Abstract
This cohort study assesses the rate of telemedicine visits according to the socioeconomic status of patients with a new cancer diagnosis.
The COVID-19 pandemic led to a decline of in-person clinical visits.1 Telemedicine increased during this time, but there was lower uptake in high-poverty areas.2 For patients newly diagnosed with cancer, a delay in care could cause irreversible harm; therefore these patients may be especially motivated to use telemedicine to keep health care appointments during the pandemic. The present study uses data from a large commercial insurer to examine the uptake of telemedicine visits among patients with newly diagnosed cancer, with a specific focus on assessing differential uptake by socioeconomic status (SES).
Methods
The HealthCore Integrated Research Database comprises single-payer administrative claims data for approximately 60 million individuals enrolled in Medicare Advantage and commercial health plans.3 Data on race and ethnicity were not available in the claims data set used in this analysis. The University of Kansas Institutional Review Board deemed this study exempt from review and patient informed consent requirements because only deidentified claims data were used.
Using the claims data, we identified patients with newly diagnosed breast (women only), lung, prostate, and colorectal cancer between January 1 and August 31, 2020. For each month, we first identified enrollees aged 18 years or older with at least 2 years of continuous enrollment prior to the first date of the month of interest (index month) and no medical claims with International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis or personal history codes for the cancer of interest during the 2 years preceding the index month (1 year for lung cancer because of its more aggressive nature and the lower likelihood of including prevalent cases with a 1 year look-back period). Enrollees meeting these criteria were evaluated for newly diagnosed cancer, defined as the presence of 1 or more medical claims with an ICD-10-CM diagnosis code for the cancer of interest (eTable in the Supplement), during the index month.
The primary outcome was receipt of a telemedicine visit within 30 days of cancer diagnosis, which was ascertained by the presence of 1 or more claims with Current Procedural Terminology or Healthcare Common Procedure Coding Systems codes for telemedicine services (eTable in the Supplement). The monthly proportion of patients who received such services was computed along with a Wilson score 95% CI. The SES index score was calculated using 7 area-level social determinants of health variables, as developed by the Agency for Healthcare Research and Quality,4 and analyzed as quartiles. Multivariable Poisson regression models were used to assess the association between SES index quartile and telemedicine visit, while controlling for age group, geographic region, cancer type, and Charlson Comorbidity Index score. All analyses were conducted using SAS, version 9.4 (SAS Institute) and Excel, version 16.0 (Microsoft Corporation).
Results
Among 16 006 newly diagnosed patients (8483 were men [53%] and 7523 were women [47%]; 8115 [50.7%] were aged 18-64 years and 7891 [49.3%] were aged ≥65 years), the rate of telemedicine visits increased from 0.4% in January 2020 and peaked in April 2020 (54.0%), and patterns of uptake differed by SES (Figure). By April 2020, 66.9% of patients in the highest SES index quartile had a telemedicine visit within 30 days of cancer diagnosis compared with 47.4% to 48.6% in the lower SES index quartiles. Patients in the highest SES index quartile (ie, quartile 4) maintained the highest rate of telemedicine use in every subsequent month. Multivariable analysis confirmed differences in telemedicine use by SES and showed differences by age group, cancer type, comorbidities, and geographic region (Table). For example, patients in the highest SES index quartile had a 31% higher risk of telemedicine use within 30 days of cancer diagnosis compared with patients in the lowest SES index quartile (risk ratio [RR] = 1.31; 95% CI, 1.17 to 1.47). Additional multivariable models confirmed statistically significant differences by SES each month from March to July 2020. For example, relative RRs comparing the use of telemedicine within 30 days of cancer diagnosis between patients in the highest SES index quartile vs those in the lowest SES index quartile were 1.29 (95% CI, 1.01 to 1.66) in March 2020 and 1.59 (95% CI, 1.18 to 2.15) in July 2020.
Figure. Monthly Proportion of Patients With a Telemedicine Visit Within 30 Days of Cancer Diagnosis by Socioeconomic Status Quartile in 2020.
