TO THE EDITOR
Prurigo nodularis (PN) is an intensely pruritic, inflammatory skin disease characterized by symmetrically distributed hyperkeratotic nodules (Kwatra, 2020; Kwon et al, 2019). The intense pruritus associated with PN often severely impacts quality of life (Huang et al, 2020c; Iking et al, 2013; Pereira et al, 2020). In our previous experience as well as in a European cohort, patients with PN had a greater severity of disease, itch intensity, and more dramatic reduction in quality of life compared to other patients with chronic pruritus (Zeidler et al, 2020; Whang et al, 2020b; Williams et al, 2020). Thus, we hypothesized that patients with PN experience higher rates of disease comorbidities and healthcare utilization compared with patients who have other pruritic, inflammatory skin conditions. To address current gaps in understanding of PN, we employed national claims data to describe the epidemiology, comorbidities, and healthcare utilization of patients with PN.
Using anonymized, nationally-representative, private insurance claims data (October 2015 - December 2019), we defined PN patients as individuals with two or more medical claims for PN using ICD-10-CM codes. For comparison to patients with inflammatory skin diseases, ICD-10-CM codes were also used to identify patients with atopic dermatitis (AD) and psoriasis. Matched controls (age- and gender- matched to PN patients) were selected from individuals without any ICD-10-CM codes for PN, AD, and psoriasis. Further details are provided in the Supplemental Materials.
In our analysis of nationwide claims data, we identified number of cases of PN, AD, and psoriasis annually. In 2016, there were 2,658 PN patients, 21,482 AD patients, and 21,073 psoriasis patients. In 2017, there were 4,823 PN patients, 38,805 AD patients, and 35,193 psoriasis patients. In 2018, there were 6,992 PN patients, 54,593 AD patients, and 47,382 psoriasis patients. In 2019, there were 9,426 PN patients, 70,298 AD patients, and 59,509 psoriasis patients. The annual period prevalence estimates in the claims database are shown in Table 1. The prevalence estimates for PN in 2016 were 18 per 100,000 overall, 22 per 100,000 for adults, and 2 per 100,000 for children and the estimates rose to 58 per 100,000 overall, 70 per 100,000 for adults, and 7 per 100,000 for children in 2019. The mean (SD) age for PN patients was 57.5 (17.0) years in 2016 and increased to 59.8 (16.9) years in 2019. The gender breakdown ranged from 44.5% male in 2016 to 46.5% male in 2019. The demographics for controls and AD and psoriasis patients are also shown in Table 1.
Table 1.
Period Prevalence Estimates (Per 100,000) for PN, AD, and Psoriasis
| PN | AD | Psoriasis | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| 2016 | 2017 | 2018 | 2019 | 2016 | 2017 | 2018 | 2019 | 2016 | 2017 | 2018 | 2019 | |
| Overall | 18 | 32 | 45 | 58 | 146 | 255 | 348 | 432 | 144 | 232 | 302 | 366 |
| Children | 2 | 4 | 6 | 7 | 419 | 742 | 1,016 | 1,275 | 15 | 26 | 33 | 40 |
| Adults | 22 | 39 | 54 | 70 | 74 | 127 | 178 | 227 | 178 | 286 | 370 | 445 |
Abbreviations: AD, atopic dermatitis; PN, prurigo nodularis.
For a comprehensive analysis of the comorbidity burden, we quantified the overall comorbidity burden with the Charlson Comorbidity Index (CCI). We also examined the comorbidity profiles using the individual components of the CCI (Figure 1). PN patients had the highest CCI of these groups, with a mean (SD) of 1.53 (2.27) compared with 0.98 (1.82) for the controls (age- and gender-matched to PN patients), 0.53 (1.16) for AD patients, and 1.16 (1.88) for psoriasis patients in 2016, and 2.32 (2.84) compared with 1.57 (2.42) for the controls, 0.75 (1.52) for AD patients, and 1.71 (2.40) for psoriasis patients in 2019 (Table 1A).
Figure 1. Comorbidity heatmap for PN, AD, and psoriasis.
