Abstract
Objective:
To detect three-dimensionally the effects of using mini-implant anchorage with the Forsus Fatigue Resistant Device (FFRD).
Materials and Methods:
The sample comprised 43 skeletal Class II females with deficient mandibles. They were randomly allocated into three groups: 16 patients (13.25 ± 1.12 years) received FFRD alone (Forsus group), 15 subjects (13.07 ± 1.41 years) received FFRD and mini-implants (FMI group), and 12 subjects (12.71 ± 1.44 years) were in the untreated control group. Three-dimensional analyses of cone beam computed tomographic images were completed, and the data were statistically analyzed.
Results:
Class I relationship and overjet correction were achieved in 88% of the cases. None of the two treatment groups showed significant mandibular skeletal effects. In the FMI group, significant headgear effect, decrease in maxillary width, and increase in the lower facial height were noted. In the FMI group, retroclination of maxillary incisors and distalization of maxillary molars were significantly higher. Proclination and intrusion of mandibular incisors were significantly greater in the Forsus group.
Conclusions:
FFRD resulted in Class II correction mainly through dentoalveolar effects and with minimal skeletal effects. Utilization of mini-implant anchorage effectively reduced the unfavorable proclination and intrusion of mandibular incisors but did not produce additional skeletal effects.
Keywords: Forsus Fatigue Resistant Device, Mini-implants, Class II malocclusion, Fixed functional, Anchorage
INTRODUCTION
Class II malocclusion is considered one of the most encountered problems in the orthodontic practice.1 Its prevalence was recently found to be between 15% and 30% in different populations.2–5 Mandibular deficiency was proven to be the most dominant component of this malocclusion.6,7
Treatment during the period of active growth depends mainly on redirection of mandibular growth, which can be achieved with a number of removable functional appliances. These appliances, however, have major limiting factors, including their dependence on patient compliance.8
The Herbst appliance was introduced in 1905 as a compliance-free Class II corrector; interest in this appliance was renewed by Pancherz in 1979.9 The Forsus Fatigue Resistant Device (FFRD) was introduced by Vogt in 2006.10 The author claimed that the FFRD was successful in the treatment of Class II division 1 malocclusion. However, the treatment effects were mainly dentoalveolar.1,11–16
Few studies and case reports have suggested the use of mini-implant anchorage in conjunction with fixed functional appliances to reduce the mandibular incisor proclination that compromised the skeletal effects.17–20 A recent trial21 was performed to test the efficiency of added mini-implant anchorage to FFRD using lateral cephalograms. However, conventional cephalograms present three-dimensional (3D) objects as two-dimensional (2D) images and are mainly based on excellent superimposition of the left and right sides, which is rarely accurate. The uncertainties in locating anatomical landmarks due to the deficiency of well-defined outlines and shadows are major drawbacks of 2D analysis.22
The aim of this clinical trial was to detect the 3D dental and skeletal changes associated with the use of indirect mini-implant anchorage with FFRD and to test the efficiency of this type of anchorage in obtaining skeletal rather than dentoalveolar effects.
MATERIALS AND METHODS
Subjects
The study method was approved by the Faculty of Dentistry Ethical Committee, Cairo University. Sample size calculation was done using G power software (Universität Düsseldorf, Düsseldorf, Germany), with an alpha value of .05 and a power of 80% based on the study by Weschler and Pancherz23 and revealed the need for 12 subjects per group. The patients and parents were informed about the nature of the study and informed consent forms were signed. The patients' eligibility criteria are shown in Table 1.
Table 1.
Eligibility Criteria of Patients Included in the Study
A computer-generated random list was created (https://www.random.org/), and allocation concealment was achieved with opaque sealed envelopes. The patients were randomly allocated into three groups: 16 patients were treated with FFRD (3M Unitek, Monrovia, Calif) (Forsus group), with a mean age of 13.25 ± 1.12 years; 15 patients received FFRD and lower mini-implants (FMI group), with mean age of 13.07 ± 1.41 years; and 15 untreated Class II subjects (12.71 ± 1.44 years) served as a control group.
Patient Attrition
None of the treatment groups' patients discontinued the trial. Two of the control patients wanted to start treatment immediately, and the third couldn’t be reached after 3 months. Thus, 12 subjects completed the observation period, and 31 subjects continued the clinical trial.
Methods
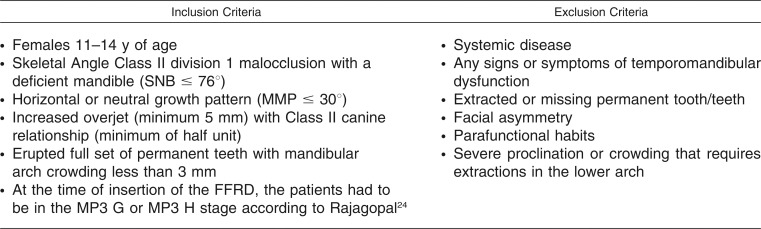
The 0.022-inch slot 3M MBT brackets were bonded to maxillary and mandibular arches, and a passive transpalatal arch was cemented to the maxillary first molars. Brackets of the mandibular canines and first premolars were bonded with exaggerated bracket tip to allow root divergence. Levelling and alignment proceeded until treatment reached a phase including 0.019 × 0.025-inch stainless-steel archwires. Wires were cinched distal to the maxillary and mandibular first molars. Periapical radiographs were taken for middle phalanges of the middle fingers of left hands of the patients at this stage to detect the MP3 stage of skeletal maturation according to Rajagopal24 (Figure 1). Cone beam computed tomographic (CBCT) images were obtained with an i-CAT CBCT unit (Imaging Sciences International, Hatfield, Pa). The first image (T1) was obtained immediately before insertion of FFRD and mini-implants in the two treatment groups.
