Abstract
Background:
Cardiovascular disease is the most common cause of death among Fabry disease patients, who carry significantly increased risk for heart failure and sudden cardiac death. Echocardiographic strain imaging and cardiac MRI are important clinical tools for early detection of cardiomyopathy before onset of systolic or diastolic dysfunction. However, studies on these imaging modalities are limited among Fabry patients.
Aim and Objective:
To evaluate echocardiographic strain pattern and correlation with cardiac MRI in Fabry disease.
Materials and Methods:
We performed a detailed analysis of global longitudinal strain and correlation with cardiac MRI finding in 9 patients diagnosed with Fabry disease.
Results:
Despite normal left ventricular ejection fraction, basal and mid inferior segments are more likely to demonstrate strain abnormalities compared to other regions. Additionally, increased interventricular septal and left ventricular posterior wall thickness are correlated with greater strain abnormalities. Finally, MRI evidence of fibrosis and infiltration are detected among most patients with strain abnormalities, but in some cases, strain imaging were able to detect early evidence of cardiomyopathy even before MRI was fully able to detect the change. Basal and mid inferoseptal segment strain abnormalities are early signs of developing cardiomyopathy among patients with Fabry disease.
Conclusion:
Though cardiac MRIs are critical tools for detection of myocardial infiltration and scarring, these findings may not always be detectable in early phases of the disease. Multiple imaging modalities maybe considered in monitoring and evaluation of cardiomyopathy in Fabry disease.
Keywords: Cardiac magnetic resonance imaging, echocardiogram, fabry disease, global longitudinal strain, regional strain
INTRODUCTION
Cardiovascular (CV) disease is the most common cause of death among patients with Fabry disease, responsible for death in 34% in male and 57% in female patients.[1] Fabry disease, an X-linked lysosomal storage disease, carries various CV complications including left ventricular (LV) hypertrophy, conduction abnormalities, coronary artery disease, mitral and aortic valve regurgitation, and aortic root dilation.[2] They are associated with significant CV morbidity and mortality, mainly due to increased risk for heart failure and sudden cardiac death.[3] CV imaging studies have shown early manifestation of LV dysfunction based on strain rate imaging with reduction in contractility in longitudinal followed by radial dimensions.[4] For this reason, strain rate imaging is critical for early detection of ventricular contractility impairment that may be overlooked by reliance on ejection fraction alone.[5] However, studies on strain pattern in Fabry patients are limited. Despite the significant mortality associated with CV dysfunction, our understanding of this disease process and its early cardiac effects are poorly understood. Furthermore, early diagnosis of Fabry-associated cardiomyopathy may prevent and delay its progression to more severe, irreversible conditions. For this reason, we investigated echocardiogram global longitudinal strain (GLS) and regional strain patterns among patients with Fabry disease and furthermore evaluated their correlations with cardiac magnetic resonance imaging (MRI) findings.
MATERIALS AND METHODS
Study patients
The study comprised nine adult patients diagnosed with Fabry disease through genetic testing. All of the patients have been diagnosed with Fabry disease for at least 5 years. Informed consent was obtained from all patients in the use of their medical records. During the office visits, clinical information was collected including demographic data, cardiac medical history, body mass index, cardiac MRI, standard echocardiogram information, GLS, and regional strain patterns. Cardiac MRI was obtained near the time of the echocardiogram used for analysis. The study was approved by the local institutional review board and conducted in accordance with the Declaration of Helsinki.
Standard echocardiography evaluation
LV end-diastolic dimensions and end-diastolic thickness of the posterior and septal walls were measured using standard M-mode in parasternal long-axis views. Right ventricular size and tricuspid annular plane systolic excursion (TAPSE) were measured in four-chamber views. LV ejection fraction (LVEF) was measured with the biplane Simpson method in apical four- and two-chamber views. Based on the most recent recommendations by the American Society of Echocardiography, diastolic dysfunction was determined by obtaining left atrial volume index, tricuspid velocity, E/e' ratio, and finally septal and lateral e' velocity. Diastolic dysfunction is present if: left atrial volume index > 34 ml/m2, tricuspid regurgitant systolic jet velocity > 2.8 m/s, average E/e' >14, and septal e' velocity < 7 and lateral e' velocity <10. If three or more criteria are positive, then E/A ratios will be examined and stage of diastolic dysfunction diagnosed based on the guideline.[6]
Regional strain analysis
GLS and regional strain measurements were performed using Siemen SC 2000 echocardiogram machines. Endocardial borders were outlined on apical four-chamber, three-chamber, and two-chamber views at the end-systolic frame. The system was tracked and divided the myocardial regions into standard segments and adjusted as indicated. Regional strains were obtained and analyzed for the following regions: (1) apical four-chamber view: inferoseptal (basal and mid), apical septal, apical lateral, and anterolateral (basal and mid) regions; (2) apical two-chamber vertical view: basal (basal, mid, and apical) and anterior (basal, mid, and apical); and (3) apical three-chamber horizontal view: inferolateral (basal and mid), apical lateral, apical septal, and anteroseptal (basal and mid) regions. Polar plot GLS patterns and the strain rates were also measured for each patient.
