Abstract
Background:
Autologous platelet concentrate (APC)/platelet-rich fibrin (PRF) of second and third generations has increased use in periodontics to optimize wound healing. Few systematic reviews (SRs) have reported improved clinical outcomes, while other studies reported significantly better results for the connective tissue graft (CTG). There is still unclear clinical evidence about APC/PRF use to treat gingival recession (GR) defects. Then, the purpose of this SR was to evaluate the use of APC/PRF membranes (2nd and 3rd generations) in root coverage (RC) procedures and assess its efficacy as a substitute biomaterial.
Materials and Methods:
An electronic search was conducted in PubMed, Cochrane Central, Web of Science, Google Scholar, BookSC databases, and gray literature. The search strategy, without date restriction up to April 2020, included keywords as “platelet-rich fibrin,” “autologous platelet concentrates,” “blood,” “systematic review,” “periodontics,” “surgery,” “tissue,” “gingiva,” “gingival recession,” “connective tissue,” “graft,” and “root coverage.” The methodological quality was evaluated through the AMSTAR2, and a population, index test, comparator, outcome strategy was used to assess specific clinical parameters such as recession depth, clinical attachment levels, and RC outcomes.
Results:
Nine SRs were included. Only three articles described the technique of APC/PRF production. Three studies reported unfavorable outcomes using APC, while six reported favorable results and postoperative discomfort reduction. Articles included in this SRs that provided information about APC/PRF membranes (n = 13) showed no significant difference between APC/PRF and the control group for the parameters analyzed.
Conclusions:
This implies that APC/PRF may be considered a feasible substitute biomaterial for treating GR defects, although the CTG still provides superior outcomes. Further long-term and controlled studies are needed to verify this finding.
Keywords: Autologous platelet concentrate, gingival recession, periodontal surgery, root coverage, systematic review
INTRODUCTION
Gingival recession (GR)[1,2] is prevalent among all age groups.[3] It is defined as gingival migration to an apical point to the cementoenamel junction, exposing the root surface and involving loss of periodontal attachment apparatus. Many etiological factors are involved in the development of GR defects,[2,4] such as the presence of muscle insertion close to the gingival margin,[2,5] reduced thickness of the alveolar bone,[6] inadequate tooth alignment,[7] reduced width of attached keratinised tissue width (KTW),[8,9] traumatic factors such as piercings[4] or incorrect toothbrushing procedures,[10] restorations invading supracrestal tissues attachment,[11] plaque-induced periodontal disease,[12] and viruses.[13] Moreover, GR defects are often associated with hypersensitivity,[9] root caries, and cervical abrasion.[14,15]
GR defects are likely to progress with time if left untreated.[16,17] This treatment is part of periodontal plastic surgery.[18] Many root coverage (RC) techniques have been developed to obtain predictable RC.[1,16,19,20] The most common methods involve the adjuvant use of either a connective tissue graft (CTG) or de-epithelized free CTG,[21] which are considered to be the gold standard for RC treatment.[15]
Periodontal plastic surgery using CTG may increase the operative time, donor site morbidity, and pain. As a result, researchers have developed other biomaterials/biologic agents as substitutes, including but not limited to allogeneic grafts,[19] xenogeneic or synthetic collagen membranes,[22] enamel matrix derivative (EMD), or autologous platelet concentrate (APC)/platelet-rich fibrin (PRF) of second and third generation (membranes).
Among alternative biomaterials, APC/PRF has gained attention, mainly the second generation of membranes. It is a strong natural fibrin matrix enriched with platelets, cytokines, and growth factors, without risk of cross-infection.[23] APC/PRF is also easy to harvest and manipulate and presents a reduced production cost with good mechanical properties.[24] In addition, alkaline phosphatase activity is significantly upregulated by PRF.[24] This three-dimensional scaffold allows a continuous release of growth factors and cytokines over 10 days,[25] enhancing the early stages of tissue repair.
Using APC, previous SRs have reported improvement in clinical attachment levels (CAL) and mean and complete RC (CRC) outcomes. However, a limited number of studies described the use of APC as a biomaterial of choice.[21,26]
In summary, the current clinical evidence is still unclear for practitioners. There is great confusion in the literature regarding outcomes and indications on the use of APC to treat GR defects.[27,28,29,30,31,32,33,34,35,36,37,38,39] Considering the controversial options, a SR is essential before making any precise clinical recommendations on the treatment of GR using APC. This review contributes to the current debate on the adoption of this biomaterial as a substitute for CTG.
Thus, the purpose of the present SR and meta-analysis was to evaluate published SRs on the use of APC/PRF, specifically concerning the membranes of 2nd and 3rd generation, in periodontal surgeries for RC.
MATERIALS AND METHODS
Protocol development
A detailed protocol was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement[40] to systematically review the literature regarding periodontal surgeries for the treatment of GR defects. The present manuscript investigated only the evidence of systematic reviews (SRs). The protocol was registered on PROSPERO (Centre for Reviews and Dissemination [CRD], University of York) (CRD42020168582). The clinical question established for the search strategy was organized using the population, index test, comparator, outcome (PICO) framework.[41]
Focused question
The PICO-focused question for the present review was as follows: “Can GR defects (single or multiple) (P) be surgically treated applying APC/PRF (membranes of 2nd and 3rd generations) as the sole filling material (I), as a substitute for the gold standard CTG (C), and exhibit significantly improved clinical outcomes (O)?”
Search strategy
An electronic search, with no date restriction and only in the English language, was conducted in the PubMed/MEDLINE, Cochrane Central, Web of Science, Google Scholar, and BookSC databases up to April 30, 2020. Furthermore, a hand search was performed, and the gray literature report and OpenGrey databases were examined to identify unpublished studies (gray literature). Searches in the reference lists of the included studies (cross-referencing) were also conducted.
Medical subject heading (MeSH) terms, keywords, and other free terms related to “platelet-rich fibrin,” “autologous platelet concentrates,” “blood,” “systematic review,” “periodontics,” “surgery,” “tissue,” “gingiva,” “gingival recession,” “connective tissue,” “graft,” and “root coverage” were used with Boolean operators (OR, AND) to combine searches. The search strategy included appropriate changes in the keywords and followed the syntactic rules of each database.
Inclusion and exclusion criteria
This SR selected studies by the following inclusion criteria: The paper must identify itself as a SR for the treatment of GR including human studies; it must be in English language; it must have included detailed information about the treatments performed and the results obtained; it must have applied platelet concentrates (membrane) as a test treatment modality, involving second and third generation of PRF. In addition, only the publication with the longest follow-up data was included, in case of an updated publication of the same group.
SRs that did not meet the entire inclusion criteria and did not achieve scoring between 8 and 16 points on the AMSTAR 2 checklist[42] were excluded, just as in vitro studies, animal studies, case reports, clinical studies, consensus, and review articles that were not systematically performed. Studies that included patients with a significant health problem (American Society of Anesthesiologists Physical Status 3 and above) or used only CTG or another APC of a nonmembrane type were also rejected.
Data extraction and method of analysis
The search and screening process was performed by two independent review authors (GVOF and JCHF), who extracted the data independently from the selected articles for further analysis, using data extraction tables, which included the following parameters: author(s) and year of publication, the focused question, the journal of publication and impact factor, the observation period, and the number of studies included; the number and characteristics of patients treated and whether for localized or multiple recession; type of interventions (flap, technique, biomaterials), outcome measures achieved for CAL, CRC, mean RC (MRC), and recession depth (RD); and whether the study contained meta-analysis, a conclusion, and occurrence of adverse effects or postoperative complications.
Selection of studies
Duplicates were excluded, and the remaining articles were screened by title and abstracts for eligibility. Further examination regarding inclusion and exclusion was subsequently made by full-text analysis. The full text of any title or abstract that did not provide enough information regarding the inclusion criteria was also obtained. The same authors (GVOF and JCHF) performed the selection and analysis, and any disagreement was discussed with a third author (NBMS). Cohen's kappa test was adopted to evaluate the reviewers' consensus.
Risk of bias and method of analysis
The same two review authors independently assessed the risk of bias and study quality of the included SRs. The methodological quality of each SR was evaluated using the AMSTAR 2 tool. The guidelines featured 16 items answered with one of four options: 1, yes; 2, no; 3, cannot answer; and 4, not applicable. Only items with option 1 generated the score. Therefore, each article could obtain a score of between 0 (no criteria fulfilled) and 16 (all criteria fulfilled).
The data collected using the AMSTAR 2 tool were rated as low quality if it scored 0–5 out of a total of 16 points, of moderate quality if it scored 6–10, or high quality if it scored between 11 and 16. The AMSTAR ratings were verified by a third reviewer (NBMS) and any discrepancy was resolved by discussion with another reviewer (RACS). Only studies scoring 8 or more were included in the present review.
The studies of interest included within the SRs were scrutinized according to the theme proposed after in-depth analysis and meta-analysis. Then, other characteristics were addressed, such as the randomization process, groups similar at baseline, blinded group allocation, random housing, blinded interventions, random and blinded outcome assessment, reporting of dropouts, and other biases (funding) domains. The mean and standard deviation values were found for final RD, final CAL, and RC and assessed. All analysis was performed using 5% of the significance level.
The heterogeneity across the studies was quantified using the Q (Chi-squared) statistic, and df was its degrees of freedom.[43] They described the percentage of the variability in effect estimates that was due to heterogeneity rather than to sampling error (chance). Tau was a measure of residual between dispersions expressed in the same units as the effect estimate, Tau2 was an estimate of the residual between variances expressed in squared units of the effect estimate, H2 estimated the ratio of the unaccounted variability relative to the sampling variability, and the Higgins index (I2) inconsistency test was also performed.
When the homogeneity between the studies was acceptable (P ≥ 0.10, I2 ≤ 50%), the fixed-effect model was used for meta-analysis. The random-effects models were applied when significant heterogeneity existed (P < 0.10, I2 > 50%). However, the percentage for I2 classified between 0% and 40% might not be significant, 30%–60% might represent moderate heterogeneity, 50%–80% might represent substantial heterogeneity, and 70%–100% might present considerable heterogeneity. I2 estimates how much of the unaccounted variability (residual heterogeneity + sampling error) is attributable to residual heterogeneity.
