Abstract
Objective:
To evaluate the changes in nasal mucociliary clearance in orthodontic patients after rapid maxillary expansion (RME) therapy.
Materials and Methods:
Forty-two children (25 boys and 17 girls) participated in this study. The RME group consisted of 21 patients (mean age, 13.8 years), who had undergone RME at the initiation of orthodontic treatment. The control group consisted of 21 subjects (mean age, 13.6 years), who were attending the department of orthodontics for active orthodontic treatment. The nasal mucociliary clearance was assessed by the saccharin test. Saccharin transit times (STTs) were measured for each treated subject before expansion (T1), after RME (T2), and after a 3-month retention period (T3). Records were obtained at the same time intervals for each group.
Results:
The STT decreased significantly in the RME group after expansion and retention (P < .05). A statistically significant difference was found when the STTs of the control and RME groups were compared after expansion and retention (P < .05).
Conclusions:
The STTs of young orthodontic patients with maxillary narrowness and without any history of nasal or systemic disease were within normal limits. However, RME increased the mucociliary clearance in patients who had maxillary narrowness, having positive effects on nasal physiology and increasing nasal cavity volume.
Keywords: Rapid maxillary expansion, Nasal mucociliary clearance, Saccharin transit time
INTRODUCTION
Rapid maxillary expansion (RME) has been widely used for the correction of maxillary width deficiency and posterior crossbite by opening the midpalatal suture. This method was first described by Angell1 in 1860 and popularized by Haas2 100 years later. Since then, it has become a conventional orthodontic treatment method, and many studies have been performed to evaluate its orthopedic as well as its orthodontic effects. The concept of RME was extended to the nasal cavity because it was suggested that, with the expansion, increases in nasal width and volume are obtained.3–6 Previous studies showed that this increase in nasal volume decreases nasal resistance and improves air flow.7–10 However, the effect of these changes on the quality of nasal respiration in orthodontic patients has not been fully investigated. The nasal cavity is specifically designed to prepare the air before it passes into the lungs.11 It is believed that nasal breathing contributes to the development of the nasofacial complex and benefits overall health.12
Mucociliary clearance (MCC) plays a pivotal role in defending the respiratory system from the nose and upper airways to the lower respiratory tract. Cleaning foreign particles over the respiratory mucosa and keeping this mucosa moist are necessary for the normal physiology of the nose. These abilities of the respiratory mucosa depend on effective ciliary activity and renewing of airway secretions. These are known as mucociliary activity, and MCC is the most important defense function of the upper and lower respiratory tracts.13 There are several methods of evaluating MCC. The saccharin test is one of the simplest, fastest, cheapest, and most reliable methods used for measuring MCC.14
The effect of RME on nasal MCC in orthodontic patients has not been studied. The purpose of this study was to evaluate the changes in nasal MCC after RME therapy.
MATERIALS AND METHODS
This study was approved by the Cumhuriyet University Human Ethics Committee (Confirmation No. 2012-08/06). Informed consent was obtained from all participants and their parents.
The sample consisted of 42 patients who sought orthodontic treatment at the Department of Orthodontics of Cumhuriyet University. Inclusion criteria included a transverse maxillary deficiency, bilateral posterior crossbite, no previous orthodontic treatment, and no history of nasal or systemic disease. Furthermore, the presence of adequate nasal anatomy and cavity spaces was confirmed by anterior rhinoscopic examination by a single qualified otolaryngologist. Patients having the following conditions were excluded from the study: diabetes mellitus, allergic rhinitis, chronic sinusitis, nasal polyposis, concha bullosa, turbinate hypertrophy, upper respiratory tract infection, and patients who had become ill with rhinosinusitis in the prior 2 weeks.