Cardiac magnetic resonance imaging
Cardiac MRI was performed on a Siemens Avanto 1.5T MR scanner using standardized imaging protocols. Conventional sequences were used to acquire cardiac function, mass, volumes, cardiac index, stroke volume, and scar imaging. The sequence used for detection of myocardial infiltration or scar is a delayed enhancement sequence, phase-sensitive inversion recovery (PSIR).Before this sequence, a time-to-inversion (TI) mapping sequence was performed to ensure the right TI for the delayed enhancement PSIR sequence was used.
Data analysis
Continuous data are presented as mean ± standard deviation and categorical variables as percentage (%). Pearson correlation test was used to determine the association between regional strain pattern and LV wall thickness. Normal strain value is defined as <−18%. Statistical analysis was performed using SPSS software (Windows version 11.5, SPSS, Inc. Chicago, IL, USA).
RESULTS
Patient population
Among nine patients included, 55.5% were males, 66.7% were Hispanic, and 22.2% were Caucasian. The mean body mass index was 24.9 ± 3.7, and the mean age was 50.6 ± 14.2 years. Comorbidities included 66.7% with hypertension, 44.4% with hyperlipidemia, and 11.1% with diabetes mellitus. No coronary artery disease or prior cardiac interventions were present in the study cohort. Patient demographic information is shown in Table 1. All patients were genetically diagnosed with different genotypes, with seven of nine patients having missense mutation.
Table 1.
Baseline characteristics
| Patient | Gender | Race | BMI | Age at echo | Age at diagnosis | Genotype | Variant type | ERT | Cardiovascular comorbidities | Cardiovascular medications |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | Hispanic | 29 | 40 | 28 | G328V | Missense | Yes | HTN, HLD | ASA, losartan |
| 2 | Male | Hispanic | 25 | 66 | 43 | R363H | Missense | Yes | HTN, Type 2 DM, HLD | ASA, atorvastatin, amlodipine |
| 3 | Male | Hispanic | 25 | 38 | 24 | W236R | Missense | No | HLD, HTN | Atorvastatin, spironolactone |
| 4 | Male | White | 23 | 49 | 21 | N272K | Missense | Yes | HTN | Metoprolol succinate |
| 5 | Female | Japanese | 23 | 59 | 16 | A143P | Missense | No | None | ASA |
| 6 | Female | Hispanic | 27 | 38 | 26 | G328V | Missense | No | None | N/A |
| 7 | Male | Hispanic | 17 | 68 | 59 | E358del | Small Deletion | Yes | None | Furosemide |
| 8 | Female | White | 26 | 65 | 60 | Y86H | Missense | Yes | HTN, HLD | ASA, atorvastatin, lisinopril, atenolol |
| 9 | Female | Hispanic | 29 | 32 | 26 | IVS4+4A>T | Intronic | Yes | HTN | N/A |
ASA=Aspirin, BMI=Body mass index, Echo=Echocardiogram, ERT=Enzyme replacement therapy, HTN=Hypertension, HLD=Hyperlipidemia, DM=Diabetes mellitus, N/A=Not applicable
Echocardiographic characteristics
The mean LVEF was 64.2% ± 6.5%. One patient had echocardiographic parameters meeting criteria for moderate diastolic dysfunction. One patient had severe concentric LV hypertrophy with interventricular septal (IVS) thickness of 2.1 ± 1.1 cm and left ventricular posterior wall (LVPW) thickness of 1.9 ± 1.1 cm with internal diameter of 3.9 ± 4.1 cm. Evaluation of right-sided function revealed a mean right ventricular TAPSE of 1.8 ± 0.3 cm and right ventricular diameter of 3.85 cm. The mean tricuspid regurgitation maximum velocity was 2.04 ± 0.3 m/s. Results are summarized in Table 2.
Table 2.