Figure 1.
Periapical radiographs showing MP3 stages G (a) and H (b).
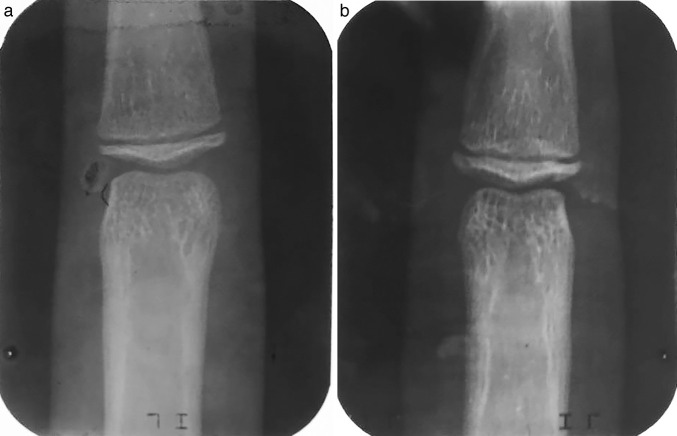
In the FMI group mini-implants (1.6 × 10 mm; 3M Unitek) were inserted under local anesthesia between the mandibular canines and first premolars according to AlSamak et al.,25 and 0.019 × 0.025-inch stainless-steel wire segments were used for fixation of the mini-implants to the mandibular arch and were bonded to the labial surface of the mandibular canines (Figure 2).
Figure 2.

The fixation wire used in the study.
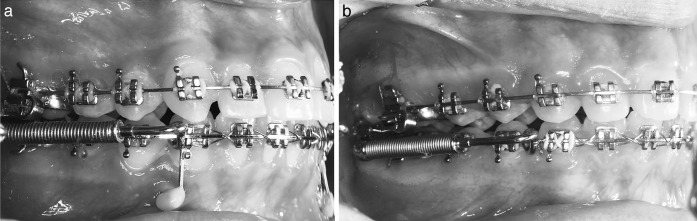
In both groups, selection of the proper size of the FFRD was done according to the manufacturer’s instructions. The pushrods of the appliance were inserted onto the mandibular archwires distal to the mandibular canines (Figure 3).
Figure 3.
Forsus Fatigue Resistant Device (FFRD) inserted in the FFRD and mini-implants (FMI) group (a) and Forsus group (b).
Follow up visits occurred every 3–4 weeks, and at these visits, the mini-implants and wire segments were checked for stability and the appliance was checked for activation. Split crimps were used for appliance activation, according to the manufacturer's instructions. Treatment was continued until overcorrection to an edge-to-edge incisor relationship was reached. The appliances and mini-implants were then removed and the second set of CBCT images (T2) was obtained.
The control group subjects were sent for uptake of the first CBCT image (T1) after inclusion in the study and random allocation. The observation period was 6.25 ± 1.06 months. The control subjects were then sent for uptake of the second images (T2), which were considered their pretreatment records. Orthodontic treatment was then performed on all patients in the control group.
CBCT Imaging and 3D Analysis
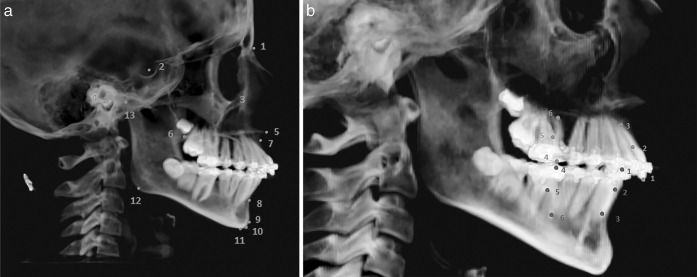
The analysis was done using Invivo Anatomage version 5.2 (Anatomage, San Jose, Calif). The assessors were blinded during the analysis. The analysis included skeletal and dental measurements (Figure 4; Table 2). The measurements were performed by the same observer twice and by another observer.
Figure 4.
(a) Skeletal landmarks used in the study: 1, Nasion; 2, Sella Turcica; 3, Orbitale; 4, Porion; 5, Anterior nasal spine; 6, Posterior nasal spine; 7, A point; 8, B point; 9, Pogonion; 10, Gnathion; 11, Menton; 12, Gonion; and 13, Condylion. (b) 1, Incisal tip of crown of maxillary/mandibular incisor; 2, Midroot of maxillary/mandibular incisor; 3, Root apex of maxillary/mandibular incisor; 4, Mesiobuccal cusp of maxillary/mandibular first molars; 5, Furcation point of maxillary/mandibular first molars; and 6, Mesiobuccal root apex of maxillary/mandibular first molars.