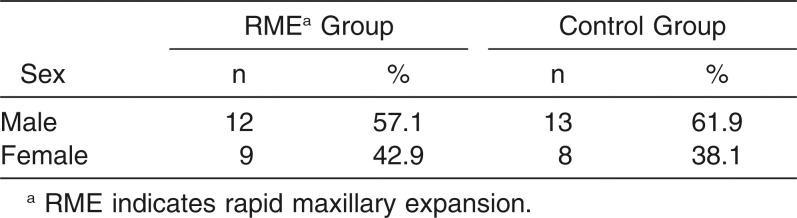
The RME group consisted of 21 patients (mean age, 13.83 years; range, 11 to 16), who had undergone bonded acrylic cap splint RME at the initiation of their orthodontic treatment. This group consisted of 12 boys (57.1%) and 9 girls (42.9%). The control group consisted of 21 subjects (mean age, 13.65 years; range, 10 to 16), of which 13 were boys (61.9%) and 8 were girls (38.1%) (Table 1). This group was attending the Department of Orthodontics of Cumhuriyet University and receiving active orthodontic treatment. The control group patients were not subjected to any interventional procedures during the study period. Power analysis carried out to determine the number of patients in the study groups led to the decision to include 20 patients in each group (α = 0.05, β = 0.10, and 1−β = 80). Having a total of 40 patients as a sample size was thought be statistically appropriate. The power of the test was found to be P = .93995. All subjects and their parents volunteered for the study. Table 1 shows the distribution of the two groups according to gender.
Table 1.
Distribution of Patients by Group According to Gender
A bonded acrylic cap splint RME appliance containing a hyrax screw (Dentaurum, Pforzheim, Germany) was used to correct the posterior crossbite in the treated subjects. The screw was activated two turns a day until the occlusal aspect of the lingual cusp of the maxillary first molars contacted the occlusal aspect of the facial cusp of the mandibular first molars. At that time, the screw was fixed with 0.014-inch ligature wire, and the appliance left for 1 week to minimize discomfort during removal. The expansion time was 2 or 3 weeks, with 6 mm–10 mm of activation. After removal, a Hawley-type removable retention appliance was used for 3 months.
Nasal MCC was assessed by the saccharin test, which was performed on all subjects as described by Nakagawa et al.15 Briefly, a 5-mg particle of saccharin was placed 2 cm inside the nonobstructed nostril on the inferior turbinate under visual control. The participant remained seated with his or her head tipped slightly forward while breathing normally (not forced), without sneezing or blowing the nose and without taking any substances that might interfere with the test. A timer was displayed to measure the transit time. Subjects were told to indicate when they noted any particular taste. The actual taste they were to expect was not specified in order to avoid false positives. Saccharin transit time (STT) is the time elapsed from the placement of the particle until the subject reports the sweet taste of saccharin. All the data were obtained by the same otolaryngologist for each treated subject before RME (T1), after RME (T2), and after 3 months of retention (T3). The records were obtained at the same time intervals for each group. All the saccharin test measurements were done under the same room conditions to avoid environmental effects.
Statistical Analysis
Data was obtained for each saccharin test at T1, T2, and T3 for both the treated and the control group. The results were calculated using the software SPSS for Windows (release 15.0, SPSS Inc, Chicago, Ill). The mean differences between groups were studied using the unpaired t test according to time intervals. A repeated analysis of variance (ANOVA) was performed to compare differences according to time intervals. The Bonferroni test was performed to determine which time interval would show the difference. The level of statistical significance was established at P = .05.