Fabry patients and standard echocardiographic characteristics
| Patient | LVEF (%) | IVSd (cm) | LVPWd (cm) | LVIDd (cm) | RVd (cm) | TAPSE (cm) | LA volume index (ml/m2) | TR maximum velocity (m/s) | E/e’ ratio | E/A ratio |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 63.2 | 1.1 | 1.1 | 5.7 | 3.6 | 2.1 | 29 | 2.1 | 6.2 | 1.1 |
| 2 | 57.5 | 1.1 | 1.0 | 3.9 | 9.1 | 1.2 | 21.2 | 2.3 | 13 | 1.1 |
| 3 | 60 | 1.2 | 1.1 | 3.7 | 3.1 | 2.2 | 28 | 1.8 | 7.1 | 1.6 |
| 4 | 65 | 1.1 | 1.2 | 4.1 | 3.4 | 2.1 | 27.7 | 2.6 | 13.4 | 0.9 |
| 5 | 62.9 | 0.8 | 0.8 | 3.9 | 3.1 | 1.9 | 24.4 | 1.8 | 9.2 | 1.3 |
| 6 | 60.4 | 0.9 | 0.9 | 4.2 | 3.8 | 1.6 | 24.9 | 1.7 | 8.7 | 1.8 |
| 7 | 79.3 | 2.1 | 1.9 | 3.9 | 2.9 | 1.3 | 96 | 2 | 9.1 | 1.2 |
| 8 | 68.3 | 1.2 | 1.2 | 3.8 | 3.3 | 2 48. | 8 | 2.5 | 18.4 | 1.6 |
| 9 | 61 | 0.8 | 0.8 | 4.3 | 2.6 | 1.8 | 18.5 | 1.6 | 8.2 | 1.9 |
| Mean | 64.6±6.1 | 1.2±0.4 | 1.1±0.3 | 4.2±0.6 | 4±1.9 | 1.8±0.3 | 37.5±22.9 | 2.1±0.3 | 10.6±3.7 | 1.3±0.3 |
LVEF=Left ventricular ejection fraction, IVSd=Interventricular septum during diastole, LVPWd=Left ventricular posterior wall during diastole, LVIDd=Left ventricular internal diameter during diastole, RVd=Right ventricular diameter during diastole, TAPSE=Tricuspid annular plane systolic excursion, LA=Left atrium, TR=Tricuspid regurgitation
Regional strain patterns
Apical four-chamber strain evaluation showed abnormal patterns in basal inferoseptal (−13% ± 10.1%) and mid inferoseptal (−12% ± 9.5%) segments, compared to other segments. Similar to apical two-chamber view, basal and mid inferior segments had abnormal strain patterns, −12.8% ±10.7% and − 13% ± 9.8%, respectively, while other segments tended to have regional strain near normal value of − 18.
From these cases, several important observations can be made. First, there was an inverse relationship between LV wall thickness and regional strain abnormalities in basal and mid inferoseptal segments. Pearson correlation analysis shows a significant correlation between IVS thickness and mid inferoseptal segment abnormality (r = 0.9, P = 0.003) and between LVPW thickness and mid inferoseptal segment abnormality (r = 0.8, P = 0.005). There was also a weak correlation between basal inferoseptal regional strain with IVS and LVPW thickness, though not statistically significant [Figure 1]. Second, there was no clear association of right ventricular systolic function or diameter with specific strain patterns. Third, there was no clear correlation between LV systolic function and strain patterns.
Figure 1.
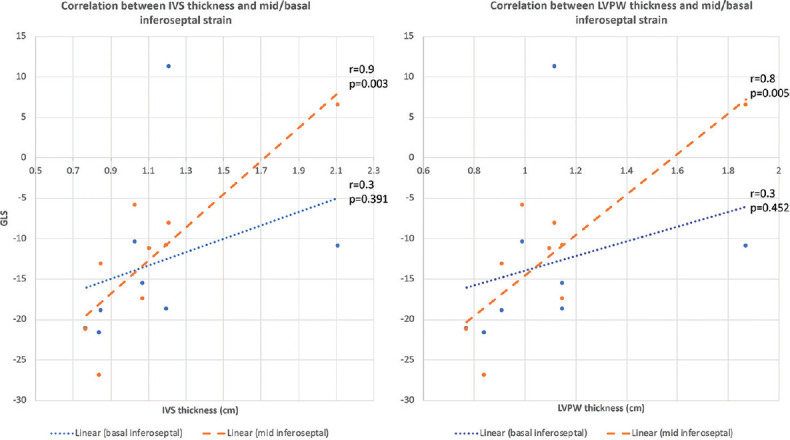
Correlation between interventricular septal and left ventricular posterior wall thickness with mid and basal inferoseptal regional strain patterns. There is an inverse relationship between left ventricular wall thickness and strain pattern in basal and mid inferoseptal segments. Pearson correlation analysis shows significant correlation between interventricular septal thickness and mid inferoseptal segment (r = 0.9, P = 0.003) and between left ventricular posterior wall thickness and mid inferoseptal segment (r = 0.8, P = 0.005)
Finally, the duration of Fabry disease diagnosis did not correlate with the severity of regional strain abnormalities in these patients. Patients (#2, 4, and 5) had been diagnosed for more than 20 years, but only patient #2 had regional strain abnormalities. There was no clear association between severity of regional strain and age of diagnosis.
