 9, 654–659. 10.1038/ncb1596 [DOI] [PubMed] [Google Scholar]
- Wahlgren J., Karlson T. D. L., Brisslert M., Vaziri Sani F., Telemo E., Sunnerhagen P., et al. (2012). Plasma Exosomes Can Deliver Exogenous Short Interfering RNA to Monocytes and Lymphocytes. Nucleic Acids Res. 40, e130. 10.1093/nar/gks463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F. W., Cao C. H., Han K., Zhao Y. X., Cai M. Y., Xiang Z. C., et al. (2021). APC-activated Long Noncoding RNA Inhibits Colorectal Carcinoma Pathogenesis through Reduction of Exosome Production. J. Clin. Invest. 131, e149666. 10.1172/jci149666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Liu W., Zou Y., Wang G., Deng Y., Luo J., et al. (2019). Three Isoforms of Exosomal circPTGR1 Promote Hepatocellular Carcinoma Metastasis via the miR449a-MET Pathway. EBioMedicine 40, 432–445. 10.1016/j.ebiom.2018.12.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Zhang Q., Zhou S., Xu H., Wang D., Feng J., et al. (2019). Circular RNA Expression in Exosomes Derived from Breast Cancer Cells and Patients. Epigenomics 11, 411–421. 10.2217/epi-2018-0111 [DOI] [PubMed] [Google Scholar]
- Wang X., Qiao D., Chen L., Xu M., Chen S., Huang L., et al. (2019). Chemotherapeutic Drugs Stimulate the Release and Recycling of Extracellular Vesicles to Assist Cancer Cells in Developing an Urgent Chemoresistance. Mol. Cancer 18, 182. 10.1186/s12943-019-1114-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S., Li T. Y., Liu W. W., Huang Y. Y. (2021). Ferroptosis and Cancer: Complex Relationship and Potential Application of Exosomes. Front Cel Dev Biol 9, 733751. 10.3389/fcell.2021.733751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xi X. j., Zeng J. j., Lu Y., Chen S. h., Jiang Z. w., He P. j., et al. (2020). Extracellular Vesicles Enhance Oxidative Stress through P38/NF‐kB Pathway in Ketamine‐induced Ulcerative Cystitis. J. Cel Mol Med 24, 7609–7624. 10.1111/jcmm.15397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing F., Liu Y., Wu S.-Y., Wu K., Sharma S., Mo Y.-Y., et al. (2018). Loss of XIST in Breast Cancer Activates MSN-C-Met and Reprograms Microglia via Exosomal miRNA to Promote Brain Metastasis. Cancer Res. 78, 4316–4330. 10.1158/0008-5472.can-18-1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Xia F., Ma L., Shan J., Shen J., Yang Z., et al. (2011). MicroRNA-122 Sensitizes HCC Cancer Cells to Adriamycin and Vincristine through Modulating Expression of MDR and Inducing Cell Cycle Arrest. Cancer Lett. 310, 160–169. 10.1016/j.canlet.2011.06.027 [DOI] [PubMed] [Google Scholar]
- Xue J., Liu Y., Luo F., Lu X., Xu H., Liu X., et al. (2017). Circ100284, via miR-217 Regulation of EZH2, Is Involved in the Arsenite-Accelerated Cell Cycle of Human Keratinocytes in Carcinogenesis. Biochim. Biophys. Acta (Bba) - Mol. Basis Dis. 1863, 753–763. 10.1016/j.bbadis.2016.12.018 [DOI] [PubMed] [Google Scholar]
- Yang J., Qi M., Fei X., Wang X., Wang K. (2021). LncRNA H19: A Novel Oncogene in Multiple Cancers. Int. J. Biol. Sci. 17, 3188–3208. 10.7150/ijbs.62573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin J., Yan X., Yao X., Zhang Y., Shan Y., Mao N., et al. (2012). Secretion of Annexin A3 from Ovarian Cancer Cells and its Association with Platinum Resistance in Ovarian Cancer Patients. J. Cel Mol Med 16, 337–348. 10.1111/j.1582-4934.2011.01316.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Wang S., Wang H., Cao J., Huang X., Chen Z., et al. (2019). Circular RNA circNRIP1 Acts as a microRNA-149-5p Sponge to Promote Gastric Cancer Progression via the AKT1/mTOR Pathway. Mol. Cancer 18, 20. 10.1186/s12943-018-0935-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X., Badawi M., Pomeroy S., Sutaria D. S., Xie Z., Baek A., et al. (2017). Comprehensive Toxicity and Immunogenicity Studies Reveal Minimal Effects in Mice Following Sustained Dosing of Extracellular Vesicles Derived from HEK293T Cells. J. Extracellular Vesicles 6, 1324730. 10.1080/20013078.2017.1324730 [DOI] [PMC free article] [PubMed] [Google Scholar]