RESULTS
Description of enrolled studies
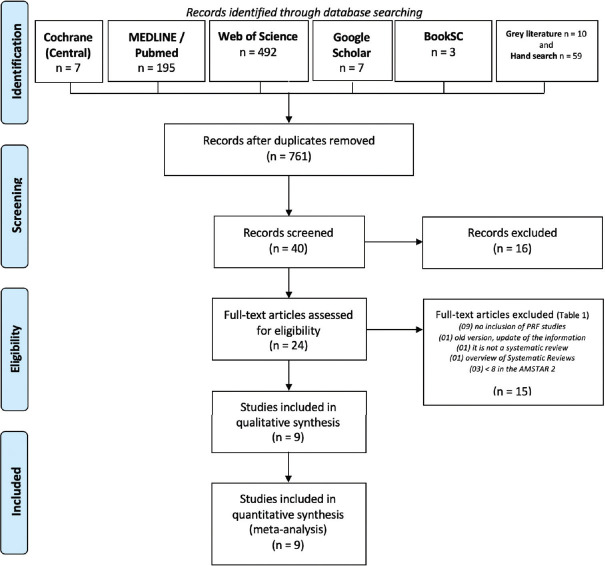
The initial electronic search provided 773 papers, and after the removal of duplicates (n = 12), 761 remained. After reviewing the titles and abstracts, 40 articles associated APC with GR, excluding 721 papers. Through a detailed analysis from the title and abstract, 16 more were removed, leaving 24 for full-text review.
From the 24 articles assessed for eligibility, 15 were excluded after full-text review [Table S1]. The reasons for exclusion were: The article included treatment of GR but did not include APC studies (n = 9), the article did not achieve a score of at least 8 with the AMSTAR 2 tool (n = 3) Table 1, one was an overview of SRs (n = 1), one was not a SR, and the last was a previous version of an updated article.
Table S1.
Excluded studies and reason for exclusions
| Quantity | Authors, year | Reasons for exclusion |
|---|---|---|
| 9 | Oates et al., 2003 | Without inclusion of APC/PRF studies |
| Chambrone et al., 2010 | ||
| Laugisch et al., 2012 | ||
| Cairo et al., 2014 | ||
| Basseti et al., 2016 | ||
| Cairo et al., 2016 | ||
| Chambrone & Tatakis, 2016 | ||
| Dai et al., 2018 | ||
| Tavelli et al., 2018 | ||
| 3 | Hofmänner et al., 2012 | Score <8 in the AMSTAR 2 analysis |
| Miron et al., 2017 | ||
| Verma et al., 2017 | ||
| 1 | Ting et al., 2018 | Overview of systematic reviews |
| 1 | Mohan et al., 2019 | It is not a systematic review |
| 1 | Chambrone et al., 2018 | Old version, update of the information |
AMSTAR – Assessment of multiple systematic reviews; APC – Autologous platelet concentrates; PRF – Platelet-Rich Fibrin
Table 1.
AMSTAR-2 rating after full-text articles analysis
| Study | Score out of 16 | Status |
|---|---|---|
| Amine et al., 2017 | 10 | Included |
| Castro et al., 2017 | 11 | Included |
| Chambrone and Tatakis, 2015 | 9 | Included |
| Chambrone et al., 2019 | 11 | Included |
| Del Fabbro et al., 2011 | 9 | Included |
| Hofmänner et al., 2012 | 5 | Excluded |
| Li et al., 2019 | 14 | Included |
| Luo et al., 2015 | 12 | Included |
| Miron et al., 2017 | 6 | Excluded |
| Moraschini and Barboza, 2016 | 11 | Included |
| Valenzuela and Oliva, 2014 | 8 | Included |
| Verma et al., 2017 | 1 | Excluded |
Finally, 9 SRs[26,44,45,46,47,48,49,50,51] were included for qualitative synthesis and quantitative analysis, providing data to perform the meta-analysis [Figure 1]. Only articles on APC in the membrane-shaped approach (n = 13) within the 9 SRs were included for statistical analysis. A detailed analysis was conducted for each SR and the original articles included in them. The k values of agreement between the two authors/reviewers for potential article inclusion were 0.90 and 0.85 for the selected articles, which showed excellent agreement.
Figure 1.
PRISMA flow diagram of the screening and selection process; n - number
Systematic reviews included
Two SRs[45,49] presented a moderate-quality study and 5[44,45,46,47,48] high-quality qualifications with the AMSTAR 2 tool. In addition, 5 SRs[26,47,48,49,51] chose the PRISMA statement as the standard guideline for its development. Castro et al.[48] also used the guidelines of the Belgian Centre for Evidence-Based Medicine. Three studies[44,45,46,50] did not report any standard applied. Beyond this, only one study[47] was registered in the International Prospective Register of SRs (PROSPERO) platform, and another study[50] did not describe the database used.
Three out of 9 articles described the APC technique of production.[45,47,48] However, the common protocols were 2700 revolutions per minute (RPM)/12 min or 3000 RPM/10 min, or still 400 g/10 min.[45]
Chambrone and Tatakis[26] and Chambrone et al.[50] did not offer conclusions about PRF, even after inserting data in the table. Furthermore, the authors reported that all RC procedures led to RD reduction and CAL gain.[50] However, SCTG + coronally advanced flap (CAF) was still the gold standard,[49,50] with an incidence of adverse effects (discomfort with or without pain) related to donor sites of SCTG within the first postoperative week.[50]
Three authors[44,47,49] were not in favor of APC, and their results were contradictory:[49] a nonsignificant benefit to treating GR,[44] no improvement of RC or CAL,[47] and a lack of a standardized protocol for the preparation of PRF membranes.[47,48,49] Three other articles[45,48,51] reported favorable effects on soft-tissue healing and postoperative discomfort reduction with good biological effects, low cost, and ease of preparation.[48] Li et al.[51] considered that PRF “should be preferred” for the treatment of Miller's Class I and II GR, and Valenzuela and Oliva[45] concluded that the regeneration efficacy of PRF in periodontal surgery is effective. Another SR[46] suggested that the addition of APC might exert a positive adjunctive effect in the treatment of GR [Table 2].
Table 2.
Details Characteristics of each SR included in this Study
| Part I | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Authors | Year | Journal | Was the systematic review standardized? | Databases/sources | Goal | AMSTAR2 rating |
| Amine et al. | 2017 | J Stomatol Oral Maxillofac Surg | PRISMA statement. The present manuscript was written according to PRISMA checklist | MEDLINE (PubMed), Cochrane, and EBSCO | Assess the clinical efficacy of alternatives procedures; ADM, XCM, EMD, and PRF, compared to conventional procedures in the treatment of localized gingival recessions | Moderate |
| Castro et al. | 2017 | J Clin Periodontol | Guidelines of the Belgian CEBAM, Belgian branch of the Dutch Cochrane centre and the PRISMA statement; limited to studies involving humans; no language or time restrictions; only studies in English; no follow-up limitations | MEDLINE/PubMed, EMBASE (Excerpta Medical Database by Elsevier), and Cochrane Central Register of Controlled Trials (CENTRAL), hand searches, citation screening, and expert recommendations | Study the beneficial effect of L-PRF used as sole filling material and as adjunct to conventional techniques in periodontal surgery | High |
| Chambrone and Tatakis | 2015 | J Periodontol | PRISMA, Cochrane collaboration, and check review checklists; without language restriction | MEDLINE, EMBASE, and hand search of any potential studies and the databases of four periodontal journals | Determine the best, practical way to treat patients with periodontal regeneration, as well as to prepare solid guidelines and treatment rationale to support decision-making for specific clinical scenarios | Moderate |
| Chambrone et al. | 2019 | J Periodontol | Not described in the text of the article. The authors referenced to other 3 articles* | Not described in the text of the article. The authors referenced to other 3 articles* | Evaluated the efficacy of different root coverage procedures in the treatment of single and multiple gingival recession | High |
| Del Fabbro et al. | 2011 | J Periodontol | Clinical trials involving human subjects, no language or time restriction was applied | MEDLINE, EMBASE, the Cochrane central register of controlled trials, and hand search | Determine whether the use of autologous platelet concentrates may affect the outcome of regenerative procedures for the treatment of periodontal defects and gingival recession | Moderate |
| Li et al. | 2019 | BioMed Research International | PRISMA; only English articles were included; only RCT | Medline, EMBASE, Cochrane Central Register of Controlled Trials, hand search of the following Periodontology journals, bibliographies of all selected articles and relevant reviews were also searched for missing articles. In addition, gray literature was obtained from Google Scholars (https://xue.glgoo.org/). Unpublished and ongoing trials were obtained from the trial registries (EU clinical trials Register: https://www.clinicaltrialsregister.eu) | Evaluate whether the three generations of APCs could provide additional effect to CAF for gingival recessions, thus to provide guidance to practitioners in their clinical work - only miller Class I and II | High |
| Luo et al. | 2015 | Journal of Oral Rehabilitation | Only RCTs with a follow-up ≥3 months, | MEDLINE, PUBMED, EMBASE, Cochrane central register of controlled trials, and hand search was carried out in the major international journals in the field of Periodontology | Evidence-based systematic review and meta-analysis was to figure out whether adjunctive use of platelet concentrates could affect the outcomes of regenerative procedures for the treatment of gingival recession | High |
| Moraschini and Barboza | 2016 | J Periodontol | PRISMA and AMSTAR guideline checklists; without restrictions on dates or language Registered in PROSPERO (CRD42015026444) | PubMed/MEDLINE, Cochrane Central register of controlled trials, Web of Science, EMBASE, manual searches of the following regular journals, Unpublished studies (gray literature) were identified by searching the open-GRAY database and the clinicaltrials.gov database, and references of the included studies (cross-referencing) were performed | Evaluate the effects of the use of PRF on the outcomes of the clinical treatments of patients with gingival recession | High |
| Valenzuela and Oliva | 2014 | Int J Odontostomatology/Not found | No language restrictions were applied | The Cochrane central register of controlled trials (CENTRAL; The Cochrane Library), MEDLINE (PubMed), EMBASE (via OVID), science citation index, Google scholar, and reference lists of the most relevant studies and engines search were checked for possible additional studies | Assess the regeneration efficacy of PRF in periodontal surgery | Moderate |
