Abstract
Objective:
To evaluate the reliability of digital orthodontic setup technology by comparing it with manual setups and models cast at the end of orthodontic treatment.
Materials and Methods:
Initial models, manual setups, and final models of 20 patients were used. The initial and final models, as well as the manual setups, were scanned using a 3Shape R-700 scanner, while the digital setups were fabricated based on the initial models using 3Shape OrthoAnalyzer software. Evaluation of the models based on the manual setup, digital setup, and final models of each patient was performed using the following linear measurements: intercanine widths, intermolar widths, and length of the upper and lower dental arches.
Results:
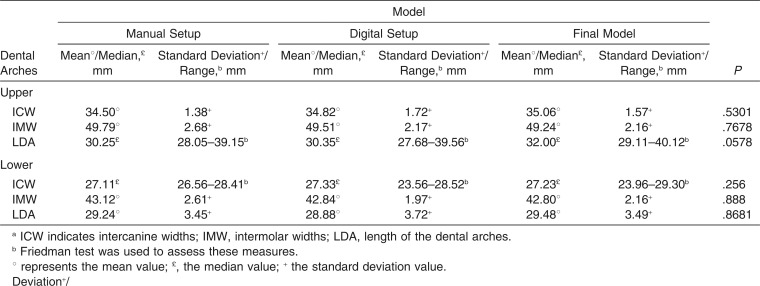
The results disclosed that none of the measures assessed through the manual setup, digital setup, and final models showed statistically significant differences (P > .05).
Conclusions:
Based on these findings, it can be inferred that digital setups are as effective and accurate as manual setups and constitute a tool for diagnosing and treatment planning that can be reliably reproduced in orthodontic treatments.
Keywords: Computer-assisted diagnosis, Dental models, Three-dimensional imaging
INTRODUCTION
Setup is a technique whereby teeth are reassembled in plaster models to depict the patient’s malocclusion.1–6 In carrying out this diagnosis, the teeth are separated from each other and from the bases of upper and lower casts, allowing them to be repositioned within the framework of orthodontic treatment planning.1–4 Setup’s key advantage lies in allowing professionals to ascertain that treatment planning is indeed viable in each case.1,3,5,6 It answers questions such as the following: Are extractions necessary or will the mere stripping of interproximal prove sufficient to align the teeth? How much interproximal stripping should be performed and on which teeth? What precautions would be necessary to ensure proper anchorage?
Fabrication of a manual setup involves a laborious technique. However, when properly performed and analyzed, it provides data that can facilitate treatment and reduce biological damage to the patient.4 Therapy should be initiated only after making sure that planning is suitable for correcting a given malocclusion.4,6
With the increasing use of digital dental models, it is now possible to build digital orthodontic setups. These allow one to review different orthodontic treatment options that can be shared with other orthodontists and health-related professionals to exchange information about the treatment. Furthermore, digital setups also make it easier to present the therapeutic alternatives to patients and/or their legal guardians, allowing them to understand the best treatment option.6–8
Given the emergence of new software, this study aimed to evaluate the reliability of digital orthodontic setup technology by comparing it with manual setups and with the final treatment models. For this purpose, OrthoAnalyzer (3Shape, Copenhagen, Denmark) computer software was employed.
MATERIALS AND METHODS
The sample size (n) consisted of 20 patients. Calculation was performed using an expected difference of 1 mm, with 80% power and an 5% alpha level. Sample size calculation was performed using BioEstat software (version 5.0, Mamirauá Institute, Belém, Pará State, Brazil). Ethical approval for this study was obtained from the Ethical Committee of the Federal University of Bahia, Faculty of Dentistry.
To be selected, patients had to meet the following criteria: orthodontic treatment must have been completed, presence of permanent teeth as far as the second molars, treatment must not involve prosthetic rehabilitation, facial growth must have been completed before the start of treatment, no involvement of orthognathic surgery, dental casts properly fabricated2 and in perfect condition, and manual setups based on the proposed treatment plan.
Manual setups, digital setups, and final models of the patients were used in the study. To fabricate the setups, the authors endeavored to comply with the key principles of a normal occlusion by preserving the original intermolar and intercanine widths, maintaining the arch form, attaining correct contact points, normal overbite and overjet, coincident and correct midlines, correct axial inclinations and angulations (tip), no rotations, normal relationship between occlusal inclined planes, and appropriate curve of Spee and curve of Wilson.
To produce the digital models, an R-700 scanner (3Shape) was used, which features a laser beam and two digital cameras capable of capturing high-resolution images. The same specialist in orthodontics scanned the models according to the specifications provided by the equipment manufacturer. The initial models, final models, and manual setups were scanned.
