Abstract
Objective:
To assess the impact of malocclusion on the quality of life.
Materials and Methods:
This cross-sectional study involved 150 subjects attending the Primary Care Unit with no history of orthodontic treatment. The Dental Aesthetic Index (DAI) with 10 occlusal characteristics were measured on study models. Oral health-related quality of life (OHRQoL) was assessed with the Malaysian version of the Oral Health Impact Profile questionnaire (OHIP-14). The Spearman rank-order correlation coefficient was used to evaluate the relationship between the malocclusion and quality of life.
Results:
Significantly weak correlations (r = .176) were found between the DAI and the OHRQoL. Females and the younger age group (12–19 years) tended to score higher on the OHIP-14 than their counterparts. For males, domain 3 (psychological discomfort; r = .462), domain 4 (physical disability; r = .312), domain 7 (handicap; r = .309), and overall score (r = .289) were weak correlates but significant to the DAI compared with females. The older age group showed a significant weak correlation in domain 3 (psychological discomfort; r = .268) and domain 7 (handicap; r = .238), whereas the younger age group showed no correlation with any domain.
Conclusions:
The DAI score does not predict the effect of malocclusion on the OHRQoL.
Keywords: Dental Aesthetic Index, Orthodontic treatment need, Quality of life
INTRODUCTION
There are many objective indexes to measure oral health. These indexes can determine how much a person’s oral health deviates from the ideal or normal condition; therefore, appropriate treatment can be provided. In malocclusion, physical deviation from the ideal occlusion, there is a high degree of subjectivity with a variety of perceptions of orthodontic treatment need among the population.1
The Index of Orthodontic Treatment Need (IOTN) is becoming the most commonly used index in orthodontic practice. Meanwhile, the Dental Aesthetic Index (DAI)—an alternative form of index—combines the clinical and aesthetic aspects of occlusion that indirectly assess the relative social acceptability of dental appearance.2 The DAI has been proven to be reliable, simple, valid, and user-friendly.3,4 Furthermore, it can be used and adapted globally and cross-culturally without any modification.5–7 Unlike the IOTN, the DAI eliminates the need of a separate instrument to assess the aesthetic component.
Silvola et al.8 discussed the impact of oral health on a person’s well-being from the functional, social, and psychological aspects. Although the DAI indicates the relative social acceptability and functionality of dental appearance,2 ideally the patient’s own psychosocial view should be included.9,10 The patient’s psychosocial view would allow each treatment plan to be tailored for the individual patient, maximizing the treatment benefit. Each patient’s self-awareness of his or her occlusion may be inconsistent with its severity.9,11 Some patients with severe malocclusion are indifferent to their condition, while others are very concerned with only minor irregularities.9 This is how the use of an occlusal index alone might be a problem: when a patient without a psychosocial need for treatment is deemed to be in need of treatment.
As orthodontists have become more aware of patients’ quality of life in oral health, more oral health-related quality of life (OHRQoL) questionnaires have been developed over the past two decades to assess patients’ perspectives and needs toward their malocclusion.12 One of the emerging tools is the Malaysian cross-cultural adaptation, the Oral Health Impact Profile (OHIP-14),13 which has been verified to be valid and reliable, and it has been used in a national survey.14,15 The introduction of the OHIP-14 highlights the importance of not only improving the malocclusion, but also the patient’s psychosocial well-being. A generic questionnaire has the benefit of capturing unforeseen effects that might go unnoticed by a specific instrument.16
The DAI is an appraisal made by the dentist, while the OHRQoL is an evaluation by the patients themselves. Therefore, it is important to assess whether any correlation exists between these two instruments. Many studies have been done to assess the correlation of malocclusion with the OHRQoL.12 However, there is still ambiguity in their relationship. Nevertheless, a systematic review conducted by Zhijian et al.17 covering publications from 1960 to 2007 found only 23 articles that met the inclusion criteria. The authors concluded that there is a moderate association between malocclusion and the QoL.
In the face of this inconsistency, the purpose of this study was to investigate the relationship between the DAI and the ORHQoL and to assess the impact of malocclusion on the OHRQoL in the adolescent and adult population.
MATERIALS AND METHODS
This study was undertaken after obtaining a detailed protocol and ethical approval from the Research Ethics Committee of Universiti Kebangsaan Malaysia (UKM 1.25.11/244/2).
Sample size calculation was performed using the Raosoft online sample-size calculator (Raosoft Inc, Seattle, Wash). With a margin of error of 5% and a confidence level of 95%, the target sample size was determined to be 150 (including 10% dropout). A systematic convenience sampling was done.