|
| ||||||
| Part II | ||||||
|
| ||||||
| Authors | Focused question | APC/PRF production (technique) | Groups | Number of studies included | Studies included in this SR/justification | Conclusions |
|
| ||||||
| Amine et al. | NR | NR | CAF CAF + EMD CAF + PRF CAF + CTG | 18 | Included: n=5/Included studies that applied PRF | SCTG is still the gold standard procedure (treatment of miller Class I and II recession-type defects) PRF studies have reported contradictory results Furthermore, a standardized protocol for the preparation of PRF membranes should be followed |
| Castro et al. | Does L-PRF promote periodontal wound healing during periodontal surgery compared to traditional techniques? | L-PRF (protocol 2700 RPM/12 min or 3000 RPM/10 min) | L-PRF (alone or associated to another biomaterial) versus CTG | 24 for SR and 14 for meta-analysis | Included: n=9[33,34,35,36,37,38,39,40,41]/Nine articles were related to Periodontal plastic surgery via CAF, with or without connective tissue graft | Favorable effects on soft tissue healing and postoperative discomfort reduction were often reported when L-PRF was used Standardization of the protocol is needed to obtain an optimal effect of L-PRF in regenerative procedures Correct handling of L-PRF as well as the use of enough clots/membranes per surgical site might be crucial to obtain benefits from this technique This biomaterial can be taken into consideration due to its reported good biological effects, low costs, and ease of preparation |
| Chambrone and Tatakis | What is the efficacy/effectiveness of RC procedures by the degree of recession? Miller Class I and II Miller Class III or IV What is the anticipated success and attachment apparatus of RC enhancements with autogenous grafts compared with alternative methods and materials? What are the relative risks from a patient’s viewpoint with the different approaches to RC procedures? |
NR | Part I: An overview of the base of SRs Part II: An alternative random-effects meta-analysis on mean percentage of RC and sites exhibiting complete RC Part III: An SR of nonrandomized trials exploring other conditions not extensively evaluated by previous SRs |
Part I: 17 for SRs Parts II and III: 94 were assessed and 52 following for meta-analysis |
Included: Part I, n=0 Articles observed but excluded (justification) n=15 - did not involve PRF membranes, n=2 - PRP [16,52] Included: PART II and III, n=4 Articles observed but excluded (justification) n=1 - PRP[53]; n=1 - fibrin glue[54]; n=1 - FFSS[55] - biomaterial existent before PRF/only studies that used PRF as type of treatment |
Did not conclude about APC/PRF |
| Chambrone et al. | NR | NR | FGG, LPF, CAF, SCTG alone or in combination with LPF or CAF, CAF in association with allograft (e.g., ADMG, others), GTR (with resorbable or nonresorbable membranes), EMD, XCM or other biomaterial Similar procedures (e.g., CAF with vertical incisions versus MCAF, without vertical incisions, etc.) |
48 for SR and 20 for meta-analysis | Included: n=4 Articles observed but excluded (justification) 01 Keceli et al. - used PRP[56] 01 Trombelli et al. - used fibrin glue[54]/treatment of single or multiple miller’s Class I or II gingival recession (recession depth>3 mm), as well as at least 10 participants per group at final examination (with a follow-up<5 years |
All RC procedures led to RD reduction and CAL gain The available evidence base indicates that the most suitable options for RC of GR, in terms of clinical outcomes and cost-to-benefit ratio, are: SCTG + CAF (gold standard); ADMG plus CAF; EMD + CAF; XCM + CAF; and CAF alone Moreover, evidence suggests that SCTG promoted better stability of the gingival margin/some degree of creeping attachment over time, compared to other surgical approaches The incidence of adverse effects, such as discomfort with or without pain, was mainly related to donor sites of SCTG. However, these conditions occurred mainly within the first week after surgery and did not influence on RC outcomes |
| Del Fabbro et al. | NR | NR | NR | 24 for SR and 14 for meta-analysis (6, treatment of GR) | Included: n=1 Article observed but excluded (justification) Platelet concentrates different of membrane structure (PRP or PCG, n=5)/only study that used PRF membrane in GR treatment |
No significant benefit of platelet concentrates was found for gingival recession |
| Li et al. | GR that attained RC; Change in RD was expressed as a reduction in recession at the final evaluation | NR | NR | 8 for SR and 8 for meta-analysis | Included: n=5 Article observed but excluded (justification) 3 excluded - PRP[53,56,57]/only APC/PRF in membrane type |
We considered that PRF should be preferred for the treatment of Classes I and II gingival recessions Overall, the risk of bias of the articles included in APCs was high, and more low-risk and high-quality researches were needed |
| Luo et al. | Primary outcome variable was the change in gingival RD | NR | Platelet concentrates or placebos were used in certain regenerative procedures of gingival recessions | 9 for SR and 9 for meta-analysis | Included: n=2 Article observed but excluded (justification) PRP [53,56,58,59]; PDGF[60,61]; PRF[62] - only KTW results/only concentrates in membrane-shaped with results of GR treatment |
Indicated that the addition of platelet concentrates might exert a positive adjunctive effect in the treatment of gingival recession |
| Moraschini and Barboza | What are the effects of PRF membranes on the treatment of gingival recession? | 3000 RPM×10 min or 2700 RPM×12 min | PRF + CAF CAF alone CTG + CAF |
n=7 | Included: n=7 [33,34,35,36,37,38,39]/compared the performances of PRF in patients with miller Class I or II gingival recession | PRF membranes did not improve the RC, or CAL in the treatment of miller Class I and II gingival recessions compared with the other treatment modalities |
| Valenzuela and Oliva | Autologous PRF for regeneration of soft tissues in the oral Efficacy for soft tissue considered the outcome of mean gain of PD and mean gain of clinical attachment level |
NR | PRF + CAF (test) CTG + CAF (Control) | 11 RCT for SR; 6 for meta-analysis | Included: n=1[35] Article observed but excluded (justification) 1 study compared PRF with PRF + BPBM and it had not control group[63] did not have the mean change[34]/Only one was related to gingival recession; other were about intrabone defects (4) and furcation (1) |
The regeneration efficacy of PRF in periodontal surgery is effective according to present information of RCT |
*(a) Chambrone L, Salinas Ortega MA, Sukekava F, Rotundo R, Kalemaj Z, Buti J, et al. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst Rev 2018;10:CD007161; (b) Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root coverage procedures for the treatment of localised recession-type defects. Cochrane Database Syst Rev 2009;2:CD007161; (c) Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root-coverage procedures for the treatment of localized recession-type defects: A Cochrane systematic review. J Periodontol 2010;81:452-78. CEBAM – Centre for Evidence-Based Medicine; EMBASE – Excerpta Medica Database; MEDLINE – Medical Literature Analysis and Retrieval System Online; RCT – Randomized controlled trials; AMSTAR – Assessment of Multiple Systematic Reviews; RC – Root coverage; FFSS – Fibrin-fibronectin sealing system; ADM – Acellular dermal matrix; APC – Autologous platelet concentrate; CAF – Coronally advanced flap; EMD – Enamel matrix derivates; L-PRF – Leukocyte and platelet-rich fibrin; PRF – Platelet-rich fibrin; PRISMA – Preferred Reporting Items for Systematic Reviews and Meta-Analyses; XCM – Xenogeneic collagen matrix; BPBM – bovine porous bone mineral; CTG – Connective tissue graft; EU – European Union; FGG – Free gingival grafts; GTR – Guided tissue regeneration; GR – Gingival Recession; IF – Impact Factor; KTW – Keratinized tissue width; LPF – Laterally positioned flap; MCAF – Modified-coronally advanced flap; PD – Probing depth; RD – Recession depth; RPM – Revolutions per minute; SCTG – Subepithelial connective tissue graft; SR – Systematic review; NR – Not Reported; n – number; ADMG – Acellular dermal matrix graft; PRP – Platelet-Rich Plasm; CAL – Clinical attachment level; PCG – Platelet concentrates graft; PDGF – Platelet-derived growth factors;
Randomized controlled trials from included systematic reviews
Only 13 randomized controlled trials (RCTs)[27,28,29,30,31,32,33,34,35,36,37,38,39] were analyzed and included in the meta-analysis. The average follow-up period was 6 months, but 3[28,36,39] studies had a longer follow-up of 12-month. In general, the studies were split-mouth, not blinded,[27,28,30,32,33,34,37,38,39] or single-blinded.[29,31,35,36] Thamaraiselvan et al.[35] and Gupta et al.[33] selected a parallel design. Kuka et al.[39] only selected Miller's Class I (currently RT1)[52] patients. All other studies included Miller's Class I and II (currently RT1).[52]
The quality assessment indicated 7 articles[28,33,34,35,36,38,39] that were classified as moderate risk (two criteria were not met or were unclear) and 6[27,29,30,31,32,37] as high risk (three or four criteria were not met or were unclear) [Figures 2 and 3]. The weight of each study was calculated proportionally to the number of citations. Therefore, the most relevant articles were Aroca et al.,[27] Jankovic et al.,[28] Jankovic et al.,[29] and Padma et al.[30] In addition, 5 authors[28,29,30,35,38] did not describe the type of centrifuge (hardware) used.
Figure 2.
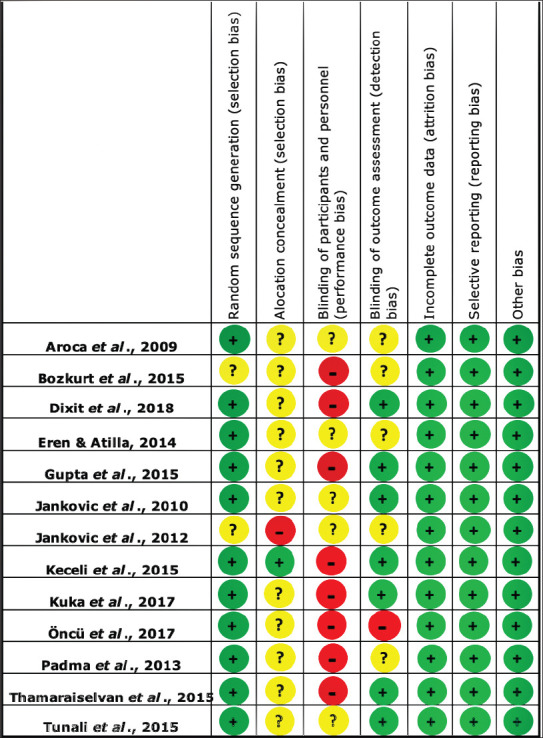
Risk of bias of the randomized controlled trials
Figure 3.