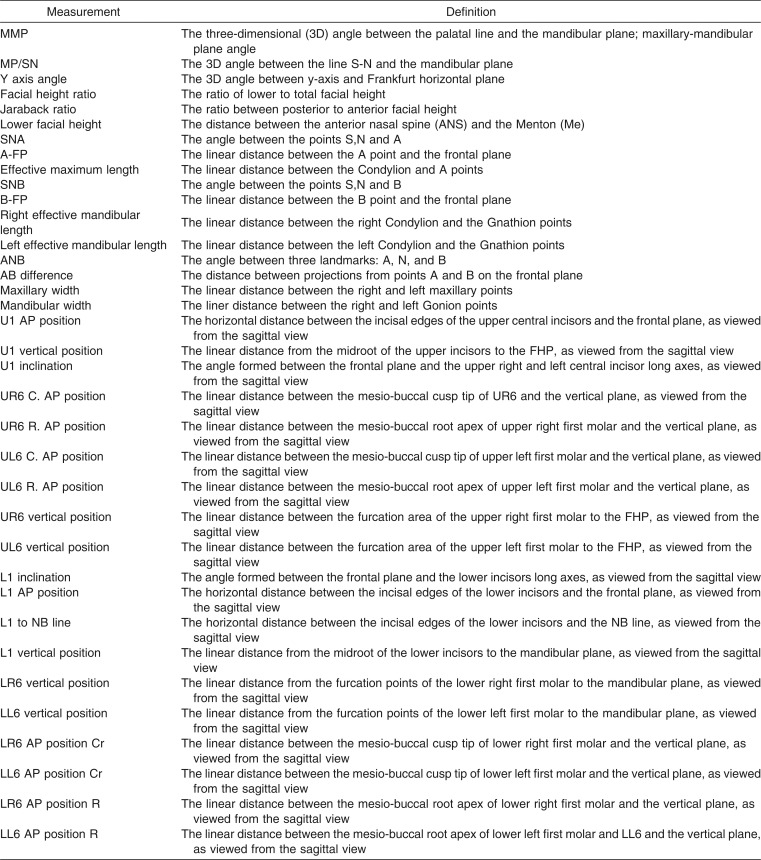
Table 2.
Definitions of the Included Measurements in the Study
Statistical Analysis
Analysis was performed with Statistical Package for the Social Sciences (SPSS) version 22.0 (SPSS Inc, Chicago, Ill) for Windows. Data were explored for normality using the Kolmogorov-Smirnov test. Concordance correlation coefficients (CCCs) were calculated to detect the intra- and interexaminer reliability of the used measurements. Paired t-tests were performed to detect the changes within each group. A one-way analysis of variance (ANOVA) test was used for comparing the mean changes among the three groups. Multiple-comparison Bonferroni tests were performed for the statistically significant ANOVA variables (P < .05) for pairwise comparisons among groups.
RESULTS
Clinical Results
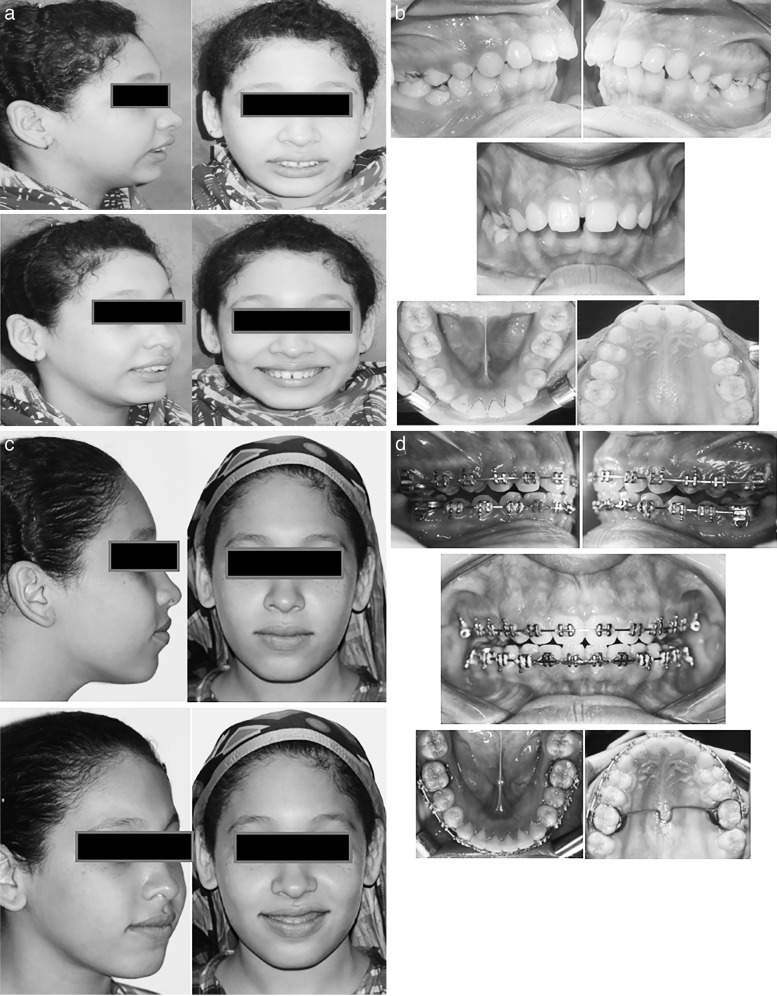
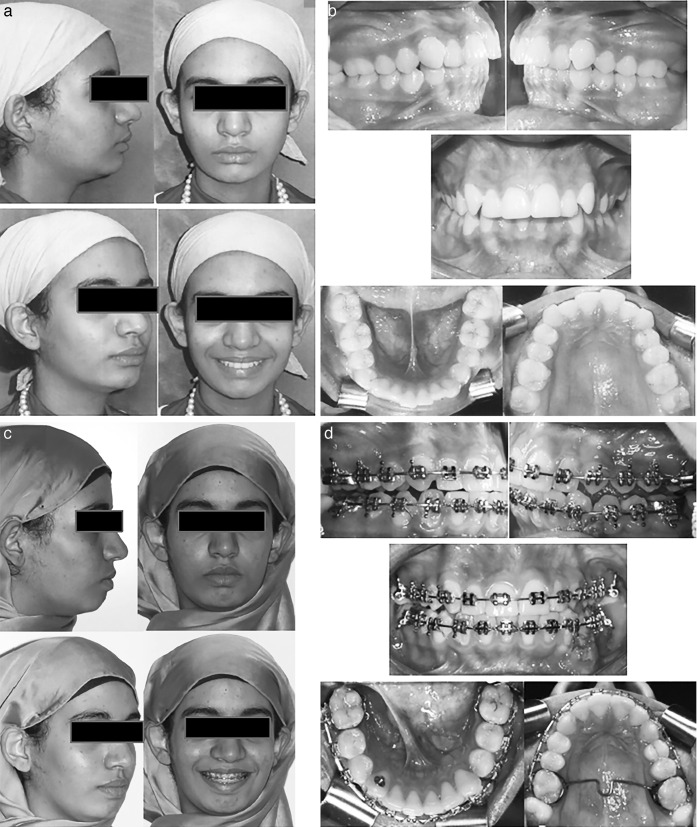
The FFRD was able to correct the Class II relationship to a dental Class I relationship (molar and canines) in 88% of the cases in a mean time of 5.34 ± 1.29 and 4.86 ± 1.32 months in the FMI and Forsus groups, respectively. There was a clinically significant improvement of the overbite, overjet, and soft tissue profile (Figures 5 and 6).