A total of 159 subjects from the Primary Care Clinic of UKM were invited to participate in this study. Consent was obtained from each subject after we explained the nature and purpose of the study. For subjects under 18, consent was obtained from their guardians. The inclusion criteria were (1) age between 12 to 35 years, (2) all teeth present excluding 3rd molars, (3) no history of orthodontic treatment, (4) no history of untreated dental caries, (5) no history of poor periodontal health or previous extraction, (6) no chronic medical conditions or craniofacial anomalies, and (7) Malay literate. A simple clinical examination was performed by A.A., followed by impressions of the maxillary and mandibular arches, which were taken with fast-setting alginate and conducted under strict infection control procedures. The impressions were sent directly to the laboratory and study models were prepared.
Subjects were then given a self-administrated questionnaire to gather sociodemographic and OHRQoL information. The short version of the OHIP-14 was used to reduce time and burden on the patients, as long questionnaires could lead to inaccurate results.18 OHIP-14 focuses on the impact of OHRQoL via seven conceptual domains (two items per domain). A 5-point Likert scale was used to rate the frequency of occurrence of a particular problem captured by the domain. The responses range from “always” to “never” (1 to 5) with an additional X-“I don’t know.” The two methods of scoring were (1) Additive (ADD) scores, ranging from 0 to 56, were calculated by adding up the response codes for each item, and (2) domain scores were calculated by averaging the score for each domain. High scores indicated poor OHRQoL. The kappa value in rerating the questionnaire by 15 (10%) of the subjects was determined to be 0.86 at an interval of 2 weeks during their reappointment schedule for the dental treatment. This showed good intraexaminer reliability.
The DAI score was obtained using the standard DAI regression equation index according to WHO guidelines.19 DAI consists of 10 occlusal characteristics related to dentofacial anomalies according to the three components of the dentition: spacing, crowding and occlusion. In order to obtain accuracy with the use of the DAI index, the examiner underwent a training and calibration exercise, measuring the parameters for the DAI components directly from the study model with a digital caliper. Triplicate measurements were made and the mean was obtained. After a patient’s total score had been calculated, it was graded on a scale of the most and least socially acceptable dental appearance that would place it in the treatment-mandatory category (Table 1). Intraclass correlation showed good intraexaminer reliability (.82). Nine broken study models were eliminated, leaving only 150 to be included in the analysis.
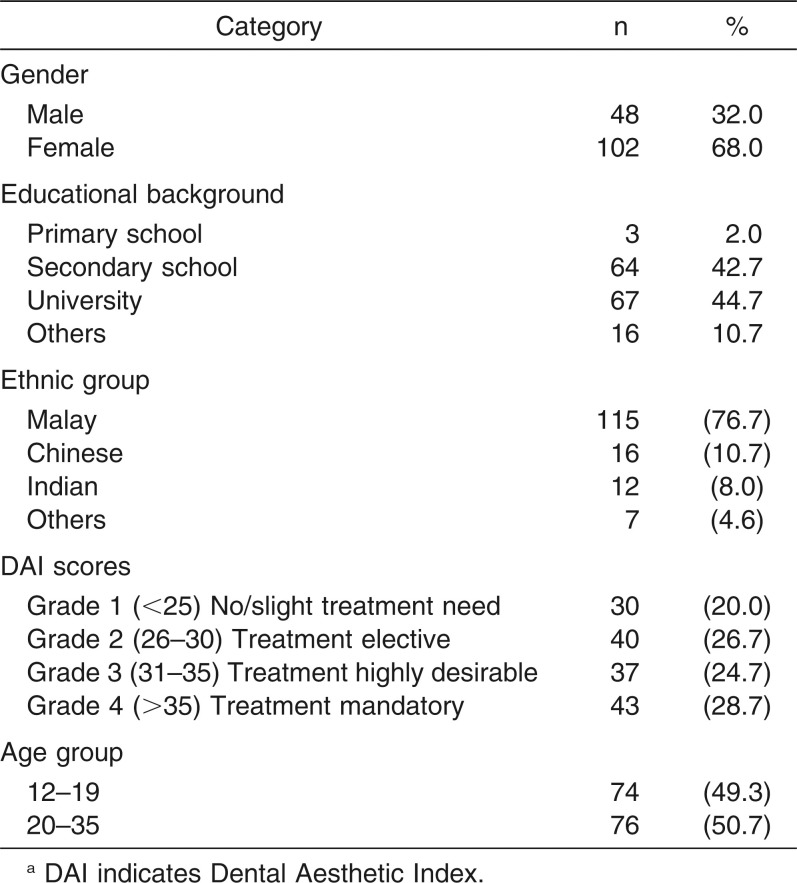
Table 1.
