Supplemental Digital Content is available in the text.
Abstract
The COVID-19 pandemic caused substantial disruptions in medical education. The University of British Columbia (UBC) MD Undergraduate Program (MDUP) is the sixth-largest medical school in North America. MDUP students and faculty developed a joint response to these disruptions to address the curriculum and public health challenges that the pandemic posed.
After clinical activities were suspended in March 2020, third- and fourth-year MDUP students formed a COVID-19 Medical Student Response Team (MSRT) to support frontline physicians, public health agencies, and community members affected by the pandemic. A nimble organizational structure was developed across 4 UBC campuses to ensure a rapid response to meet physician and community needs. Support from the faculty ensured the activities were safe for the public, patients, and students and facilitated the provision of curricular credit for volunteer activities meeting academic criteria.
As of June 19, 2020, more than 700 medical students had signed up to participate in 68 projects. The majority of students participated in projects supporting the health care system, including performing contact tracing, staffing public COVID-19 call centers, distributing personal protective equipment, and creating educational multimedia products. Many initiatives have been integrated into the MDUP curriculum as scholarly activities or paraclinical electives for which academic credit is awarded. This was made possible by the inherent flexibility of the MDUP curriculum and a strong existing partnership between students and faculty.
Through this process, medical students were able to develop fundamental leadership, advocacy, communication, and collaboration skills, essential competencies for graduating physicians. In developing a transparent, accountable, and inclusive organization, students were able to effectively meet community needs during a crisis and create a sustainable and democratic structure capable of responding to future emergencies. Open dialogue between the MSRT and the faculty allowed for collaborative problem solving and the opportunity to transform disruption into academic innovation.
Medical education has undergone many paradigm shifts over the past decades. However, no shift has been as swift and unprecedented as that imposed by the COVID-19 pandemic. As the disease devastated communities, it also disrupted the clinical education of medical students, posing an immediate challenge for the academic progression of students in their clinical years. 1 The sudden availability of time as clinical rotations were suspended, together with a growing public health crisis, led many medical students to form volunteer response organizations to serve urgent physician, community, and health system needs. 2,3 These student-led organizations, when conducted safely and appropriately, provided great value to both community relief efforts and the advancement of students’ education. In this article, we outline the student-led COVID-19 Medical Student Response Team (MSRT) at the University of British Columbia (UBC), describe how the MSRT partnered with the UBC Faculty of Medicine to translate critical public health volunteer activities into academic credit, and explore the implications of this innovative model of curricular integration for medical education.
Effects of COVID-19 on Medical Education in British Columbia
The UBC MD Undergraduate Program (MDUP) is the sixth-largest medical school in North America; 1,152 students are distributed across 4 campuses in the province of British Columbia, with the majority (784) based in Vancouver. On March 17, 2020, the British Columbia Ministry of Health declared a public health emergency due to COVID-19. The MDUP suspended all medical student clinical activities and advised strict adherence to physical distancing protocols. Lectures and small group case-based learning sessions, a primary component of the first- and second-year curriculum, were quickly transitioned to online platforms and video conferencing. However, the disruption of clinical training had a huge impact on the academic progression of third- and fourth-year students. At the time of these pandemic-related policy changes, 291 third-year students were engaged in clinical rotations across British Columbia and 298 fourth-year students were completing elective rotations locally, in other parts of Canada, or internationally. As rotations were suspended with an uncertain time frame to resume, many students experienced significant confusion and anxiety about their professional careers and futures.
The UBC COVID-19 MSRT
The UBC COVID-19 MSRT was established immediately following the suspension of clinical rotations by 6 third- and fourth-year medical students (V.W.L.T., A.Y., M.J.H., Z.S., D.M., and G.C.). This student-led, grassroots initiative was rapidly organized across all UBC campuses, providing the main vehicle for student volunteer activities. The purpose of the MSRT was to: (1) support physicians directly affected, (2) contribute to public health agency efforts, (3) support community members disproportionately affected, and (4) engage and educate the public.
Organization
As of June 19, 2020, the MSRT had more than 700 students signed up to participate, including those UBC students returning home to British Columbia from other Canadian provinces or abroad where they were completing elective rotations. Volunteers were matched to community needs through 2 online request forms: one for individual physician support and the other for paraclinical COVID-19-related projects. These forms were located on secure Canadian servers, and inputs were organized on the back end by a randomized table that automatically updated to identify available volunteers. This rapid triage to match volunteers to projects prioritized fairness and transparency, allowing the MSRT to quickly expand while ensuring operations remained efficient and organized.