RESULTS
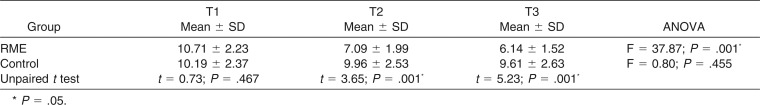
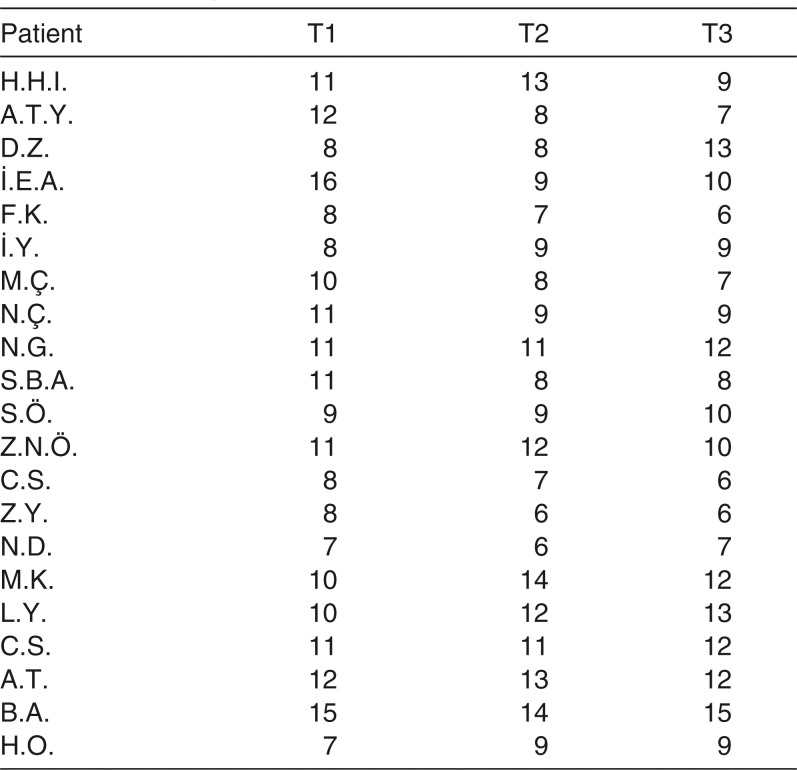
There was no statistically significant difference between the groups according to age (P = .648) or gender (P = .53). The STT in the RME group had decreased significantly after expansion (T2; P < .05), and it continued to decrease during the retention period (T3); however, this decrease is not statistically significant according to T2 (P > .05). The STT did not decrease significantly in the control group during the study period (P > .05). A statistically significant difference was found when the STT of the control and RME groups were compared after expansion and retention (P < .05; Table 2).
Table 2.
Saccharin Transport Times (Min) of Groups According to Time Intervals
DISCUSSION
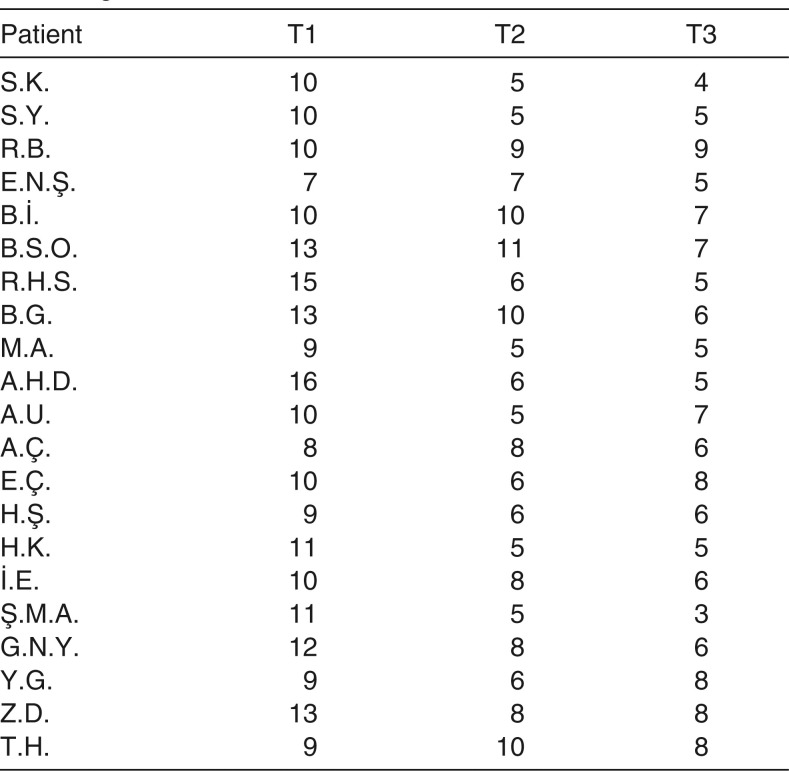
The maxillary bones form approximately 50% of the nasal cavity's anatomic structure. Therefore, treatment modalities that alter the morphology of the maxillary dental arch, such as RME whose effects have been noted in the midpalatal suture as well as in the neighboring structures such as the internasal, nasomaxillary, and frontomaxillary sutures, can affect the geometry and function of the nasal cavity.5,16 Previous investigators have reported that RME changes the nasal cavity's anatomy with an increase in nasal volume, which in turn decreases nasal airway resistance and establishes predominant nasal respiration.7,8,17,18 However, the effect of these changes on nasal MCC has not been truly understood. Wertz3 reported that no justification for airway enlargement existed for RME unless an obstruction was present in the anteroinferior aspect of the nose, the area most affected by RME. On the other hand, RME has been suggested as a treatment option for rhinostenosis caused by a septal deformity, nasal infection, allergic rhinitis, and obstructive sleep apnea,19,20 which were reported as having prolonged STTs.21–24 In our study, STT was decreased after both expansion and retention in the RME group, compared with the control group (Table 2). It is possible that this is primarily the result of improved mucociliary function, which in turn is due to the increase in nasal cavity volume, decrease in nasal resistance, and improvement in air flow after RME.