Distribution of Sociodemographic Characteristics, DAI,a and OHIP-14 Scores
The data and relationship between the DAI and OHRQoL were analyzed using the Statistical Package for Social Science software for Windows version 22.0 (SPSS Inc, Chicago, Ill).
RESULTS
A total of 159 subjects among the adolescent and adults participated in the study. However, nine records were excluded from analysis due to the broken study models. As shown in Table 1, of the 150 subjects, approximately two-thirds were female (102; 68%). Most of the subjects had at least university-level education (67; 44.7%), and 64 (42.7%) were educated only to the secondary level (132; 40.8%).
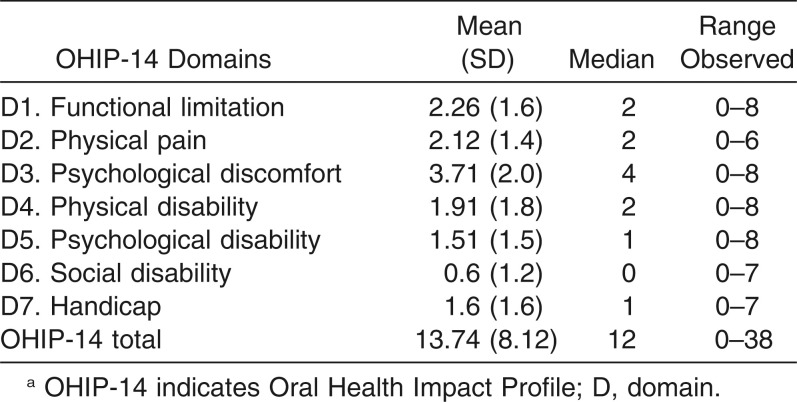
Table 2 depicts the mean, standard deviation, median, and range observed in OHIP-14 for each domain in all 150 subjects. The overall mean score (± SD) for OHIP-14 was 13.74 ± 8.12. Domain 3 (psychological discomfort) had the highest impact, with a mean score of 3.71 ± 2.0. The domain with the least impact was domain 6 (social disability), with a mean score of 0.6 ± 1.2. Females scored higher means in four out of seven domains (domain 4, psychological discomfort; domain 4, physical disability; domain 5, psychological disability; domain 6, social disability; domain 7, handicap) along with the total score. Generally, the younger age group (12–19 years) scored higher means than did the older age group (20–35) in five out of seven (domain 3, psychological discomfort; domain 4, physical disability; domain 5, psychological disability; domain 6, social disability; domain 7 handicap) as well as the total score.
Table 2.
Mean, Standard Deviation (SD), Median, and Range Observed in OHIP-14a
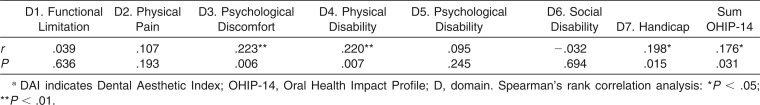
Table 3 shows the Spearman rank-order correlation coefficients between the DAI and OHIP-14 scores, which showed significant but almost no correlation (r = .176) between the two instruments at all grades of the DAI summative score. Domain 3 (r = .223; P < .01) and domain 4 (r = .220; P < .01) had the strongest correlation. Domain 7 (r = .198; P < .05) was observed to have a significant but weaker correlation.
Table 3.
Spearman Correlation Between DAI and OHIP-14a
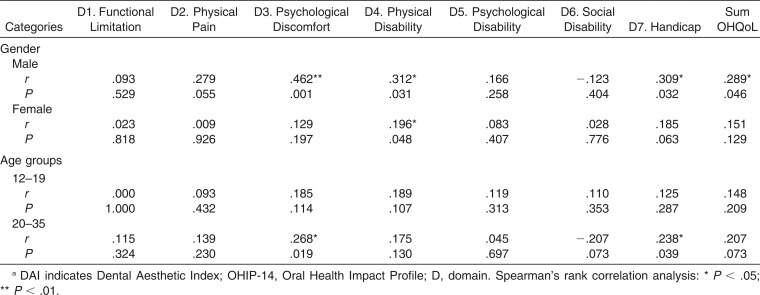
Table 4 displays the Spearman rank-order correlation coefficients between the DAI score and the OHIP-14 score for gender and age categories. Although females on average had a slightly higher impact scores than males, none of the correlations between the DAI and OHIP-14 was significant except for domain 4 (r = .196). However, for males there were significant correlations in domains 3 (r = .462), 4 (r = .312), and 7 (r = .309), and total score (r = .289). Between the age groups, no significant correlation was observed in the 12–19 age groups, whereas the older age groups showed significant but weak correlations in domain 3 (r = .268) and domain 7 (r = .248). There was no correlation in the total score for either age group.