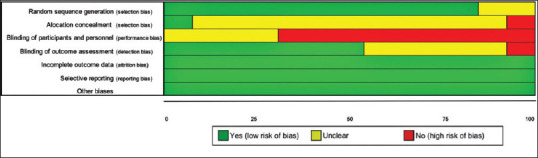
Risk of bias color score. Green, low risk of bias; yellow, unclear bias; red, high risk of bias
Only the technique of CAF[29,30,31,32,34,35,36,38,39] and its modification (MCAF)[27,28,33,37] was surgically applied. Five articles chose[29,31,34,36,37] CTG as the control group, and 7 only raised the flap and repositioned it coronally.[27,30,32,33,35,38,39] One study used EMD as the control group[28]. The test group in all RCTs was the APC group.[27,28,29,30,31,32,33,34,35,36,37,38,39] One study[32] used concentrated growth factor (CGF), which is considered third-generation APC.
According to the conclusions described in each study, 4[27,28,32,34] considered that PRF offered no additional benefit in terms of MRC or short-term wound healing for the treatment of multiple GRs;[27] the findings were not sufficient to advocate the clinical effect of PRF,[34] and no relevant advantages or benefits compared to the controls were reported.[28,32,34] On the other hand, some authors[28,29,31,36,37] reported avoiding using a donor site and decreased discomfort postoperatively in the APC group. Moreover, APC helped in early healing[33,35] in the first[28] and 2nd weeks,[29] due to the presence of growth factors,[34] which might have enhanced the results. APC provided additional benefits along with MRC in the treatment of RT1 GR when compared with CAF alone;[30] CAF + PRF was considered a superior choice for treatment over the control,[33] beyond interesting results in better soft-tissue healing[39] and a significant increase in the gingival thickness (GT), which might improve the predictability and long-term stability of the soft tissue in RC.[33,38] Moreover, authors[34,35] reported that PRF might have positive, albeit weak, but significant clinical results for RC.
Bias was more likely to exist in non-RCTs.[53] Only one study[27] included patients who smoked, despite the controversy in the literature about its negative influence of smoking on periodontal healing[54] or a high success rate after accomplished RC surgery (CAF)[55] [Table 3].
Table 3.
Articles extracted from the SRs included in this study, which were included in the meta-analysis
| Authors, year | SRs included that cited | Protocol applied | Follow-up | Design | Weight (%) | Conclusions* |
|---|---|---|---|---|---|---|
| Aroca et al., 2009 | Del Fabbro et al., 2011; Chambrone and Tatakis, 2015, Luo et al., 2015, Moraschini and Barboza, 2016; Castro et al., 2017 (5 articles) | Hardware: EBA 20, Hettich GmbH and Co KG, Tuttlingen, Germany; Setting: 3000 r.p.m./10 min. (Tube type: NR); (named: fibrin clot, PRF); 4 membranes prepared (but is not clearly described if the authors applied the four membranes in situ) | 6 months | RCT Split-mouth not blind (miller Class I and II) | 13.16 | Multiple gingival recessions indicated that MCAF surgery alone or in combination with PRF are effective procedures to cover denuded roots. No additional benefit in terms of mean root coverage or short-term wound healing for the treatment of multiple gingival recessions (PRF group) |
| Jankovic et al., 2010 | Chambrone and Tatakis, 2015; Moraschini and Barboza, 2016; Amine et al., 2017; Castro et al., 2017; Chambrone et al., 2019 (5 articles) | Hardware: NR; Setting: 3000 r.p.m. (approximately 400G)/10 min. (Tube type: NR); (named: PRF); 1 membrane | 12 months | RCT Split-mouth Not blind (Miller Class I and II) | 13.16 | Both techniques proved to be clinically successful in the treatment of GR. Minor advantages of PRF membrane use as graft material are related to advanced tissue healing during the 1st week postsurgery and a decrease in patient discomfort during the early wound healing period. The study did not succeed in demonstrating any clinical advantage of the use of PRF compared to EMD in coverage of GR (MCAF) |
| Jankovic et al., 2012 | Valenzuela and Oliva, 2014; Chambrone and Tatakis, 2015; Moraschini and Barboza, 2016; Amine et al., 2017; Castro et al., 2017 (5 articles) | Hardware: NR; Setting: 3000 r.p.m. (approximately 400G)/10 min. (Tube type: NR); (named: PRF); 1 membrane | 6 months | RCT Split-mouth single-blind (miller Class I and II) | 13.16 | Clinical implications and advantages of PRF membrane as a graft material are related to avoidance of a donor site surgical procedure, advanced tissue healing for the first 2 weeks postsurgery, and a major decrease in patient discomfort during the early wound-healing period. A high level of observed clinical parameter equivalence between CTG and PRF groups powerfully supports the clinical value of PRF use |
| Padma et al. 2013 | Luo et al., 2015; Moraschini and Barboza, 2016; Amine et al., 2017; Castro et al., 2017; Li et al., 2019 (5 articles) | Hardware: NR; Setting: 3000 r.p.m./10 min. (Tube type: NR); (named: PRF); 1 membrane | 6 months | RCT split-mouth Not blind (Miller Class I and II) | 13.16 | CAF surgery alone or in combination with PRF are effective procedures to cover denuded roots. The data obtained from a combination of CAF-PRF after a period of 6 months showed additional benefits along with mean root coverage in the treatment of miller’s class I and II gingival recessions when compared with the CAF technique alone |
| Thamaraiselvan et al., 2015 | Moraschini and Barboza, 2016; Amine et al., 2017; Castro et al., 2017; Li et al., 2019 (4 articles) | Hardware: NR; Setting: 3000 r.p.m./10 min. (Following original technique, Choukroun et al. 2001*); (Tube type: NR); (named: fibrin clot, PRF); 1 membrane | 6 months | RCT parallel Single-blind (Miller Class I and II) | 10.54 | The ease of applying PRF in the dental clinic and its beneficial outcomes, including reduction of bleeding and rapid healing, holds promise even though the mechanisms involved are still poorly understood |
| Eren and Atilla, 2014 | Moraschini and Barboza, 2016; Amine et al., 2017; Castro et al., 2017 (3 articles) | Hardware: Nüve Laboratory Equipments, NF200, Ankara, Turkey; Setting: 400G/12 min. (Glass-coated plastic tube); (named: fibrin clot, PRF); 1 membrane (thickness of 1 mm; PRF membrane was doubled by placing one part onto the other) | 6 months | RCT split-mouth Single-blind (Miller Class I and II) | 7.89 | A clinical advantage of PRF as a graft material is related to avoidance of a donor site and a major decrease in patient discomfort after operation. Due to these features, it could be concluded that CAF + PRF technique may represent an alternative to the traditional CAF + SCTG technique |
| Tunali et al., 2015 | Moraschini and Barboza, 2016; Castro et al., 2017; Chambrone et al., 2019 (3 articles) | Hardware: EBA 20, Hettich GmbH and Co KG, Tuttlingen, Germany; Setting: 2700 r.p.m./12 min. (Prepared according to the protocol developed by Choukroun et al. in 2001 - Process Protocol*); (Glass tube); (named: L-PRF, autologous PRF); 1 membrane | 12 months | RCT Split-mouth Single-blind (Miller Class I and II) | 7.89 | L-PRF membrane, in combination with a CAF procedure, is safe and effective for the treatment of Miller Class I and II gingival recession defects, without the significant morbidity or potential clinical difficulties associated with donor-site surgery |
| Gupta et al., 2015 | Castro et al., 2017; Li et al., 2019 (2 articles) | Hardware: RC-4, REMI Laboratories, Mumbai, India; Setting: 2700 r.p.m./12 min. (Glass tube); (named: PRF clot, PRF membrane); 1 membrane (1 mm area of RBC layer as the leukocytes and platelets are found to be concentrated at the junction of PRF clot and RBC layer) | 6 months | RCT Parallel Not blind (miller Class I and II) | 5.26 | It can be safely concluded that CAF alone and in combination with PRF membrane is a highly predictable procedure for the treatment of miller Class I and Class II gingival recessions. However, PRF provided an additional advantage of earlier healing and quicker attainment of optimal gingival tissue thickness which was maintained throughout the follow-up period. As adequate gingival tissue thickness is a known predictive factor for long-term stability of soft tissue recession coverage; it can be inferred that the use of PRF in conjunction with CAF can prove to be a superior choice for the treatment of such defects. PRF being an autologous material might possess both regenerative capacities as well as resorption potential. |