The manual setups had been previously fabricated by graduate students from the Specialization Program in Orthodontics, Federal University of Bahia, according to the treatment plan proposed under the supervision of an orthodontics instructor following the method described by Araújo et al.2 The manual setups were made and used for diagnosis and planning prior to the orthodontic treatment.
In scanning the manual setups, the same technique was used for initial models. However, given that wax—where the teeth are mounted—is not scanned by the laser, Spotcheck SKD-S2 (Magnaflux, Glenview, Ill) solvent developer had to be used on the wax area. The final models were scanned without the use of a developer.
The digital setups were constructed based on the initial models scanned using the OrthoAnalyzer (3Shape) software. The researcher who built the digital setup had access to the treatment plan, examinations, and initial models. However, he was blinded to the manual setup and final model. The setup was based on the anchorage requirements, the final desired position for the whole maxilla and mandible according to the treatment plan, the expected torque loss related to wire play and other factors, the amount of overcorrection for rotation control, and the arch forms.
Initially, the upper and lower arch forms were obtained and the crown axis determined. The teeth were sectioned one by one, preserving the anatomy of the tooth crown in the mesiodistal and buccolingual directions (Figure 1A), while ensuring that each section extended right through the contact point. After this stage, manual adjustment of individual teeth to their ideal positions was performed according to the treatment plan. The mounting was initiated by repositioning the lower incisors. One side was mounted at a time, and the arch form was maintained. Finally, the models in occlusion were evaluated for potential collisions between the teeth, and when necessary, corrections were made (Figure 1B).
Figure 1.
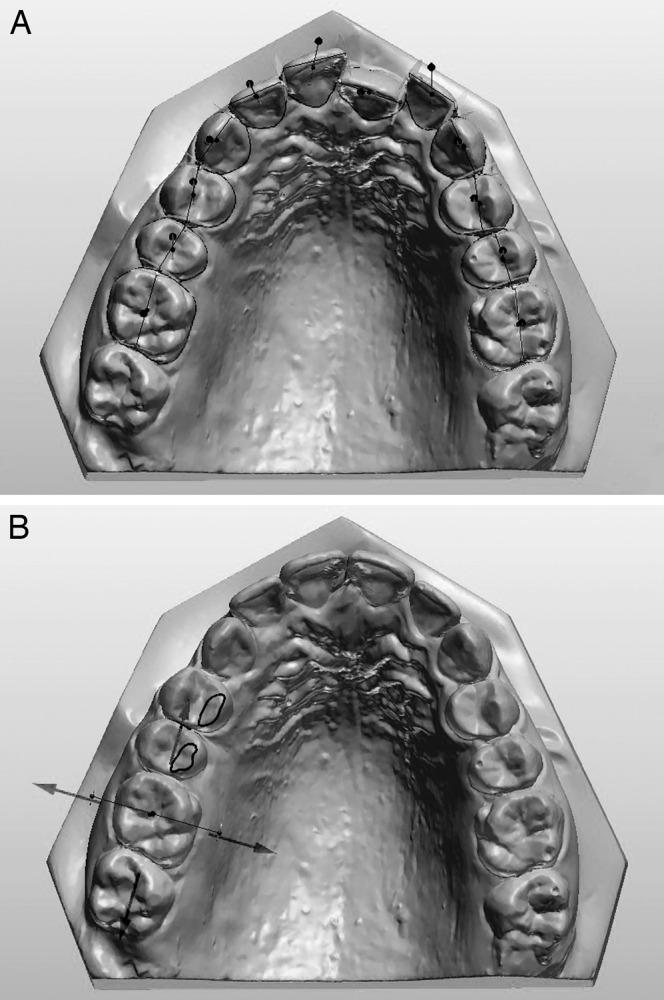
(A) Maxillary model preparation process. (B) Image depicting teeth manipulation.
When ready, the digital setups were saved as digital models, and no further changes were allowed to be made in tooth positions to ensure reliable measurements.
Comparisons between digital models in terms of manual setup, digital setup, and final model were carried out by means of linear measurements: intercanine and intermolar widths and length of the upper and lower dental arch (Figure 2). The measurements were performed by a properly calibrated examiner with the aid of OrthoAnalyzer software (3Shape).
Figure 2.