Table 4.
Spearman Correlation Between DAI and OHIP-14 According to Gender and Age Groupsa
DISCUSSION
Many studies have assessed the influence of malocclusion on the quality of life.9,12,16,17,20–24 A study in Malaysia utilized IOTN as the instrument.20 Most of these studies have focused on a specific group such as children, orthodontic patients, or patients seeking orthodontic care.9,12,16,17,20–24 The current study used DAI as the instrument and covered a wider age range of population that comes for primary dental care, not specifically seeking orthodontic treatment.
Studies on orthodontic patients have focused on physical pain, psychological discomfort, and disability.12,20,25 In this study, the patients in primary care also indicated that psychological discomfort (domain 3) had the highest oral impact among the seven domains (Table 2). Feu et al.9 reported that psychological discomfort was the secondmost negatively impacting domain. One study has shown that aesthetic improvement in malocclusion provides improvement in oral health–related quality of life, particularly in psychological discomfort and psychological disability.8 It is reasonable to assume that aspects of physical appearance play an important role in malocclusion, since it is more of an aesthetic deviation from the ideal of normal occlusion.26 The DAI was designed to assess relative social acceptability of dental appearance, and this was reflected in the results of this study, in which the DAI scores were significantly correlated with the three domains that include physical appearance. Four domains (3, 4, 6, and 7) of OHIP-14 cover aspects of facial appearance. However, only three domains (3, 4, and 7) were most affected. Domain 3 (psychological discomfort), which was found to be related to aesthetic impairment,27 was observed to have the highest impact in the study. Liu et al.12 reported correlations of malocclusion with the OHIP-14, namely, that domains 3, 5, 6, and 7 were significantly affected. In another study, discomfort in eating (an aspect of physical discomfort) was also significantly correlated with malocclusion.22
In the gender category, females generally scored higher on their OHIP-14 than did males. This trend was also reflected in other studies.9,20,21,25 Females are thought to be more self-conscious, and they tend to report a higher oral impact than do males.25 This higher score may be due the larger number of females (twice as many) compared with the males (Table 1). However, males also tend to score lower than females in three domains (psychological discomfort, physical disability, and handicap) and in total OHIP-14 scores wherein significant correlations existed (Table 4). This indicates that although males tend to be less conscious of their appearance,28 they probably are more aware of their malocclusion.
For the age category, the younger group scored higher in OHIP-14 but there was no correlation with the DAI. The older group scored lower but had significant (P < .05) correlations in two domains (psychological discomfort and handicap; Table 4). The tendency for the younger group to overrate their problems is probably due to the fact that this age group represents a period of intense social and affective relationships, in which dental aesthetics and smile have a strong potential to influence the individuals’ physical attractiveness.26 Older groups tended to be more correlated with their malocclusion, even though they scored lower. This is in agreement with Abu Alhaija et al.,29 wherein the correlation between malocclusion and OHRQoL was higher in the older groups.
In this study, OHIP-14 exhibited a few domains (mainly 3, 4, and 7) that have significant but weak correlations with patients’ malocclusion, which suggests that the higher the grade of malocclusion, the more likely are these domains affected. This was also observed in another study, wherein quality of life was related to emotional rather than functional or social well-being.23
The generic questionnaire does not directly assess malocclusion,12 which is an asymptomatic deviation from the aesthetic norm rather than an acute disease.12,30 Therefore, the sensitivity of OHIP-14 to changes in malocclusion is lower compared with other oral conditions. Currently, no validated QoL instrument can be specifically applied to malocclusion. Further research is required to integrate a condition-specific questionnaire for malocclusion, which should have a higher sensitivity to assess the impact of malocclusion on the ORQoL. We also noted that this weak correlation is a universal finding in other studies as well. It may suggest that the correlation values of .20 to .30 are the strongest correlation values between the DAI and OHRQoL.