A designated faculty advisor with expertise in public health and infectious disease (M.K.) reviewed requests to ensure they were safe, appropriate for the level of training of medical students, and consistent with public health guidelines and medical school policies. Liability coverage was achieved through an approved dual-party agreement waiver for personal errands and UBC liability insurance for Faculty of Medicine approved extracurricular activities through a pro bono legal service and UBC Safety and Risk Services, respectively.
Partnerships between the MSRT and key UBC stakeholders, including the Medical Undergraduate Society (the student governing body) and the Faculty of Medicine, were important to establish MSRT legitimacy and encourage student involvement. Designated students attended meetings with committees overseeing curricular change during the COVID-19 pandemic, including the daily Undergraduate Medical Education COVID-19 Implementation Task Force meetings and the monthly Undergraduate Medical Education Committee meetings. These meetings were an opportunity for students to update the faculty on MSRT projects and, importantly, to provide student input into the process of curricular adaptation.
The MSRT also worked closely with students from other UBC health care disciplines (e.g., nursing, pharmacy, dentistry) to share resources for developing similar volunteer organizations. Expanding beyond the borders of British Columbia, the MSRT collaborated with medical students across Western Canada to develop a website (https://covid19medstudents.ca) to share innovations and centralize information regarding regional COVID-19 response efforts.
Projects
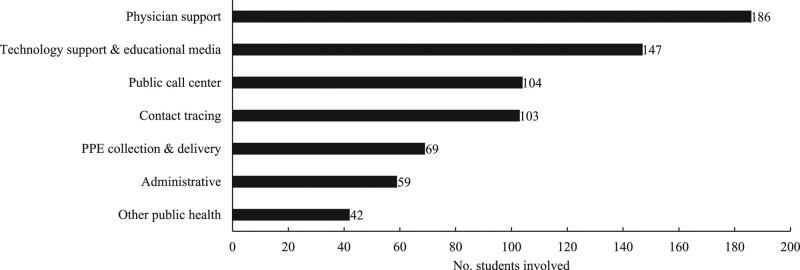
As of June 19, 2020, the MSRT had 68 projects involving 524 students in 710 distinct activity roles (see Figure 1). A complete list of the projects at each of the UBC campuses is included in Supplemental Digital Appendix 1 at http://links.lww.com/ACADMED/B111. There were 96 project requests from health authorities, physicians, and public health organizations. Of these requests, 61 (64%) were accepted based on predetermined criteria and principles. Safety of the public, patients, and students was of paramount importance. Projects were rejected if they did not meet safety standards or were contrary to public health recommendations.
Figure 1.
University of British Columbia COVID-19 Medical Student Response Team volunteer activities by activity role and number of student volunteers, as of June 19, 2020. Note that 1 student can fill more than 1 activity role. Abbreviation: PPE, personal protective equipment.
In addition to these projects, more than 200 frontline physicians requested help with childcare, pet care, and essential errands. Requests were made by physicians of all specialties with the most from those in family medicine (30%), emergency medicine (14%), pediatrics (12%), and internal medicine (10%).
Knowledge dissemination included the creation of various multimedia products. A public website (https://covid19medstudents.ca), created to combine medical student opportunities across Western Canada, had more than 9,000 page views as of June 19, 2020. The MSRT media team also created multimedia products to inform the public about COVID-19 and dispel misinformation. For example, the team created an infographic, a series of educational videos, and a website. The infographic has had more than 63,000 views on Twitter and has been translated into 10 languages (see Supplemental Digital Appendix 2 at http://links.lww.com/ACADMED/B111). Working closely with the UBC Faculty of Medicine Educational Technology Team, students helped produce an animated video series, which was translated into 24 languages and disseminated through an official UBC YouTube playlist. 4
Curricular Integration of COVID-19 Activities
The MSRT was established within days of clinical rotations being suspended and before the MDUP had defined a clear path forward to promotion and graduation for third- and fourth-year students. While students rapidly organized to fill urgent gaps in the public health system, they also began working with the faculty to find solutions that would allow them to continue their academic work and participate in pandemic relief. Classes continued online for first- and second-year students, so the MSRT capped their volunteer work at 20 hours per week to protect time for these students to complete their academic work. For third- and fourth-year students, their volunteer activities were directly integrated into the curriculum.