Correlation of cardiac magnetic resonance imaging with regional strain abnormalities
Among the nine patients, eight received cardiac MRI evaluation. Five of them (#2, 3, 4, 5, and 9) did not have any evidence of inflammation, infiltration, or scar formation on cardiac MRI. Notably, patients #2 and #3 did have echocardiographic evidence of myocardial dysfunction in basal and mid inferoseptal regions based on regional strain pattern. The other three patients (#1, 7, and 8) had LV wall thickening with delayed hyperenhancement in basal and inferolateral myocardial regions. Among these three patients, the changes seen on cardiac MRI were reflected in two of the patients who also had abnormal echocardiogram strain patterns seen in mid and/or basal inferior regions as well. Results are shown in Table 3. Figure 2 shows the echocardiographic strain pattern and cardiac MRI from patient 7.
Table 3.
Echocardiogram strain analysis and cardiac magnetic resonance imaging findings
| Patient | Echocardiogram | Strain imaging | Cardiac MRI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||
| LVEF (%) | IVSd (cm) | LVPWd (cm) | LVIDd (cm) | Basal inferoseptal | Mid inferoseptal | Basal inferior | Mid inferior | Myocardial hypertrophy (severity/location) | Myocardial fibrosis | |
| 1 | 63.2 | 1.1 | 1.1 | 5.7 | −11.3 | −11.3 | −10.7 | −15.1 | Mild/septum | + |
| 2 | 57.5 | 1 | 1 | 3.9 | −10.4 | −5.9 | −18.3 | −15.9 | − | − |
| 3 | 60 | 1.2 | 1.1 | 3.7 | 11.2 | −8.1 | −10.2 | −9.3 | − | − |
| 4 | 65 | 1.1 | 1.2 | 4.1 | −15.6 | −17.5 | 9.1 | −13.4 | − | − |
| 5 | 62.9 | 0.9 | 0.8 | 3.9 | −21.7 | −26.9 | −12.2 | −26.2 | − | − |
| 6 | 60.4 | 0.9 | 0.9 | 4.2 | −18.9 | −13.2 | −10.5 | −10.5 | No MRI | No MRI |
| 7 | 79.3 | 2.1 | 1.9 | 3.9 | −10.5 | 6.8 | −11.2 | 5.3 | Severe/symmetric | + |
| 8 | 68.3 | 1.2 | 1.2 | 3.8 | −18.7 | −10.8 | −32.4 | −5.7 | Mild/symmetric | + |
| 9 | 61 | 0.8 | 0.8 | 4.3 | −21.1 | −21.2 | −15.5 | −26.5 | − | − |
LVEF=Left ventricular ejection fraction, IVSd=Interventricular septum during diastole, LVPWd=Left ventricular posterior wall during diastole, LVIDd=Left ventricular internal diameter during diastole, MRI=Magnetic resonance imaging
Figure 2.
