Abstract
The COVID-19 pandemic continues to limit medical students’ full reintegration into clinical learning environments, thus exacerbating an ongoing challenge in identifying a robust number of clinical educational activities at excellent clinical sites for all students. Because medical students across the United States were removed from direct patient care activities in mid-March 2020 due to COVID-19, medical centers have prioritized and implemented changes to the process of patient care. As some barriers are being lifted in the face of a highly contagious and deadly infection, the use of telehealth (delivery of health services remotely via telephone, video, and secure messaging), although not new, is rapidly expanding into all aspects of patient care. Health care providers have been encouraged to conduct many interactions at a physical distance. Telehealth largely replaced face-to-face visits for nonemergency care in an attempt to slow viral transmission while enabling physicians to continue to deliver patient education, manage acute and chronic illness, and nurture caring doctor–patient relationships. Health care providers, many of whom were initially reluctant to embrace telehealth technology and logistics, are becoming nimbler and more aware of the many positive aspects of telehealth. The authors suggest that integrating medical students into telehealth activities would help maintain and improve patients’ health, extend the capabilities of health care teams and systems during and after the pandemic, and increase medical students’ opportunities for experiential learning and professional identity formation. The authors expand on these 3 goals, suggest several concrete student telehealth activities, propose a curricular strategy, and outline opportunities to overcome key barriers to full alignment of telehealth and undergraduate medical education.
The COVID-19 pandemic, which has no clear end, has limited and continues to limit the clinical experiences of medical students. This situation has exacerbated an ongoing challenge for medical schools: identifying clinical sites and patient care experiences for medical students to achieve learning goals while contributing to the health of patients and communities. As of January 2021, medical students have been only tentatively integrated into telehealth activities (delivery of health care remotely via telephone, video, and secure messaging), but COVID-19 may serve as a catalyst to innovation. 1 A more comprehensive expansion of an undergraduate medical education telehealth curriculum would be transformational—both immediately and into the postpandemic future. COVID-19 has created the conditions for a rapid uptake of telehealth technology as care shifts to locations outside of the clinic, emergency department, and hospital. A true transformation in the nation’s use of telehealth will need to encompass not only implementing the technical requirements but also providing dedicated training and experiential learning for our future physicians. If telehealth is implemented effectively, we will rapidly accumulate experience vital to addressing the long-standing access to medical care challenges in rural and other underserved communities. Coproducing telehealth curricula with students will accelerate high-quality and safe implementation, increase our capacity to provide care during the pandemic, and sustain the impact of this transformation as medical education and our health care system evolve to a new normal after the pandemic.
The opportunity exists during the pandemic to integrate our intelligent, caring, and technologically adept medical students into all aspects of telehealth to achieve the following goals: (1) maintaining and improving the health of patients immediately, (2) serving health care teams and systems through the pandemic crisis and recovery, and (3) increasing medical students’ opportunities for experiential learning and professional identity formation.
In this article, we expand on these 3 goals, suggest several concrete student telehealth activities, propose a curricular strategy, and outline opportunities to overcome key existing barriers to full alignment of telehealth and medical education.
Maintaining and Improving the Health of Patients
In response to the pandemic and stay-at-home orders, many patients have been asked to postpone elective procedures, delay preventive services, and limit face-to-face interactions for nonemergency care for serious acute and chronic conditions. The medical community is scrambling to identify opportunities to fill these care gaps as the urgent need for triage and follow-up of patients with symptoms suggestive of COVID-19 has been prioritized. Technological advances have enabled care for many acute and chronic conditions despite barriers, like restricted patient mobility, physical distance, and limited access to appropriate transportation. 2 Many evidence-based interventions by phone are available, 3 and meaningful—though limited—physical examination maneuvers can be done virtually even with basic telehealth technology, such as the telephone. 4–6
Lessons learned from centers with long-standing telehealth programs can be integrated into a new standard of care to effectively serve patients during the pandemic and beyond. In-person visits for chronic disease management, review of test results, or follow-up on a hospital/emergency department visit can be rapidly transitioned to video or telephone visits, as can visits for patients with significant mobility barriers With a clear protocol in place, a routine, scheduled face-to-face visit could be easily transitioned to a telehealth interaction if a patient has a last-minute transportation issue or experiences other barriers to in-person attendance, thus potentially reducing the no-show and cancellation rate and improving access to care. By aligning the work of interprofessional teams and their trainees, patient education and adherence to treatment plans may be enhanced with frequent telehealth check-ins by a member of the health care team.