Third-year students
In 2015, Flexible and Enhanced Learning (FLEX) was added to the MDUP curriculum. 5 This novel series of 3 courses allows students to develop and pursue individual learning interests in depth. Courses can take place in academic settings or communities across British Columbia, Canada, or globally. The curriculum provides dedicated time for FLEX project work in 3 academic years (years 1, 2, and 4), with guidance and feedback from FLEX advisors and activity supervisors. Students are evaluated according to the CanMEDS competency framework. 6 This established framework for medical education in Canada includes 7 roles (medical expert, communicator, collaborator, scholar, professional, leader, and health advocate) that students must develop during their medical training; these roles are integrated into the MDUP exit competencies. 7
In response to the sudden interruption of third-year clinical rotations, the MDUP moved the year 4 FLEX course from November 2020 to April 2020 and, working in close partnership with the MSRT, created a new series of FLEX projects allowing students to combine COVID-19 volunteer service with a self-selected scholarship activity. Eligible projects had to be directly related to medicine or public health, as opposed to personal support for frontline physicians. In addition, all students were required to identify a supervisor and carry out their project while adhering to the scholarly standards proposed by Glassick. 8 A brief literature review relevant to their project and a written reflection on their learning were expected at the end of each FLEX project. There was no formal service-learning framework applied to these projects at initiation because the intent was to quickly integrate public service and student promotion to the next academic year. The following are examples of volunteer projects that were transformed into FLEX projects.
Supporting anesthesiologist wellness.
The Anesthesiology Department of a large tertiary care center in Greater Vancouver requested a task force of medical students to find innovative ways to improve morale among some of the most at-risk frontline physicians. Working with a psychiatrist supervisor, the students surveyed department staff and identified areas of concern, including personal and family safety, physician workload, and burnout. They then performed a detailed review of existing mental health and wellness resources. The final product was the British Columbia Physician Wellness in COVID-19 infographic, a comprehensive, practical, and user-friendly resource with embedded links to help physicians manage anxiety and stay safe (see Supplemental Digital Appendix 3 at http://links.lww.com/ACADMED/B111). This resource has been used by health authorities and physicians across British Columbia.
Infection control rapid literature reviews.
The infection prevention and control leadership of the 2 major Vancouver health authorities requested a student task force to regularly review the rapidly evolving COVID-related infection control literature to inform hospital policies. Students identified, appraised, and summarized key medical publications on a daily basis; these summaries were then reviewed by health authority leaders and used to update guidelines and disseminate knowledge to frontline staff.
Connecting with compassion.
Due to outbreaks of COVID-19, many long-term care facilities were locked down, resulting in significant social isolation for residents. Geriatricians requested a team of medical students to video conference with long-term care facility residents and provide them companionship through conversation, activities, and music. The group expanded their efforts across the province and launched quality improvement studies to demonstrate and augment the project’s impact. 9
Fourth-year students
At the onset of the pandemic, although fourth-year students’ elective rotations were suspended, the priority was to provide them with an academic pathway to graduation. In collaboration with the MSRT, the Faculty of Medicine approved elective credit for sanctioned paraclinical volunteer activities, stipulating that fourth-year students had to formally register their activities and complete a brief written reflection. This action allowed students to continue to support the health system while developing the CanMEDS competencies and to graduate on schedule.
Implications for Medical Education
The rapid development of the MSRT and the integration of its volunteer activities into the formal curriculum solved 3 urgent needs: (1) the need many students felt to contribute meaningfully to the pandemic response, (2) the needs of a health system in crisis, and (3) the need for academic advancement despite the suspension of clinical and elective rotations. This model has significant implications for medical education in both times of crisis and periods of calm.
Curriculum flexibility and teaching social responsibility
Canada has long been a pioneer in the ongoing transformation of medical education. McMaster University introduced the world’s first problem-based learning curriculum in 1969 10; the Royal College of Physicians and Surgeons of Canada developed the CanMEDS framework of essential physician competencies; and the principle of a “spiral curriculum,” first described by Bruner in 1960, 11 was implemented by McMaster University in 2005 and by UBC in 2015. 12–14
The UBC FLEX program is one of the most recent innovations in medical education, providing credit for students to pursue their scholarly passions longitudinally across their medical training, and it is unique among Canadian medical schools. The FLEX program is also designed to fulfill the UBC Faculty of Medicine Social Responsibility and Accountability Framework. 15 This framework states that the role of medical education, beyond ensuring knowledge competency, is to develop physicians who meet the current and future health care needs of society. To meet accreditation standards, Canadian medical schools are required to demonstrate that their curricular content reflects this social responsibility mandate. 16
The FLEX program proved to be an ideal way to integrate student social activism and tangible academic competencies. Its inherent flexibility, both within the MDUP curriculum structure and in the myriad projects that students can pursue, along with its essential role in fostering social responsibility and the CanMEDS competencies, allowed medical education to continue despite the interruption in clinical rotations. This success also rests on a core tenet of Canadian medical education that physicians are more than knowledge or technical experts. They must have a holistic set of skills and attitudes to meet the priority health needs of the communities they serve.