| Keceli et al., 2015 | Castro et al., 2017; Chambrone et al., 2019 (2 articles) | Hardware: Mikro 22 R Hettich Centrifugal Machine, Tuttlingen, Germany; Setting: NR (Tube type: NR); (named: L-PRF); 1 membrane | 6 months | RCT split-mouth Single-blind (Miller Class I and II) | 5.26 | PRF does not develop the primary outcome like obtained with CAF + CTG. It might have positively, albeit weakly, an important clinical variable in recession treatment, by the activity of growth factors and the fibrin matrix constituent. However, this finding is still not sufficient to advocate the true clinical effect of PRF |
| Öncü et al., 2017 | Chambrone et al., 2019 (1 article) | Hardware: PC-02, Process; Setting: 2700 r.p.m./12 min (Glass-coated plastic tube); (named: fibrin clot, PRF); 1 membrane | 6 months | RCT split-mouth (multiple gingival recession) (Miller Class I and II) | 2.63 | Control and test were effective. PRF avoids a donor site, which means a major decrease in postoperative discomfort |
| Bozkurt et al., 2015 | Li et al., 2019 (1 article) | Hardware: Medifuge, Silfradentsr, S. Sofia, Italy; Setting: CGF (30′′ acceleration, 2’ 2700 r.p.m., 4’ 2400 r.p.m., 4’ 2700 r.p.m., 3’ 3000 r.p.m., and 36′′ deceleration and stop)/14:06 min. (Glass-coated plastic tube); (named: CGF); 1 membrane (thickness of 1 mm) | 6 months | RCT split-mouth RCT split-mouth (Miller Class I and II) | 2.63 | CGF + CAF was not superior to CAF alone in providing a consistent reduction in the baseline recession |
| Kuka et al., 2017 | Li et al., 2019 (1 article) | Hardware: Hettich EBA 20 centrifuge, Tutlingen, Germany; Setting: 3000 r.p.m./10 min. (Following De Sanctis and Zucchelli technique, 2007*); (Tube type: Glass-coated plastic tube); (named: PRF); 1 membrane | 12 months | RCT split-mouth (only Miller Class I) | 2.63 | CAF + PRF and CAF approaches were successful in root coverage of multiple Miller class I gingival recessions. Clinically, the CAF + PRF procedure resulted in better soft tissue healing. PRF might be an alternative to different grafting materials for the treatment of multiple gingival recessions |
| Dixit et al., 2018 | Li et al., 2019 (1 article) | Hardware: NR; Setting: 2700 r.p.m./12 min. (Tube type: NR; only 6 mL); (named: PRF); 1 membrane | 6 months | RCT split-mouth (Miller Class I and II) | 2.63 | Single tooth gingival recessions by CAF indicated that only benefit of the addition of PRF appears to be a significant increase in the thickness of gingiva which may improve the predictability and long-term maintenance of achieved soft tissue root coverage |
The weight of each work was evaluated proportionally appear in other SRs; *Reported by authors[2]. PRF – Platelet-rich in fibrin; L-PRF – Leukocyte- platelet-rich in fibrin; CAF – Coronally advanced flap; GR – Gingival recession; SCTG – Subepithelial connective tissue graft; CGF – Concentrated growth factor; EMD – Enamel matrix derivative; SR – Systematic review; RCT – Randomized controlled trials; MCAF – Modification CAF. Articles referred (protocols): Choukroun J, Adda F, Schoeffler C, Vervelle A. An opportunity in perioimplantology: The PRF [in French]. Implantodontie 2001;42:55-62. (The L-PRF was prepared according to the protocol developed by Choukroun et al. in 2001 (Process Protocol)); Dohan Ehrenfest DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:37-44. (The blood was quickly collected, and the tubes were immediately centrifuged at 2,700 rpm for 12 min 5 using a Hettich Universal 320 table centri- fuge (Hettich Instruments) at room temperature); De Sanctis M, Zucchelli G. Coronally advanced flap: A modified surgical approach for isolated recession-type defects: Three-year results. J Clin Periodontol 2007;34:262-8 (protocol used 3000 r.p.m. × 10 min.); Tatakis DN, Chambrone L, Allen EP, Langer B, McGuire MK, Richardson CR, et al. Periodontal soft tissue root coverage procedures: A consensus report from the AAP regeneration workshop. J Periodontol 2015;86:S52-5. (use of glass-coat plastic tube), RPM – Revolutions per minute; NR – Not Reported; G – Gravitational force; CTG – Connective tissue graft; RBC – Red blood cells
Publication bias and statistical analysis
The parameters RD, CAL, CRC, MRC, and RC (mm) were obtained to fill Table 4. Only the parameters RD, CAL, and RC were used in the meta-analysis, which combined only similar comparisons that reported the same outcome measures. Due to the extreme difference observed in the results of Öncü[37] for RC, due to be considered not well-conducted with very wide confidence interval and weak strength, it was excluded from the meta-analysis.
Table 4.
Parameters obtained from randomized controlled trials included in Meta-analysis. recession depth, clinical attachment level, complete root coverage (%), mean root coverage (%), and root coverage (mm)
| Authors/year | Cited by (ref) | n | RD M (f) C | RD (f) SD C | RD M (f) T | RD (f) SD T | CAL M C | CAL SD C | CAL M T | CAL SD T | CRC (%) C | CRC (%) T | MRC (%) C | MRC (%) (SD) C | MRC (%) T | MRC (% SD) T | RC (mm) C | RC (mm) SD C | RC (mm) T | RC (mm) SD T |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aroca et al., 2009 | [64,65,67,68,69] | 20 | 0.2 | 0.4 | 0.6 | 0.6 | 2.56 | 1.24 | 2.47 | 1.36 | 74.62 | 52.23 | 91.5 | 11.4 | 80.7 | 14.7 | 2.3 | 0.5 | 2.3 | 0.5 |
| Bozkurt et al., 2015 | [70] | 20 | 0.56 | 0.53 | 0.43 | 0.50 | 2.58 | 0.62 | 2.83 | 0.62 | 45.8 | 56.7 | 82.06 | 17.49 | 86.67 | 15.59 | 2.29 | 0.56 | 2.47 | 0.54 |
| Dixit et al., 2018 | [70] | 12 | 0.58 | 1.00 | 0.50 | 0.52 | 2.17 | 0.83 | 2.08 | 0.67 | NR | NR | 79.5 | NR | 82.87 | NR | 2.25 | 0.12 | 2.42 | 0.38 |
| Eren and Atilla, 2014 | [51,64,69] | 22 | 0.16 | 0.33 | 0.18 | 0.32 | 1.59 | 0.65 | 1.32 | 0.55 | 77.3 | 72.7 | 94.2 | NR | 92.7 | NR | 2.45 | 0.34 | 2.49 | 0.29 |
| Gupta et al., 2015 | [64,70] | 26 | 0.40 | 0.74 | 0.27 | 0.59 | 2.47 | 0.74 | 3.27 | 0.8 | 73.3 | 80 | 86.6 | 23.83 | 91 | 19.98 | 2.07 | 0.59 | 2.53 | 0.64 |
| Jankovic et al., 2010 | [51,64,65,66,69] | 20 | 1.15 | 0.65 | 1.05 | 0.45 | NR | NR | NR | NR | 60 | 65 | 70.5 | 11.76 | 72.1 | 9.55 | 2.75 | 0.61 | 3.05 | 0.76 |
| Jankovic et al., 2012 | [51,64,65,69,71] | 15 | 0.38 | 0.48 | 0.68 | 0.45 | 2.96 | 0.42 | 2.87 | 0.39 | 79.56 | 75.85 | 70.5 | NR | 72.1 | NR | 3.07 | 0.3 | 2.83 | 0.37 |
| Keceli et al., 2015 | [52,66] | 40 | 0.7 | 0.45 | 0.25 | 0.37 | 1.70 | 0.66 | 1.35 | 0.52 | 35 | 55 | 79.9 | NR | 89.6 | NR | 2.50 | 0.77 | 3.41 | 0.83 |
| Kuka et al., 2018 | [70] | 24 | 0.85 | 0.24 | 0.40 | 0.52 | 2.8 | 0.35 | 2.15 | 0.78 | 74.63 | 88.36 | 74.63 | 8.05 | 88.36 | 15.45 | 2.51 | 0.33 | 2.75 | 0.35 |
| Öncü et al., 2017 | [66] | 20 | 0.68 | 0.92 | 0.90 | 1.03 | 1.77 | 0.97 | 2.07 | 1.17 | 60 | 50 | 84 | NR | 77.12 | NR | 3.49 | 0.09 | 3.03 | 0.1 |
| Padma et al. 2013 | [51,64,68,69,70] | 15 | 1.13 | 0.72 | 0 | 0 | 2.69 | 0.36 | 3.75 | 1.9 | NR | NR | 68.44 | 17.42 | 100 | 0 | 2.31 | 0.49 | 3.44 | 1.09 |
| Thamaraiselvan et al., 2015 | [51,64,69,70] | 20 | 1.6 | 0.51 | 1.3 | 0.91 | 1.8 | 0.91 | 2.5 | 1.17 | 50 | 50 | 65 | 44.47 | 74.16 | 28.98 | 1.3 | 0.08 | 1.6 | 0.27 |
| Tunali et al., 2015 | [64,66,69] | 10 | 0.98 | 0.75 | 1.05 | 0.74 | 3.04 | 0.7 | 2.7 | 1.04 | 18.2 | 13.6 | 77.36 | NR | 76.63 | NR | 3.04 | 0.77 | 3.4 | 0.83 |
Black boxes – Information provided by SR; White boxes – Information collected manually from the original articles; NR – Not reported; C – Control group; T – Test Group; RD – Recession depth; CAL – Clinical attachment level; CRC – Complete root coverage; MRC – Mean root coverage; RC – Root coverage; SD – Standard deviation; M – Mean; F – Final; SR – Systematic review
The outcome variables from each study were combined for continuous data, using a random-effects model because of the high heterogeneity found (I2RD = 80.14%; I2CAL = 73.53%; I2RC = 67.7%), confirmed by Tau that represents the amount of true heterogeneity. The results were graphically presented by forest plots [Figure 4]. Funnel plots [Figure S1 (544.7KB, tif) ] and normal Q-Q plots [Figure S2 (806KB, tif) ] assessed the publication bias. The patient was considered the unit of analysis.
Figure 4.
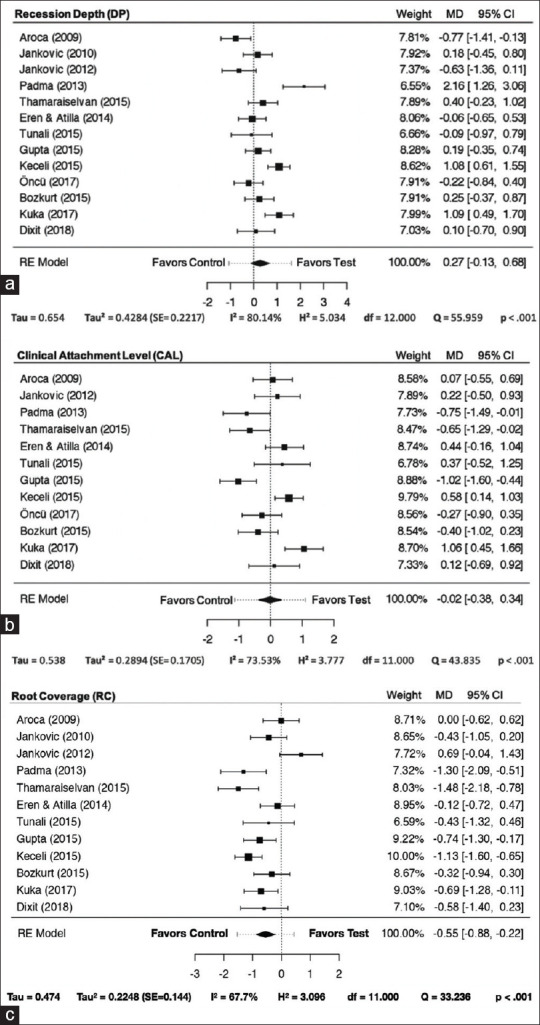
Forest plot. (a) Recession depth; (b) Clinical attachment level; (c) Root coverage; MD - Mean deviation; CI - Confidence interval; RE - Random-effects
The forest plots [Figure 4a-c] evaluated RD, CAL, and RC, and there was no significant statistical significance among the groups (P = 0.179, 0.922, and 0.652, respectively). In RD, the result was slightly favorable to PRF treatment (0.27 [−0.13–0.68]), increasing the heterogeneity caused mainly by Padma et al.[30] CAL remained practically neutral. The RC favored the control group (−0.55 [−0.88–0.22]).