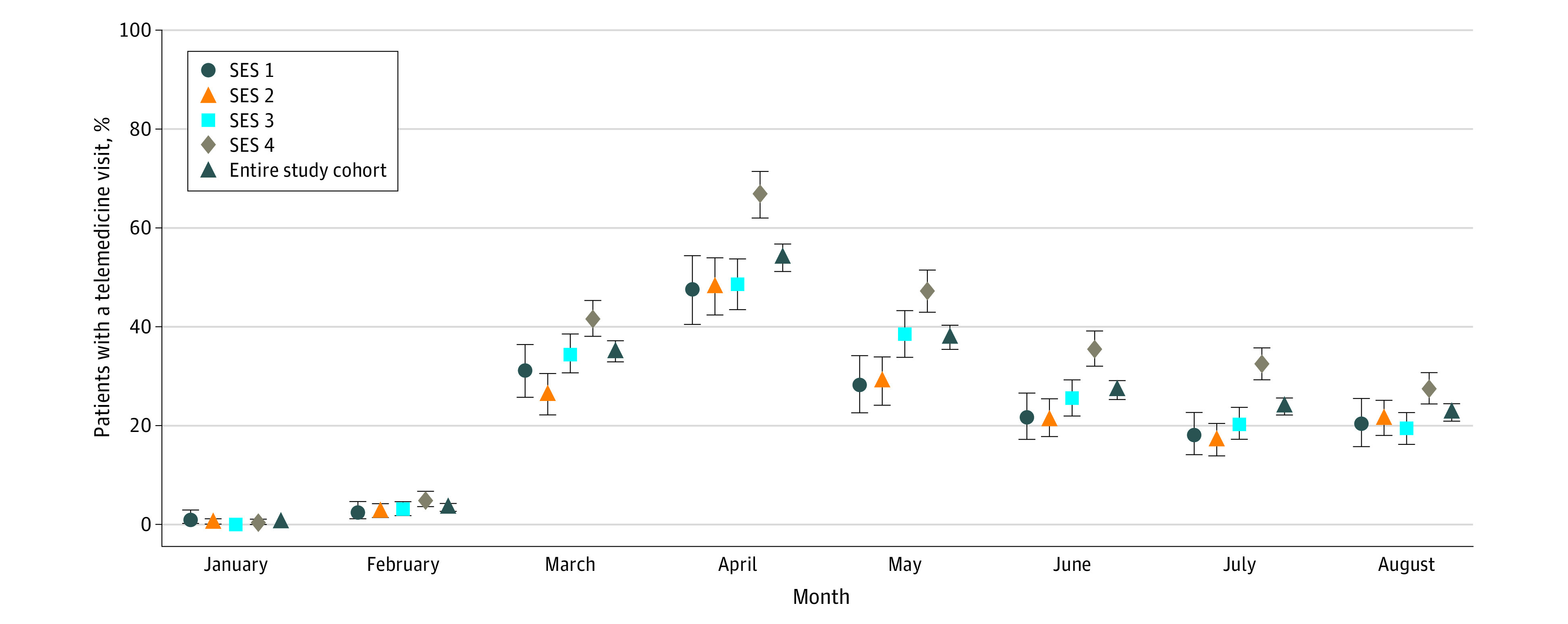
The lowest socioeconomic status (SES) quartile is SES 1, and SES 4 is the highest quartile. Error bars represent the 95% Wilson score CIs for the proportions.
Table. Multivariable-Adjusted Relative Difference in Proportions of Patients Who Had a Telemedicine Visit Within 30 Days of Cancer Diagnosis in 2020 .
| Variable | Risk Ratio (95% CI) |
|---|---|
| SES index quartile | |
| 1 (lowest) | [Reference] |
| 2 | 0.94 (0.83-1.07) |
| 3 | 1.06 (0.94-1.19) |
| 4 (highest) | 1.31 (1.17-1.47) |
| Age group, y | |
| 18-64 | [Reference] |
| ≥65 | 0.89 (0.83-0.95) |
| Cancer type | |
| Breast | [Reference] |
| Colorectal | 0.96 (0.86-1.07) |
| Lung | 1.24 (1.13-1.37) |
| Prostate | 1.01 (0.92-1.10) |
| Charlson Comorbidity Index score | |
| 0 | [Reference] |
| 1 | 1.05 (0.95-1.16) |
| 2 | 1.04 (0.92-1.16) |
| ≥3 | 1.26 (1.15-1.38) |
| Region | |
| Northeast | [Reference] |
| Midwest | 0.74 (0.66-0.82) |
| South | 0.72 (0.64-0.80) |
| West | 1.13 (1.02-1.25) |
Abbreviation: SES, socioeconomic status.
Discussion
Disparities in cancer care and the resulting outcomes have been well described before the COVID-19 pandemic. Development of telemedicine capabilities has the potential to reduce these disparities by increasing access to consultations, second opinions, and follow-up visits. Yet the findings of the present study suggest that development of telemedicine capabilities is insufficient to reduce and, in fact, may widen disparities. We acknowledge that this study is limited in that disparities in telemedicine use may be attributable to patient preferences for in-person vs telemedicine visits rather than disparities in oncologic care. Differences in telemedicine use may also be attributable to patient access to and comfort with the technological requirements of telemedicine.5 Published studies have found that telemedicine can improve access to health care services, including specialized care, and can provide patient satisfaction comparable to in-person visits.6 Future implementation of new care delivery methods must have equitable access at its core.
eTable. ICD-10-CM, CPT, and HCPCS Codes Used in This Study to Identify Individuals With Cancer and Use of Telemedicine
References
- 1.Uscher-Pines L, Sousa J, Jones M, et al. Telehealth use among safety-net organizations in California during the COVID-19 pandemic. JAMA. 2021;325(11):1106-1107. doi: 10.1001/jama.2021.0282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff (Millwood). 2021;40(2):349-358. doi: 10.1377/hlthaff.2020.01786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NIH Collaboratory Distributed Research Network . HealthCore data description: rethinking clinical trials. April 4, 2018. Accessed August 30, 2021. https://rethinkingclinicaltrials.org/nih-collaboratory-drn/healthcore/
- 4.Bonito A, Bann C, Eicheldinger C, Carpenter L. Creation of new race-ethnicity codes and socioeconomic status (SES) indicators for Medicare beneficiaries. Agency for Healthcare Research and Quality. Published January 2008. Accessed March 24, 2021. https://archive.ahrq.gov/research/findings/final-reports/medicareindicators/medicareindicators1.html
- 5.Royce TJ, Sanoff HK, Rewari A. Telemedicine for cancer care in the time of COVID-19. JAMA Oncol. 2020;6(11):1698-1699. doi: 10.1001/jamaoncol.2020.2684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha Z, Schapira RM, Laud PW, McNutt G, Roter DL. Patient satisfaction with physician-patient communication during telemedicine. Telemed J E Health. 2009;15(9):830-839. doi: 10.1089/tmj.2009.0030 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. ICD-10-CM, CPT, and HCPCS Codes Used in This Study to Identify Individuals With Cancer and Use of Telemedicine