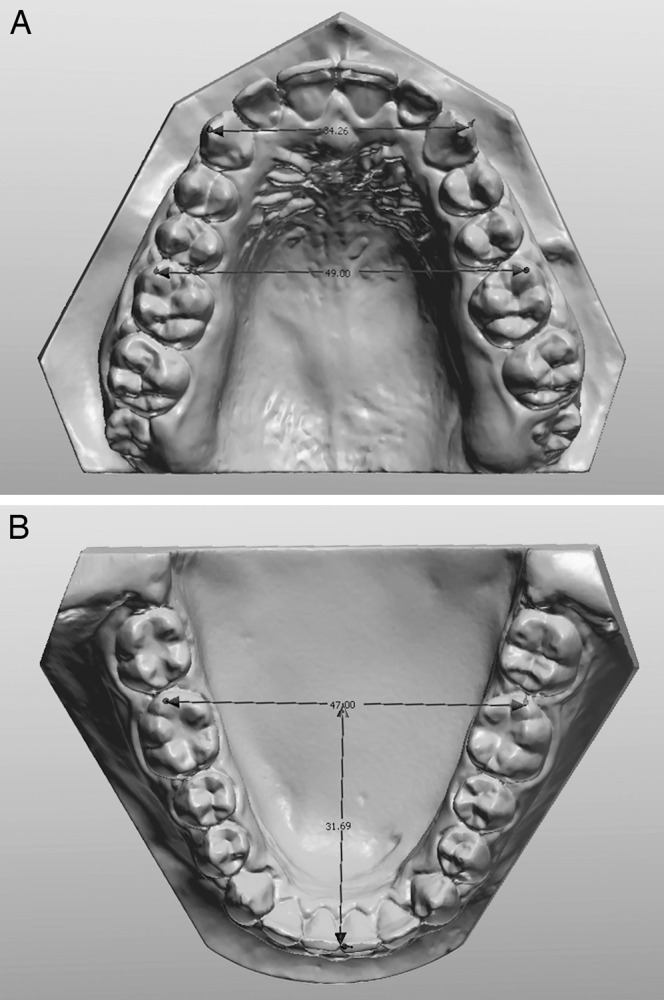
(A) Intercanine and intermolar widths of the maxillary arch. (B) Length of the mandibular arch.
Prior to measuring, five patients were randomly selected. The digital measurements were performed at two different points in time with 2-week intervals between them, under the same conditions, by a single duly trained operator. The measured values were subjected to a statistical test to determine random error. For all variables, random error was calculated according to Dahlberg’s formula (S2 = Σd2/2n) to verify intraexaminer agreement.
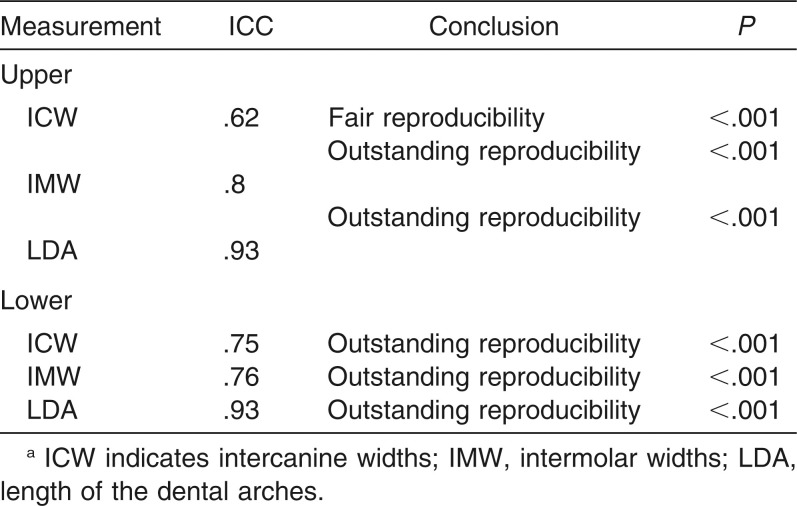
Analysis of the reproducibility of measurements was performed by testing intraclass correlation, with a confidence level of 95%.
Statistical Analysis
Statistical analysis was performed with BioEstat software (version 5.0, Mamirauá Institute, Belém, Pará State, Brazil).
D'Agostino-Pearson test was employed to observe normal data distribution. Moreover, repeated-measures analysis of variance (ANOVA) and Friedman test were used to test the null hypothesis of no difference between the measurements of the setup methods and final models of the patients. The significance level was set at 5%.
RESULTS
Method error calculation took into account reliable measurements given their remarkable reproducibility potential. Correlations for most measurements were rated as outstanding (r = .75 to .93), whereas in evaluating the intercanine width in the upper arch, there was a statistically significant correlation (P < .001), which was given a positive rating (r = .62; Table 1).