Serving Health Care Teams and Systems
As we rapidly adapt to prioritize acute needs during the pandemic, many of our health care teams have been left with limited personnel resources, especially as some of us prepare for redeployment to help with predicted surges of COVID-19 cases in some regions. Most medical students in the United States were put on a clinical pause starting in mid-March 2020 to preserve essential personal protective equipment (PPE) and to protect them from infection. Initially, some of us argued to expedite the safe return of students to the clinical setting because they can add value to health care teams and practices—and they need the clinical learning experience. 7,8 However, some frontline educators are overwhelmed with providing direct clinical care, and in some clinical sites, ongoing PPE shortages may keep students from returning. Meanwhile, at the time of writing, many other clinician educators have not yet been reassigned to acute care settings and are available to provide supervision to medical students. The potential clearly exists for clinical learning environments to more fully adopt a “learning is work and work is learning” strategy focused on connecting learners and learning objectives with meaningful opportunities to serve. 9 Too often, our clearly identified goals around population health, patient education, and transitions of care are not properly resourced or prioritized. Rather than being viewed as observers or liabilities, medical students who are properly trained in these concepts and skills and empowered to be valuable members of a health care team can actively advance these goals. The lessons we learn from thoughtfully integrating students into the telehealth care system during the pandemic will also be invaluable to durable transformation of the clinical learning environment, a transformation that has been repeatedly called for but remained elusive before the pandemic.
Facilitating Experiential Learning and Professional Identity Formation
Ensuring our trainees develop into competent, ethical, and caring physicians is the mission of medical education. Internalizing a mature medical professional identity, defined as coming to “think, act, and feel like a physician,” is an essential component (if not the ultimate goal) of becoming a physician. 10 However, there are many barriers to the implementation of what medical education scholars and policy leaders have asserted would be the most effective and efficient educational structure to get trainees to the level of expertise needed for unsupervised practice: a time-variable, competency-based medical education that includes extensive supervised clinical experience. 11,12 We assert that the emergence of COVID-19 has presented an opportunity to explore ways in which educational telehealth activities can dramatically expand the structures and processes of medical education, providing evidence and experience that will continue to be applicable after the pandemic has ended.
In Table 1, we have categorized educational telehealth activities as either related to COVID-19 (i.e., outreach and education for patients at high risk of severe disease and initial evaluation and follow-up of patients with symptoms suggestive of coronavirus infection) or unrelated to COVID-19. Both types of activities can dramatically expand experiential learning opportunities for students during the crisis while providing experience and evidence to support ongoing student involvement in telehealth in the postpandemic era. Whether curricula employ milestones, competencies, or entrustable professional activities (EPAs) as organizing concepts, various telehealth encounters present an opportunity for student learning, observation by preceptors, and assessment with feedback to facilitate professional development. Table 1 has suggestions for telehealth activities that could serve as opportunities for students to perform each of the Core EPAs for Entering Residency. 13
Table 1.
Examples of Telehealth Activities, Both Related and Unrelated to COVID-19, to Teach Core Entrustable Professional Activities (EPAs) for Entering Residencya
In light of the expected future demand for telehealth, students and residents will need specific and dedicated training to develop the expertise required to care for patients and populations in this setting. While we would not advocate for telehealth to replace the majority of face-to-face clinical medical education experiences, opportunities exist to develop these activities into observable and rewarding learning activities. Greater use of telehealth may help address some of the barriers to providing care to rural communities where certain health care professionals are not available. A mentored telehealth experience for students and residents may increase their willingness to provide this type of care and better understand its utility and limitations. Technology can enable direct observation via distance precepting, either with the preceptor, patient, and learner all participating via a 3-way video call (like a Zoom meeting) or with the learner using 2 devices—one to connect with the patient and one to connect with the preceptor.