The funnel plots showed asymmetry, represented by points outside the triangular area of the 95% CI region, which indicated a possibility of publication bias. Three studies of CAL and RC, and 5 of RD, increased the RC heterogeneity (I2) significantly, contributing to the asymmetry [Figure S1 (544.7KB, tif) ]. The Q-Q plot presented a similar result only for RC, with 4 studies outside the line [Figure S2 (806KB, tif) and Table 4].
DISCUSSION
Autologous platelet concentrate/platelet-rich fibrin generations, protocol, and number of membranes surgically applied
There are three generations of APCs/PRFs. The first generation is mainly represented by the platelet-rich plasma.[48] The second generation is represented by PRF, which is a superior scaffold[56] and induces a significant release of cytokines[57,56] from a three-dimensional fibrin matrix, creating an enhanced process of healing when gradually released after the fibrin matrices resorb.[58,59] Since then, PRF has been extensively applied.[25,48,60,57] For the third-generation, a modification was proposed, which is the CGF,[61] alternating the centrifugation speed from 2400 rpm (547 g) to 3000 rpm (855 g) with different times. This last generation is characterized by containing abundant CGF in its rigid fibrin,[61] yielding results in speeding tissue proliferation and differentiation up.[62]
The present study did not accept investigations[26,44,46,50,51] that included the first generation of APC because of the lack of membrane structure, which is viscous and difficult to keep entirely on the surgical site, creating bias concerning the efficiency and outcomes. Therefore, the second[27,28,29,30,31,33,34,35,36,37,38,39] and third[32] generations were included, with no significant differences between them, contradicting the literature.[50] The studies relied on the superiority of continuously releasing many growth factors and molecules, accelerating cell proliferation and migration, stimulating the synthesis of Type I collagen, and neoangiogenesis.[63] In addition, second- and third-generation APC is easier to handle, insert, and keep in position, during periodontal surgeries. Moreover, it has increased anti-inflammatory and antibacterial effects, and the membrane remained solid after 1 week, compared to the first generation, which after 3 days completely dissolved, releasing the growth factors only in the 1st h.[64]
A limitation of this review was that none of included articles conducted an APC/PRF qualification or quantification of the levels of the cells, growth factors, cytokines, or other molecular components.[65] This step is important because it plays a significant role in the self-regulation of inflammatory and infectious phenomena.[55] Moreover, there is a lack of standardized protocol for preparing[47,48,49] and handling of APC/PRF (e.g., how many membranes should be placed per surgical site), limiting the data interpretation.[48] Only 3 out of 9 SRs described the protocol applied, 2700 RPM/12 min, 3000 RPM/10 min,[47,48] or still 400 g/10 min.[45] Of the initially enrolled studies, five[28,29,30,35,38] did not report the hardware used, limiting the equipment details and likely resulting in different structured APC membranes. In addition, Castro et al.[48] discussed the handle and number of APC membranes, with one membrane elected as the treatment standard for all RCTs in that study. Only Aroca et al.[27] prepared 4 membranes, and it is unclear whether they applied all in situ. No study standard gave a minimum thickness and/or the number of membranes to treat GR. Subsequently, it might be suggested that 4 unfolded or at least 2 folded membranes to be used to achieve a significant substantivity in the long-term.
A possible substitute for connective tissue graft
The primary reason to substitute CTG is based on the incidence of adverse effects such as discomfort with or without pain related to donor sites within the first postoperative week.[44] Although 4 out of 7 SRs[45,46,48,51] described favorable adjunctive effects from APC on soft-tissue healing, postoperative discomfort reduction, and positive results in RD and CAL, another 3[44,47,49] reported contradictory results with nonsignificant benefit,[66] still recommending CTG as the gold-standard procedure for RC and CAL to treat RT1 GR defects.
The literature remains controversial on the clinical outcomes of APC/PRF in GR defects. Superior results for CTG with improved long-term tissue stability[67] compared to APC/PRF were previously reported. On the other hand, Li et al.[51] considered that PRF “should be preferred,” and Valenzuela and Oliva[45] concluded that the regeneration efficacy of PRF is effective. Only one SR[46] suggested that the addition of APC/PRF might exert a positive adjunctive effect. Nevertheless, the current study verified a divided opinion on APC/PRF application on GR coverage, but with more SRs in favor of using APC during RC procedures.
Some interesting findings can give greater support to the use of PRF, which has the potential to shorten the treatment period;[29] in addition, it induces a decrease of matrix metalloproteinase-8 (MMP-8) and interleukin-1 beta, and an increase in a tissue inhibitor of MMP-1 levels within 10 days, promoting periodontal wound healing in the earlier phase of the process.[68]
Surgical technique used in the included studies
The only surgical technique used for all studies was the CAF and MCAF, considered the gold-standard procedure. Both techniques require periosteal incisions, eliminating the muscle tension.[1,69] The MCAF precludes the need for vertical incisions and sutures, thus achieving better and stable RC.
A difference in preference was observed among the studies between CAF and MCAF. Moraschini et al.[47] considered CAF instead of MCAF that was used by Aroca et al.,[27] while another study[50] stated CAF and MCAF as the “same procedure.” However, current knowledge shows that CAF yields an inferior result compared to MCAF,[70] and outcomes showed a significant correlation between long-term stability and regular maintenance. The MCAF results after one year for CRC and MRC were, respectively, 88% and 97%,[71] and after 5 years, 85% and 94.6%.[70] CAF and MCAF, when compared, achieved a respective CRC of 77.7% versus 89.3%,[72] with MCAF presenting a higher success rate. MCAF had a favorable result beyond a better postoperative course, with less scar tissue formation.
Periodontal parameters assessed
The mean percentage of RC among the studies may range between 9% and 100%[73] and is influenced by different prognostic factors, categorization, and professional experience.[50] This SR observed that MRC ranged between 65% and 100%, indicating agreement with the literature.
The maintenance of long-term success for GR treatment remains unclear since most of the studies had a limited period of follow-up, 6–12-month.[27,28,29,30,31,32,33,34,35,36,37,38,39] In addition, factors such as KTW and GT that influenced the outcomes of RC were not included in the analyses.[74] However, GT and KTW were not the aims of this study, and as previously stressed in a SR by Tavelli and coworkers,[75] scarce information regarding the effect of GT on RC on published studies impedes a deeper look into this aspect. If applied APC/PRF as a substitute, promising results have been found,[31] which may be explained by the biology of APC/PRF (contains several growth factors influencing tissue proliferation).[31,37] Nonetheless, this statement needs to be confirmed with further studies.
The main outcomes set were RD, CAL, and RC, appropriate for assessing GR treatment. Of all RCTs, only one[30] achieved 100% success in the test group to reduce RD, providing superior RC (almost 1 mm more), and CAL gained more than 1 mm. Furthermore, less morbidity, enhanced healing,[29] and fewer clinical difficulties occurred with donor-site surgery.[31,36,37] Twelve studies[27,28,29,30,31,32,33,34,35,36,37,38,39] provided no additional advantage of APC for RC.
The results between APC/PRF and controls had similar success rates, as previously reported.[76] RD reduction results were more promising in the APC/PRF group[28,32,33,34,35,38,39] as in the literature.[58] Twelve RCTs assessed CAL and showed no significant benefit of APC/PRF in CAL gain. RCTs were evaluated for RC percentage, and the results showed that APC/PRF with CAF exerted a slightly less satisfactory outcome than the control (CAF/MCAF alone or associated with CTG). To add to the controversy, another SR reported favorable outcomes highlighted in the APC group.[58] There was no statistical significance in any parameters. Nonetheless, neither RCTs followed up longer than 12 months nor reported adherence to the CONSORT statement.[77] Longer follow-up studies are warranted to confirm conclusions, and adherence to the PROSPERO, PRISMA, and CONSORT statements[78] is essential to increase the quality and transparency of studies.[54]
There is an enthusiasm for the use of APC/PRF to cover the exposed root. However, it is primarily necessary to define a standard reproducible technique to obtain an optimal effect of the APC/PRF. Nevertheless, a divided opinion was kept for the treatment of RT1 (Miller's Class I and II). On the one hand, vast confusion was caused by the RCTs regarding the lack of recommendations for APCs/PRFs. In contrast, considering the superiority of the SRs studies, a majority recommended the use of APC/PRF as a feasible substitute biomaterial for GR treatment. Therefore, the main result found in this SR to treat GR with RC procedures showed better overall response for the control groups.