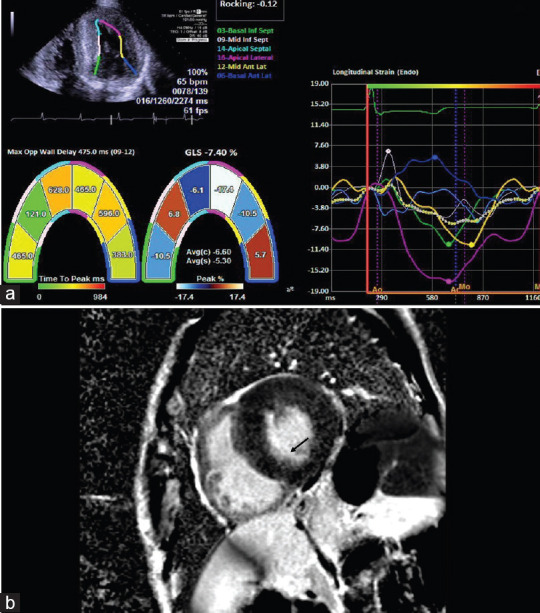
(a) Echocardiogram strain image and cardiac magnetic resonance imaging of a Fabry patient showing myocardial dysfunction with abnormal strain values and (b) myocardial fibrosis (black arrow), respectively
Sex-specific regional strain pattern findings
There were four females in this study group with a mean age of 48.5 ± 16.2 years and five males with a mean age of 52.3 ± 14 years. The mean LVEF was similar between malesfour-chamber regional strain pattern showed greater abnormal strain patterns in both basal and mid inferoseptal segments among males than females (−7.4% ± 10.6% and − 7.3% ± 8.9% vs. −21.7% ± 5% and − 20.1% ± 1.5%). Other strains' segments were similar and without evidence of significant abnormalities.
DISCUSSION
Our study demonstrated a relatively reduced regional strain in the basal and mid inferoseptal segments compared to apical and anterolateral regions in apical four-chamber view. Consistently, in apical two-chamber view, there is a relatively reduced regional strain in basal and mid inferior segments compared to apical and anterior segments. All of these patients had normal systolic function with LVEF ranging from 57% to 79%. Additionally, there was a strong correlation between mid inferoseptal regional strain with LV wall thickness. With increasing wall thickness, there were more abnormal strain patterns, which is one of the hallmarks of cardiomyopathy in Fabry disease. It is likely that mid and basal inferoseptal regions are early segments to show decline in cardiac function.
This study also highlights another important observation that average GLS value may not truly reflect the early dysfunction seen in regional strain.[7] As the classic GLS strain value noted in these studies was cumulative data of all segments, a closer observation showed that there may be significant discrepancies in regional strain value between each segment (i.e. overall regional strain of −18% with −30% in apical septal segment but −11.3% in basal and mid inferoseptal segments). This is an important concept that instead of focusing on the mean GLS value alone, close attention and evaluation of individual wall segments must be made to avoid overlooking early signs of cardiac dysfunction.
Different from congestive heart failure from other etiologies, LV dysfunction is not detected until advanced stage in Fabry disease. Among patients who died from Fabry disease, the diagnosis was made relatively late in age: median age of 40 years in men and 55 years in women.[1] The delay in diagnosis led to progression of cardiomyopathy into advanced stage, which contributed to the eventual death.[8] One of the pathognomonic markers of Fabry cardiomyopathy is found in inferolateral basal or mid basal segments seen on cardiac MRI and posterior basal segments on strain pattern.[9] Consistent with this finding, our study showed that abnormal strain patterns correlate with MRI findings. However, in two patients with abnormalities on strain analysis, cardiac MRI did not show signs of myocardial inflammation or scarring. For this reason, strain analysis may be a more sensitive tool to detect early myocardial changes that may not always be detected on cardiac MRI.
The mechanism underlying this selective inferior regional strain abnormalities in early stage of disease is not well understood and currently under investigation. Histological analysis shows accumulation of glycosphingolipids in cardiomyocytes, coronary vessel, cardiac conduction system, and valve leaflets. There is also increased interstitial fibrosis in subepicardial layer, especially in the posterolateral basal portion of the left ventricle.[2] Another recent case–control study on untreated Fabry disease patients showed greater abnormality in subepicardial longitudinal strain with an inverse relationship between maximal wall thickness and transmural strain and subepicardial strain.[10] Several anatomical and physiological conditions may predispose myocardial dysfunction in this region. The basal inferior portion of the myocardium maybe more prone to accumulation of glycosphingolipids due to decreased capillary density and increased diastolic filling pressures causing poor motility. Additionally, the deposition of glycosphingolipids in the endothelium of small arterioles and capillaries may lead to microvascular ischemia and thus fibrosis in the region.[11] This is supported by positron emission tomography studies conducted among patients with Fabry disease. Despite normal coronary arteries on angiogram, there is reduced coronary flow reserve suggesting microvascular dysfunction and potentially ischemia.[11,12]
The strength of this study is the detailed review of strain pattern and correlation with cardiac MRI findings. The limitations are the small cohort of patients and lack of control group without Fabry disease. The small cohort of this study may not make the conclusion generalizable but paves a way for larger population study. Additionally, different from other studies where strain patterns on echocardiogram are readily obtainable among patients without Fabry disease, cardiac MRIs were not routinely done on those without high suspicion for cardiomyopathy and thus difficult to find a healthy, control group with cardiac MRI data. Finally, the echocardiographic measures were not performed by 1 operator but by 2–3 operators, which may lead to some variability.