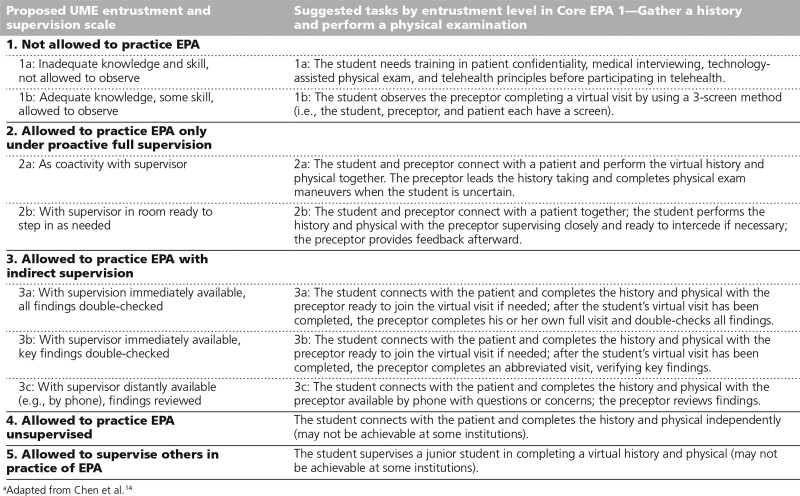
As a student’s skills improve, a preceptor may decide the student is sufficiently trustworthy to conduct telehealth visits with indirect supervision to increase the volume and efficiency of both experiential learning and extension of the health care team. Table 2 suggests a model to adapt Chen et al’s 14 medical student entrustment scale for telehealth activities, using Core EPA 1 as an example.
Table 2.
Proposed Undergraduate Medical Education (UME) Entrustment Scalea for Telehealth With Suggested Student Telehealth Activities by Entrustment Level, Using Core Professional Entrustable Activity (EPA) for Entering Residency 1 as an Example
Overcoming Barriers
For meaningful integration of medical students into telehealth, several challenges must be addressed. While most teaching faculty, themselves the products of the current medical education system, are well versed in supervising medical students during direct face-to-face patient care, many are also learning to provide telehealth for the first time. This situation presents the opportunity to teach faculty and students about the required technology and best practices in parallel, as many of their needs are similar. Key goals and messaging for each activity (i.e., telephone, video, or secure messaging) and common patient conditions must be rapidly and iteratively developed. Strategies for assessing students will need to be adapted to these novel teaching activities.
The electronic medical record (EMR) can serve either to facilitate the incorporation of student education into the emergence of telehealth practices or to block it completely. To fully implement the 3 goals outlined in this article, academic medical centers must give students functional access to the EMR that parallels that of physicians and other health care professionals. This is not the reality at many academic medical centers, where students’ notes are discounted, ignored, and ultimately left out of the permanent medical record. Student documentation of telehealth visits, when edited and signed by a licensed physician, should become a permanent part of the record; this approach would decrease the duplication of documentation and, therefore, the burden on the health care team, while facilitating preceptor review and feedback. The 2018 revision to the Medicare Claims Processing Manual allowing teaching physicians to verify in the medical record all student documentation rather than redocumenting the work makes this a viable, yet currently underused, possibility. 15 Additionally, as the health care team increasingly accesses the EMR via mobile devices and uses voice recognition software to facilitate documentation, students would be well served by having had supervised experience using these technologies.
Conclusions
The COVID-19 pandemic, like other crises, is providing opportunities to accelerate the transformation of medical education and the improvement of our health care system. 16 To take full advantage of this time in our history, we must creatively address the barriers to returning our sidelined students to patient care in educationally meaningful ways. This expansion of medical education is both possible and desirable as we seek to connect students to consequential work that serves our patients, community, and health care team members in this time of great need, while aligning students’ activities with learning goals. Although telehealth is not new, being able to provide care to patients with limited mobility or in rural communities has been an ongoing challenge. The COVID-19 era has brought this issue of accessible care to the forefront and has required medical schools to explore and invest more heavily in telehealth and to reimagine the role telehealth strategies might have in the curricular transformation of health professions education. Indeed, the purposeful curricular implementation of telehealth would serve as a tremendous investment in our students and in the health of our patients and communities.