Table 1.
Results of Intraclass Correlation (ICC) Between Measurementsa
In analyzing the data, the Friedman test was used to assess the length of the upper arch in the manual setup, digital setup, and final model. Likewise, the same test was applied to evaluate the intercanine width in the lower arch of the manual setup. An ANOVA was used to assess the remaining measures. Descriptive statistics and results are shown in Table 2.
Table 2.
Descriptive Statistics and Results of Friedman and Analysis of Variance Tests for Manual Setups, Digital Setups, and Final Modelsa
None of the measures assessed with the aid of the manual setup, digital setup, and final models showed any statistically significant differences (P > .05).
DISCUSSION
Studies on virtual setup reliability are still scant in the literature, and this contrasts with the increasing sophistication and investment in the development of these tools. In using the setup, the main goal is to provide the orthodontist with a realistic view of how a case that is being planned will likely end, no matter if the setup is physical or digital. Thus, the setup should not be constructed artistically to help persuade the patient to accept treatment but very carefully, in line with the treatment goals and limitations of orthodontic mechanics.2
In the study, the digital models were also analyzed by converting the manual setup and final model into digital models. According to Sousa et al.,4 the digital models proved as reliable as plaster models (casts) in obtaining the measures commonly used for diagnosis. Fleming et al.5 reported that digital models offer a high degree of validity when compared with the direct measurement of plaster models, and the differences between these approaches are likely to be within clinically acceptable limits. However, there may be small differences between measurements made on plaster models vs digital models. Therefore, to obtain more accurate results and to avoid confusion caused by model analysis methods, models were analyzed by converting manual setups into digital models.
The results indicated that manual setups are reliable tools for planning treatment. This is because there are no differences in the measurements performed in the final models vs the manual setups, thus confirming the results found by Im et al.9 As a result, this lack of differences between the manual and digital setups suggests that the digital setups allow one to envision the treatment goals in a manner similar to manual setups.
Digital setups seem to offer advantages over manual setups. Initially, the program is easy to learn and manipulate. In addition, image setups are easy to store as they do not require large physical spaces, as is the case with plaster models, whose storage costs are extremely costly in many cities around the world. Finally, communication between professionals and the patient is facilitated, since setups can be sent over the Internet, avoiding potential breakage during shipping and handling. This advantage is also mentioned by some authors regarding digital models.10–17 In recent years, replacing conventional diagnostic methods with other more technologically advanced methods has become common in the medical and dental areas.18,19 The use of digital setups seems to have the potential to reinforce this trend, which could mean further development in the process of storing information required for orthodontic diagnosis. In this study, the program used to perform the digital setup provided poor visualization of the gum line. The gum does not follow extensive tooth movements, which hinders gum line analysis.
Araújo et al.2 emphasized the various disadvantages of manual setups, including a lengthy fabrication time given that professionals spend a few hours doing laboratory work, although this factor does not preclude its use. This assertion proves even more flexible when the digital setup is used as an aid in orthodontic diagnosis. Although this investigation did not evaluate the time it takes to construct a model, it was found that the time taken to construct a digital setup from scanning of the initial model to completion was 2 hours. On the other hand, preparing the manual setup directly on the plaster models involves cutting, preparing the teeth and model bases, and mounting the planned occlusion, and it takes much longer.
The results of this study demonstrate that the use of digital orthodontic setups is reliable and an excellent method of orthodontic treatment, as it allows a three-dimensional view of the patient’s occlusion at the end of treatment. This enables greater confidence in the application of any orthodontic therapy. A comparison between the setups and the final model in this study reassures orthodontists with respect to the use of setups, both manual and digital, as a tool to determine the orthodontic therapy of choice.
Nevertheless, further studies are warranted to assess the reliability of virtual setups and to develop algorithms to predict gingival response to tooth movement, which would allow further refinement of orthodontic planning.
CONCLUSION
Based on these findings, it can be inferred that digital setups are as effective and accurate as manual setups and consist of a tool for diagnosis and treatment planning that can be reliably reproduced in orthodontic treatments.
ACKNOWLEDGMENT
We thank Dr David Normando for assistance with the statistical analysis.