CONCLUSIONS
Within the limitations of this SR, the utilization of the APC/PRF membranes, although a valid alternative to the traditional CTG, showed inferior results in terms of RC. Prospective investigations, including analysis of GT and KTW, are required since they have been demonstrated as significant prognostic factors for long-term outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Funnel plot of the included studies. A. Recession depth; B. Clinical attachment level; C. Root coverage
Normal Q-Q plot to verify the normality of the studies included. A. Recession depth; B. Clinical attachment level; C. Root coverage c
REFERENCES
- 1.Wennström JL. Mucogingival therapy. Ann Periodontol. 1996;1:671–701. doi: 10.1902/annals.1996.1.1.671. [DOI] [PubMed] [Google Scholar]
- 2.Camargo PM, Melnick PR, Kenney EB. The use of free gingival grafts for aesthetic purposes. Periodontol 2000. 2001;27:72–96. doi: 10.1034/j.1600-0757.2001.027001072.x. [DOI] [PubMed] [Google Scholar]
- 3.O'leary TJ, Drake RB, Jividen G, Allen MF. The incidence of gingival recession in young males: Relationship to gingival and plaque score. Periodontics. 1968;6:109–11. [PubMed] [Google Scholar]
- 4.Chambrone L, Chambrone LA. Gingival recessions caused by lip piercing: Case report. J Can Dent Assoc. 2003;69:505–8. [PubMed] [Google Scholar]
- 5.Priyanka M, Sruthi R, Ramakrishnan T, Emmadi P, Ambalavanan N. An overview of frenal attachments. J Indian Soc Periodontol. 2013;17:12–5. doi: 10.4103/0972-124X.107467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wennström JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J Clin Periodontol. 1987;14:121–9. doi: 10.1111/j.1600-051x.1987.tb00954.x. [DOI] [PubMed] [Google Scholar]
- 7.Stoner JE, Mazdyasna S. Gingival recession in the lower incisor region of 15-year-old subjects. J Periodontol. 1980;51:74–6. doi: 10.1902/jop.1980.51.2.74. [DOI] [PubMed] [Google Scholar]
- 8.De Rouck T, Eghbali R, Collys K, De Bruyn H, Cosyn J. The gingival biotype revisited: Transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J Clin Periodontol. 2009;36:428–33. doi: 10.1111/j.1600-051X.2009.01398.x. [DOI] [PubMed] [Google Scholar]
- 9.Chambrone L, Tatakis DN. Long-term outcomes of untreated buccal gingival recessions: A systematic review and meta-analysis. J Periodontol. 2016;87:796–808. doi: 10.1902/jop.2016.150625. [DOI] [PubMed] [Google Scholar]
- 10.Khocht A, Simon G, Person P, Denepitiya JL. Gingival recession in relation to history of hard toothbrush use. J Periodontol. 1993;64:900–5. doi: 10.1902/jop.1993.64.9.900. [DOI] [PubMed] [Google Scholar]
- 11.Parma-Benfenati S, Frigazzato PA, Ruben MP. The effect of restorative margins on the postsurgical development and nature of the periodontium.Part I. Int J Periodontics Restorative Dent. 1985;5:30–51. [PubMed] [Google Scholar]
- 12.Löe H, Anerud A, Boysen H. The natural history of periodontal disease in man: Prevalence, severity, and extent of gingival recession. J Periodontol. 1992;63:489–95. doi: 10.1902/jop.1992.63.6.489. [DOI] [PubMed] [Google Scholar]
- 13.Prato GP, Rotundo R, Magnani C, Ficarra G. Viral etiology of gingival recession.A case report. J Periodontol. 2002;73:110–4. doi: 10.1902/jop.2002.73.1.110. [DOI] [PubMed] [Google Scholar]
- 14.Chambrone L, Pannuti CM, Tu YK, Chambrone LA. Evidence-based periodontal plastic surgery. II. An individual data meta-analysis for evaluating factors in achieving complete root coverage. J Periodontol. 2012;83:477–90. doi: 10.1902/jop.2011.110382. [DOI] [PubMed] [Google Scholar]
- 15.Buti J, Baccini M, Nieri M, La Marca M, Pini-Prato GP. Bayesian network meta-analysis of root coverage procedures: Ranking efficacy and identification of best treatment. J Clin Periodontol. 2013;40:372–86. doi: 10.1111/jcpe.12028. [DOI] [PubMed] [Google Scholar]
- 16.Löst C. Depth of alveolar bone dehiscences in relation to gingival recessions. J Clin Periodontol. 1984;11:583–9. doi: 10.1111/j.1600-051x.1984.tb00911.x. [DOI] [PubMed] [Google Scholar]
- 17.Agudio G, Cortellini P, Buti J, Pini Prato G. Periodontal conditions of sites treated with gingival augmentation surgery compared with untreated contralateral homologous sites: An 18- to 35-year long-term study. J Periodontol. 2016;87:1371–8. doi: 10.1902/jop.2016.160284. [DOI] [PubMed] [Google Scholar]
- 18.Miller PD., Jr Regenerative and reconstructive periodontal plastic surgery.Mucogingival surgery. Dent Clin North Am. 1988;32:287–306. [PubMed] [Google Scholar]
- 19.Gapski R, Parks CA, Wang HL. Acellular dermal matrix for mucogingival surgery: A meta-analysis. J Periodontol. 2005;76:1814–22. doi: 10.1902/jop.2005.76.11.1814. [DOI] [PubMed] [Google Scholar]
- 20.Mahajan A, Bharadwaj A, Mahajan P. Comparison of periosteal pedicle graft and subepithelial connective tissue graft for the treatment of gingival recession defects. Aust Dent J. 2012;57:51–7. doi: 10.1111/j.1834-7819.2011.01648.x. [DOI] [PubMed] [Google Scholar]
- 21.Pini-Prato G, Nieri M, Pagliaro U, Giorgi TS, La Marca M, Franceschi D, et al. Surgical treatment of single gingival recessions: Clinical guidelines. Eur J Oral Implantol. 2014;7:9–43. [PubMed] [Google Scholar]
- 22.Dai A, Huang JP, Ding PH, Chen LL. Long-term stability of root coverage procedures for single gingival recessions: A systematic review and meta-analysis. J Clin Periodontol. 2019;46:572–85. doi: 10.1111/jcpe.13106. [DOI] [PubMed] [Google Scholar]
- 23.Saluja H, Dehane V, Mahindra U. Platelet-rich fibrin: A second generation platelet concentrate and a new friend of oral and maxillofacial surgeons. Ann Maxillofac Surg. 2011;1:53–7. doi: 10.4103/2231-0746.83158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang YC, Zhao JH. Effects of platelet-rich fibrin on human periodontal ligament fibroblasts and application for periodontal infrabony defects. Aust Dent J. 2011;56:365–71. doi: 10.1111/j.1834-7819.2011.01362.x. [DOI] [PubMed] [Google Scholar]
- 25.Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V, et al. Use of platelet-rich fibrin in regenerative dentistry: A systematic review. Clin Oral Investig. 2017;21:1913–27. doi: 10.1007/s00784-017-2133-z. [DOI] [PubMed] [Google Scholar]
- 26.Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: A systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86:S8–51. doi: 10.1902/jop.2015.130674. [DOI] [PubMed] [Google Scholar]
- 27.Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D. Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6-month study. J Periodontol. 2009;80:244–52. doi: 10.1902/jop.2009.080253. [DOI] [PubMed] [Google Scholar]
- 28.Jankovic S, Aleksic Z, Milinkovic I, Dimitrijevic B. The coronally advanced flap in combination with platelet-rich fibrin (PRF) and enamel matrix derivative in the treatment of gingival recession: A comparative study. Eur J Esthet Dent. 2010;5:260–73. [PubMed] [Google Scholar]
- 29.Jankovic S, Aleksic Z, Klokkevold P, Lekovic V, Dimitrijevic B, Kenney EB, et al. Use of platelet-rich fibrin membrane following treatment of gingival recession: A randomized clinical trial. Int J Periodontics Restorative Dent. 2012;32:e41–50. [PubMed] [Google Scholar]
- 30.Padma R, Shilpa A, Kumar PA, Nagasri M, Kumar C, Sreedhar A. A split mouth randomized controlled study to evaluate the adjunctive effect of platelet-rich fibrin to coronally advanced flap in Miller's class-I and II recession defects. J Ind Soc Periodontol. 2013;17:631–6. doi: 10.4103/0972-124X.119281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eren G, Atilla G. Platelet-rich fibrin in the treatment of localized gingival recessions: A split-mouth randomized clinical trial. Clin Oral Investig. 2014;18:1941–8. doi: 10.1007/s00784-013-1170-5. [DOI] [PubMed] [Google Scholar]
- 32.Bozkurt Doğan Ş, Öngöz Dede F, Ballı U, Atalay EN, Durmuğlar MC. Concentrated growth factor in the treatment of adjacent multiple gingival recessions: A split-mouth randomized clinical trial. J Clin Periodontol. 2015;42:868–75. doi: 10.1111/jcpe.12444. [DOI] [PubMed] [Google Scholar]
- 33.Gupta S, Banthia R, Singh P, Banthia P, Raje S, Aggarwal N. Clinical evaluation and comparison of the efficacy of coronally advanced flap alone and in combination with platelet rich fibrin membrane in the treatment of Miller Class I and II gingival recessions. Contemp Clin Dent. 2015;6:153–60. doi: 10.4103/0976-237X.156034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keceli HG, Kamak G, Erdemir EO, Evginer MS, Dolgun A. The adjunctive effect of platelet-rich fibrin to connective tissue graft in the treatment of buccal recession defects: Results of a randomized, parallel-group controlled trial. J Periodontol. 2015;86:1221–30. doi: 10.1902/jop.2015.150015. [DOI] [PubMed] [Google Scholar]
- 35.Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian Soc Periodontol. 2015;19:66–71. doi: 10.4103/0972-124X.145790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tunalι M, Özdemir H, Arabacι T, Gürbüzer B, Pikdöken L, Firatli E. Clinical evaluation of autologous platelet-rich fibrin in the treatment of multiple adjacent gingival recession defects: A 12-month study. Int J Periodontics Restorative Dent. 2015;35:105–14. doi: 10.11607/prd.1826. [DOI] [PubMed] [Google Scholar]
- 37.Öncü E. The use of platelet-rich fibrin versus subepithelial connective tissue graft in treatment of multiple gingival recessions: A randomized clinical trial. Int J Periodontics Restorative Dent. 2017;37:265–71. doi: 10.11607/prd.2741. [DOI] [PubMed] [Google Scholar]
- 38.Dixit N, Lamba AK, Faraz F, Tandon S, Aggarwal K, Ahad A. Root coverage by modified coronally advanced flap with and without platelet-rich fibrin: A clinical study. Indian J Dent Res. 2018;29:600–4. doi: 10.4103/ijdr.IJDR_22_17. [DOI] [PubMed] [Google Scholar]