Acknowledgments:
The authors wish to acknowledge the Medical College of Wisconsin medical students for piloting and providing feedback on several different telehealth experiences while unable to provide direct patient care in the spring of 2020. Patrick Foy, Paul Bergl, Joanne Bernstein, and Cynthia Kay included telehealth activities in required internal medicine clinical rotations while most of our medical students were on a clinical pause.
Footnotes
Funding/Support: Each author receives salary support from the Kern Family Foundation to serve in the Robert D. and Patricia E. Kern Institute for the Transformation of Medical Education at the Medical College of Wisconsin.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
References
- 1.Waseh S, Dicker AP. Telemedicine training in undergraduate medical education: Mixed-methods review. JMIR Med Educ. 2019;5:e12515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ambert-Pompey S, Konecky B, Ahlstrom D, Keefer A. Improving access: Team-based primary care via telehealth in the VA. SGIM Forum. 2017;40:1–3. [Google Scholar]
- 3.Schwartz MD, Jensen A, Wang B, et al. Panel management to improve smoking and hypertension outcomes by VA primary care teams: A cluster-randomized controlled trial. J Gen Intern Med. 2015;30:916–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chorin E, Padegimas A, Havakuk O, et al. Assessment of respiratory distress by the Roth score. Clin Cardiol. 2016;39:636–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greenhalgh T, Koh GCH, Car J. Covid-19: A remote assessment in primary care. BMJ. 2020;368:m1182. [DOI] [PubMed] [Google Scholar]
- 6.Weinstein RS, Krupinski EA, Doarn CR. Clinical examination component of telemedicine, telehealth, mHealth, and connected health medical practices. Med Clin North Am. 2018;102:533–544. [DOI] [PubMed] [Google Scholar]
- 7.Kalet AL, Jotterand F, Muntz M, Thapa B, Campbell B. Hearing the call of duty: What we must do to allow medical students to respond to the COVID-19 pandemic. WMJ. 2020;119:6–7. [PubMed] [Google Scholar]
- 8.DeWitt DE. Fighting COVID-19: Enabling graduating students to start internship early at their own medical school. Ann Intern Med. 2020;173:143–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Schaik SM, Reeves SA, Headrick LA. Exemplary learning environments for the health professions: A vision. Acad Med. 2019;94:975–982. [DOI] [PubMed] [Google Scholar]
- 10.Cruess RL, Cruess SR, Steinert Y. Amending Miller’s pyramid to include professional identity formation. Acad Med. 2016;91:180–185. [DOI] [PubMed] [Google Scholar]
- 11.Lucey CR, Thibault GE, ten Cate O. Competency-based, time-variable education in the health professions: Crossroads. Acad Med. 2018;93(3 suppl):S1–S5. [DOI] [PubMed] [Google Scholar]
- 12.Kogan JR, Whelan AJ, Gruppen LD, Lingard LA, Teunissen PW, ten Cate O. What regulatory requirements and existing structures must change if competency-based, time-variable training is introduced into the continuum of medical education in the United States? Acad Med. 2018;93(3 supplS27–S31. [DOI] [PubMed] [Google Scholar]
- 13.Association of American Medical Colleges. Core Entrustable Professional Activities for Entering Residency: Curriculum Developers’ Guide. https://store.aamc.org/downloadable/download/sample/sample_id/63. Published 2014. Accessed February 12, 2021.
- 14.Chen HC, van den Broek WE, ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90:431–436. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual 2018. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R4068CP.pdf. Published May 2018. Accessed February 12, 2021.
- 16.Barry JM. The Great Influenza: The Story of the Deadliest Pandemic in History. 2004.New York, NY: Viking; [Google Scholar]