Figure 5.
Intraoral and extraoral photos of a Forsus group patient before and after treatment.
Figure 6.
Intraoral and extraoral photos of Forsus Fatigue Resistant Device and mini-implants (FMI) group patient before and after treatment.
Statistical Results of CBCT Analysis
Normality tests showed the data to be normally distributed. The CCC values ranged from good to excellent (0.721–0.974) in terms of intra- and interobserver agreement of the selected measurements at 95% confidence limits.
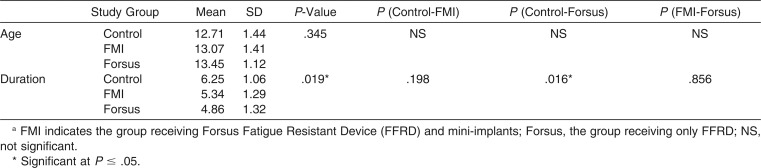
There were no statistically significant differences among the mean ages of the three groups. The control group observation period showed a statistically significant longer duration than the Forsus group (Table 3).
Table 3.
Comparison of Mean Ages and Duration of the Three Study Groups (One-Way Analysis of Variance [ANOVA] and Multiple Bonferroni Method Tests)a
Skeletal Changes (Tables 4 and 5)
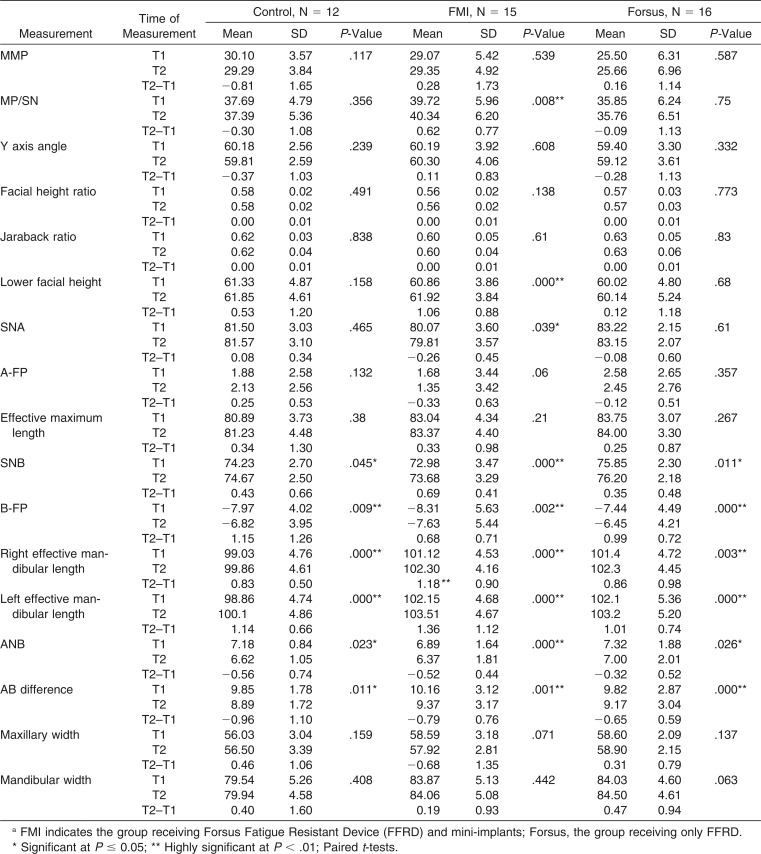
Table 4.