The limitations of this study must be taken into consideration. The subjects in this study were selected by convenience sampling: patients who sought treatment at the primary dental clinic. Block sampling was not administered, hence the large numbers of females. In addition, those who do not seek dental treatment might have different priorities and different perspectives in their OHRQoL. A larger sample size would increase the sensitivity of the impact of malocclusion on the OHRQoL, which could be explored more fully among various age groups.
CONCLUSIONS
The findings of significant weak correlations between the DAI and the OHRQoL suggest that the DAI grade cannot strongly predict the OHQoL of the patients. The females and the younger age group (12–19 years) tended to score higher on the OHIP-14 score compared with their counterparts.
More domains with weak correlations were found in the males and older age group than in the females and younger age group, respectively.
REFERENCES
- 1.Borzabadi-Farahani A. Principles in Contemporary Orthodontics. Los Angeles: InTech; 2011. An overview of selected orthodontic treatment needs indices; pp. 216–232. In:Naretto S, ed. [Google Scholar]
- 2.Cons NC, Jenny J, Kohout K. DAI The Dental Aesthetic Index. Iowa City: University of Iowa College of Dentistry; 1986. pp. 1–20. [Google Scholar]
- 3.Jenny J, Cons NC. Comparing and contrasting two orthodontic indices, the Index of Orthodontic Treatment Need and the Dental Aesthetic Index. Am J Orthod Dentofacial Orthop. 1996;110:410–416. doi: 10.1016/s0889-5406(96)70044-6. [DOI] [PubMed] [Google Scholar]
- 4.Beglin FM, Firestone AR, Vig KW, Beck FM, Kuthy RA, Wade D. A comparison of the reliability and validity of 3 occlusal indexes of orthodontic treatment need. Am J Orthod Dentofacial Orthop. 2001;120:240–246. doi: 10.1067/mod.2001.116401. [DOI] [PubMed] [Google Scholar]
- 5.Tessarollo FR, Feldens CA, Closs LQ. The impact of malocclusion on adolescents’ dissatisfaction with dental appearance and oral functions. Angle Orthod. 2012;82:403–409. doi: 10.2319/031911-195.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peterson P, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of diseases and risks to oral health. Bull World Health Org. 2005;83:661–669. [PMC free article] [PubMed] [Google Scholar]
- 7.Peres SH, Goya S, Cortellazzi KL, Ambrosano GM, Meneghim Mde C, Pereira AC. Self-perception and malocclusion and their relation to oral appearance and function. Cien Saude Colet. 2011;16:4059–4066. doi: 10.1590/s1413-81232011001100011. [DOI] [PubMed] [Google Scholar]
- 8.Silvola AS, Varimo M, Tolvanen M, Rusanen J, Lahti S, Pirttiniemi P. Dental aesthetics and quality of life in adults with severe malocclusion before and after treatment. Angle Orthod. 2014;84:594–599. doi: 10.2319/060213-417.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feu D, de Oliveira BH, de Oliveira Almeida MA, Kiyak HA, Miguel JA. Oral health related quality of life and orthodontic treatment seeking. Am J Orthod Dentofacial Orthop 2010. 138:152–159. doi: 10.1016/j.ajodo.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 10.Kok YV, Mageson P, Harradine NW, Sprod AJ. Comparing a quality of life measure and the Aesthetic Component of the Index of Orthodontic Treatment Need (IOTN) in assessing orthodontic treatment need and concern. J Orthod. 2004;31:312–318. doi: 10.1179/146531204225020625. [DOI] [PubMed] [Google Scholar]
- 11.Albino JEN, Laurence SD, Tedesco LA. Psychological and social effects of treatment. J Behav Med. 1994;17:81–98. doi: 10.1007/BF01856884. [DOI] [PubMed] [Google Scholar]
- 12.Liu Z, McGrath C, Hägg U. Associations between orthodontic treatment need and oral health-related quality of life among young adults: does it depend on how you assess them. Community Dent Oral Epidemiol. 2011;39:137–144. doi: 10.1111/j.1600-0528.2010.00573.x. [DOI] [PubMed] [Google Scholar]