Table 3.
Saccharin Transport Times (Min) of RME Group According to Time Intervals
The saccharin test and rhinoscintigraphy are the most commonly used techniques for measuring nasal MCC. Tc-99m-MAA is the most popular radiopharmaceutical used in rhinoscintigraphy.25 Although rhinoscintigraphy is a reliable and easily reproducible technique, it has potential side effects. Therefore, in our study, we used the saccharin test to evaluate nasal MCC, which varies with location, climate, exposure to tobacco smoke, and environmental pollutants.26 Standardization of room conditions and environmental factors during the saccharin test is important for the reliability of results. To standardize the temperature, humidity, and atmospheric pressure among subjects, we carried out the study within the same city with the same climate, partial atmospheric pressure, and room conditions. Patient selection was the other issue. The subjects were selected from a group of healthy, young orthodontic patients with narrow maxillas. Changes in medical and systemic conditions and patients' nasal health were examined by the same otolaryngologist before each measurement.
Table 4.
Saccharin Transport Times (Min) of Control Group Patients According to Time Intervals
MCC is an important factor in normal nasal function. It is the first line of airway defense against noxious stimuli in the environment. Inhaled particles are trapped within the mucus of the airways and are transported to the pharynx by ciliary motion. Then they are either swallowed or coughed up.27 Normal nasal MCC time of children is in the range of 9.96 ± 2.61 minutes in the orthostatic (upright) position.28 Lale et al.26 concluded that the average STT for an adult free from nasal disease is 7–15 minutes. They also concluded that patients who have prolonged MCC time—greater than 19 minutes—have a disturbed nasal MCC. On the other hand, improvement in nasal MCC decreases the STT. Homer et al.27 reported that 5% hypertonic saline douching solutions and isotonic saline solutions improve mucociliary clearance more than 3% in normal healthy subjects. Our results show that there is a negative correlation between increase in nasal cavity volume and decrease in STT after RME and retention.
Nasal mucus provides a continuous blanketlike lining in the nasal cavity onto which particles in the turbulent inhaled airstream impact and stick; 80% of particles larger than 12.5 µm are filtered from the air before they reach the pharynx.26 This property of respiratory mucosa depends on effective ciliary activity and renewal of airway secretions. MCC may be disturbed under a variety of conditions that affect ciliary activity, including smoking. Although the STT of passive smokers is within normal limits, nonsmokers, who have a healthier nasal ciliary epithelium than smokers, have a lower STT.29 Cazzolla et al.30 reported that the risk of respiratory infections was reduced in mouth-breathing children due to normalization of upper airway function after RME. In our study, initial MCC times are within normal limits in both the RME and control groups (Table 2). However, STT was lower after RME and the retention period in the RME group compared with the control group. These results reveal that RME improves MCC, which is a fundamental function required to maintain the health and protective functions of the nose.
The results of this study show that otolaryngologists should seek an orthodontic consultation for their patients with upper airway problems and maxillary narrowness to improve nasal breathing with RME. Furthermore, these patients will, in all probability, have an orthodontic indication. Further studies are required using larger groups including long-term results for better understanding the relation between nasal breathing and RME therapy.