- 39.Kuka S, Ipci SD, Cakar G, Yılmaz S. Clinical evaluation of coronally advanced flap with or without platelet-rich fibrin for the treatment of multiple gingival recessions. Clin Oral Investig. 2018;22:1551–8. doi: 10.1007/s00784-017-2225-9. [DOI] [PubMed] [Google Scholar]
- 40.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14:579. doi: 10.1186/s12913-014-0579-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Del Fabbro M, Bortolin M, Taschieri S, Weinstein R. Is platelet concentrate advantageous for the surgical treatment of periodontal diseases.A systematic review and meta-analysis? J Periodontol. 2011;82:1100–11. doi: 10.1902/jop.2010.100605. [DOI] [PubMed] [Google Scholar]
- 45.Valenzuela HM, Oliva MP. Regeneration efficacy of platelet-rich fibrin in patients undergoing periodontal surgery: A systematic review and meta-analysis. Int J Odontostomatol. 2014;8:21–8. [Google Scholar]
- 46.Luo HY, Li RM, Wang CL, Peng L, Ye L. The adjunctive use of platelet concentrates in the therapy of gingival recessions: A systematic review and meta-analysis. J Oral Rehabil. 2015;42:552–61. doi: 10.1111/joor.12278. [DOI] [PubMed] [Google Scholar]
- 47.Moraschini V, Barboza Edos S. Use of platelet-rich fibrin membrane in the treatment of gingival recession: A systematic review and meta-analysis. J Periodontol. 2016;87:281–90. doi: 10.1902/jop.2015.150420. [DOI] [PubMed] [Google Scholar]
- 48.Castro AB, Meschi N, Temmerman A, Pinto N, Lambrechts P, Teughels W, et al. Regenerative potential of leucocyte- and platelet-rich fibrin. Part A: Intra-bony defects, furcation defects and periodontal plastic surgery. A systematic review and meta-analysis. J Clin Periodontol. 2017;44:67–82. doi: 10.1111/jcpe.12643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Amine K, El Amrani Y, Chemlali S, Kissa J. Alternatives to connective tissue graft in the treatment of localized gingival recessions: A systematic review. J Stomatol Oral Maxillofac Surg. 2018;119:25–32. doi: 10.1016/j.jormas.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 50.Chambrone L, Ortega MA, Sukekava F, Rotundo R, Kalemaj Z, Buti J, et al. Root coverage procedures for treating single and multiple recession-type defects: An updated Cochrane systematic review. J Periodontol. 2019;90:1399–422. doi: 10.1002/JPER.19-0079. [DOI] [PubMed] [Google Scholar]
- 51.Li R, Liu Y, Xu T, Zhao H, Hou J, Wu Y, et al. The additional effect of autologous platelet concentrates to coronally advanced flap in the treatment of gingival recessions: A systematic review and meta-analysis. Biomed Res Int. 2019;2019:2587245. doi: 10.1155/2019/2587245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kobayashi E, Flückiger L, Fujioka-Kobayashi M, Sawada K, Sculean A, Schaller B, et al. Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin Oral Investig. 2016;20:2353–60. doi: 10.1007/s00784-016-1719-1. [DOI] [PubMed] [Google Scholar]
- 53.Rodella LF, Favero G, Boninsegna R, Buffoli B, Labanca M, Scarì G, et al. Growth factors, CD34 positive cells, and fibrin network analysis in concentrated growth factors fraction. Microsc Res Tech. 2011;74:772–7. doi: 10.1002/jemt.20968. [DOI] [PubMed] [Google Scholar]
- 54.Anitua E, Sánchez M, Nurden AT, Nurden P, Orive G, Andía I. New insights into and novel applications for platelet-rich fibrin therapies. Trends Biotechnol. 2006;24:227–34. doi: 10.1016/j.tibtech.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 55.Dohan Ehrenfest DM, de Peppo GM, Doglioli P, Sammartino G. Slow release of growth factors and thrombospondin-1 in Choukroun's platelet-rich fibrin (PRF): A gold standard to achieve for all surgical platelet concentrates technologies. Growth Factors. 2009;27:63–9. doi: 10.1080/08977190802636713. [DOI] [PubMed] [Google Scholar]
- 56.Takeda Y, Katsutoshi K, Matsuzaka K, Inoue T. The effect of concentrated growth factor on rat bone marrow cells in vitro and on calvarial bone healing in vivo. Int J Oral Maxillofac Implants. 2015;30:1187–96. doi: 10.11607/jomi.3995. [DOI] [PubMed] [Google Scholar]
- 57.Dohan Ehrenfest DM, Bielecki T, Jimbo R, Barbé G, Del Corso M, Inchingolo F, et al. Do the fibrin architecture and leukocyte content influence the growth factor release of platelet concentrates.An evidence-based answer comparing a pure platelet-rich plasma (P-PRP) gel and a leukocyte- and platelet-rich fibrin (L-PRF)? Curr Pharm Biotechnol. 2012;13:1145–52. doi: 10.2174/138920112800624382. [DOI] [PubMed] [Google Scholar]
- 58.Bae JH, Kim YK, Myung SK. Effects of platelet-rich plasma on sinus bone graft: Meta-analysis. J Periodontol. 2011;82:660–7. doi: 10.1902/jop.2010.100529. [DOI] [PubMed] [Google Scholar]
- 59.Hofmänner P, Alessandri R, Laugisch O, Aroca S, Salvi GE, Stavropoulos A, et al. Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions – A systematic review. Quintessence Int. 2012;43:545–54. [PubMed] [Google Scholar]
- 60.Eren G, Tervahartiala T, Sorsa T, Atilla G. Cytokine (interleukin-1beta) and MMP levels in gingival crevicular fluid after use of platelet-rich fibrin or connective tissue graft in the treatment of localized gingival recessions. J Periodontal Res. 2016;51:481–8. doi: 10.1111/jre.12325. [DOI] [PubMed] [Google Scholar]
- 61.de Sanctis M, Zucchelli G. Coronally advanced flap: A modified surgical approach for isolated recession-type defects: Three-year results. J Clin Periodontol. 2007;34:262–8. doi: 10.1111/j.1600-051X.2006.01039.x. [DOI] [PubMed] [Google Scholar]
- 62.Zucchelli G, De Sanctis M. Long-term outcome following treatment of multiple Miller class I and II recession defects in esthetic areas of the mouth. J Periodontol. 2005;76:2286–92. doi: 10.1902/jop.2005.76.12.2286. [DOI] [PubMed] [Google Scholar]
- 63.Zucchelli G, De Sanctis M. Treatment of multiple recession-type defects in patients with esthetic demands. J Periodontol. 2000;71:1506–14. doi: 10.1902/jop.2000.71.9.1506. [DOI] [PubMed] [Google Scholar]
- 64.Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: An explorative and reliability study. J Clin Periodontol. 2011;38:661–6. doi: 10.1111/j.1600-051X.2011.01732.x. [DOI] [PubMed] [Google Scholar]
- 65.Fleming PS, Lynch CD, Pandis N. Randomized controlled trials in dentistry: Common pitfalls and how to avoid them. J Dent. 2014;42:908–14. doi: 10.1016/j.jdent.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 66.Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. The influence of tobacco smoking on the outcomes achieved by root-coverage procedures: A systematic review. J Am Dent Assoc. 2009;140:294–306. doi: 10.14219/jada.archive.2009.0158. [DOI] [PubMed] [Google Scholar]
- 67.Kaval B, Renaud DE, Scott DA, Buduneli N. The role of smoking and gingival crevicular fluid markers on coronally advanced flap outcomes. J Periodontol. 2014;85:395–405. doi: 10.1902/jop.2013.120685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, et al. Advanced platelet-rich fibrin: A new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol. 2014;40:679–89. doi: 10.1563/aaid-joi-D-14-00138. [DOI] [PubMed] [Google Scholar]
- 69.Simonpieri A, Del Corso M, Sammartino G, Dohan Ehrenfest DM. The relevance of Choukroun's platelet-rich fibrin and metronidazole during complex maxillary rehabilitations using bone allograft.Part I: A new grafting protocol. Implant Dent. 2009;18:102–11. doi: 10.1097/ID.0b013e318198cf00. [DOI] [PubMed] [Google Scholar]
- 70.Choukroun J. An opportunity in paroimplantology: PRF. Implantodontie. 2001;42:55–62. [Google Scholar]
- 71.Verma UP, Yadav RK, Dixit M, Gupta A. Platelet-rich fibrin: A paradigm in periodontal therapy –A systematic review. J Int Soc Prev Community Dent. 2017;7:227–33. doi: 10.4103/jispcd.JISPCD_429_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zucchelli G, Mele M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M. Coronally advanced flap with and without vertical releasing incisions for the treatment of multiple gingival recessions: A comparative controlled randomized clinical trial. J Periodontol. 2009;80:1083–94. doi: 10.1902/jop.2009.090041. [DOI] [PubMed] [Google Scholar]
- 73.Pini-Prato G. The Miller classification of gingival recession: Limits and drawbacks. J Clin Periodontol. 2011;38:243–5. doi: 10.1111/j.1600-051X.2010.01655.x. [DOI] [PubMed] [Google Scholar]
- 74.Cairo F, Cortellini P, Pilloni A, Nieri M, Cincinelli S, Amunni F, et al. Clinical efficacy of coronally advanced flap with or without connective tissue graft for the treatment of multiple adjacent gingival recessions in the aesthetic area: A randomized controlled clinical trial. J Clin Periodontol. 2016;43:849–56. doi: 10.1111/jcpe.12590. [DOI] [PubMed] [Google Scholar]
- 75.Tavelli L, Barootchi S, Cairo F, Rasperini G, Shedden K, Wang HL. The effect of time on root coverage outcomes: A network meta-analysis. J Dent Res. 2019;98:1195–203. doi: 10.1177/0022034519867071. [DOI] [PubMed] [Google Scholar]
- 76.Sculean A, Gruber R, Bosshardt DD. Soft tissue wound healing around teeth and dental implants. J Clin Periodontol. 2014;41(Suppl 15):S6–22. doi: 10.1111/jcpe.12206. [DOI] [PubMed] [Google Scholar]
- 77.Schulz KF, Altman DG, Moher D CONSORT Group. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sarkis-Onofre R, Cenci MS, Demarco FF, Lynch CD, Fleming PS, Pereira-Cenci T, et al. Use of guidelines to improve the quality and transparency of reporting oral health research. J Dent. 2015;43:397–404. doi: 10.1016/j.jdent.2015.01.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Funnel plot of the included studies. A. Recession depth; B. Clinical attachment level; C. Root coverage
Normal Q-Q plot to verify the normality of the studies included. A. Recession depth; B. Clinical attachment level; C. Root coverage c