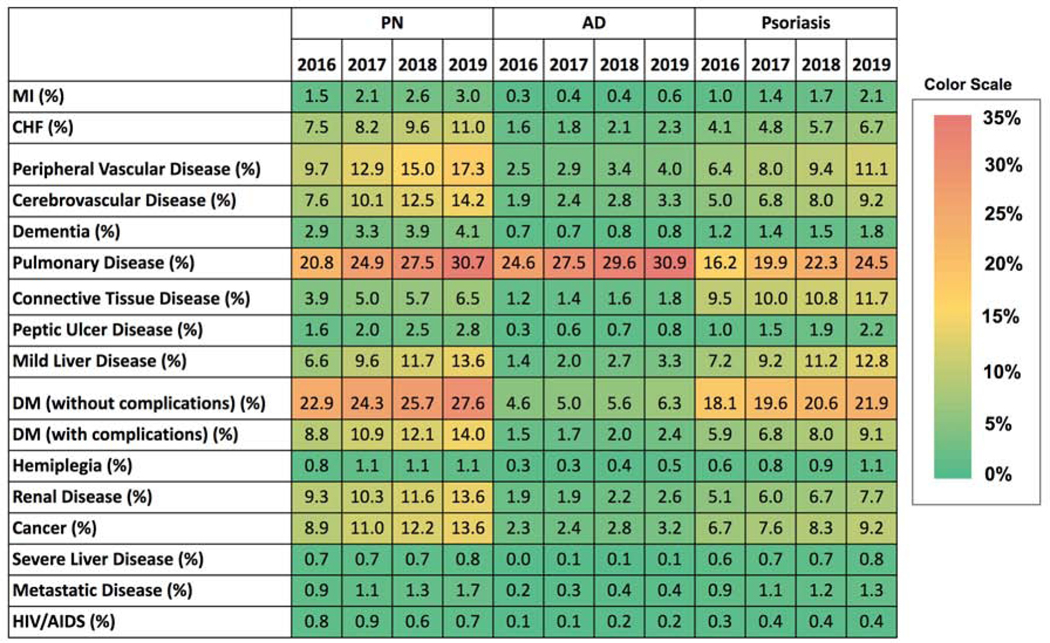
Comorbidity heatmap comparing the comorbidity prevalence (in percentages) for patients with PN, AD, and psoriasis; color scale where green indicates the lowest percentage of the comorbidity burden and red indicates the highest percentage of the comorbidity burden (prevalence corresponds to the annual period prevalence). AD, atopic dermatitis; AIDS, acquired immunodeficiency syndrome; CHF, congestive heart failure; DM, diabetes mellitus; Ml, myocardial infraction; PN, prurigo nodularis.
The top five specialties seen by PN patients, by the estimated number of visits per year per patient, were internal medicine (2.01), dermatology (1.87), family practice (1.60), cardiology or cardiovascular disease (0.85), and orthopedics or orthopedic surgery (0.49). For comparison, estimates of the most visited specialties for controls and patients with atopic dermatitis and psoriasis are provided in Table 1C.
Patients with PN had a higher burden of several cardiovascular, pulmonary, and other systemic diseases when compared to AD and psoriasis patients (Boozalis et al, 2018; Whang et al, 2019; Huang et al, 2020a). PN patients may experience higher disease burden as the itch in PN is thought to be the most severe of chronic pruritic dermatoses (Steinke et al, 2018). PN is also associated with a broad range of diseases such as liver disease, renal disease, HIV, and malignancies among others (Kwatra, 2020; Dazzi et al, 2011).
The higher disease burden of PN translates to higher healthcare utilization of specialty care by patients. PN patients saw dermatologists more frequently than controls as well as AD and psoriasis patients. Consistent with our findings of the higher rates of comorbid cardiovascular disease in PN patients, these patients also had the highest estimated utilization of cardiology or cardiovascular disease specialty visits in this study. Our results support prior findings indicating that PN patients had a higher utilization of care from specialists (Huang et al, 2020b). Additionally, PN patients are more likely to be hospitalized, have longer inpatient stays, and higher inpatient costs of care, compared to the general population (Whang et al, 2019; Whang et al, 2020a).
In summary, PN was associated with higher healthcare utilization of specialty care and comorbidity burden than age- and gender-matched controls as well as compared with patients with AD and psoriasis. PN patients often remain recalcitrant to treatment and suffer from impaired quality of life due to their chronic itch-scratch cycle and associated comorbidity burden. Limitations of this study include the retrospective nature of the analysis and the identification of patients with PN with the ICD-10-CM code, which require further validation. To increase the validity of PN identification through ICD-10-CM codes for this study, we defined PN patients as those who had at least two claims with the corresponding ICD-10-CM code based on the methodology that has been previously published (Steinke et al, 2018). However, the ICD-10-CM code for PN requires further validation. Furthermore, the increase in annual prevalence estimates for PN, AD, and psoriasis observed in the study could also be a result of increasing coding of these diagnoses in the claims data along with rising awareness by the medical profession. The findings presented here should be considered preliminary and the foundation for further research since the study is based upon retrospective claims data. Overall, this study provides a nationwide description of the epidemiology, comorbidities, and healthcare utilization of PN as compared to control and other similar pruritic, inflammatory skin diseases at the national level.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Susanne Churchill, Erica Meyer, and Nathan Palmer of the Department of Biomedical Informatics at Harvard Medical School for providing assistance with claims data access.