Mean Values of Parameters at the Beginning (T1) and End (T2) and the Mean Difference (T2-T1) of the Skeletal Measurements in the Three Study Groupsa
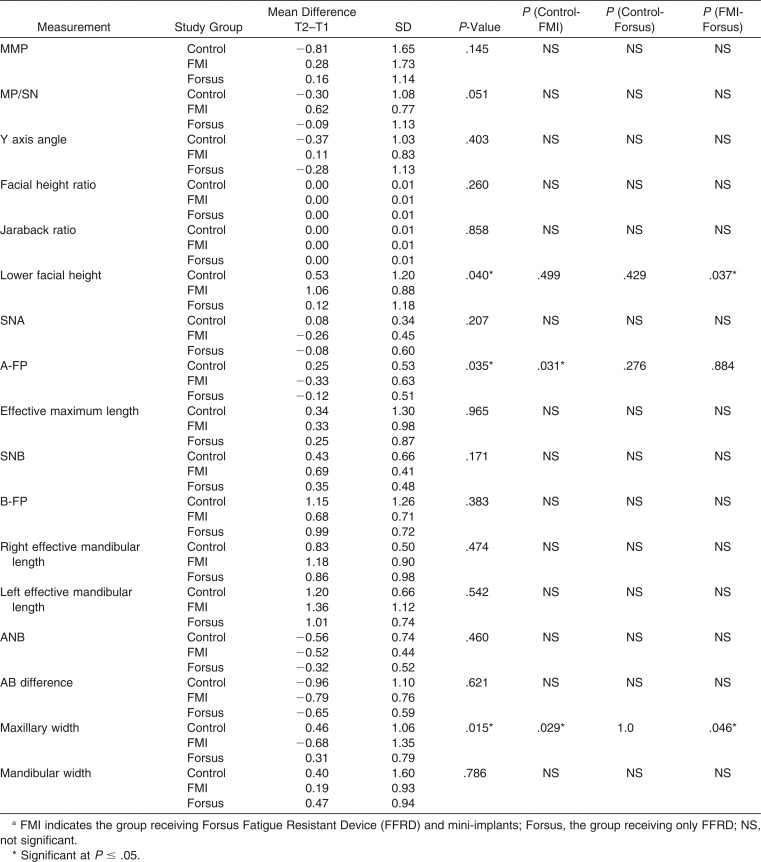
Table 5.
Comparison of the Mean Differences (T2-T1) for the Skeletal Measurements Among the Three Study Groups (One-Way Analysis of Variance [ANOVA] and Multiple Bonferroni Method Tests)a
Most of the vertical skeletal measurements did not change significantly with treatment in both groups. The lower facial height and MP/SN increased significantly only in the FMI group. SNA decreased significantly only in the FMI group. SNB, B-FP, and right and left effective mandibular lengths increased significantly in the three groups. The ANB and A-B difference decreased significantly in all groups. As for the transverse plane, maxillary and mandibular widths did not show statistically significant differences.
Upon comparing the three groups, the FMI group showed statistically significant maxillary retrusion (A-FP decreased by −0.33 ± 0.63 mm) and significant reduction in the maxillary width (−0.68 ± 1.35 mm).
Dentoalveolar Changes (Tables 6 and 7)
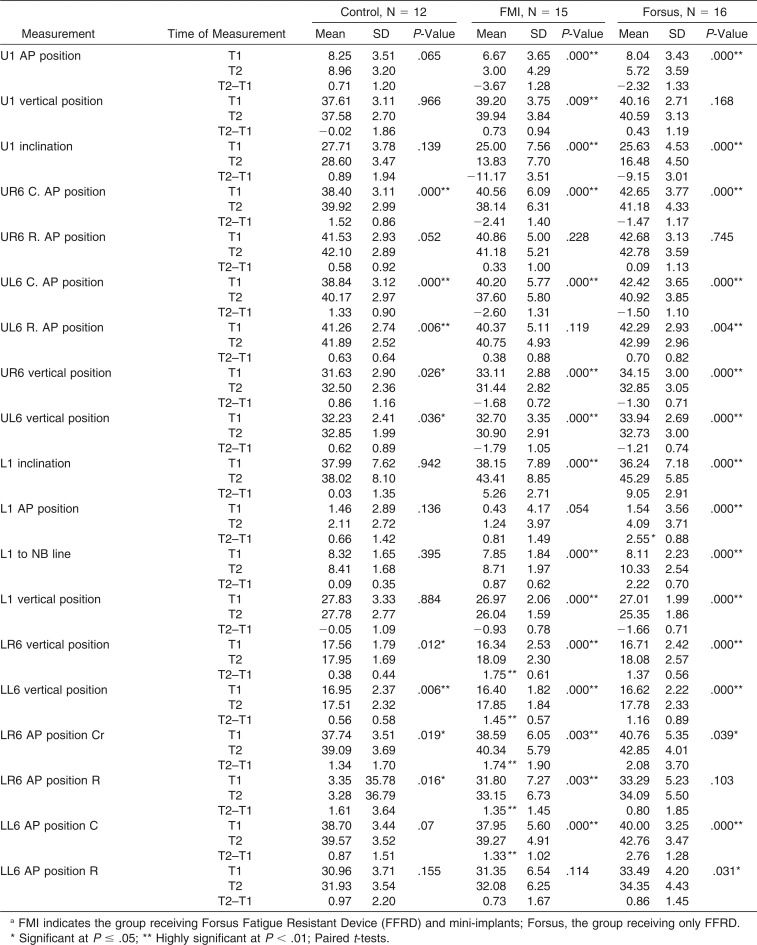
Table 6.
