Abstract
The coronavirus disease 2019 (COVID-19) pandemic has generated many challenges for physicians, including multiple post-covid long-term effects that are still being studied. We report a case of patient who developed a retropharyngeal abscess with a concomitant viral pneumonia resembling Covid and its management.
Keywords: COVID 19, SARS-CoV-2, Abscess, Retropharyngeal, Diabetes
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been a major topic of discussion around the world since it was first identified in Wuhan, China. While most patients with COVID-19 are asymptomatic or suffer minor morbidity, a significant number of patients experience life-threatening symptoms including acute respiratory distress syndrome (ARDS) and multi-organ failure [1]. We report a case of deep neck abscess in a patient with a COVID-19 like viral pneumonia.
Case Report
A 60 year old diabetic and hypertensive male who was also a smoker and alcoholic presented to our hospital with history of dysphagia and odynophagia since 4 days. He also complained of difficulty in breathing and a swelling involving the submental region since 2 days. There was no history of fever, cough, dental caries, foreign body, trauma or upper respiratory infection. On examination he had a hypo nasal voice with drooling of saliva, trismus and grade one stridor. Chest auscultation was normal and he maintained an oxygen saturation of 95%. A diffuse swelling was noted in the submental region extending upto the upper border of thyroid cartilage. Due to the trismus a laryngoscopic examination was not feasible and the patient was planned for emergency tracheostomy and incision and drainage of the submental abscess. His blood investigations revealed neutrophilic leukocytosis and uncontrolled sugars for which the patient was put on a sliding scale of insulin. The patient’s Covid—RTPCR (Reverse transcription-Polymerase) test was negative.
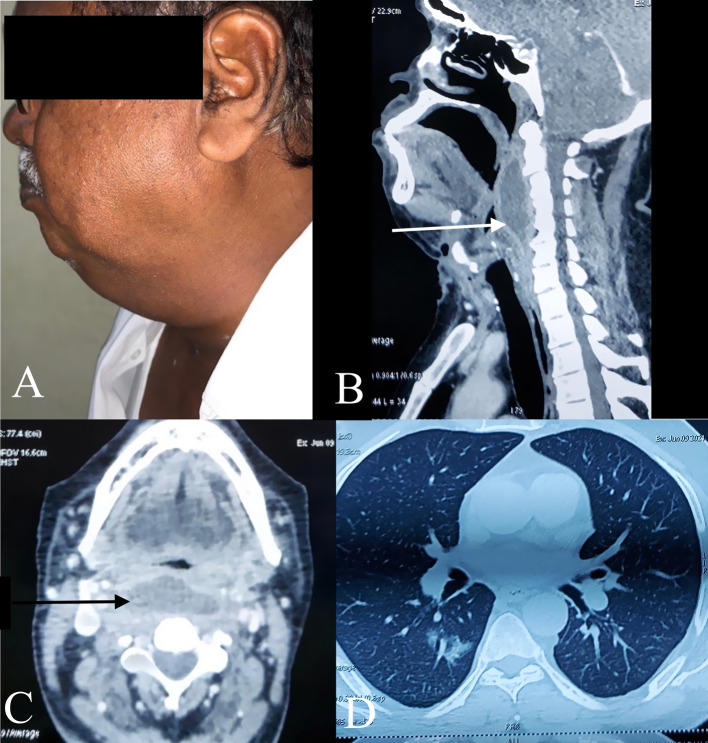
Following Covid precautions the patient underwent an emergency tracheostomy followed by incision of the submental abscess and 15 ml of pus was drained. Postoperatively despite management of the patient with intravenous antibiotics and strict glycemic control, pus was constantly draining from the incision site, his oxygen saturation continued to be 95% and patient’s dysphagia and hyponasal voice persisted. A Flexible fibreoptic laryngoscopy showed a mucosa covered bulge in the oropharynx extending till the level of arytenoids. With a high index of suspicion for covid a computed tomography (CT) scan with contrast of the neck and thorax was done which showed a large retropharyngeal space fluid collection from C1-C6 measuring 5.2 x 2.2 x 7.7 cm with extension to bilateral parapharyngeal space and left submandibular space as seen in Fig. 1. Thoracic cuts showed multiple central and peripheral ground glass opacities in the right upper lobe and bilateral lower lobes, findings that were typical of viral pneumonia with a CT severity of 4/25 and Co RADS 5. The patient denied any known contact with a Covid case
Fig. 1.
a Photograph of the patient showing the submandbibular abscess. b The computed tomography image of the neck in the lateral plane showing the retropharyngeal abscess (white arrow). c The computed tomography image of the neck in axial plane showing the retropharyngeal abscess (black arrow). d The Computed tomography image of thorax showing viral pneumonia
A multidisciplinary approach involving internal medicine and otolaryngology was instituted for appropriate management of the patient which included management of viral pneumonia, glycemic control and surgical management of the abscess. Patient was taken up for transoral drainage of the retropharyngeal abcess and 15 ml pus was drained and sent for microbiology. Culture showed growth of klebsiella pneumoniae sensitive to Piperacillin- tazobactum, Ciprofloxacin and Imipenem. A ryle’s tube was maintained for feeding which was maintained for 2 days and then oral feeds were started. His complaints of hypo nasal voice and dysphagia improved significantly. He was discharged 4 days after the procedure when the repeat flexible scopy and x ray neck lateral view showed resolution of the abscess and was advised home isolation as shown in Fig. 2.