CONCLUSION
Our study showed that evidences of regional strain abnormalities in basal and especially mid-inferoseptal regions of the left ventricule are early indications of myocardial dysfunction among patients with Fabry disease. Equally important, although cardiac MRIs are critical tools for detection of myocardial infiltration and scarring, these findings may not always be detectable in early phases of the disease. Even before reaching detection level on MRI, echocardiographic strain analysis can help in detecting early abnormalities of cardiomyopathy. Multiple imaging modalities and detailed strain analysis are highly recommended among Fabry patients in detecting and preventing cardiomyopathy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mehta A, Clarke JT, Giugliani R, Elliott P, Linhart A, Beck M, et al. Natural course of Fabry disease: Changing pattern of causes of death in FOS-Fabry outcome survey. J Med Genet. 2009;46:548–52. doi: 10.1136/jmg.2008.065904. [DOI] [PubMed] [Google Scholar]
- 2.Akhtar MM, Elliott PM. Anderson-Fabry disease in heart failure. Biophys Rev. 2018;10:1107–19. doi: 10.1007/s12551-018-0432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel V, O'Mahony C, Hughes D, Rahman MS, Coats C, Murphy E, et al. Clinical and genetic predictors of major cardiac events in patients with Anderson-Fabry disease. Heart. 2015;101:961–6. doi: 10.1136/heartjnl-2014-306782. [DOI] [PubMed] [Google Scholar]
- 4.Weidemann F, Breunig F, Beer M, Sandstede J, Störk S, Voelker W, et al. The variation of morphological and functional cardiac manifestation in Fabry disease: Potential implications for the time course of the disease. Eur Heart J. 2005;26:1221–7. doi: 10.1093/eurheartj/ehi143. [DOI] [PubMed] [Google Scholar]
- 5.Linhart A. The heart in Fabry disease. In: Mehta A, Beck M, Sunder-Plassmann G, editors. Fabry Disease: Perspectives from 5 Years of FOS. 20. Oxford: Oxford PharmaGenesis; 2006. [PubMed] [Google Scholar]
- 6.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314. doi: 10.1016/j.echo.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Stokke TM, Hasselberg NE, Smedsrud MK, Sarvari SI, Haugaa KH, Smiseth OA, et al. Geometry as a confounder when assessing ventricular systolic function: Comparison between ejection fraction and strain. J Am Coll Cardiol. 2017;70:942–54. doi: 10.1016/j.jacc.2017.06.046. [DOI] [PubMed] [Google Scholar]
- 8.Waldek S, Patel MR, Banikazemi M, Lemay R, Lee P. Life expectancy and cause of death in males and females with Fabry disease: Findings from the Fabry Registry. Genet Med. 2009;11:790–6. doi: 10.1097/GIM.0b013e3181bb05bb. [DOI] [PubMed] [Google Scholar]
- 9.Jurcut R. Third in a series on Fabry disease: What is the importance of imaging in Fabry disease? Ejournal Cardiol Pract. 2016;14:9–26. [Google Scholar]
- 10.Esposito R, Santoro C, Sorrentino R, Riccio E, Citro R, Buonauro A, et al. Layer-specific longitudinal strain in Anderson-Fabry disease at diagnosis: A speckle tracking echocardiography analysis. Echocardiography. 2019;36:1273–81. doi: 10.1111/echo.14399. [DOI] [PubMed] [Google Scholar]
- 11.Elliott PM, Kindler H, Shah JS, Sachdev B, Rimoldi OE, Thaman R, et al. Coronary microvascular dysfunction in male patients with Anderson-Fabry disease and the effect of treatment with alpha galactosidase A. Heart. 2006;92:357–60. doi: 10.1136/hrt.2004.054015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tomberli B, Cecchi F, Sciagrà R, Berti V, Lisi F, Torricelli F, et al. Coronary microvascular dysfunction is an early feature of cardiac involvement in patients with Anderson-Fabry disease. Eur J Heart Fail. 2013;15:1363–73. doi: 10.1093/eurjhf/hft104. [DOI] [PubMed] [Google Scholar]