Abbreviations
- PN
prurigo nodularis
- AD
atopic dermatitis
- CCI
Charlson Comorbidity Index
- SD
standard deviation
Footnotes
DATA AVAILABILITY STATEMENT
Under law and regulations, the database cannot be made available. Due to data use agreements, the claims data must remain private; inquiries regarding the data can be directed to the corresponding author (SGK).
CONFLICT OF INTEREST STATEMENT
SGK is an advisory board member/consultant for Abbvie, Galderma, Incyte Corporation, Pfizer Inc., Regeneron Pharmaceuticals, and Kiniksa Pharmaceuticals and has received grant funding from Galderma, Pfizer Inc. and Kiniksa Pharmaceuticals.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Boozalis E, Tang O, Patel S, Semenov YR, Pereira MP, Ständer S, et al. Ethnic differences and comorbidities of 909 prurigo nodularis patients. J Am Acad Dermatol. 2018;79(4):714–719.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dazzi C, Erma D, Piccinno R, Veraldi S, Caccialanza M. Psychological factors involved in prurigo nodularis: A pilot study. J Dermatolog Treat. 2011;22(4):211–214. [DOI] [PubMed] [Google Scholar]
- Huang AH, Canner JK, Khanna R, Kang S, Kwatra SG. Real-World Prevalence of Prurigo Nodularis and Burden of Associated Diseases. J Invest Dermatol. 2020a;140(2):480–483.e4. [DOI] [PubMed] [Google Scholar]
- Huang AH, Canner JK, Williams KA, Grossberg AL, Kwatra MM, Kwatra SG. Healthcare resource utilization and payer cost analysis of patients with prurigo nodularis. Br J Dermatol. 2020b;183(1):182–184. [DOI] [PubMed] [Google Scholar]
- Huang AH, Williams KA, Kwatra SG. Prurigo Nodularis: Epidemiology and Clinical Features. J Am Acad Dermatol. 2020c;0(0). [DOI] [PubMed] [Google Scholar]
- Iking A, Grundmann S, Chatzigeorgakidis E, Phan NQ, Klein D, Ständer S. Prurigo as a symptom of atopic and non-atopic diseases: aetiological survey in a consecutive cohort of 108 patients. J Eur Acad Dermatol Venereol. 2013;27(5):550–557. [DOI] [PubMed] [Google Scholar]
- Kwatra SG. Breaking the Itch–Scratch Cycle in Prurigo Nodularis. N Engl J Med. 2020;382(8):757–758. [DOI] [PubMed] [Google Scholar]
- Kwon CD, Khanna R, Williams KA, Kwatra MM, Kwatra SG. Diagnostic Workup and Evaluation of Patients with Prurigo Nodularis. Med (Basel, Switzerland). 2019;6(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira MP, Hoffmann V, Weisshaar E, Wallengren J, Halvorsen JA, Garcovich S, et al. Chronic nodular prurigo: clinical profile and burden. A European cross-sectional study. J Eur Acad Dermatol Venereol. February 2020. [DOI] [PubMed] [Google Scholar]
- Steinke S, Zeidler C, Riepe C, Bruland P, Soto-Rey I, Storck M, et al. Humanistic burden of chronic pruritus in patients with inflammatory dermatoses: Results of the European Academy of Dermatology and Venereology Network on Assessment of Severity and Burden of Pruritus (PruNet) cross-sectional trial. J Am Acad Dermatol. 2018;79(3). [DOI] [PubMed] [Google Scholar]
- Whang KA, Kang S, Kwatra SG. Inpatient Burden of Prurigo Nodularis in the United States. Med (Basel, Switzerland). 2019;6(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whang K, Gabriel S, Chavda R, Kwatra S. Emergency department utilization by patients with prurigo nodularis in the United States. J Am Acad Dermatol. 2020a. [DOI] [PubMed] [Google Scholar]
- Whang KA, Khanna R, Williams KA, Mahadevan V, Semenov Y, Kwatra SG. Health-Related QOL and Economic Burden of Chronic Pruritus. J Invest Dermatol. 2020b. September 14:S0022202X(20)32063-7. [DOI] [PubMed] [Google Scholar]
- Williams KA, Roh YS, Brown I, Sutaria N, Bakhshi P, Choi J, et al. Pathophysiology, diagnosis, and pharmacological treatment of prurigo nodularis. Expert Rev Clin Pharmacol. 2020. November 15. [DOI] [PubMed] [Google Scholar]
- Zeidler C, Pereira MP, Dugas M, Augustin M, Storck M, Weyer-Elberich V, et al. The burden in chronic prurigo: patients with chronic prurigo suffer more than patients with chronic pruritus on non-lesional skin: A comparative, retrospective, explorative statistical analysis of 4,484 patients in a real-world cohort. J Eur Acad Dermatol Venereol. 2020. September 13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