Fig. 2.
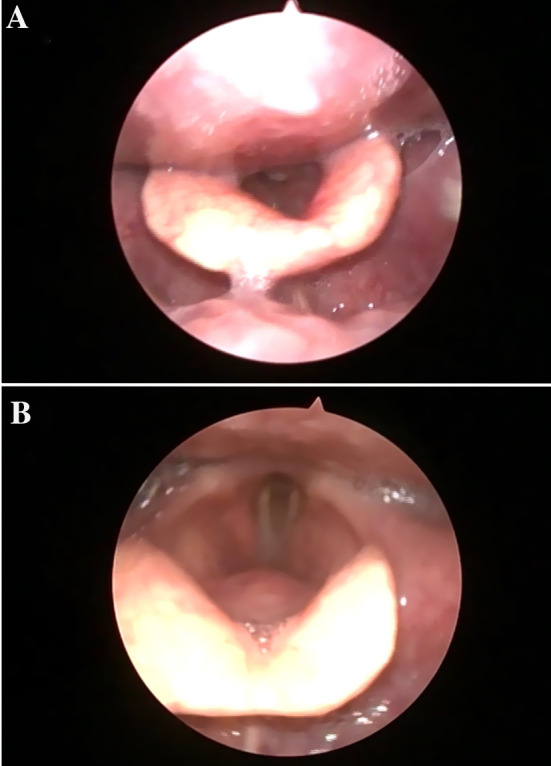
a The flexible laryngoscopy image prior to drainage of the retropharyngeal abscess showing a bulge in posterior pharyngeal wall. b The postoperative flexible laryngoscopy image at the time of discharge
Discussion
Majority of deep neck space abscesses and infections arise from septic foci involving mucosal surfaces of the upper airway, digestive tracts and mandibular teeth. Precipitating factors for deep neck infections and abscesses include dental infections, trauma, tonsillitis, foreign body and head and neck malignancies [2]. They occur via direct extension and develop in the potential spaces between the layers of deep cervical fascia [3]. The most common presenting symptoms include fever, neck swelling, sore throat, dysphagia, dyspnea, odynophagia, torticollis, otalgia, drooling and respiratory distress [2, 3]. Deep neck space abscesses can develop rapidly and potentially cause life threatening complications, therefore early diagnosis is imperative in the management of these patients. Deep neck infections in immunocompromised patients with underlying systemic diseases such as diabetes and chronic renal failure have been described to have a higher complication rate [4]. Bacterial cultures from deep neck infections are usually polychromies, with aerobic gram-positive streptococcus being most commonly isolated [5]. Other aerobic gram-positive organisms such as Staphylococcus epidermidis and Staphylococcus aureus have been reported as the next most commonly isolated organism. Aerobic gram-negative pathogens such as Escherichia coli and Hemophilus influenzae have also been isolated but less commonly [6].
COVID-19 is the cause of significant morbidity and mortality in the ongoing pandemic. Upper airway symptoms in patients with COVID-19 disease include pharyngodynia, nasal congestion, rhinorrhea, smell and taste dysfunction [7]. Laryngeal complications in COVID-19 patients can affect voice, airway and swallowing [8]. However only one other case of retropharyngeal abcess in a suspected Covid patient has been published so far [9]. Much like our case this patient was also covid RT PCR negative with a strong evidence of covid pneumonia on radiology.
The retropharyngeal space extends from the skullbase to the chest, lies posterior to the pharynx, bound by the buccopharyngeal fascia anteriorly, the prevertebral fascia posteriorly and the carotid sheaths laterally. Retropharyngeal abscess is more common in children than in adults, and the mortality rate is estimated between 1 and 2% [10]. Once descending mediastinitis occurs, the mortality rate approaches 25%, despite the use of antibiotic therapy [11]. Retropharyngeal abscesses can develop following a nasopharyngeal viral infection. Rhinovirus has been reported to lead to a secondary bacterial oropharyngeal infection that subsequently caused the development of a retropharyngeal abscess in a one month-old infant [12]. Epstein-Barr virus infection has been suggested to be associated with retropharyngeal abscess formation in children [13]. A retropharyngeal abscess can also develop as either a co-infection or a secondary complication of influenza virus infection [14]. Compared to children with the abundance of retropharyngeal lymph nodes, abscesses in adults is rarely caused by nasal or pharyngeal infection. Risk factors for retropharyngeal abscess in adults mostly include dental infections, tuberculosis cervical spine osteomyelitis and trauma by foreign body ingestion or instrumentation such as intubation and laryngoscopy. Clinical diagnosis of retropharyngeal abscess can pose a challenge due to the non-specificity of symptoms. Studies have described difficulties with using CT modality to differentiate between cellulitis involving the retropharyngeal space and retropharyngeal abscess formation [15].