Mean Values of Parameters at the Beginning (T1) and End (T2) and the Mean Difference (T2-T1) of the Dento-Alveolar Measurements in the Three Study Groupsa
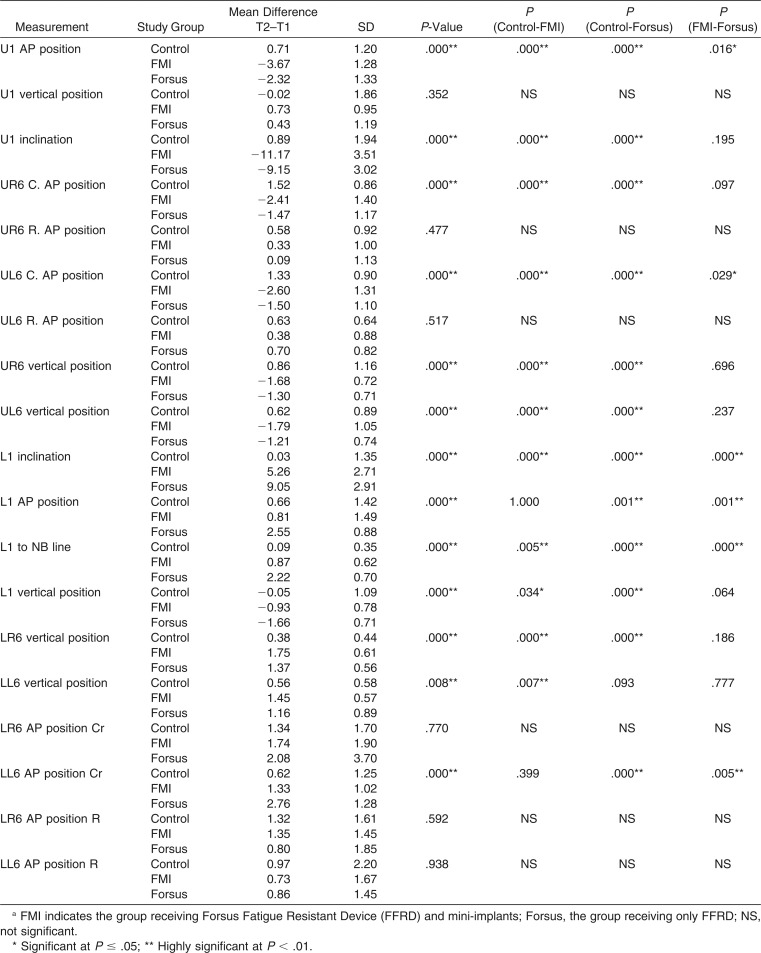
Table 7.
Comparison of the Mean Differences (T2-T1) for the Dento-Alveolar Measurements Among the Three Study Groups (One-Way Analysis of Variance [ANOVA] and Multiple Bonferroni Method Tests)a
Statistically significant retroclination of the maxillary incisors was evident in the FMI and Forsus groups as compared to the control group (−11.17° ± 3.51° and −9.15° ± 3.01°). The maxillary incisors were significantly extruded in the FMI group only.
The maxillary first molars significantly moved mesially in the control group in contrast to the FMI and Forsus groups, in which they significantly moved distally. The maxillary first molars showed significant extrusion in the control group and significant intrusion in the FMI and Forsus groups.
The mandibular incisors were significantly proclined (5.26° ± 2.71° and 9.05° ± 2.91° in the FMI and Forsus groups, respectively) and intruded in the treatment groups, as compared with the control group. In the Forsus group the mandibular incisors moved significantly forward more than in the other two groups (0.66 ± 1.42 mm, 0.81 ± 1.49 mm, and 2.55 ± 0.88 mm in the control, FMI, and Forsus groups, respectively).
The mandibular first molars were significantly extruded and moved in a mesial direction in the three groups. The mesialization was shown to be most significant in the Forsus group.
DISCUSSION
The subjects included in the study were Class II division 1 females, with the exclusion of Class II division 2, which was proven to be a separate entity that differs from Class II division 1.26 A previous trial21 included male and female subjects, who have different growth patterns and rates,27 having Class II division 1 and 2 occlusions, which might have led to questionable results.
To overcome the drawback of unreliable chronological age as an indicator of skeletal maturation stage,28 the MP3 staging method was used according to Rajagopal,24 and only the MP3 G and H stage patients were included. An untreated control group was included in order to compare the results of the fixed functional phase in the FMI and Forsus groups with the effect of the normal growth, as was previously recommended.29,30 Previous noncontrolled trials16,31 mentioned that they could not assess whether the skeletal changes were due to growth or treatment.
The vertical changes showed that the FMI group had a significant increase in the MP/SN angle, which cannot be considered clinically significant (MP/SN increased by 0.68° ± 0.77°). However, both Forsus and FMI groups showed a statistically significant intrusion for the maxillary first molars, which was greater in the FMI group (1.3 mm and 1.78 mm, respectively). The molar intrusion was also evident in previous studies12 but was not reported in others.21,32 This was coupled with the significant mandibular molar extrusion that was reported in both treatment groups (more in the FMI group). It could be considered that the intrusive effect on the maxillary molars was compensated for by the extrusion of the mandibular ones. The remaining factor was the more significant maxillary molar distalization in the FMI group due to the redistribution of forces to the maxilla after the addition of mini-implants (mean of 2.5 mm) that was proven in the literature to cause more bite opening.33
As for the antero-posterior skeletal changes, there was a significant reduction of the SNA and ANB angles together with a significant increase in SNB and effective mandibular length in both treatment groups. The occurrence of the same findings in the control group negated the effect of appliances as a driver for these skeletal changes. These results were in agreement with those of other studies1,15,16,21 and in disagreement with the findings of Jones et al.,32 who reported 4.4 mm of mesial mandibular movement, which could be attributable to their use of the Pitchfork analysis that was previously proven to be inaccurate.34 The one significant skeletal effect over the control group was the headgear effect produced by the FFRD in both treatment groups.