Faculty–student collaboration
A strong faculty–student partnership was essential to both the success of the MSRT and the incorporation of volunteer work into the curriculum. The MDUP has a history of involving students in decision making, particularly in the redesign of the curriculum and governance structure that has happened since 2015. The FLEX program has also generated a wide professional network of relationships between faculty and students. During the COVID-19 pandemic, students and faculty were able to draw on this history of collaboration to create mutually beneficial outcomes.
The MSRT represented an organic expression of students’ desire to assist COVID-19 pandemic response efforts while productively filling the vacuum created when clinical rotations were suspended, and most students likely would have continued to volunteer even without receiving academic credit. However, faculty endorsement and support significantly enhanced the power and efficiency of the response effort. Student representation on the Undergraduate Medical Education COVID-19 Implementation Task Force fostered an appreciation among faculty for the scope and professionalism of student activities, reinforcing the decision to give credit for volunteer work. The designated faculty advisor (M.K.) to the MSRT ensured that all paraclinical volunteer activities met MDUP criteria for safety and were consistent with current public health recommendations. MDUP endorsement through curricular credit, partial liability coverage, and circulation of MSRT communications further legitimized the response team and enhanced student involvement.
Future Directions*
By June 2020, a plan was created to transition the MSRT to report to the UBC Medical Undergraduate Society (the student governing body) to create a more democratic and sustainable organizational framework and an official connection to the MDUP governance structure. The official medical student volunteer response to all future emergencies will be managed by a new Emergency Response Committee under the Medical Undergraduate Society.
The FLEX program will continue to play an essential role in helping students to develop the CanMEDS competencies and become socially responsible physicians, as well as in preparing them for future crises. Along with teaching basic research and analytical skills, the FLEX program could include public health training on topics such as epidemiology and contact tracing in its Foundations of Scholarship course for first-year students. Future projects could include the development of a permanent medical student team to assist with vaccination for seasonal diseases such as influenza, sporadic outbreaks such as measles, or a mass vaccination campaign for COVID-19. Should future health emergencies result in the disruption of clinical training, the FLEX program remains a critical mechanism to continue education.
Conclusions
The COVID-19 pandemic has been the source of both profound disruption and great opportunity in medical education. UBC medical students responded to the challenge by creating a large, effective organization to rapidly provide a health system in crisis with needed volunteers and creative solutions. Through MSRT projects, students were able to realize a powerful desire to serve their communities and contribute to the health systems where they will spend their careers. Along the way, they developed essential professional skills as leaders, collaborators, health advocates, and communicators. The UBC Faculty of Medicine supported and guided this effort from the beginning, eventually using it to provide high-quality medical education in the time of COVID-19. The MSRT and the novel curricular partnership that followed were innovations in the context of an emergency, but success was possible only because of a strong history of faculty–student communication and partnership as well as a flexible curriculum with a mandate to develop well-rounded physicians who are accountable to society. These elements should be developed and strengthened in institutions around the world to build resiliency in medical education for future emergencies.
Acknowledgments:
The authors thank all members of the British Columbia COVID-19 Medical Student Response Team (MSRT) for their dedication to this initiative. The volunteers are key to the continued success of the organization, and it would be impossible to carry on this important work without their support. The authors also thank the University of British Columbia Faculty of Medicine for their ongoing encouragement and willingness to work collaboratively with students to create the best outcomes for curricular reform during this pandemic. They offer special thanks to the Flexible and Enhanced Learning (FLEX) team, Dr. Alice Mui and Dr. Richard Lazenby, and to Zachary Rothman, the Faculty of Medicine Educational Technology team, and Gloo Studios for producing extraordinary public education media. Finally, they thank the physicians of British Columbia, the Canadian Federation of Medical Students, all health authorities in British Columbia, their community partners, and the many pro bono lawyers who helped in multifaceted ways to support the work of this organization.