- 13.Fernandes MJ, Ruta DA, Ogden GR, Pitts NB, Ogston SA. Assessing oral health-related quality of life in general dental practice in Scotland: validation of the OHIP-14. Community Dent Oral Epidemiol. 2006;34:53–62. doi: 10.1111/j.1600-0528.2006.00254.x. [DOI] [PubMed] [Google Scholar]
- 14.Saub R, Locker D, Allison P, Dsiman, M Cross-cultural adaptation of the Oral Health Impact Profile (OHIP) for the Malaysian adult population. Community Dent Health. 2007;24:166–175. [PubMed] [Google Scholar]
- 15.Saub R, Locker D, Allison P. Comparison of two methods in deriving a short version of oral health-related quality of life measure. Community Dent Health. 2008;25:132–136. [PubMed] [Google Scholar]
- 16.O’Brien C, Benson PE, Marshman Z. Evaluation of a quality of life measure for children with malocclusion. J Orthod. 2007;34:185–193. doi: 10.1179/146531207225022185. [DOI] [PubMed] [Google Scholar]
- 17.Zhijian L, Colman M, Urban H. The impact of malocclusion/orthodontic treatment need on the quality of life: a systematic review. Angle Orthod. 2009;79:585–591. doi: 10.2319/042108-224.1. [DOI] [PubMed] [Google Scholar]
- 18.Saub R, Locker D, Allison P. Derivation and validation of the short version of the Malaysian Oral Health Impact Profile. Community Dent Oral Epidemiol. 2005;33:378–383. doi: 10.1111/j.1600-0528.2005.00242.x. [DOI] [PubMed] [Google Scholar]
- 19.WHO . Oral Health Surveys Basic Methods. Geneva: World Health Organization; 1997. 4th ed. [Google Scholar]
- 20.Masood Y, Masood M, Zainul NNB, Araby NBAA, Hussain SF, Newton T. Impact of malocclusion on oral health related quality of life in young people. Health Qual Life Outcomes. 2013;26:11–25. doi: 10.1186/1477-7525-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Oliveira CM, Sheiham A. The relationship between normative orthodontic treatment need and oral health-related quality of life. Community Dent Oral Epidemiol. 2003;31:426–436. doi: 10.1046/j.1600-0528.2003.00002.x. [DOI] [PubMed] [Google Scholar]
- 22.Manjith CM, Karnam SK, Manglam S, Praveen MN, Mathur A. Oral Health-Related Quality of Life (OHQoL) among adolescents seeking orthodontic treatment. J Contemp Dent Pract. 2012;13:294–298. doi: 10.5005/jp-journals-10024-1140. [DOI] [PubMed] [Google Scholar]
- 23.Onyeaso CO, Aderinokun GA. The relationship between dental aesthetic index (DAI) and perceptions of aesthetics, function and speech amongst secondary school children in Ibadan, Nigeria. Int J Ped Dent. 2003;13:336–341. doi: 10.1046/j.1365-263x.2003.00478.x. [DOI] [PubMed] [Google Scholar]
- 24.Johal A, Cheung MY, Marcene W. The impact of two different malocclusion traits on the quality of life. Br Dent J. 2007;202:1–4. doi: 10.1038/bdj.2007.33. [DOI] [PubMed] [Google Scholar]
- 25.Rusanen J, Lahti S, Tolvanen M, Pirttiniemi P. Quality of life in patients with severe malocclusion before treatment. Eur J Orthod. 2010;32:43–48. doi: 10.1093/ejo/cjp065. [DOI] [PubMed] [Google Scholar]
- 26.Traebert ESA, Peres MA. Do malocclusions affect the individual’s oral health quality of life. Oral Health Prev Dent. 2006;5:3–11. [PubMed] [Google Scholar]
- 27.Wong AHH, Cheung CS, McGrath C. Developing a short form of oral health impact profile (OHIP) for dental aesthetics: OHIP-aesthetic. Community Dent Health. 2007;35:64–72. doi: 10.1111/j.1600-0528.2007.00330.x. [DOI] [PubMed] [Google Scholar]
- 28.Heravi F, Farzanegan F, Tabatabaee M, Sadeghi M. Do malocclusions affect the oral health-related quality of life. Oral Health Prev Dent. 2011;9:229–233. [PubMed] [Google Scholar]
- 29.Abu Alhaija ESJ, Al–Nimri KS, Al–Khateeb SN. Self perception of malocclusion among north Jordanian school children. Eur J Orthod. 2005;27:292–295. doi: 10.1093/ejo/cjh094. [DOI] [PubMed] [Google Scholar]
- 30.Klages U, Claus N, Wehrbein H, Zentner A. Development of a questionnaire for assessment of the psychosocial impact of dental aesthetics in young adults. Eur J Orthod. 2006;28:103–111. doi: 10.1093/ejo/cji083. [DOI] [PubMed] [Google Scholar]