CONCLUSIONS
The STTs of young orthodontic patients with maxillary narrowness and with no history of nasal or systemic disease are within normal limits.
However, increasing nasal cavity volume by RME increases the MCC in patients with maxillary narrowness, resulting in positive effects on nasal physiology.
REFERENCES
- 1.Angell EC. Treatment of irregularities of the permanent or adult teeth. Dent Cosmos. 1860;1:540–544. [Google Scholar]
- 2.Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961;31:73–90. [Google Scholar]
- 3.Wertz RA. Changes in nasal airflow incident to rapid maxillary expansion. Angle Orthod. 1968;38:1–11. doi: 10.1043/0003-3219(1968)038<0001:CINAIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Warren DW, Hershey GH, Turvey TA, Hinton VA, Hairfield WM. The nasal airway following maxillary expansion. Am J Orthod Dentofacial Orthop. 1987;91:111–116. doi: 10.1016/0889-5406(87)90467-7. [DOI] [PubMed] [Google Scholar]
- 5.El H, Palomo JM. Three-dimensional evaluation of upper airway following rapid maxillary expansion: a CBCT study. Angle Orthod. 2014;84(2):265–273. doi: 10.2319/012313-71.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iwasaki T, Saitoh I, Takemoto Y, Inada E, Kanomi R, Hayasaki H, Yamasaki Y. Improvement of nasal airway ventilation after rapid maxillary expansion evaluated with computational fluid dynamics. Am J Orthod Dentofacial Orthop. 2012;141(3):269–278. doi: 10.1016/j.ajodo.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 7.Doruk C, Sökücü O, Bicakci AA, Yilmaz U, Taş F. Comparison of nasal volume changes during rapid maxillary expansion using acoustic rhinometry and computed tomography. Eur J Orthod. 2007;29:251–255. doi: 10.1093/ejo/cjl069. [DOI] [PubMed] [Google Scholar]
- 8.Babacan H, Sokucu O, Doruk C, Ay S. Rapid maxillary expansion and surgically assisted rapid maxillary expansion effects on nasal volume. Angle Orthod. 2006;76:66–71. doi: 10.1043/0003-3219(2006)076[0066:RMEASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Magnusson A, Bjerklin K, Nilsson P, Jönsson F, Marcusson A. Nasal cavity size, airway resistance, and subjective sensation after surgically assisted rapid maxillary expansion: a prospective longitudinal study. Am J Orthod Dentofacial Orthop. 2011;140(5):641–651. doi: 10.1016/j.ajodo.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 10.Oliveira De Felippe N, Da Silveira A, Viana G, Kusnoto B, Smith B, Evans C. Relationship between rapid maxillary expansion and nasal cavity size and airway resistance: short– and longterm effects. Am J Orthod Dentofacial Orthop. 2008;134:370–382. doi: 10.1016/j.ajodo.2006.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Keller JL, Kacker A. Choanal atresia, charge association, and congenital nasal stenosis. Otolaryngol Clin North Am. 2000;33:1343–1351. doi: 10.1016/s0030-6665(05)70285-1. [DOI] [PubMed] [Google Scholar]
- 12.McDonald JP. Airway problems in children: can the orthodontist help. Ann Acad Med Singapore. 1995;24:158–162. [PubMed] [Google Scholar]
- 13.Timms DJ. The reduction of nasal airway resistance by rapid maxillary expansion and its effects on respiratory disease. J Laryngol Otol. 1984;98:357–362. doi: 10.1017/s0022215100146730. [DOI] [PubMed] [Google Scholar]
- 14.Andersen IB, Camner P, Jensen Pl, Philipson K, Proctor DF. A comparison of nasal and tracheobronchial clearance. Arch Environ Health. 1974;29:290–293. doi: 10.1080/00039896.1974.10666589. [DOI] [PubMed] [Google Scholar]