Supplementary Material
Footnotes
Supplemental digital content for this article is available at http://links.lww.com/ACADMED/B111.
Funding/Support: None reported.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Vivian W.L. Tsang, Email: vivianwltsang@alumni.ubc.ca.
Alec Yu, Email: alec.yu@alumni.ubc.ca.
Morgan J. Haines, Email: morgan.haines@alumni.ubc.ca.
Zach Sagorin, Email: zachsagorin@alumni.ubc.ca.
Devon Mitchell, Email: devon.mitchell@alumni.ubc.ca.
Geoffrey Ching, Email: g.ching@alumni.ubc.ca.
Cheryl L. Holmes, Email: cheryl.holmes@ubc.ca.
References
- 1.Iacobucci G. Covid-19: Medical schools are urged to fast-track final year students. BMJ. 2020;368:m1064. [DOI] [PubMed] [Google Scholar]
- 2.Soled D, Goel S, Barry D, et al. Medical student mobilization during a crisis: Lessons from a COVID-19 medical student response team. Acad Med. 2020;95:1384–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalet AL, Jotterand F, Muntz M, Thapa B, Campbell B. Hearing the call of duty: What we must do to allow medical students to respond to the COVID-19 pandemic. WMJ. 2020;119:6–7. [PubMed] [Google Scholar]
- 4.UBC Medicine-Educational Media. COV-Ed. https://www.youtube.com/playlist?list=PL242bEng6nyIGrPckgmc6zCbMzZdX7yVk. Updated March 9, 2021. Accessed April 12, 2021.
- 5.UBC Faculty of Medicine. FLEX (Flexible and Enhanced Learning). https://mednet.med.ubc.ca/Teaching/FLEX/Pages/default.aspx. Accessed April 12, 2021.
- 6.Frank JR, Snell L, Sherbino J. CanMEDS 2015 Physician Competency Framework. 2015Ottawa, Canada: Royal College of Physicians and Surgeons of Canada; http://canmeds.royalcollege.ca/uploads/en/framework/CanMEDS%202015%20Framework_EN_Reduced.pdf. Accessed April 12, 2021. [Google Scholar]
- 7.UBC Faculty of Medicine. MD undergraduate program. Exit competencies. http://med-fom-ugrad.sites.olt.ubc.ca/files/2015/08/UBC-Exit-Competencies-June-2013-update.pdf. Published June 2013. Accessed April 29, 2021.
- 8.Glassick CE. Boyer’s expanded definitions of scholarship, the standards for assessing scholarship, and the elusiveness of the scholarship of teaching. Acad Med. 2000;75:877–880. [DOI] [PubMed] [Google Scholar]
- 9.UBC Faculty of Medicine News. Combatting social isolation during COVID-19. https://www.med.ubc.ca/news/combatting-social-isolation-during-covid-19. Published June 1, 2020. Accessed April 12, 2021.
- 10.Neville AJ, Norman GR. PBL in the undergraduate MD program at McMaster University: Three iterations in three decades. Acad Med. 2007;82:370–374. [DOI] [PubMed] [Google Scholar]
- 11.Bruner JS. The Process of Education. 1960.Cambridge, MA: Harvard University Press; [Google Scholar]
- 12.Wright AD, Fraser SK, Smirl JD, van Donkelaar P. Comparison of spiral versus block curriculum styles in preparing medical students to diagnose and manage concussions. Br J Sports Med. 2017;51:A61–A62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pallie W, Carr DH. The McMaster Medical education philosophy in theory, practice and historical perspective. Med Teach. 1987;9:59–71. [DOI] [PubMed] [Google Scholar]
- 14.Servant-Miklos VFC. Fifty years on: A retrospective on the world’s first problem-based learning programme at McMaster University Medical School. Health Prof Educ. 2019;5:3–12. [Google Scholar]
- 15.Parhar G. How can medical education train socially responsible physicians? UBCMJ. 2019;10:8–9. [Google Scholar]
- 16.Committee on Accreditation of Canadian Medical Schools. Standards for accreditation of medical education programs leading to the M.D. degree. https://cacms-cafmc.ca/sites/default/files/documents/CACMS_Standards_and_Elements_AY_2020-2021.pdf. Published 2019. Accessed April 12, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.