The mean of distal movement of the maxillary molars and distalization of the anterior dentition were significantly greater in the FMI group. Retroclination of maxillary incisors was significant enough to cause a subsequent lock of occlusion that prohibited the creation of a Class I canine relationship in 12% of the cases. These findings were in agreement with those of Aslan et al.21 Another study32 reported mesial movement of the maxillary molars with the FFRD. Cacciatore et al.16 reported 0.7 mm of distal movement of the maxillary molars after FFRD therapy.
Regarding the mandibular incisor changes, the introduction of mini-implants with rigid attachment to the mandibular canines in the current study resulted in remarkable favorable changes in limiting the proclination of the mandibular incisors. It was confirmed by the change in their antero-posterior position (0.81 mm in the FMI group and 2.55 mm in the Forsus group). These results were in agreement with those of Aslan et al.,21 who reported more limited proclination of mandibular incisors (3.6° ± 5.07° and 9.3° ± 3.8° in the FMI and Forsus groups, respectively). Both treatment groups showed significant intrusion of the mandibular incisors, which was less in the FMI group (0.93 mm) than in the Forsus group (1.61 mm).
In the current study, the pushrod was inserted distal to the mandibular canines and led to 9.3° of proclination of mandibular incisors in the Forsus group. However, Cacciatore et al.16 placed the pushrod distal to the mandibular first premolars, which resulted in a mean of 5° of mandibular incisor proclination. This may give rise to the question of whether the distal placement of the pushrod could have resulted in reduction of the unwanted mandibular incisor mesial movement; this question requires further studies.
As for the mandibular first molars, significant mesialization was only reported for the Forsus group, versus the other two groups (mean of 2.76 mm), which could be explained by the significantly greater mandibular incisor proclination, which in turn created more space for the mandibular molars to tip mesially.
The incorporation of mini-implants with FFRD reduced the mandibular incisor proclination but could not lead to additional increase in the mandibular growth. It led to significant restriction of maxillary growth and distalization of the maxillary dentition. This might shed light on the indications of this modality in patients with mild to moderate dento-alveolar maxillary excess.
CONCLUSIONS
FFRD was successful in treatment of Class II division 1 malocclusion through dentoalveolar changes and minimal significant skeletal changes.
The use of mini-implants with FFRD could not produce significant additional sagittal skeletal effects.
The incorporation of mini-implants with FFRD decreased the mandibular dentoalveolar side effects and increased the distalizing effects of the appliance on the maxillary arch.
REFERENCES
- 1.Oztoprak M, Nalbantgil D, Uyanlar A, Arun T. A cephalometric comparative study of Class II correction with Sabbagh Universal Spring 2 and Forsus Fatigue Resistant Device appliances. Eur J Dent. 2012;6:302–310. [PMC free article] [PubMed] [Google Scholar]
- 2.Vásquez M, Baccetti T, Franchi L, McNamara JA., Jr Dentofacial features of Class II malocclusion associated with maxillary skeletal protrusion: a longitudinal study at the circumpubertal growth period. Am J Orthod Dentofacial Orthop. 2009;135:568.e1–568.e7. doi: 10.1016/j.ajodo.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 3.Silva R, Kang D. Prevalence of malocclusion among Latino adolescents. Am J Orthod Dentofacial Orthop. 2001;119:313–315. doi: 10.1067/mod.2001.110985. [DOI] [PubMed] [Google Scholar]
- 4.Lew K, Foong W, Loh E. Malocclusion prevalence in an ethnic Chinese population. Aust Dent J. 1993;38:442–449. doi: 10.1111/j.1834-7819.1993.tb04759.x. [DOI] [PubMed] [Google Scholar]
- 5.Garner L, Butt M. Malocclusion in black Americans and Nyeri Kenyans: an epidemiologic study. Angle Orthod. 1985;55:139–146. doi: 10.1043/0003-3219(1985)055<0139:MIBAAN>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.McNamara JA., Jr Components of Class II malocclusion in children 8–10 years of age. Angle Orthod. 1981;51:177–202. doi: 10.1043/0003-3219(1981)051<0177:COCIMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Perillo L, Padricelli G, Isola G, Femiano F, Chiodono P, Matarese G. Class II malocclusion division 1: a new classification method by cephalometric analysis. Eur J Paediatr Dent. 2012;13:192–196. [PubMed] [Google Scholar]
- 8.McSherry PF, Bradley H. Class II correction-reducing patient compliance: a review of the available techniques. J Orthod. 2000;27:219–225. doi: 10.1179/ortho.27.3.219. [DOI] [PubMed] [Google Scholar]
- 9.Pancherz H. Treatment of Class II malocclusions by jumping the bite with the Herbst appliance. A cephalometric investigation. Am J Orthod. 1979;76:423–442. doi: 10.1016/0002-9416(79)90227-6. [DOI] [PubMed] [Google Scholar]
- 10.Vogt W. The Forsus Fatigue Resistant Device. J Clin Orthod. 2006;40(6):368–377. [PubMed] [Google Scholar]