As the pandemic is ongoing there is still inadequate data on the various sequelae of covid infection and the pathogenesis of the abscess in covid pneumonia needs to be investigated. In our case the general immunocompromised state due to uncontrolled diabetes may be the major contributory factor for the deep neck abscess. Through this case report we would also like to stress upon the need for following covid precautions even in RT- PCR negative patients, especially in the emergency setting.
Authors' Contributions
All authors made substantial contribution to this paper and all the authors have approved the version to be published.
Funding
No funds, grants, or other support was received.
Availability of Data and Material
Data transparency has been maintained.
Declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the institution ethics committee.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
The participants have consented to the submission of the case details for publication.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma Thorp, Carrie S (1998) Neck abscess: an unusual presentation of a thoracic malignancy. J Laryngol Otol 112:891–892. [DOI] [PubMed]
- 3.Motahari SJ, Poormoosa R, Nikkhah M, Bahari M, Shirazy SMH, Khavarinejad F (2014) Treatment and prognosis of deep neck infections. Indian J Otolaryngol 67:134–137. [DOI] [PMC free article] [PubMed]
- 4.Chen MK, Wen YS, Chang CC, Lee HS, Huang MT, Hsiao HC. Deep neck infections in diabetic patients. Am J Otolaryngol. 2000;21:169–173. doi: 10.1016/S0196-0709(00)85019-X. [DOI] [PubMed] [Google Scholar]
- 5.Huang T, Tseng F, Yeh T, Hsu C, Chen Y. Factors affecting the bacteriology of deep neck infection: a retrospective study of 128 patients. Acta Otolaryngol. 2006;126:396–401. doi: 10.1080/00016480500395195. [DOI] [PubMed] [Google Scholar]
- 6.Cordesmeyer R, Kauffmann P, Markus T, Sömmer C, Eiffert H, Bremmer F. Bacterial and histopathological findings in deep head and neck infections: a retrospective analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124:11–15. doi: 10.1016/j.oooo.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Lovato A, de Filippis C. Clinical presentation of COVID-19: a systematic review focusing on upper airway symptoms. Ear Nose Throat J. 2020;99:569–576. doi: 10.1177/0145561320920762. [DOI] [PubMed] [Google Scholar]
- 8.Naunheim MR, Zhou AS, Puka E, Franco RA, Carroll TL, Teng SE. Laryngeal complications of COVID-19. Laryngoscope Investigative Otolaryngol. 2020;5:1117–1124. doi: 10.1002/lio2.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang T, Liu H, Liang C, Zhang H, Liao J, Liu H (2021) Retropharyngeal abscess in an adult With Pneumonia during COVID-19 outbreak. J Craniofac Surg 32(2):691–693. [DOI] [PubMed]
- 10.Qureshi Hannan A, Ference Elisabeth H, Tan Bruce K, et al. National trends in retropharyngeal abscess among adult inpatients with peritonsillar abscess. Otolaryngol Head Neck Surg. 2015;152:661–666. doi: 10.1177/0194599814568286. [DOI] [PubMed] [Google Scholar]
- 11.Renzo M, Barbara J, Ugo C, et al. Descending necrotizing mediastinitis: ten years’ experience. Ear Nose Throat J. 2004;83:776–780. [PubMed] [Google Scholar]
- 12.Hee J, Sung SSI, Jin Kyu Kim, Jung Ji Mi, Eun Sun Kim, Soo Han Choi (2013) Retropharyngeal abscess coinfected with Sta phylococcus aureus and Mycobacterium tuber culosis after rhinoviral infection in a 1month old infant. Korean J Pediatr 56:86–89 [DOI] [PMC free article] [PubMed]
- 13.Takoudes TG, Haddad J. Retropharyngeal abscess and Epstein-Barr virus infection in children. Ann Otol Rhinol Laryngol. 1998;107:1072–1075. doi: 10.1177/000348949810701213. [DOI] [PubMed] [Google Scholar]
- 14.Foster C, Kaplan SL (2018) Severe head and neck infections following influenza virus infection in children. Open Forum Infectious Diseases 5:S697–S698, 2346.
- 15.Harkani A, Hassani R, Ziad T, Aderdour L, Nouri H, Rochdi Y. Retropharyngeal abscess in adults: five CASE reports and review of the literature. Sci World J. 2011;11:1623–1629. doi: 10.1100/2011/915163. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data transparency has been maintained.