- 15.Nakagawa NK, Franchini ML, Driusso P, Oliveira LR, Saldiva PHN, Lorenzi-Filho G. Mucociliary clerance is impaired in acutely ill patients. Chest. 2005;128:2772–2777. doi: 10.1378/chest.128.4.2772. [DOI] [PubMed] [Google Scholar]
- 16.Habersack K, Karoglan A, Sommer B, Benner KU. High resolution multislice computerized tomography with multiplanar and 3-dimensional reformation imaging in rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2007;131:776–781. doi: 10.1016/j.ajodo.2005.09.030. [DOI] [PubMed] [Google Scholar]
- 17.Palaisa J, Ngan P, Martin C, Razmus T. Use of conventional tomography to evaluate changes in the nasal cavity with rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2007;132:458–466. doi: 10.1016/j.ajodo.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 18.Ribeiro ANC, de Paiva JB, Rino-Neto J, Illipronti-Filho E, Trivino T, Mongelli Fantini S. Upper airway expansion after rapid maxillary expansion evaluated with cone beam computed tomography. Angle Orthod. 2012;82:458–463. doi: 10.2319/030411-157.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Timms DJ. Rapid maxillary expansion in the treatment of nasal obstruction and respiratory disease. Ear Nose Throat J. 1987;66:242–247. [PubMed] [Google Scholar]
- 20.Gray LP. Rapid maxillary expansion and impaired nasal respiration. Ear Nose Throat J. 1987;66:248–251. [PubMed] [Google Scholar]
- 21.Nuutinen J, Rauch-Toskala E, Saano V. Ciliary beating frequency in chronic sinusitis. Arch Otolaryngol Head Neck Surg. 1993;119:645–647. doi: 10.1001/archotol.1993.01880180061011. [DOI] [PubMed] [Google Scholar]
- 22.Stanley PJ, Wilson R, Greenstone MA, Mackay IS, Cole PJ. Abnormal nasal mucociliary clearance in patients with rhinitis and its relationship to concomitant chest disease. Br J Dis Chest. 1985;79:77–82. doi: 10.1016/0007-0971(85)90010-5. [DOI] [PubMed] [Google Scholar]
- 23.Djukanovic R. Nasal polyps: a model for chronic mucosal inflammation. Clin Exp Allergy. 1995;25:582–585. doi: 10.1111/j.1365-2222.1995.tb01104.x. [DOI] [PubMed] [Google Scholar]
- 24.Wanner A, Salathé M, O’Riordan TG. Mucociliary clearance in the airways. Am J Respir Crit Care Med. 1996;154:1868–1902. doi: 10.1164/ajrccm.154.6.8970383. [DOI] [PubMed] [Google Scholar]
- 25.Di Giuda D, Galli J, Calcagni ML, et al. Rhinoscintigraphy: a simple radioisotope technique to study the mucociliary system. Clin Nucl Med. 2000;25:127–130. doi: 10.1097/00003072-200002000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Lale AM, Mason JD, Jones NS. Mucociliary transport and its assessment: a review. Clin Otolaryngol Allied Sci. 1998;23(5):388–396. doi: 10.1046/j.1365-2273.1998.00173.x. [DOI] [PubMed] [Google Scholar]
- 27.Homer JJ, Dowley AC, Condon L, El-Jassar P, Sood S. The effect of hypertonicity on nasal mucociliary clearance. Clin Otolaryngol Allied Sci. 2000;25(6):558–560. doi: 10.1046/j.1365-2273.2000.00420.x. [DOI] [PubMed] [Google Scholar]
- 28.Passali D, Ciampoli MB. Normal values of mucociliary transport time in young subjects. Int J Pediatr Otorhinolaryngol. 1985;9:151–156. doi: 10.1016/s0165-5876(85)80015-x. [DOI] [PubMed] [Google Scholar]
- 29.Habesoglu M, Demir K, Yumusakhuylu AC, Yilmaz AS, Oysu C. Does passive smoking have an effect on nasal mucociliary clearance. Otolaryngol Head Neck Surg. 2012;147(1):152–156. doi: 10.1177/0194599812439004. [DOI] [PubMed] [Google Scholar]
- 30.Cazzolla AP, Campisi G, Lacaita GM, et al. Changes in pharyngeal aerobic microflora in oral breathers after palatal rapid expansion. BMC Oral Health. 2006;6:2. doi: 10.1186/1472-6831-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]