- 11.Franchi L, Alvetro L, Giuntini V, Masucci C, Defraia E, Baccetti T. Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in Class II patients. Angle Orthod. 2011;81:678–683. doi: 10.2319/102710-629.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gunay E, Arun T, Nalbantgilc D. Evaluation of the immediate dentofacial changes in late adolescent patients treated with the Forsus Fatigue Resistant Device. Eur J Dent. 2011;5:423–432. [PMC free article] [PubMed] [Google Scholar]
- 13.Bilgiç F, Hamamci O, Başaran G. Comparison of the effects of fixed and removable functional appliances on the skeletal and dentoalveolar structures. Aust Orthod J. 2011;27:110–116. [PubMed] [Google Scholar]
- 14.Mahamad I, Neela P, Mascarenhas R, Husain A. A comparison of Twin-block and Forsus Fatigue Resistant Device functional appliance. A cephalometric study. Int J Orthod Milwaukee. 2012;23:49–58. [PubMed] [Google Scholar]
- 15.Bilgiç F, Başaran G, Hamamci O. Comparison of Forsus FRD EZ and Andresen activator in the treatment of Class II, division 1 malocclusions. Clin Oral Investig. 2015;19(2):445–451. doi: 10.1007/s00784-014-1237-y. [DOI] [PubMed] [Google Scholar]
- 16.Cacciatore G, Alvetro L, Defraia E, Ghislanzoni L, Franchi L. Active-treatment effects of the Forsus Fatigue Resistant Device during comprehensive Class II correction in growing patients. Korean J Orthod. 2014;44:136–142. doi: 10.4041/kjod.2014.44.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manni A, Pasini M, Mauro C. Comparison between Herbst appliances with or without miniscrew anchorage. Dent Res J. 2012;9:S216–S222. doi: 10.4103/1735-3327.109762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gandedkar N, Revankar A, Ganeshkar S. Correction of a severe skeletal Class II occlusion with a fixed functional appliance anchored on mini-implants: a patient report. World J Orthod. 2010;11:369–379. [PubMed] [Google Scholar]
- 19.Luzi C, Luzi V, Carletti P, Melsen B. The Miniscrew-Anchored Herbst—a case report. J Clin Orthod. 2012;46:399–405. [PubMed] [Google Scholar]
- 20.Luzi C, Luzi V. Skeletal Class II treatment with the miniscrew-anchored Herbst. Orthod Fr. 2013;84:307–318. doi: 10.1051/orthodfr/2013070. [DOI] [PubMed] [Google Scholar]
- 21.Aslan B, Kucukkaraca E, Turkoz C, Dincer M. Treatment effects of the Forsus Fatigue Resistant Device used with miniscrew anchorage. Angle Orthod. 2014;84:76–87. doi: 10.2319/032613-240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karatas OH, Toy E. Three-dimensional imaging techniques: a literature review. Eur J Dent. 2014;8:132–140. doi: 10.4103/1305-7456.126269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weschler D, Pancherz H. Efficiency of three mandibular anchorage forms in Herbst treatment: a cephalometric investigation. Angle Orthod. 2004;75:23–27. doi: 10.1043/0003-3219(2005)075<0023:EOTMAF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Rajagopal S. A comparison of modified MP3 stages and the cervical vertebrae as growth indicators. J Clin Orthod. 2002;36:398–406. [PubMed] [Google Scholar]
- 25.AlSamak S, Psomiadis S, Gkantidis N. Positional guidelines for orthodontic mini-implant placement in the anterior alveolar region: a systematic review. Int J Oral Maxillofac Implants. 2013;28:470–479. doi: 10.11607/jomi.2659. [DOI] [PubMed] [Google Scholar]
- 26.Al-Khateeb E, Al-Khateeb S. Anteroposterior and vertical components of Class II division 1 and division 2 malocclusion. Angle Orthod. 2009;79:859–866. doi: 10.2319/062208-325.1. [DOI] [PubMed] [Google Scholar]
- 27.Chung C, Wong W. Craniofacial growth in untreated skeletal Class II subjects: a longitudinal study. Am J Orthod Dentofacial Orthop. 2002;122:619–626. doi: 10.1067/mod.2002.129195. [DOI] [PubMed] [Google Scholar]
- 28.Hägg U, Taranger J. Maturation indicators and the pubertal growth spurt. Am J Orthod. 1982;82:299–309. doi: 10.1016/0002-9416(82)90464-x. [DOI] [PubMed] [Google Scholar]
- 29.Riesmeijer A, Prahl-Andersen B, Mascarenhas A, Joo B, Vig K. A comparison of craniofacial Class I and Class II growth patterns. Am J Orthod Dentofacial Orthop. 2004;125:463–471. doi: 10.1016/j.ajodo.2003.05.012. [DOI] [PubMed] [Google Scholar]
- 30.Stahl F, Baccetti T, Franchi L, McNamara JA., Jr Longitudinal growth changes in untreated subjects with Class II division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2008;134:125–137. doi: 10.1016/j.ajodo.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 31.Aras A, Ada E, Saracoğlu H, Gezer N, Aras I. Comparison of treatments with the Forsus Fatigue Resistant Device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2011;140:616–625. doi: 10.1016/j.ajodo.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 32.Jones G, Buschang P, Kim K, Oliver D. Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. Angle Orthod. 2008;78:332–338. doi: 10.2319/030607-115.1. [DOI] [PubMed] [Google Scholar]
- 33.Fuziy A, Rodrigues, de Almeida R, Janson G, Angelieri F, Pinzan A. Sagittal, vertical, and transverse changes consequent to maxillary molar distal movement with the pendulum appliance. Am J Orthod Dentofacial Orthop. 2006;130:502–510. doi: 10.1016/j.ajodo.2004.12.031. [DOI] [PubMed] [Google Scholar]
- 34.Mannchen R. A critical evaluation of the Pitchfork analysis. Eur J Orthod. 2001;23:1–14. doi: 10.1093/ejo/23.1.1. [DOI] [PubMed] [Google Scholar]