REFERENCES
- 1.Kim SH, Park YG. Easy wax setup technique for orthodontic diagnosis. J Clin Orthod. 2000;34:140–144. [Google Scholar]
- 2.Araújo TM, Fonseca LM, Caldas LD, Costa-Pinto RA. Preparation and evaluation of orthodontic setup. Dental Press J Orthod. 2012;17:146–165. [Google Scholar]
- 3.Mattos CT, Gomes AC, Ribeiro AA, Nojima LI, Nojima M da C. The importance of the diagnostic setup in the orthodontic treatment plan. Int J Orthod. 2012;23:35–39. [PubMed] [Google Scholar]
- 4.Sousa MV, Vasconcelos EC, Janson G, Garib D, Pinzan A. Accuracy and reproducibility of 3-dimensional digital model measurements. Am J Orthod Dentofacial Orthop. 2012;142:269–273. doi: 10.1016/j.ajodo.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 5.Fleming PS, Marinho V, Johal A. Orthodontic measurements on digital study models compared with plaster models: a systematic review. Orthod Craniofac Res. 2011;14:1–16. doi: 10.1111/j.1601-6343.2010.01503.x. [DOI] [PubMed] [Google Scholar]
- 6.Marcel T. Three-dimensional on-screen virtual models. Am J Orthod Dentofacial Orthop. 2001;119:666–668. doi: 10.1067/mod.2001.116502. [DOI] [PubMed] [Google Scholar]
- 7.Santoro M, Galkin S, Teredesai M, Nicolay OF, Cangialosi TJ. Comparison of measurements made on digital and plaster models. Am J Orthod Dentofacial Orthop. 2003;124:101–105. doi: 10.1016/s0889-5406(03)00152-5. [DOI] [PubMed] [Google Scholar]
- 8.Quimby ML, Vig KWL, Rashid RG, Firestone AR. The accuracy and reliability of measurements made on computer-based digital models. Angle Orthod. 2004;74:298–303. doi: 10.1043/0003-3219(2004)074<0298:TAAROM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Im J, Cha JY, Lee KJ, Yu HS, Hwang CJ. Comparison of virtual and manual tooth setups with digital and plaster models in extraction cases. Am J Orthod Dentofacial Orthop. 2014;145:434–442. doi: 10.1016/j.ajodo.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 10.Palmer NG, Yacyshyn JR, Northcott HC, Nebbe B, Major PW. Perceptions and attitudes of Canadian orthodontists regarding digital and electronic technology. Am J Orthod Dentofacial Orthop. 2005;128:163–167. doi: 10.1016/j.ajodo.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Rheudea B, Sadowskyb PL, Ferrierac A, Jacobsond A. An evaluation of the use of digital study models in orthodontic diagnosis and treatment planning. Angle Orthod. 2005;75:300–304. doi: 10.1043/0003-3219(2005)75[300:AEOTUO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Mayers M, Firestone AR, Rashid R, Vig KW. Comparison of peer assessment rating (PAR) index scores of plaster and computer-based digital models. Am J Orthod Dentofacial Orthop. 2005;128:431–434. doi: 10.1016/j.ajodo.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 13.Okunami TR, Kusnoto B, Begole E, Evans CA, Sadowsky C, Fadavif S. Assessing the American Board of Orthodontics objective grading system: digital vs plaster dental casts. Am J Orthod Dentofacial Orthop. 2007;131:51–56. doi: 10.1016/j.ajodo.2005.04.042. [DOI] [PubMed] [Google Scholar]
- 14.Horton HM, Miller JR, Gaillard PR, Larson BE. Technique comparison for efficient orthodontic tooth measurements using digital models. Angle Orthod. 2010;80:254–261. doi: 10.2319/041709-219.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noh H, Nabha W, Cho J, Hwang H. Registration accuracy in the integration of laser-scanned dental images into maxillofacial cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2011;140:585–591. doi: 10.1016/j.ajodo.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 16.Slaj M, Spalj S, Jelusic D, Slaj M. Discriminant factor analysis of dental arch dimensions with 3-dimensional virtual models. Am J Orthod Dentofacial Orthop. 2011;140:680–687. doi: 10.1016/j.ajodo.2010.12.022. [DOI] [PubMed] [Google Scholar]
- 17.Danz JC, Katsaros C. Three-dimensional portable document format: a simple way to present 3-dimensional data in an electronic publication. Am J Orthod Dentofacial Orthop. 2011;140:274–276. doi: 10.1016/j.ajodo.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 18.Abdelkarim A. Myths and facts of cone beam computed tomography in orthodontics. J World Fed Orthod. 2012;1:e3–e8. [Google Scholar]
- 19.Abdelkarim A. A cone beam CT evaluation of oropharyngeal airway space and its relationship to mandibular position and dentocraniofacial morphology. J World Fed Orthod. 2012;1:e55–e59. [Google Scholar]